Abstract
The aim of our study was to evaluate the efficacy of infliximab for the treatment of patients with refractory Kawasaki disease (KD) and investigate the dynamic changes of cytokines during infliximab treatment. We have performed a study of cytokine and proinflammatory molecule levels in 43 KD patients including 18 responders to IVIG, 14 nonresponders, and 11 patients treated with infliximab. We determined serum levels of soluble TNF receptor I (sTNFR I) and IL-6, as well as VEGF, damage associated molecular pattern (DAMP) molecules; myeloid-related protein (MRP)8/MRP14 and S100A12 sequentially. In eight patients, fever subsided immediately upon infliximab treatment. Four patients, who started infliximab after 12 d of illness, developed coronary artery lesions. Each of the cytokines was elevated before infliximab treatment in all patients. Although serum levels of proinflammatory cytokines decreased dramatically after infliximab treatment, DAMP molecules and VEGF and markers of local tissue damage were not suppressed. In contrast, in IVIG responders all cytokines decreased markedly after IVIG treatment. We show that infliximab is one of the adoptive therapies in refractory KD patients. Different behaviors of proinflammatory cytokines and DAMP molecules and VEGF after infliximab treatment suggest that infliximab is effective for suppression of cytokine-mediated inflammation, but could not completely block local vasculitis.
Similar content being viewed by others
Main
Kawasaki disease (KD) is the most common systemic vasculitis syndrome primarily affecting small and medium-sized arteries, particularly the coronary artery. Although timely treatment with high-dose i.v. immune globulin (IVIG) is now accepted as reducing the incidence of coronary artery lesions (CAL), approximately 15% of the patients do not respond to IVIG treatment and have persistent fever as a manifestation of ongoing inflammation. These patients are at highest risk for development of CAL (1). The current practice for patients with KD and persistent or recrudescent fever after IVIG is to institute additional therapies, which may include one or more repeat doses of IVIG, high-dose pulse methylprednisoline, cyclophosphamide, methotrexate, ulinastatin, cyclosporine A (CyA), or plasmapheresis (2,3). Recently, potential new therapeutic approaches with infliximab (Remicade), a chimeric mouse-human MAb against tumor necrosis factor (TNF)-α, have been reported in refractory KD patients (4).
During the acute phase of KD, serum levels of proinflammatory cytokines such as TNF-α are elevated (5). In experimental studies of this syndrome, characterized by vasculitis resulting in coronary, as well as extracoronary, aneurysms, and stenosis, the attenuation of cytokine responses, especially IL-6, after infusions of IVIG may play an integral role in the rapid resolution of most of the symptoms in children with KD (6). In addition to these proinflammatory cytokines, VEGF, and markers of local inflammation of the family of damage-associated molecular pattern molecules (DAMPs) such as myeloid-related protein (MRP) 8/MRP14 and S100A12 have been reported to increase in acute KD and to play a crucial role in inflammation and are probably involved in the pathophysiology of acute vasculitis (7–13).
MRP8/MRP14, two calcium-binding proteins in the S-100 family, binds to microvascular endothelial cells and may participate in the genesis of a proinflammatory and prothrombotic state during systemic vasculitis (9,13). MRP8/MRP14 are released in high amounts at local sites of inflammation and have been recently described as novel members of the DAMP-family acting as endogenous ligands of toll-like receptor 4 (TLR4) (12,14). We reported that MRP8/MRP14 levels closely correlate with disease activity in acute KD and potential biomarker to predict both responses to IVIG therapy and coronary artery sequelae in the acute stage of KD (8,9). Another member of the S100 family, S100A12, also binds to endothelial cells via the receptor for advanced glycation end products (RAGE) and induces cell activation and cytokine production through the nuclear factor-kappa-B signaling pathway (10,11). Transcript and protein levels of these three S100 proteins are reported to be strongly up-regulated during the acute stage of KD and decrease significantly in response to IVIG treatment and are possibly involved in the pathophysiology of acute vasculitis (8–11,15).
Here, we report the distinct effects of infliximab on systemic inflammation and local vasculitis, evaluating both proinflammatory and DAMP molecules and VEGF expression during infliximab treatment.
METHODS
Study population and blood samples.
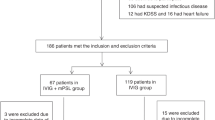
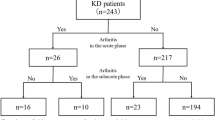
Patients with acute KD seen at the University Hospitals of Toyama University and Toho University School of Medicine between January 2005 and December 2007 were enrolled. All patients fulfilled the diagnostic criteria for KD and were initially treated with IVIG (2 g/kg body weight for 1 d) and oral aspirin (30 mg/kg/d) (16). Patients whose fever subsided within 48 h of IVIG treatment (2 g/kg body weight for 1 d) were considered responders. Patients whose fever did not subside within 48 h of the first IVIG treatment (2 g/kg body weight for 1 d) but responded to the second IVIG were designated nonresponders. Refractory KD was defined as the persistence or recrudescence of fever at least 48 h after the end of the multiple administrations of IVIG or IVMP infusion. Infliximab was used to the patient who was more than 1-y-old and received BCG vaccine. Thirty-one age-matched healthy control patients (16 males and 15 females), aged 3 mo to 7 y 5 mo (median 3.8 y), were enrolled during the same period.
Two-dimensional echocardiography was performed before and after treatment with IVIG as well as at 2 and 4 wk after the onset of KD, which was defined as the day on which fever developed. A coronary artery with a diameter of 3 mm or more (4 mm if the subject was over the age of 5 y) by echocardiogram was considered abnormal (16). The presence of CAL was assessed 1 mo after the onset of KD.
Patient demographic characteristics, therapies administered for KD before and after infliximab treatment, C-reactive protein (CRP) levels, dose, patient response to infliximab, and coronary artery outcome were recorded for all patients. Blood samples were collected from patients before and within 48 h after infliximab treatment in refractory KD and before and within 48 h after the first IVIG treatment in responders and nonresponders to IVIG. Simultaneously, blood samples were collected from healthy control patients on a single occasion. Parental informed consent was obtained for each child enrolled in this study, which was approved by the Research Ethics Committee of Toyama University Hospital.
Determination of serum cytokine levels.
Serum concentrations of soluble tumor necrosis factor-alpha receptor I (sTNFRI), IL-6, VEGF, MRP 8/MRP 14, S100A12, and soluble receptor for advanced glycation end product (sRAGE) were determined by a sandwich enzyme-linked immunosorbent assay (ELISA). Commercial kits to quantitative human sTNFRI (Bender MedSystem, Vienna, Austria), human IL-6 (BioSource International, CA), human VEGF (Immuno-Biologic Laboratories, Fujioka, Japan), and sRAGE (Quantikine; R&D Systems, Minneapolis, MN) were used according to the manufacturer-recommended procedures (17,18). Serum concentrations of S100A12 and MRP8/MRP14 were determined by a double-sandwich ELISA using a specific antibody without cross reactivity to other S100 proteins, as described previously (19).
Statistical analysis.
All results were expressed as mean ± SD. Paired t test was used to test for significance of the same parameter, within the same group, respectively. Analysis of variance or χ2 test was used to test for significance of variables among three different groups. If data did not follow a normal distribution, the paired t test was replaced by a Wilcoxon signed rank test. When the data followed a normal distribution determined by Shapiro-Wilks test, comparisons between the two groups were performed using an unpaired t test or a Welch's test depending on equal or unequal variance. If the data did not follow a normal distribution, then a Mann Whitney U test was used.
RESULTS
Patient clinical characteristics and laboratory data.
Table 1 shows the clinical characteristics of the 43 KD patients enrolled, comprising 18 responders, 14 nonresponders to the first IVIG, and 11 refractory KD patients treated with infliximab. The refractory KD patients and nonresponders had a significantly higher maximum concentration of CRP, a higher incidence of CALs, and a longer duration of fever compared with the responders. There were no significant difference between the groups with respect to age and the maximum number of white blood cells (WBCs).
In the refractory KD group, 10 patients received three or more IVIG infusions and eight patients received one to three doses of pulse methylprednisolone (30 mg/kg/dose i.v.) (Table 2). One patient did not use IVIG because she had a history of allergic reaction to immunglobulin. In addition, CyA was used in one patient (Table 2). All failed to become persistently afebrile after these treatments.
Patient outcome.
Of the 11 refractory patients, 10 received a single infusion of 5 mg/kg of infliximab: one patient received a second infusion of 5 mg/kg. In eight of the 11 patients, fever subsided dramatically in response to the infliximab treatment and other symptoms disappeared (Table 2). In three patients, fever persisted and needed additional therapy after infliximab treatment. Four patients had coronary artery abnormalities documented by echocardiography before infliximab therapy and had transient dilatation that resolved postinfliximab infusion (Table 2); these patients continued to have CAL after treatment. Seven patients had normal coronary arteries preinfliximab and postinfliximab treatment. All 11 patients (excluding Patient 1, who died) were followed for 6–26 mo (median follow-up 17 mo) with no apparent complications of their infliximab therapy. Tuberculin reactions before and 6 mo after infliximab treatment disclosed no evidence of tuberculosis in all patients. Chest CT after 6 mo of infliximab treatment revealed normal findings in all patients.
Serum cytokine levels.
The changes in serum levels of cytokines in refractory KD, and responders and nonresponders are shown in Table 3 and Figures 1 and 2.
Sequential changes of proinflammatory cytokines, CRP (left), sTNFR I (middle), and IL-6 (right), in refractory KD patients who were treated with infliximab (•), compared with responders (□). Blood samples were collected from patients before and within 48 h after infliximab treatment in refractory KD and before and within 48 h after the first IVIG treatment in responders to IVIG. The p value shows changes between before and after treatment in each group. *p < 0.05, †p < 0.01.
Sequential changes of endothelial cell specific cytokines and markers of local tissue damage, myeloid-related protein (MRP8/MRP14) (left), S100A12 (left middle), sRAGE (right middle), and VEGF (right), in refractory KD patients who were treated with infliximab (•), compared with responders (□). p value shows changes between before and after treatment in each group. *p < 0.05, †p < 0.01.
Serum CRP levels were higher in the refractory KD and nonresponders groups than the responders before treatment (Fig. 1). Levels decreased in both the refractory and responders after treatment but increased further in the nonresponders. Before treatment, SNTFR was increased in all three groups by comparison with controls before treatment and declined to the normal level after treatment in all three groups. Serum IL6 was increased in all three patient groups by comparison with controls before treatment and was significantly higher in the refractory group than the other two groups. After treatment, all three groups decreased but remained higher than controls and were indistinguishable from each other.
Serum levels of MRP8/MRP14 and S100A12 were higher than controls in all three patient groups before treatment with the levels in the refractory patients and nonresponders higher than the responders (Fig. 2). After treatment, levels decreased in the responders, but increased further in the refractory patients and nonresponders. Serum levels of sRAGE were lower than controls in the refractory and nonresponder groups before treatment, whereas they were similar to controls in the responder group. Levels of sRAGE increased in all three groups after treatment but remained below normal in the refractory and nonresponder groups. Serum levels of VEGF were higher than controls in all three patient groups before and after treatment with only moderate changes seen after treatment.
As a result, each of the cytokines was elevated compared with healthy controls before treatment in all patients. Although serum IL-6 and sTNFRI levels dramatically decreased after infliximab treatment and correlated with serum CRP levels and fevers, the serum levels of VEGF and DAMP-molecules such as MRP8/MRP14 and S100A12 remained high after infliximab treatment in refractory KD. This pattern of cytokines in refractory KD is different from responders or nonresponders after IVIG treatment; all cytokines decreased markedly in responders and did not decrease in nonresponders.
DISCUSSION
In this study, we show for the first time that different cytokines and proinflammatory DAMP-molecules are up-regulated and changed dynamically during IVIG and infliximab treatment in refractory KD patients (Table 3, Fig. 1 and 2). In refractory KD, the serum sTNFRI and IL-6 levels reacted to infliximab treatment, but VEGF and DAMP-molecules like MRP8/MRP14 and S100A12 as well as sRAGE were not significantly affected.
Previous studies have shown that sTNFRI is the natural homeostatic regulator of TNF-α activity and may reflect the true biologic activity of TNF-α more closely than serum TNF-α level (20). IL-6 causes many of the clinical and laboratory features of KD and is a reflection of a vigorous acute phase response (21). A recent case study reported that serum IL-6 was elevated and then decreased after infliximab treatment in a refractory KD patient (22). In this study, the fact that the serum levels of sTNFRI and IL-6 are elevated and decrease after infliximab treatment suggest infliximab blocks systemic inflammation and inhibits the process of signaling of cytokines via TNF-α in KD.
In contrast, the serum levels of MRP8/MRP14, S100A12, and VEGF remained high after infliximab treatment. MRP8/MRP14, a complex of two calcium-binding proteins of the S-100 family, form heterodimers and are secreted by neutrophils and monocytes in response to inflammatory signaling cascades (Fig. 3) (8,9,23). The MRP8/MRP14 heterodimer binds to microvascular endothelial cells and phagocytes and may participate in the genesis of a proinflammatory and prothrombotic state during systemic vasculitis (24). Specifically, these proteins regulate adhesion of neutrophils and monocytes to endothelial cells and are implicated in their transmigration into the vessel wall (25). MRP8/MRP14 is believed to have an important functional role in vasculitis syndromes and serves as a marker identifying patients at risk for developing CAL during acute phase of KD (8). Interestingly, MRP8/MRP14 has recently been identified as novel endogenous ligands of TLR4, which directly promote inflammation. MRP14 −/− mice are protected from LPS-induced shock due to a lack of TNF-α production compared with wild-type mice indicating that MRP8/MRP14 act up-stream of TNF-α in the inflammatory cascade (12). This hypothesis is supported by our data showing that blockade of TNF-α efficiently inhibits down-stream pathways of systemic inflammation, such as the expression of IL-6, but does not completely block expression of local proinflammatory mechanisms. Whether this lack of action has negative consequences with respect to the long-term prognosis of KD-patients after infliximab treatment cannot be answered by this relatively small cohort but requires a prospective follow-up study including a larger number of patients.
TNF-α and other proinflammatory cytokines activate endothelium and lead to the expression of carboxylated N-glycans. MRP8/MRP14 are released in high amounts at local sites of inflammation and have been recently described as novel members of the DAMP-family acting as endogenous ligands of TLR4. Activated neutrophils and monocytes secrete MRP-8/MRP-14 heterodimers, which bind to the carboxylated N-glycans and heparin sulfate on the endothelial cell surface. Leukocytes also secrete S100A12, which binds to the RAGE expressed on endothelial cells, lymphocytes, and macrophages. This receptor signals through the nuclear factor-kappa-B pathway and induces expression of many proinflammatory molecules. The net result of S100 protein binding is platelet aggregation and adherence to endothelium, increased expression of vascular cell adhesion molecule-1 and intercellular adhesion molecule-1, adhesion of neutrophils and monocytes, loosening of endothelial cell junctions, and trafficking of inflammatory cells across the endothelial cell barrier. Adapted from Burns J, J Am Coll Cardiol 48:1265–1267, copyright © 2006 American College of Cardiology Foundation Published by Elsevier Inc., with permission.
Another member of the S100 family, S100A12, is also released by neutrophils, binds to the RAGE on endothelial cells and leukocytes, and induces cell activation and cytokine production through the nuclear factor-kappa-B signaling pathway (26) (Fig. 3). Transcript and protein levels of all three of these S100 proteins are increased in circulating leukocytes and in serum during the acute phase of KD (8–11,15,23). Taken together, these observations support the hypothesis that MRP8/MRP14 heterodimers and S100A12 participate directly in the pathogenesis of the coronary artery vasculitis in KD and contribute to endothelial cell damage and transmigration of leukocytes into the arterial wall independent of TNF-α activity. Moreover, during acute KD, sRAGE may block the binding of S100A12 to RAGE on the cell surface by neutralizing this proinflammatory protein. The fact that concentrations of MRP8/MRP14 and S100A12 did not change during infliximab treatment indicates that MRP8/MRP14 and S100A12 maintain signaling of local vascular injury despite the blockade of TNF-α. Lower levels of sRAGE detected in KD patients might thus confer susceptibility to hyperinflammation (27). Lower levels of sRAGE may reflect insufficient compensation of S100A12 because of the occurrence of dramatic and strong inflammation in refractory KD patients during infliximab treatment.
VEGF enhances proliferation and migration of endothelial cells in collaboration with nitric oxide and may contribute to later vascular remodeling after the acute phase of KD (7). Because systemic overproduction of VEGF has been demonstrated in acute KD, VEGF is considered to be involved in the pathophysiology of KD, especially in the development of CAL (28,29).
This study shows that serum IL-6 and sTNFRI levels dramatically decreased after treatment and correlated with serum CRP levels and fevers; however, the serum levels of VEGF, MRP8/MRP14, and S100A12 remained high after infliximab treatment, especially in patients with CAL. In contrast, in IVIG responders all cytokines decreased markedly after IVIG treatment. These data indicate that proinflammatory cytokines decrease in response to infliximab treatment, but VEGF and local inflammatory proteins of the DAMP-family such as MRP8/MRP14 and S100A12, which were reported to be important factors in development of CAL during acute stage of KD, do not. Thus, it seems that infliximab is effective for the suppression of systemic inflammation, but could not completely block the local vasculitis in KD.
We have now successfully treated eight of the 11 refractory KD patients. Three patients who did not respond to infliximab treatment needed additional therapy. Four patients developed CAL despite infliximab therapy: of note, these patients were treated later than the patients without CAL and had signs of CAL before treatment. Histopathological studies have shown that transient infiltration by granulocytes occurs in the very early stage of acute KD, before infiltration of mononuclear cells, suggesting granulocytes act as a trigger in the pathogenesis of CAL (30). In light of our data, to prevent the progression of CAL and to prevent the secretions of MRP8/MRP14 and S100A12 from inflammatory cells such as neutrophils and monocytes, early administration of infliximab, or combination therapy with IVIG may lead to the successful cessation of the inflammatory response and vasculitis.
Study limitations.
Limitations of this study include its retrospective nature, small number of patients, and the administration of multiple different therapies after the first IVIG infusion failure. Different IVIG preparations were used at different centers and concomitant or sequential antiinflammatory therapies administered to several of these patients precluded a final assessment of the effect of infliximab infusion. In conclusion, in this study, we show for the first time that inflammatory cytokines are up-regulated and changed dynamically during Infliximab treatment in refractory KD patients. Infliximab was effective for suppression of systemic inflammation, but could not completely block the local vasculitis in refractory KD patients. The early administration of infliximab or combination therapy with IVIG might be recommended for refractory KD patients.
Abbreviations
- CAL:
-
coronary artery lesions
- CRP:
-
C-reactive protein
- IVIG:
-
intravenous immune globulin
- KD:
-
Kawasaki disease
- MRP:
-
myeloid-related protein
- sRAGE:
-
soluble receptor for advanced glycation end product
- sTNFRI:
-
soluble tumor necrosis factor-alpha receptor I
- DAMP:
-
damage associated molecular pattern molecules
References
Tremoulet AH, Best BM, Song S, Wang S, Corinaldesi E, Eichenfield JR, Martin DD, Newburger JW, Burns JC 2008 Resistance to intravenous immunoglobulin in children with Kawasaki disease. J Pediatr 153: 117–121
Pinna GS, Kafetzis DA, Tselkas OI, Skevaki CL 2008 Kawasaki disease: an overview. Curr Opin Infect Dis 21: 263–270
Hashino K, Ishii M, Iemura M, Akagi T, Kato H 2001 Re-treatment for immune globulin-resistant Kawasaki disease: a comparative study of additional immune globulin and steroid pulse therapy. Pediatr Int 43: 211–217
Burns JC, Best BM, Mejias A, Mahony L, Fixler DE, Jafri HS, Melish ME, Jackson MA, Asmar BI, Lang DJ, Connor JD, Capparelli EV, Keen ML, Mamun K, Keenan GF, Ramilo O 2008 Infliximab treatment of intravenous immunoglobulin-resistant kawasaki disease. J Pediatr 153: 833–838
Gupta M, Noel GJ, Schaefer M, Friedman D, Bussel J, Johann-Liang R 2001 Cytokine modulation with immune gamma-globulin in peripheral blood of normal children and its implications in Kawasaki disease treatment. J Clin Immunol 21: 193–199
Nishimura S, Zaitsu M, Hara M, Yokota G, Watanabe M, Ueda Y, Imayoshi M, Ishii E, Tasaki H, Hamasaki Y 2003 A polymorphism in the promoter of the CD14 gene (CD14/-159) is associated with the development of coronary artery lesions in patients with Kawasaki disease. J Pediatr 143: 357–362
Hamamichi Y, Ichida F, Yu X, Hirono KI, Uese KI, Hashimoto I, Tsubata S, Yoshida T, Futatani T, Kanegane H, Miyawaki T 2001 Neutrophils and mononuclear cells express vascular endothelial growth factor in acute Kawasaki disease: its possible role in progression of coronary artery lesions. Pediatr Res 49: 74–80
Hirono K, Foell D, Xing Y, Miyagawa-Tomita S, Ye F, Ahlmann M, Vogl T, Futatani T, Rui C, Yu X, Watanabe K, Wanatabe S, Tsubata S, Uese K, Hashimoto I, Ichida F, Nakazawa M, Roth J, Miyawaki T 2006 Expression of myeloid-related protein-8 and -14 in patients with acute Kawasaki disease. J Am Coll Cardiol 48: 1257–1264
Viemann D, Strey A, Janning A, Jurk K, Klimmek K, Vogl T, Hirono K, Ichida F, Foell D, Kehrel B, Gerke V, Sorg C, Roth J 2005 Myeloid-related proteins 8 and 14 induce a specific inflammatory response in human microvascular endothelial cells. Blood 105: 2955–2962
Foell D, Ichida F, Vogl T, Yu X, Chen R, Miyawaki T, Sorg C, Roth J 2003 S100A12 (EN-RAGE) in monitoring Kawasaki disease. Lancet 361: 1270–1272
Ye F, Foell D, Hirono KI, Vogl T, Rui C, Yu X, Watanabe S, Watanabe K, Uese K, Hashimoto I, Roth J, Ichida F, Miyawaki T 2004 Neutrophil-derived S100A12 is profoundly upregulated in the early stage of acute Kawasaki disease. Am J Cardiol 94: 840–844
Vogl T, Tenbrock K, Ludwig S, Leukert N, Ehrhardt C, van Zoelen MA, Nacken W, Foell D, van der Poll T, Sorg C, Roth J 2007 MRP8 and MRP14 are endogenous activators of Toll-like receptor 4, promoting lethal, endotoxin-induced shock. Nat Med 13: 1042–1049
Viemann D, Barczyk K, Vogl T, Fischer U, Sunderkötter C, Schulze-Osthoff K, Roth J 2007 MRP8/MRP14 impairs endothelial integrity and induces a caspase-dependent and -independent cell death program. Blood 109: 2453–2460
Foell D, Wittkowski H, Vogl T, Roth J 2007 S100 proteins expressed in phagocytes: a novel group of damage-associated molecular pattern molecules. J Leukoc Biol 81: 28–37
Abe J, Jibiki T, Noma S, Nakajima T, Saito H, Terai M 2005 Gene expression profiling of the effect of high-dose intravenous Ig in patients with Kawasaki disease. J Immunol 174: 5837–5845
Shulman ST, Inocencio J, Hirsch R 1995 Kawasaki disease. Pediatr Clin North Am 42: 1205–1222
Adolf GR, Apfler I 1991 A monoclonal antibody-based enzyme immunoassay for quantitation of human tumor necrosis factor binding protein I, a soluble fragment of the 60 kDa TNF receptor in biological fluids. J Immunol Methods 143: 127–136
Hirata C, Nakano K, Nakamura N, Kitagawa Y, Shigeta H, Hasegawa G, Ogata M, Ikeda T, Sawa H, Nakamura K, Ienaga K, Obayashi H, Kondo M 1997 Advanced glycation end products induce expression of vascular endothelial growth factor by retinal Muller cells. Biochem Biophys Res Commun 236: 712–715
Vogl T, Propper C, Hartmann M, Strey A, Strupat K, van den Bos C, Sorg C, Roth J 1999 S100A12 is expressed exclusively by granulocytes and acts independently from MRP8 and MRP14. J Biol Chem 274: 25291–25296
Furukawa S, Matsubara T, Umezawa Y, Okumura K, Yabuta K 1994 Serum levels of p60 soluble tumor necrosis factor receptor during acute Kawasaki disease. J Pediatr 124: 721–725
Ueno Y, Takano N, Kanegane H, Yokoi T, Yachie A, Miyawaki T, Taniguchi N 1989 The acute phase nature of interleukin 6: studies in Kawasaki disease and other febrile illnesses. Clin Exp Immunol 76: 337–342
Saji T, Kemmotsu Y 2006 Infliximab for Kawasaki syndrome. J Pediatr 149: 426
Burns JC 2006 S100 proteins in the pathogenesis of Kawasaki disease. J Am Coll Cardiol 48: 1265–1267
Eue I, Konig S, Pior J, Sorg C 2002 S100A8, S100A9 and the S100A8/A9 heterodimer complex specifically bind to human endothelial cells: identification and characterization of ligands for the myeloid-related proteins S100A9 and S100A8/A9 on human dermal microvascular endothelial cell line-1 cells. Int Immunol 14: 287–297
Srikrishna G, Panneerselvam K, Westphal V, Abraham V, Varki A, Freeze HH 2001 Two proteins modulating transendothelial migration of leukocytes recognize novel carboxylated glycans on endothelial cells. J Immunol 166: 4678–4688
Hoffmann MA, Drury S, Fu C, Qu W, Taguchi A, Lu Y, Avila C, Kambham N, Bierhaus A, Nawroth P, Neurath MF, Slattery T, Beach D, McClary J, Nagashima M, Morser J, Stern D, Schmidt AM 1999 RAGE mediates a novel proinflammatory axis: a central cell surface receptor for S100/ calgranulin polypeptides. Cell 97: 889–901
Wittkowski H, Hirono K, Ichida F, Vogl T, Ye F, Yanlin X, Saito K, Uese K, Miyawaki T, Viemann D, Roth J, Foell D 2007 Acute Kawasaki disease is associated with reverse regulation of soluble receptor for advance glycation end products and its proinflammatory ligand S100A12. Arthritis Rheum 56: 4174–4181
Terai M, Yasukawa K, Narumoto S, Tateno S, Oana S, Kohno Y 1999 Vascular endothelial growth factor in acute Kawasaki disease. Am J Cardiol 83: 337–339
Yasukawa K, Terai M, Shulman ST, Toyozaki T, Yajima S, Kohno Y, Rowley AH 2002 Systemic production of vascular endothelial growth factor and fms-like tyrosine kinase-1 receptor in acute Kawasaki disease. Circulation 105: 766–769
Naoe S, Shibuya K, Takahashi K, Wakayama M, Masuda H, Tanaka M 1991 Pathological observations concerning the cardiovascular lesions in Kawasaki disease. Cardiol Young 1: 212–220
Acknowledgements
We thank Drs. Ayumi Miyazaki, Osamu Higuchi, Shinichi Tsubata for their invaluable contributions to collection of patients samples. We also thank Chang Bo, Chikako Sakai, Hitoshi Moriuchi, and Neil E. Bowles for their excellent assistance.
Author information
Authors and Affiliations
Additional information
Supported by grants from the Japan Kawasaki Disease Research Center, from The Ministry of Education, Culture, Sports, Science, and Technology in Japan (Grant-in-Aid for Scientific Research 20790721), and from the Ministry of Health, Labor and Welfare in Japan (Grant-in-Aid for Clinical Research H20 008).
Rights and permissions
About this article
Cite this article
Hirono, K., Kemmotsu, Y., Wittkowski, H. et al. Infliximab Reduces the Cytokine-Mediated Inflammation but Does Not Suppress Cellular Infiltration of the Vessel Wall in Refractory Kawasaki Disease. Pediatr Res 65, 696–701 (2009). https://doi.org/10.1203/PDR.0b013e31819ed68d
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e31819ed68d
This article is cited by
-
Targeted Use of Prednisolone with Intravenous Immunoglobulin for Kawasaki Disease
Clinical Drug Investigation (2021)
-
Infliximab versus intravenous immunoglobulin for refractory Kawasaki disease: a phase 3, randomized, open-label, active-controlled, parallel-group, multicenter trial
Scientific Reports (2018)
-
Analysis of biomarker serum levels in IVIG and infliximab refractory Kawasaki disease patients
Clinical Rheumatology (2018)
-
Kawasaki disease: guidelines of Italian Society of Pediatrics, part II - treatment of resistant forms and cardiovascular complications, follow-up, lifestyle and prevention of cardiovascular risks
Italian Journal of Pediatrics (2018)
-
TNF and IL-1 Targeted Treatment in Kawasaki Disease
Current Treatment Options in Rheumatology (2016)