Abstract
The effect of inflation length on lung aeration pattern, tidal volumes, and functional residual capacity (FRC) immediately after birth was investigated. Preterm rabbits (28 d), randomized into four groups, received a 1-, 5-, 10-, or 20-s inflation (SI) followed by ventilation with 5 cm H2O end-expiratory pressure. Gas volumes were measured by plethysmography and uniformity of lung aeration by phase contrast x-ray imaging for 7 min. The first inspiratory volume significantly (p < 0.001) increased with inflation duration from a median (IQR) of 0.2 (0.1–3.1) mL/kg for 1-s inflation to 23.4 (19.3–30.4) mL/kg for 20-s SI. The lung was uniformly aerated, and the FRC and tidal volume fully recruited after 20-s SI. A 10-s SI caused a higher FRC (p < 0.05) at 7 min, and a 20-s SI caused a higher FRC (p < 0.05) at 20 s and 7 min than a 1- or 5-s SI. The mean (SD) time for 90% of the lung to aerate was 14.0 (4.1) s using 35 cm H2O peak inflation pressure. In these rabbits, 10- and 20-s SI increased the inspiratory volume and produced a greater FRC, and a 20-s SI uniformly aerated the lung before ventilation started.
Similar content being viewed by others
Main
Many preterm infants need positive pressure ventilation (PPV) during the transition to air breathing at birth to assist lung aeration and the initiation of pulmonary gas exchange. It is possible that an initial sustained inflation (SI) might overcome the long time constant of a liquid-filled lung and facilitate early gas exchange to reduce the need for intubation (1,2). However, this procedure is not commonly used because of the risk of overinflating and damaging the lung during the initial inflation (3). Despite this, the international guidelines on neonatal resuscitation state that an initial SI may be beneficial during stabilization at birth (4). However, a recommended duration for the SI was not provided (4) because of a lack of evidence, as few studies have investigated the use of SIs during ventilation at birth. Although a few physiologic and clinical studies have examined the effect of different durations of inflation (1,2,5–9), there is currently no consistent view whether it is beneficial or what duration is most appropriate.
We have recently used phase contrast x-ray imaging to determine the rate and spatial pattern of lung aeration at birth in spontaneously breathing (10) and mechanically ventilated preterm rabbit pups (11). Using this technique, the entry of air into the lung and its spatial distribution can be imaged and measured breath-by-breath (12).
In this study, we have investigated the effect of SIs of different durations on the recruitment of functional residual capacity (FRC), lung aeration patterns, and tidal volumes (Vt) from birth. We hypothesized that increasing the duration of the first inflation would increase the recruitment of FRC and tidal volume from the first breath after birth because of the longer time constant for the air/liquid interface to move into the distal airways.
METHODS
Animal experiments.
All animal procedures were approved by the SPring-8 Animal Care and Monash University's School of Biomedical Science's Animal Ethics Committees. Studies were conducted in experimental hutch 3 of beam line 20B2, in the Biomedical Imaging Centre at the SPring-8 synchrotron in Japan.
Experiments were performed on six litters of New Zealand White rabbits using 35 pups delivered at 28 d gestation (term 32 d; 28 d correlates approximately with human infants of 26–28 wk of gestation). The does were anesthetized (Propofol; 12 mg/kg bolus, 100 mg · kg−1 · h−1 i.v. infusion, then isofluorane 1 to 2%), intubated, and ventilated. The pups were sequentially delivered by hysterotomy, leaving the fetal membranes over the nose and mouth to prevent air entering the lungs. The pups were sedated (Nembutal 0.1 mg i.p.), a topical anesthetic (5% xylocaine) was applied, and an endotracheal tube (18-gauge plastic catheter) inserted via tracheostomy; the endotracheal tube was blocked to prevent air from entering the lung before imaging commenced. The fetal membranes were then removed, the umbilical cord ligated and cut, and the pup was placed in a water-filled plethysmograph (see later). The pups were then ventilated for 7 min while they were simultaneously imaged. After the experiment, pups were killed by anesthetic overdose.
Plethysmography.
Lung gas volume changes were measured using water-based plethysmography (11). The pup was placed in the plethysmograph (head out), which consisted of a sealed water-filled (warmed to 37°C) perspex chamber open to the atmosphere via a water column. The pup's head was located outside the chamber and a rubber diaphragm formed a watertight seal around the pup's neck. The increase in lung volume caused by lung aeration displaced water from the chamber into the water column and the resulting increase in pressure was recorded electronically using a computerized data acquisition system (Powerlab, ADInstruments Sydney, Australia). The plethysmograph was calibrated before each experiment by measuring the pressure change caused by injecting a known volume of water (1 mL) into the sealed chamber. We recorded FRC, initial volume, tidal volume, minute volume, inspiratory and expiratory times, airway pressure, ventilator rate, and gas flow.
Mechanical ventilation.
A purpose-built small animal ventilator was used to ventilate pups with air in a time cycled, pressure-limited mode (PPV). Ventilation commenced with a peak inflation pressure (PIP) of 35 cm H2O and an inspiration time of 1, 5, 10, or 20 s, depending on the group (see later). A PIP of 35 cm H2O was chosen based on earlier observations in ventilated preterm rabbit pups (13,14) and is similar to the inspiratory pressures (35 H2O) generated by spontaneous breathing preterm pups during the first breaths (15). After the first inflation, pups were ventilated with a fixed inspiration and expiration time (rate 24/min, 1:1.5 inspiration: expiration ratio), starting with a PIP of 35 cm H2O, which was then adjusted (increased or decreased by 2 cm H2O per minute) to generate a tidal volume of ∼10 mL/kg, end-expiratory pressure (PEEP) was set at 5 cm H2O.
Protocol.
The pups were randomly allocated to one of the four ventilation groups:
-
Group 1: PPV from the start (No SI).
-
Group 2: Inflation for 5 s followed by PPV (5 SI).
-
Group 3: Inflation for 10 s followed by PPV (10 SI).
-
Group 4: Inflation for 20 s followed by PPV (20 SI).
Phase contrast x-ray imaging.
Phase contrast x-ray imaging was used to demonstrate the effect of SI duration on the rate and spatial pattern of lung aeration. Details describing the imaging and analytical procedures have been reported previously (10,16,17). The x-ray energy used was 24 keV, the detector (Hamamatsu, C4742-95HR) was located 2.0 m down stream of the pups, and a short exposure time (50 ms) and a relatively long inspiration time (1 s) were used to minimize motion blur. Image acquisition was triggered by the ventilator at the onset of inspiration, which triggered a sequence of images at 300-ms intervals. A shutter, located upstream from the rabbit pup, prevented radiation exposure between image acquisitions, and the timing of each image acquisition was recorded digitally in unison with the plethysmograph recording.
During the 20-s SI, the rate of increase in air volume within different regions of the lung was measured by dividing the images into quadrants and measuring the air volume in each quadrant (at end expiration or during the SI) using a phase retrieval analysis (11). This analysis has recently been validated (11) and uses extrathoracic landmarks to track pup movement between consecutive images to ensure that the relative amount of lung in each quadrant does not change over time. As the amount of lung (thus potential air volume) varies between the quadrants, the air volume of each quadrant at each time point was expressed as a percentage of the maximum volume achieved in that quadrant after complete lung aeration.
The images were not magnified during acquisition but have been cropped and enlarged for presentation. Actual image size is 19 mm (wide) by 21 mm high.
Analysis.
The first inflation volume was calculated by measuring the gas volume at the end of the first inflation. FRC was defined as the volume of air remaining in the lung at end expiration, and Vt recruitment refers to the gradual increase in Vt for a given pressure gradient.
FRC was calculated at 20 s, 1, 3, and 7 min by determining the average FRC after four consecutive inflations at these times. FRC was assumed to be zero at the start of ventilation. To compare the first inflation volume and FRC between the groups, a one-way ANOVA followed by a Tukey HSD post hoc test was used. Significance was defined as p < 0.05, and data were analyzed using SPSS software (SPSS for windows, version 15.0, 2006, Chicago, IL).
RESULTS
Twenty-six of 31 pups were delivered alive and studied. Two pups were excluded because of equipment malfunction. None of the pups developed a pneumothorax, which was verified using imaging. The average pup weight (SD) in each group was as follows: group 1 (no SI), 34.4 g (2.4); group 2 (5-s SI), 40.1 g (5.4); group 3 (10-s SI), 36.2 g (2.1); and group 4 (20-s SI), 37.9 g (2.3). Each group contained six pups.
First inflation volume.
Compared with the volume achieved with a normal 1-s inflation (no SI) [median (IQR)], a SI of 10 and 20 s, but not 5 s, significantly increased the average volume of the first inflation (Table 1; Figs. 1 and 2). Furthermore, the volume achieved by a 20-s SI was significantly greater than that achieved by a 10-s SI (p < 0.05) and did not result in either total lung or regional overinflation (Figs. 1,2,and 4E–H). Indeed, the gas volume achieved by a 20-s SI [23.4 (19.3–30.4) mL/kg] was similar to the end-inflation gas volume measured during the subsequent ventilation period (Fig. 1), when the pups had recruited a FRC of ∼13 mL/kg and were ventilated to reach a Vt of ∼10 mL/kg (Fig. 1). Furthermore, during the 20-s SI, although the upper (rostral) regions of the lungs aerated faster than the lower (caudal) regions, resulting in significantly greater volumes between 6 and 13 s of the SI (Fig. 3), relative air volumes were similar in all regions by 20 s. This indicates that, during a SI, the increase in air volumes in the aerated regions is eventually slow, allowing the other regions to “catch up” (Fig. 3).
Plethysmograph recordings of lung gas volumes from newborn rabbit pups delivered preterm and ventilated from birth. The four recordings show the following: (A) The first inflation was not sustained (no SI; i.e. 1 s in duration); (B) first inflation held for 5 s; (C) first inflation held for 10 s; and (D) first inflation held for 20 s. Pups were then ventilated initially with a PEEP of 5 cm H2O and PIP of 35 cm H2O, which was later changed to achieve a tidal volume of ∼10 mL/kg.
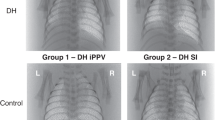
Phase contrast x-ray images from prematurely delivery newborn rabbit pups ventilated from birth. Top panel are the images from the group with no SI (1 s in duration; images A, B, C, and D). Bottom panel are the images from the group with SI of 20 s (images E, F, G, and H). Images were acquired at 1 (A and E), 5 (B and F), 10 (C and G), and 20 (D and H) s after birth. The double asterisks (**) indicate images acquired at the end of the first inflation. Images acquired after the first inflation were acquired at end inspiration.
The increase in air volume during the 20-s SI by dividing the phase contrast x-ray images into quadrants: red circle, lower left (left caudal region); blue circle, lower right (right caudal region); purple triangle, upper left (left rostral region); and blue triangle, upper right (right rostral region). The relative air volume was significantly greater in both upper (rostral) (purple and blue triangle), compared with both lower (caudal) (red and blue circle), regions as indicated by the asterisks.
The phase contrast x-ray images and movie sequences (Figs. 4 and 5) clearly demonstrate that the spatial pattern of lung aeration is not uniform and that a finite period (∼15 s; Fig. 3) is required before the lung is uniformly aerated. As determined from the image sequences, a 20-s SI completely aerated the lungs in five of six pups, before the onset of PPV (Figs. 1 and 4E–H). However, a 10-s SI completely aerated the lungs in only one of six pups, whereas no pups had completely aerated their lungs after a 5-s SI (Figs. 1 and 5A–D).
Phase contrast x-ray images from preterm rabbit pups ventilated from birth. Top panel are the images from the group with a 5-s SI (images A, B, C, and D). Bottom panel are the images from the group with a 10-s SI (images E, F, G, and H). Images were acquired at 1 (A and E), 5 (B and F), 10 (C and G), and 20 (D and H) s after birth. The double asterisks (**) indicate images acquired at the end of the first inflation. Images acquired after the first inflation were acquired at end inspiration.
Assuming the pressure gradient (35 cm H2O) remained constant throughout the SI, the mean maximum lung inflation rate and minimum resistance for moving the air/liquid interface into the distal airways were calculated. During the 20-s SI, the mean lung inflation rate was 3.5 (3.5) mL · kg−1 · s−1 (range, 1.6 to 9.6 mL · kg−1 · s−1), whereas after aeration was complete, lung inflation rates during PPV were >20-fold higher (81.7 (32.1) mL · kg−1 · s−1), despite a lower mean pressure gradient (26 (4.2) cm H2O). The resistance to lung inflation was 25.3 (29.6) cm H2O/(mL · kg−1 · s−1) during the 20-s SI, whereas during PPV in the same pups, the resistance was nearly a 100-fold lower [0.38 (0.08) cm H2O/(mL · kg−1 · s−1)]. The mean time taken to reach 90% (21.5 (5.5) mL/kg) of the 20-s SI volume was 14.0 (4.1) s and also varied considerably between pups (8.6 s to >20 s).
FRC.
The median (IQR) FRC of each group at each time point is shown in Table 1. Compared with a 1-s inflation (No SI), a 5-s SI did not result in a significantly higher FRC at any of the time points measured. However, a 10-s SI resulted in a significantly higher FRC at 7 min after birth, and a 20-s SI resulted in a significantly higher FRC at 20 s and 7 min after birth.
Tidal volume.
After a 20-s SI, the tidal volume (Vt) did not increase after the first inflation (Figs. 1 and 6). As a result, during the first seven inflations, the mean (SD) expired tidal volumes in the 20-s SI group (14.1 (5.1) mL/kg) were significantly greater than the first seven inflations in all other groups (No SI, 2.0 (1.8) mL/kg, p < 0.05; 5 SI, 4.9 (3.8) mL/kg, p < 0.001; 10 SI, 6.6 (2.3) mL/kg, p < 0.05). Pups receiving a 10-s SI gradually recruited Vt during the first 10 breaths. They had significantly (p < 0.05) larger Vt than pups receiving a 5-s SI or no SI (Figs. 1 and 6). Pups not receiving a SI had the slowest tidal volume recruitment.
DISCUSSION
This study has shown that an initial SI of 20 s significantly increased the volume of air entering the lung during the first inflation in preterm rabbit pups ventilated from birth using PPV. The phase contrast x-ray images demonstrated that, although the spatial pattern of lung aeration is not uniform during the first SI, by the end of 20 s, the lung had completely and uniformly aerated before the onset of PPV. Our data also demonstrated that lung aeration requires a finite time, occurring at a maximum rate of 3.5 (3.5) mL · kg−1 · s−1 and results in 90% lung aeration within 14.0 (4.1) s using an inflating pressure of 35 cm H2O. Furthermore, increasing the duration of the SI from 5 to 10 to 20 s significantly increased the FRC at 20 s and both a 10- and 20-s SI resulted in a small, but significant increase in FRC at 7 min compared with no SI. The phase contrast images show that a 20-s SI progressively aerated the entire lung without causing visible overexpansion of regions that rapidly aerated (upper lobes), whereas slower regions continued to aerate (lower lobes). Overexpanded, regions of the lung bulge out between the ribs and can be clearly seen in the phase contrast images (unpublished observations). However, in Fig. 4H (acquired at the end of a 20-s SI), gaps between the ribs and the edge of the lung are clearly visible.
In contrast to a 10- and 20-s SI, almost no gas entered the lung during a 1-s inflation in pups not receiving a SI (Figs. 1,2,and 4). Furthermore, although the application of PEEP facilitated the rapid accumulation of an FRC, during a 1-s inflation, tidal expansion of the lung was restricted to aerated regions (Fig. 4). In contrast, tidal expansion of the lung after a 20-s SI occurred evenly throughout the lung and was comparable with the volume observed after the first breath of spontaneously breathing term rabbit pups (15).
The inspiratory volume measured during the first breath in healthy term infants were in a similar range to that observed after a 10-s SI (2,18–20). Vyas et al. (18) found a strong positive correlation between the first inspiratory volume and the FRC reached after the first breath, which is consistent with the findings of this study (Figs. 1,2,4,and 5). The same inspiratory volume was achieved in asphyxiated infants when an initial inflation of 5 s was given (2), but not with standard ventilation (21). In our study, because the lung was fully recruited after the 20-s SI, the pressures used for subsequent inflations were initially too large, resulting in a Vt of ∼12 mL/kg. Despite reducing the PIP to 26 (4.2) cm H2O, the Vt remained high, indicating that lung compliance was continuing to increase throughout this period (Fig. 6). It is possible that a SI with a smaller starting pressure could be used to initiate lung aeration; however, it is likely that the duration of the SI will need to be significantly longer to achieve uniform lung aeration.
The FRC measured after the 10- or 20-s initial SI were in the same range as the FRC measured in spontaneously breathing term rabbit pups (10–20 mL/kg) during the same time period (15). This could explain why, in clinical studies, a 10- to 20-SI is more successful in improving gas exchange than a 5-s SI (5,7–9).
Very preterm infants commonly have problems clearing their airways of liquid at birth. When respiratory support is needed, our results indicate that an initial SI would allow more air to enter the lung before the start of PPV (2,9). During the 20-s SI, the resistance for moving the air/liquid interface from the proximal into the distal airways during the first inflation was ∼100-fold higher than during PPV, and that several seconds were required to overcome this resistance and achieve an adequate lung volume for a given inflating pressure. Given the large viscosity difference between air and liquid, it is not surprising that resistance to the first inflation is so much greater than similar inflations after lung aeration.
The high resistance and low flow rates during the first inflation clearly indicate that inflation times of a second or less are likely to be insufficient to achieve an adequate lung gas volume in an apnoeic animal. This is evident in the phase contrast x-ray images, which demonstrated that after a 1-s inflation, no air entered the distal gas exchange regions of the lung (Figs. 2 and 4). Some regions were aerated by a 5-s SI, and the numbers of regions were increased further by a 10-s SI, whereas the lung was fully aerated after a 20-s SI. These observations are supported by the finding that the mean time taken to aerate 90% of the lung during a SI with an inflating pressure of 35 cm H2O was 14.0 (4.1) s. However, this time varied considerably between individuals and will be determined by the initial pressure gradient. As the pressure gradient increases, the time constant for complete lung aeration will obviously decrease, but the possibility of overexpansion in lung regions aerating first is likely to be high. Thus, lower pressures and a longer first inflation time would appear preferable.
Although a SI of 20 s increased the FRC created at the onset of tidal ventilation, the beneficial effect of a SI on FRC rapidly decreased with increasing ventilation time. As lung gas volume can be lost very quickly in these immature pups in the absence of PEEP, it is not surprising that using PEEP during PPV is more important for maintaining FRC than an initial SI. As all groups were ventilated with PEEP, this explains why the difference in FRC observed between the groups when measured after 7 min of ventilation was small. In the absence of PEEP, we have demonstrated only a very small FRC was achieved with a 20-s SI, indicating that an initial SI should always be combined with the application of PEEP (9).
The FRC varied markedly between the individuals, which limited our ability to detect differences between the groups. This large variability most likely results from differences in lung maturity between the pups. However, it is interesting that the variation in FRC was markedly less at 1 min (Table 1) in pups receiving a 20-s SI than in all other groups. It is possible that a 20-s SI at 35 cm H2O was enough to overcome all the different factors that contribute to the time constant for lung aeration, leading to less variation in FRC. This suggestion is consistent with the finding that the time taken to achieve 90% lung aeration varies considerably (8.6 to >20 s), but with most (five of six) pups fully aerating their lungs within 20 s.
We used ventilated preterm rabbit pups to demonstrate the principles of how initial inflations of different durations affect FRC, tidal volumes, and the uniformity of lung aeration. Although very preterm infants resuscitated under different circumstances (e.g. in a horizontal position) may have partially aerated lungs before ventilation starts because of spontaneous breathing, we believe that the principles displayed in this study are likely to apply to preterm infants. Indeed, the high viscosity of liquid, compared with air, will always increase the resistance to lung inflation in liquid-filled versus air-filled airways, no matter what the species. Thus, an inflation of sufficient duration will overcome the different time constants, caused for example by different sized airways, allowing more uniform aeration before PPV begins. On the other hand, if the lung is only partially aerated, during PPV air will preferentially enter and inflate aerated regions because air-filled airways have a much (100-fold) lower resistance than liquid-filled airways. In liquid-filled regions, the air/liquid interface will move distally only after the pressure in the aerated regions exceeds the pressure gradient required to overcome the resistance to liquid movement. If the inflation time is short (<1 s), the airway pressure will only exceed the required pressure briefly during inspiration, thereby greatly increasing the time and number of inflations required to fully aerate and recruit the lung. This contention is supported by the finding that for a given inflating pressure, tidal volumes recruit more slowly in the absence of a SI and that increasing the duration of the SI increases the rate of lung recruitment (Fig. 6).
To translate these results to clinical practice, we suggest that respiratory function monitoring is used during ventilation at birth to measure the gas volumes entering the lung. One could observe the first inspiratory volume during a SI and once a certain volume (FRC + tidal volume) is reached, the SI should then be stopped and tidal ventilation started.
A SI resulted in more uniform lung aeration, better recruitment of FRC, and more consistent tidal volumes from the start of tidal ventilation. We found no evidence that a SI caused overdistension of the lung and believe that a SI may reduce VILI at birth by minimizing shear stress caused by rapid expansion and deflation of the lung before it is uniformly aerated. Studies evaluating lung injury caused by a SI are needed, although a SI of 10 s has been used in a randomized controlled trial and was associated with less BPD (9).
In conclusion, during PPV with PEEP after birth, increasing the duration of the initial inflation to 10 or 20 s increased the gas volume entering the lung, allowing ventilation of the distal gas exchange regions from the first inflation. The results demonstrate that uniform lung aeration requires a finite period of time because of the long time constant caused by the high resistance for the air/liquid interface to move through the airways. As a result, in ventilated preterm rabbit pups, using a peak inflation pressure of 35 cm H2O, a mean initial SI of 14.0 (4.1) s is required to mostly (90%) aerate the lungs. Although we measured a larger FRC at 7 min with a SI of 10 to 20 s, the effect of a SI on FRC rapidly decreases with increasing ventilation time, indicating that the application of PEEP is also important.
Abbreviations
- FRC:
-
functional residual capacity
- PEEP:
-
positive end-expiratory pressure
- PPV:
-
positive pressure ventilation
- PIP:
-
peak inflation pressure
- SI:
-
sustained inflation
- Vt:
-
tidal volume
References
Hird MF, Greenough A, Gamsu HR 1991 Inflating pressures for effective resuscitation of preterm infants. Early Hum Dev 26: 69–72
Vyas H, Milner AD, Hopkin IE, Boon AW 1981 Physiologic responses to prolonged and slow-rise inflation in the resuscitation of the asphyxiated newborn infant. J Pediatr 99: 635–639
Bjorklund LJ, Ingimarsson J, Curstedt T, John J, Robertson B, Werner O, Vilstrup CT 1997 Manual ventilation with a few large breaths at birth compromises the therapeutic effect of subsequent surfactant replacement in immature lambs. Pediatr Res 42: 348–355
The International Liaison Committee on Resuscitation 2006 The International Liaison Committee on Resuscitation (ILCOR) consensus on science with treatment recommendations for pediatric and neonatal patients: neonatal resuscitation. Pediatrics 117: e978–e988
Harling AE, Beresford MW, Vince GS, Bates M, Yoxall CW 2005 Does sustained lung inflation at resuscitation reduce lung injury in the preterm infant?. Arch Dis Child Fetal Neonatal Ed 90: F406–F410
Klopping-Ketelaars WA, Maertzdorf WJ, Blanco CE 1994 Effect of sustained inflations applied directly after cord clamping on lung function in premature newborn lambs. Acta Paediatr 83: 1017–1021
Lindner W, Hogel J, Pohlandt F 2005 Sustained pressure-controlled inflation or intermittent mandatory ventilation in preterm infants in the delivery room? A randomized, controlled trial on initial respiratory support via nasopharyngeal tube. Acta Paediatr 94: 303–309
Lindner W, Vossbeck S, Hummler H, Pohlandt F 1999 Delivery room management of extremely low birth weight infants: spontaneous breathing or intubation?. Pediatrics 103: 961–967
te Pas AB, Walther FJ 2007 A randomized, controlled trial of delivery-room respiratory management in very preterm infants. Pediatrics 120: 322–329
Hooper SB, Kitchen MJ, Wallace MJ, Yagi N, Uesugi K, Morgan MJ, Hall C, Siu KK, Williams IM, Siew M, Irvine SC, Pavlov K, Lewis RA 2007 Imaging lung aeration and lung liquid clearance at birth. FASEB J 21: 3329–3337
Kitchen MJ, Lewis RA, Morgan MJ, Wallace MJ, Siew ML, Siu KK, Habib A, Fouras A, Yagi N, Uesugi K, Hooper SB 2008 Dynamic measures of regional lung air volume using phase contrast x-ray imaging. Phys Med Biol 53: 6065–6077
Kitchen MJ, Pavlov KM, Hooper SB, Vine DJ, Siu KK, Wallace MJ, Siew ML, Yagi N, Uesugi K, Lewis RA 2008 Simultaneous acquisition of dual analyser-based phase contrast X-ray images for small animal imaging. Eur J Radiol 68: S49–S53
Morley C, Robertson B, Lachmann B, Nilsson R, Bangham A, Grossmann G, Miller N 1980 Artificial surfactant and natural surfactant. Comparative study of the effects on premature rabbit lungs. Arch Dis Child 55: 758–765
te Pas AB, Siew M, Wallace MJ, Kitchen M, Fouras A, Lewis RA, Yagi N, Uesugi K, Donath S, Davis PG, Morley CJ, Hooper SB 2009 Establishing functional residual capacity at birth: the effect of sustained inflation and positive end expiratory pressure in a preterm rabbit model. Pediatr Res. January 28, 2009. [Epub ahead of print]
Lachmann B, Grossmann G, Nilsson R, Robertson B 1979 Lung mechanics during spontaneous ventilation in premature and fullterm rabbit neonates. Respir Physiol 38: 283–302
Lewis RA, Yagi N, Kitchen MJ, Morgan MJ, Paganin D, Siu KK, Pavlov K, Williams I, Uesugi K, Wallace MJ, Hall CJ, Whitley J, Hooper SB 2005 Dynamic imaging of the lungs using x-ray phase contrast. Phys Med Biol 50: 5031–5040
Kitchen MJ, Paganin D, Lewis RA, Yagi N, Uesugi K, Mudie ST 2004 On the origin of speckle in x-ray phase contrast images of lung tissue. Phys Med Biol 49: 4335–4348
Vyas H, Field D, Milner AD, Hopkin IE 1986 Determinants of the first inspiratory volume and functional residual capacity at birth. Pediatr Pulmonol 2: 189–193
Vyas H, Milner AD, Hopkins IE 1981 Intrathoracic pressure and volume changes during the spontaneous onset of respiration in babies born by cesarean section and by vaginal delivery. J Pediatr 99: 787–791
Saunders RA, Milner AD 1978 Pulmonary pressure/volume relationships during the last phase of delivery and the first postnatal breaths in human subjects. J Pediatr 93: 667–673
Boon AW, Milner AD, Hopkin IE 1979 Lung expansion, tidal exchange, and formation of the functional residual capacity during resuscitation of asphyxiated neonates. J Pediatr 95: 1031–1036.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by grants from the Australian Research Council, the Australian National Health and Medical Research Council, and by a financial support from the Access to Major Research Facilities Programme, which is a component of the International Science Linkages Programme established under the Australian Government's innovation statement, Backing Australia's Ability. Arjan B. te Pas is recipient of a Ter Meulen Fund grant for working visits, Royal Netherlands Academy of Arts and Sciences, The Netherlands and recipient of a Royal Women's Hospital postgraduate scholarship. Marcus J. Kitchen is a recipient of an ARC Post-Doctoral Fellowship.
Rights and permissions
About this article
Cite this article
te Pas, A., Siew, M., Wallace, M. et al. Effect of Sustained Inflation Length on Establishing Functional Residual Capacity at Birth in Ventilated Premature Rabbits. Pediatr Res 66, 295–300 (2009). https://doi.org/10.1203/PDR.0b013e3181b1bca4
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e3181b1bca4
This article is cited by
-
Respiratory strategy at birth initiates distinct lung injury phenotypes in the preterm lamb lung
Respiratory Research (2022)
-
Lung recruitment improves the efficacy of intubation-surfactant-extubation treatment for respiratory distress syndrome in preterm neonates, a randomized controlled trial
BMC Pediatrics (2022)
-
Higher CPAP levels improve functional residual capacity at birth in preterm rabbits
Pediatric Research (2022)
-
Recent Update on Neonatal Resuscitation
Indian Journal of Pediatrics (2022)
-
Sustained inflations versus UK standard inflations during initial resuscitation of prematurely born infants in the delivery room: a study protocol for a randomised controlled trial
Trials (2017)