Abstract
Preterm infants are at high risk of brain injury, and high-dose recombinant erythropoietin (rEpo) may be therapeutic. However, the effect of rEpo on the development of retinopathy of prematurity (ROP) is unknown. We hypothesized that (1) rEpo would cross the blood–eye barrier and (2) early rEpo would modulate ROP in a rat model. Epo concentrations were measured by ELISA from the plasma and the homogenized eye tissue at timed intervals after rEpo injection. Flat-mounted retinas were prepared from rats given rEpo (0, 5000, or 30,000 U/kg i.p. qid × 3) on postnatal d (P) 1–3 that were raised in room air (RA) or cyclic oxygen exposure (COE) with O2 cycling every 24 h between 50% and 10% for 14 d. Photomicrographs of the fluorescein- or ADPase-stained P20 retinas were examined. rEpo penetrated into the eye in a dose- and time-dependent manner. COE increased retinal vascular pathology and decreased vessel density compared with RA controls. The 30,000 U/kg dose of rEpo increased the ROP clock hour scores, but only in ADPase-stained tissues. In contrast, 5000 U/kg rEpo did not change the incidence or severity of ROP by any measure. High-dose rEpo may protect against preterm brain injury with minimal impact on ROP.
Similar content being viewed by others
Main
Recombinant erythropoietin (rEpo) is commonly used to stimulate the red blood cell production in anemic preterm infants (1). However, functional Epo receptors are present on many cells including neurons, astrocytes, and endothelia, so rEpo effects are not limited to erythropoiesis (2–4). In the brain, rEpo decreases neuronal apoptosis (5,6), oxidative injury (7–11), excitotoxicity (12,13), and inflammation (11,14). rEpo also has protective effects on oligodendrocytes in vitro and in vivo (15–17). For at-risk preterm neonates, these properties could potentially reduce neuronal death or white matter injury, thereby improving neurodevelopmental outcomes (18).
The safety of rEpo doses used to promote erythropoiesis in preterm infants has been extensively studied, and one meta-analysis found that rEpo plus iron was associated with an increased risk (RR: 1.71, CI: 1.15–2.54) of stage 3 retinopathy of prematurity (ROP) (19), whereas three reports found no association (20–22). Because rEpo does not cross the BBB at low doses, neuroprotective doses are high: in neonatal studies doses range from 500 to 30,000 U/kg. We found that three daily injections of 5000 U/kg provided optimal neuroprotection in neonatal rats (23). Before large-scale clinical trials of early, high-dose rEpo in preterm infants, the potential effect of this drug on the development of ROP must be evaluated.
ROP is a developmental disorder characterized by the abnormal growth of immature blood vessels in the retina (24). The disease primarily affects low birth weight (<1250 g) and preterm infants born <31 wk gestation (25). Retinal vascularization begins around 16 wk gestation and continues to term gestation (26). It is hypothesized that exposure to oxygen at preterm birth disrupts retinal vascularization and thereby triggers ROP. ROP occurs in two phases, the first is characterized by a loss of retinal vasculature immediately after birth and the second is characterized by uncontrolled proliferation of retinal vessels. Several angiogenic cytokines that may contribute to ROP are under investigation. Focusing on Epo, it is important to note that Epo receptors are expressed by the fetal retina (2) and are necessary for normal retinal development (27). However, high concentrations of intraocular Epo are associated with diabetic retinopathy in adults (28). In a transgenic mouse model of ROP, down-regulation of the Epo gene decreased retinal vascular budding, whereas injection of rEpo exacerbated ROP (29). Thus, the rationale to understand the impact of rEpo on retinal vascular development is strong.
We previously speculated that early high-dose rEpo could have one of two opposing effects on the developing retina (30): (1) rEpo might sustain blood vessel growth immediately after preterm birth thus preventing the first phase of ROP or (2) rEpo may exacerbate the uncontrolled vascular proliferation characteristic of phase II ROP. To test these hypotheses, we characterized the effects of early high-dose rEpo in neonatal rats exposed to either 14-d cyclic oxygen exposure (COE) or room air (RA). In addition, we determined the dose-dependent pharmacokinetic penetration of systemic rEpo into the neonatal rat eye. These data describe the impact of high-dose rEpo on retinal vascular development in rats and help determine whether trials of high-dose rEpo for neuroprotection in the premature neonatal population may safely proceed.
METHODS
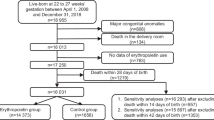
The Animal Care and Use Committees at the University of Washington in accordance with US National Institutes of Health guidelines approved all protocols. Timed-pregnant Sprague-Dawley rats (Harlan, San Diego, CA) were purchased to permit immediate exposure to cycling oxygen from birth until postnatal d (P) 14. Animals were housed with a 12 h light/dark cycle and fed ad libitum. Pups were initially weighed and distributed to create weight-matched litters (n = 9–13/litter, 194 total). Rats were euthanized with an overdose of Euthasol (Virbac AH Inc., Fort Worth, TX).
Pharmacokinetics.
P1 animals were injected i.p. with 500, 5000, or 30,000 U/Kg rEpo, and then killed at 2, 4, 6, 24, or 48 h after injection. Blood was obtained by left ventricular puncture and then PBS was transcardially perfused to exsanguinate the retina. The eyes were enucleated, pooled, and tissues were homogenized in iced sucrose buffer containing protease inhibitors (31). Blood was spun at 2500 × g for 10 m and plasma collected. Tissues were frozen at −80°C until assayed. Epo concentrations were determined by ELISA (R&D Systems, Minneapolis, MN).
ROP model.
Experimental ROP was induced by raising rat pups exposed to variable hyperoxia in a cycling oxygen chamber (OxyCycler, Biospherix, Redfield, NY) alternating every 24 h between hyperoxia (50% O2) and hypoxia (10% O2) for 14 d. Control animals remained in the RA. All animals received one of the three treatments daily from P1 to P3: saline (0), 5000, or 30,000 U/Kg i.p. rEpo (Epogen, Amgen Inc., Thousand Oaks, CA, USA). Control and oxygen-exposed (OE) groups were cross-fostered by exchanging dams every 48 h to minimize the impact of COE on the adult rats. The OE pups were then allowed to recover in the RA for 6 d. Mortality and litter weights were monitored throughout the experiment. Retinal vascular development was assessed at P20 (32). The ROP is consistent in 75–80% of treated animals.
Angiography with fluorescein-dextran.
Animals were perfused with a fluorescein-dextran solution (molecular weight: 1.5 × 105; Sigma Chemical Co. Aldrich, St. Louis, MO) at 0.03 mL/g body weight through the left ventricle (33). The eyes were enucleated and immersion fixed for 1 h in 10% formalin before the anterior structures were removed. The posterior eye cups were then fixed in 10% formalin for 3 h. The retinas were dissected from the retinal pigment epithelium and optic nerve, cut radially into four equal segments, and flat mounted. The retinas were photographed using an Olympus BX microscope (filter U-M643 ex: 470–90 nM em: 515 nM) with a Microfire digital camera (Optronics, Goleta, CA).
ADPase staining for retinal blood vessels.
To confirm the retinal vascular anatomy, the retinas from a subset of rats with and without exposure to rEpo were examined on P1, P4, P8, P14, and P20 using ADPase detection of endothelia (34). Enucleated eyes were fixed in 10% formalin (1 h, 4°C), anterior structures were removed, and the posterior eye cup was washed (3×, 5 min, 4°C) in 0.1 M cacodylate buffer with 5% sucrose (pH 7.2). The eyes were then fixed overnight (4°C) in 2% paraformaldehyde in 0.1 M cacodylate buffer with 5% sucrose (pH 7.2). After fixation, the retina was dissected free and washed three times in the buffer (last wash with 1% triton added). The retinas were incubated at 37°C for 45 min in ADPase with lead and magnesium in Trisma maleate (pH 7.2) with 1% triton while being continuously agitated. After incubation, the retinas were washed (3×, 5 min) in the buffer (first wash with 1% triton). The ADPase was then developed in 10% ammonium sulfide for 1 min then rinsed in distilled water. The retinas were flat mounted on glass slides with glycerol and examined with the bright field microscopy.
ROP grading.
Photomicrographs were scored by two observers blinded to the treatments. The extent of injury was determined first by dividing whole retinal flat-mount images at low magnification (20×) into imaginary “clock hour” segments (12 equal pie-shaped areas per retina). A binary score was assigned to each segment based on the absence (0) or presence (1) of vascular pathology. Retinal vascular pathology was characterized first by the presence of an avascular peripheral retina, then by the presence of vascular tufts or buds and increased vessel tortuosity. Tufting and vascular buds were characterized as abnormal only in the setting of avascularity. Scores were summed to assign an overall score for each retina (maximum = 12). Severity of disease was evaluated by quantifying the density of blood vessels. Flat-mounted retinas were divided into three concentric circles, centered on the optic disc: central (zone 1), middle (zone 2), and peripheral (zone 3). Using a standardized grid overlaid on high-magnification (40×) retinal images, the vessel density was quantified by counting the vessel crossings in 12 areas per zone. Two retinas per rat were graded, scores were averaged, and then the individual rat scores from each observer were averaged together, so that each rat contributed only one score to the final statistical analysis.
Statistical analysis.
Multivariate, univariate, or repeated-measures ANOVA, or nonparametric analysis, was performed as appropriate before post hoc comparisons were made using software (SPSS, Chicago, IL). Levene's test was used to determine whether data were homogenous. For ANOVA, F statistics with degrees of freedom (subscribed) and probability levels were reported and data were expressed as means and include SE (SEM) and number of subjects (N). Two-tailed post hoc comparisons were limited to a priori hypotheses. Post hoc tests included t test (two groups) or Dunnett's test (multiple comparisons to a single control). Chi-square test was used to compare rates. An initial (uncorrected) alpha criterion of p < 0.05 was used.
RESULTS
Pharmacokinetics.
Epo concentrations measured in the plasma and the eye extract increased in a dose-dependent manner after i.p. injection of rEpo, however, the kinetics differed considerably. Timed plasma and eye rEpo concentrations from P1 rats are compared after 500, 5000, or 30,000 U/Kg of rEpo (Fig. 1). Pharmacokinetic parameters calculated from these data are listed in Table 1. Plasma rEpo concentrations (Fig. 1A) peak by 6 h (27,457 ± 12,480 mU/mL after 30,000 U/kg i.p.) and decline slowly at all doses tested. In contrast, eye rEpo concentrations (Fig. 1B) continue to accumulate after a 30,000 U/kg dose with the peak concentration (93 ± 21 mU/mg protein) measured 24 h after injection. This pattern of prolonged penetration and accumulation of rEpo into the eye was less pronounced after 5000 U/kg rEpo (peak Epo concentration was 14 ± 7 mU/mg protein at 6 h), and absent at 500 U/kg/dose. Despite the delayed timing between plasma and eye rEpo measures, there was a very strong correlation between the total exposure [area under the curve (AUC)] for the plasma and the eye (r2 = 0.9986, p = 0.024), indicating that the accumulation in the eye was dose dependent. These data establish that high-dose rEpo penetrates the blood–eye barrier and can accumulate in the eyes of neonatal rats.
A pharmacokinetic scatter plot illustrating the mean (±SEM) Epo concentrations measured from plasma (A) and eye homogenates (B). On postnatal d 1 (P1), rats were given an i.p. injection of 500 (▪), 5000 (▴), or 30,000 (○) U/kg of rEpo and were then killed at scheduled intervals. At the lower doses, Epo peaks quickly and declines slowly with a similar profile in both the plasma and eye. After a 30,000 U/kg dose, Epo continues to accumulate in the eye, whereas it is decline in the plasma. Error bars shown at all times and doses.
Cyclic oxygen exposure.
Fluorescein and ADPase staining of retinal vessels from rats raised in RA or OE conditions confirmed that COE disrupted normal vascular development, and that these changes persist until P20. Exposure to cyclic oxygen increased the incidence of retinal neovascularization (defined by clock hour score >2) in the both fluorescein- (RA = 12% versus OE = 81%, χ2 = 8.66, p = 0.003) and ADPase-labeled (RA = 10% versus OE = 74%, χ2 = 5.178, p = 0.023) retina, and the mean values for each group are shown in Figure 2 for the fluorescein-filled (upper panel) and ADPase-stained (bottom panel) retinas from RA and COE rats. Figure 3 shows photomicrographs of the fluorescein- and ADPase-labeled retina from RA and COE rats to illustrate typical pathologic characteristics (e.g., avascular periphery, tufting, tortuosity) resulting from neonatal COE.
Histograms showing the mean (±SEM) clock hour scores denoting the extent of neovascularization in rat retinas. Newborn rats were raised in room air (□) or 14 d of cyclic oxygen exposure (▪) and treated daily from P1–P3 with the dose of rEpo indicated in the x axis. On P20, the retinas were removed and flat mounted and blood vessels were labeled using fluorescein perfusion (A) or ADPase staining (B). Significant Dunnett's test comparisons to control are indicated as *p < 0.05 with n = 6–17 per group.
Fluorescein- (top panels) and ADPase-labeled (bottom panels) blood vessels in the retinas from room air (left panels) and cyclic oxygen-exposed (right panels) rats at P20 illustrate some of the pathologic characteristics of experimental retinopathy of prematurity. The retinas on the right exhibit avascular periphery, and capillary tufting and tortuosity after neonatal cyclic oxygen exposure. All images are ×40 magnification and the scale bar is 500 μm.
COE decreased the density of blood vessels in P20 rat retina. Mean blood vessel densities for fluorescein- and ADPase-labeled images are listed by treatment group and retinal zone in Table 2. COE resulted in a significant reduction in the retinal vessel density, which was most pronounced in zone 3, when compared with RA control animals.
Effects of high-dose rEpo.
The 5000 U/kg dose of rEpo did not alter clock hours of pathology (Fig. 2, upper panel, filled bars). A modest increase in clock hour pathology was noted for the 30,000 U/kg rEpo dose, but only in the ADPase-stained retinas (Fig. 2, bottom panel, filled bars, p < 0.05). In contrast, the vessel density was unchanged by rEpo treatment at any dose even in the presence of COE (Table 2).
To determine whether rEpo treatment from P1 to P3 might have had a transient effect on early retinal vascular development that was no longer apparent at P20, we examined the retinas at P1, P4, P8, and P14 to detect possible acute effects of 5000 U/kg. Figure 4 shows the progressive vascular development in the ADPase-stained retina at these stages. There were no differences noted in the pattern of retinal vascular development between control (data shown) and rEpo-treated rats (data not shown).
ADPase-stained retinas from untreated neonatal rats illustrate the patterns of neonatal vascular development. The retinas were collected on P1 (top left), P4 (top right), P8 (bottom left), and P14 (bottom right). There were no differences in the pattern of early retinal vascular development between untreated and rEpo-treated rats (data not shown). All images are ×40 magnification and the scale bar is 500 μm.
DISCUSSION
The major findings of this report are as follows. First, high-dose rEpo administered systemically can penetrate the neonatal rat blood–eye barrier. At extremely high doses (30,000 U/kg), rEpo accumulates slowly in the eye and persists for up to 48 h after a single dose. Second, in neonatal rats, three doses of 5000 U/kg rEpo administered daily from birth produced neither acute nor delayed effects on the incidence or severity of retinal neovascularization under normoxic or COE conditions. Finally, although three doses of 30,000 U/kg of rEpo increased the extent of vascular pathology (as quantified by clock hours) in COE conditions, this effect was not evident in rats raised in RA. This suggests that rEpo alone, even at extremely high doses not recommended for neuroprotection (24), is not sufficient to increase abnormal vascularization of the developing retina. These data support the observation that in the rat model, repeated neuroprotective doses of rEpo (5000 U/Kg) given at intervals that might be appropriate for neuroprotection (23), do not exacerbate ROP. The implications of these data may be considered in more detail.
We used i.p. rEpo administration because it is as effective as i.v. administration in delivering rEpo to the intravascular space as well as to the tissues including the brain (31). Epo concentration was substantially increased in the eye tissue 24 h after rEpo injection (30,000 U/kg), at a time when it has substantially declined in the plasma. From this, we conclude that systemic rEpo can penetrate the blood–eye barrier and accumulate in the eye tissue. These data confirm the possibility that high concentrations of rEpo during the neonatal period have the potential to affect retinal vascular development.
There are two commonly used rodent models of ROP: mouse and rat (33,35,36). We chose to study rEpo in the rat model because this model uses COE from birth, whereas the mouse model does not begin oxygen exposure until P7. This is important because one suggested protocol for neuroprotection in extremely preterm infants is to begin high-dose rEpo treatment on d 1 of life (37,38). To be thorough, we used both fluorescein and ADPase staining to characterize the extent and severity of COE-induced injury. Both methods are effective for examining the retinal vasculature (39), but because fluorescein staining depends on adequate vascular perfusion, we felt it was important to validate these results by ADPase staining. Consistent with previous reports, we found that COE disrupts the retinal vascular growth in neonatal rats (40,41). We also detected an effect of rEpo treatment on one index (extent), but only after a very high dose of rEpo (30,000 U/kg × 3). There were no detectable effects of 5000 U/kg/dose × 3 on neonatal retinal vascularization under either normoxic or COE conditions. This is a commonly used neuroprotective regimen in animal models as the circulating Epo levels obtained by administering 5000 U/kg i.p. in a rat pup are roughly equivalent to those reached in extremely preterm infants given between 500 and 1000 U/kg i.v (31).
The potential contribution of rEpo to the development of ROP in preterm populations is controversial. Most data come from retrospective studies or meta-analyses of prospective studies for which ROP was not a primary outcome measure. The Cochrane review noting an increase in ROP after early rEpo use has raised concerns (19). In fact, the association of anemia with ROP (35) raises the possible interpretation that ROP is more directly related to anemia and only incidentally related to rEpo, which is used to treat anemia. It should also be noted, however, that there was great heterogeneity in the few studies evaluated and the overall relative risk ratio for any ROP in rEpo-treated infants was 1.18 compared with the stage 3 ROP risk ratio described earlier. In addition, supplemental iron was used in combination with rEpo in every case, thus the effect of rEpo alone remains unknown. Other studies have raised questions about cumulative dosing of rEpo affecting ROP rather than absolute dosing (42–44). Still others question the timing of rEpo dosing relative to the timing of vascular proliferation in the retina, which generally occurs around 32 wk corrected gestational age (35,44).
So what do we know about the pathogenesis of ROP? It is thought to occur in two phases. The first phase occurs as a result of premature birth and consequent exposure of the immature retina to a relatively hyperoxic environment. Premature exposure to oxygen results in down-regulation of HIF/HLF and subsequent reduction of downstream growth factors (VEGF, IGF-1, Epo) leading to stunted vascular development. As the developing retinal tissue becomes increasingly metabolically active, it becomes hypoxic from insufficient blood flow and oxygen delivery. Hypoxia-inducible growth factors are up-regulated, resulting in phase II ROP: abnormal blood vessel proliferation. Based on this information, four effects of systemically administered rEpo are plausible: (1) rEpo given early (in phase I) might prevent the vessel loss and, therefore, abrogate the development of phase II ROP, (2) early rEpo might exacerbate ROP by triggering uncontrolled proliferation of the retinal vessels, (3) rEpo effects may depend on the timing and developmental stage during which it is given and only rEpo given later will have an effect and worsen the second phase of ROP, or (4) rEpo given alone may have no effect on retinal vascularization.
In a mouse model of ROP, early rEpo treatment decreased the development of ROP, whereas late treatment given during the proliferative stage contributed to neovascularization and disease (35). In contrast, we found no beneficial effect of early rEpo administration on retinal vascularization in the rat model. Although these differences may be explained by differences in the species and the oxygen conditions, we are confident in our analysis as we thoroughly examined rat retinas at P1, P4, P8, and at P20 as the retinal vasculature was maturing. At no point was there indication that 5000 U/Kg rEpo was increasing retinal angiogenesis or exacerbating ROP.
Because we had equipoise as to whether rEpo might increase or decrease the severity of ROP, we used a model of moderate ROP, so we could detect either an improvement or a worsening of disease. Although we found no evidence of harm using 5000 U/kg rEpo, further investigation of rEpo under conditions of severe ROP is warranted.
We conclude that early rEpo administration of 5000 U/kg per dose does not increase the risk of ROP in the rat model. We recommend against repeated administration of higher doses such as 30,000 U/kg in those at risk for ROP given the potential for worsening disease in subjects with the immature retinas. At this point, we find no evidence supporting the contention that early, high-dose (5000 U/Kg) rEpo administration increases the risk of ROP, and we find that continued consideration of high-dose rEpo to provide neuroprotection for preterm infants is reasonable.
Abbreviations
- COE:
-
cyclic oxygen exposure
- Epo:
-
erythropoietin
- OE:
-
oxygen exposed
- P:
-
postnatal day
- RA:
-
room air
- rEpo:
-
recombinant erythropoietin
- ROP:
-
retinopathy of prematurity
References
Stockman JA III, Graeber JE, Clark DA, McClellan K, Garcia JF, Kavey RE 1984 Anemia of prematurity: determinants of the erythropoietin response. J Pediatr 105: 786–792
Juul SE, Yachnis AT, Christensen RD 1998 Tissue distribution of erythropoietin and erythropoietin receptor in the developing human fetus. Early Hum Dev 52: 235–249
Juul SE, Yachnis AT, Rojiani AM, Christensen RD 1999 Immunohistochemical localization of erythropoietin and its receptor in the developing human brain. Pediatr Dev Pathol 2: 148–158
Carlini RG, Reyes AA, Rothstein M 1995 Recombinant human erythropoietin stimulates angiogenesis in vitro. Kidney Int 47: 740–745
Kumral A, Genc S, Ozer E, Yilmaz O, Gokmen N, Koroglu TF, Duman N, Genc K, Ozkan H 2006 Erythropoietin downregulates bax and DP5 proapoptotic gene expression in neonatal hypoxic-ischemic brain injury. Biol Neonate 89: 205–210
Spandou E, Soubasi V, Papoutsopoulou S, Karkavelas G, Simeonidou C, Kaiki-Astara A, Guiba-Tziampiri O 2004 Erythropoietin prevents hypoxia/ischemia-induced DNA fragmentation in an experimental model of perinatal asphyxia. Neurosci Lett 366: 24–28
Sakanaka M, Wen TC, Matsuda S, Masuda S, Morishita E, Nagao M, Sasaki R 1998 In vivo evidence that erythropoietin protects neurons from ischemic damage. Proc Natl Acad Sci USA 95: 4635–4640
Bryl E, Mysliwska J, Debska-Slizien A, Rachon D, Bullo B, Lizakowski S, Mysliwski A, Rutkowski B 1998 The influence of recombinant human erythropoietin on tumor necrosis factor alpha and interleukin-10 production by whole blood cell cultures in hemodialysis patients. Artif Organs 22: 177–181
Chattopadhyay A, Choudhury TD, Bandyopadhyay D, Datta AG 2000 Protective effect of erythropoietin on the oxidative damage of erythrocyte membrane by hydroxyl radical. Biochem Pharmacol 59: 419–425
Bany-Mohammed FM, Slivka S, Hallman M 1996 Recombinant human erythropoietin: possible role as an antioxidant in premature rabbits. Pediatr Res 40: 381–387
Sun Y, Calvert JW, Zhang JH 2005 Neonatal hypoxia/ischemia is associated with decreased inflammatory mediators after erythropoietin administration. Stroke 36: 1672–1678
Keller M, Yang J, Griesmaier E, Gorna A, Sarkozy G, Urbanek M, Gressens P, Simbruner G 2006 Erythropoietin is neuroprotective against NMDA-receptor-mediated excitotoxic brain injury in newborn mice. Neurobiol Dis 24: 357–366
Kawakami M, Iwasaki S, Sato K, Takahashi M 2000 Erythropoietin inhibits calcium-induced neurotransmitter release from clonal neuronal cells. Biochem Biophys Res Commun 279: 293–297
Villa P, Bigini P, Mennini T, Agnello D, Laragione T, Cagnotto A, Viviani B, Marinovich M, Cerami A, Coleman TR, Brines M, Ghezzi P 2003 Erythropoietin selectively attenuates cytokine production and inflammation in cerebral ischemia by targeting neuronal apoptosis. J Exp Med 198: 971–975
Sugawa M, Sakurai Y, Ishikawa-Ieda Y, Suzuki H, Asou H 2002 Effects of erythropoietin on glial cell development; oligodendrocyte maturation and astrocyte proliferation. Neurosci Res 44: 391–403
Genc K, Genc S, Baskin H, Semin I 2006 Erythropoietin decreases cytotoxicity and nitric oxide formation induced by inflammatory stimuli in rat oligodendrocytes. Physiol Res 55: 33–38
Vitellaro-Zuccarello L, Mazzetti S, Madaschi L, Bosisio P, Gorio A, De Biasi S 2007 Erythropoietin-mediated preservation of the white matter in rat spinal cord injury. Neuroscience 144: 865–877
Vohr BR, Wright LL, Dusick AM, Mele L, Verter J, Steichen JJ, Simon NP, Wilson DC, Broyles S, Bauer CR, Delaney-Black V, Yolton KA, Fleisher BE, Papile LA, Kaplan MD 2000 Neurodevelopmental and functional outcomes of extremely low birth weight infants in the National Institute of Child Health and Human Development Neonatal Research Network, 1993–1994. Pediatrics 105: 1216–1226
Ohlsson A, Aher SM 2006 Early erythropoietin for preventing red blood cell transfusion in preterm and/or low birth weight infants. Cochrane Database Syst Rev 3: CD004863
Aher SM, Ohlsson A 2006 Early versus late erythropoietin for preventing red blood cell transfusion in preterm and/or low birth weight infants. Cochrane Database Syst Rev 3: CD004865
Garcia MG, Hutson AD, Christensen RD 2002 Effect of recombinant erythropoietin on “late” transfusions in the neonatal intensive care unit: a meta-analysis. J Perinatol 22: 108–111
Kotto-Kome AC, Garcia MG, Calhoun DA, Christensen RD 2004 Effect of beginning recombinant erythropoietin treatment within the first week of life, among very-low-birth-weight neonates, on “early” and “late” erythrocyte transfusions: a meta-analysis. J Perinatol 24: 24–29
Kellert BA, McPherson RJ, Juul SE 2007 A comparison of high-dose recombinant erythropoietin treatment regimens in brain-injured neonatal rats. Pediatr Res 61: 451–455
Tasman W, Patz A, McNamara JA, Kaiser RS, Trese MT, Smith BT 2006 Retinopathy of prematurity: the life of a lifetime disease. Am J Ophthalmol 141: 167–174
Palmer EA, Flynn JT, Hardy RJ, Phelps DL, Phillips CL, Schaffer DB, Tung B 1991 Incidence and early course of retinopathy of prematurity. The Cryotherapy for Retinopathy of Prematurity Cooperative Group. Ophthalmology 98: 1628–1640
Ashton N 1980 Oxygen and the retinal blood vessels. Trans Ophthalmol Soc U K 100: 359–362
Heeschen C, Aicher A, Lehmann R, Fichtlscherer S, Vasa M, Urbich C, Mildner-Rihm C, Martin H, Zeiher AM, Dimmeler S 2003 Erythropoietin is a potent physiologic stimulus for endothelial progenitor cell mobilization. Blood 102: 1340–1346
Watanabe D, Suzuma K, Matsui S, Kurimoto M, Kiryu J, Kita M, Suzuma I, Ohashi H, Ojima T, Murakami T, Kobayashi T, Masuda S, Nagao M, Yoshimura N, Takagi H 2005 Erythropoietin as a retinal angiogenic factor in proliferative diabetic retinopathy. N Engl J Med 353: 782–792
Morita M, Ohneda O, Yamashita T, Takahashi S, Suzuki N, Nakajima O, Kawauchi S, Ema M, Shibahara S, Udono T, Tomita K, Tamai M, Sogawa K, Yamamoto M, Fujii-Kuriyama Y 2003 HLF/HIF-2alpha is a key factor in retinopathy of prematurity in association with erythropoietin. EMBO J 22: 1134–1146
McPherson RJ, Juul SE 2008 Recent trends in erythropoietin-mediated neuroprotection. Int J Dev Neurosci 26: 103–111
Statler PA, McPherson RJ, Bauer LA, Kellert BA, Juul SE 2007 Pharmacokinetics of high-dose recombinant erythropoietin in plasma and brain of neonatal rats. Pediatr Res 61: 671–675
Madan A, Penn JS 2003 Animal models of oxygen-induced retinopathy. Front Biosci 8: d1030–d1043
Smith LE, Wesolowski E, McLellan A, Kostyk SK, D'Amato R, Sullivan R, D'Amore PA 1994 Oxygen-induced retinopathy in the mouse. Invest Ophthalmol Vis Sci 35: 101–111
Lutty GA, McLeod DS 2005 Phosphatase enzyme histochemistry for studying vascular hierarchy, pathology, and endothelial cell dysfunction in retina and choroid. Vision Res 45: 3504–3511
Chen J, Connor KM, Aderman CM, Smith LE 2008 Erythropoietin deficiency decreases vascular stability in mice. J Clin Invest 118: 526–533
Penn JS, Thum LA 1988 Oxygen-induced retinopathy in the rat. Basic Life Sci 49: 1025–1028
Fauchere JC, Dame C, Vonthein R, Koller B, Arri S, Wolf M, Bucher HU 2008 An approach to using recombinant erythropoietin for neuroprotection in very preterm infants. Pediatrics 122: 375–382
Juul SE, McPherson RJ, Bauer LA, Ledbetter KJ, Gleason CA, Mayock DE 2008 A phase I/II trial of high-dose erythropoietin in extremely low birth weight infants: pharmacokinetics and safety. Pediatrics 122: 383–391
Penn JS, Henry MM 1996 Assessing retinal neovascularization in an animal model of proliferative retinopathy. Microvasc Res 51: 126–130
Penn JS, Thum LA 1989 The rat as an animal model for retinopathy of prematurity. Prog Clin Biol Res 314: 623–642
Penn JS, Tolman BL, Lowery LA 1993 Variable oxygen exposure causes preretinal neovascularization in the newborn rat. Invest Ophthalmol Vis Sci 34: 576–585
Brown MS, Baron AE, France EK, Hamman RF 2006 Association between higher cumulative doses of recombinant erythropoietin and risk for retinopathy of prematurity. J AAPOS 10: 143–149
Romagnoli C, Zecca E, Gallini F, Girlando P, Zuppa AA 2000 Do recombinant human erythropoietin and iron supplementation increase the risk of retinopathy of prematurity?. Eur J Pediatr 159: 627–628
Suk KK, Dunbar JA, Liu A, Daher NS, Leng CK, Leng JK, Lim P, Weller S, Fayard E 2008 Human recombinant erythropoietin and the incidence of retinopathy of prematurity: a multiple regression model. J AAPOS 12: 233–238
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was supported by the Neonatal Biology Research Fund.
Rights and permissions
About this article
Cite this article
Slusarski, J., McPherson, R., Wallace, G. et al. High-Dose Erythropoietin Does Not Exacerbate Retinopathy of Prematurity in Rats. Pediatr Res 66, 625–630 (2009). https://doi.org/10.1203/PDR.0b013e3181bc33e6
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e3181bc33e6