Abstract
The observation on the impact of constipation on nutritional and growth status in healthy children was never reported. During a 4-y period, we evaluated the consequence of constipation on growth in children. The enrolled children were aged between 1 and 15 y with constipation. Medical response of constipation to treatment was evaluated by the scoring of constipation symptoms. The correlation of therapeutic effect of constipation with growth status at 12 wk and 24 wk was statistically evaluated. About 2426 children (1284 boys, 1142 girls) with a mean age of 7.31 ± 3.65 (range 1.1–14.9) y were enrolled. After 12-wk treatment, significant increase of z-scores of height-for-age, weight-for-age, and body mass index-for-age were all found in patients with good medical responses (1377 cases) than in those with poor medical responses (1049 cases). The 1049 patients with poor medical response received advanced medications; significant increase of z-scores of height-for-age, weight-for-age, and body mass index were also found in these patients. A marked increase of appetite was significantly correlated with better gain on height and weight after treatment. We conclude that chronic constipation may retard growth status in children, and a long-term medication for constipation in children appears beneficial to their growth status.
Similar content being viewed by others
Main
The prevalence of constipation continues to remain high in many developing countries. It is associated with several adverse outcomes throughout life. Constipation generally is defined by the hard nature of the stool, the pain associated with its passage, or the failure to pass three stools per week (1). It is a very common frustration for children, parents, and physicians. In most pediatric cases, constipation is temporary and not serious. However, in some cases constipation can lead to various complications such as nausea, abdominal pain, or rectal bleeding caused by anal fissure (2,3). Patients diagnosed with chronic diseases such as irritable bowel syndrome with constipation, for example, were more likely to report weight loss (4–6). The observation or discussion about the impact of constipation on nutritional status or growth status in healthy children was never reported.
The present study was undertaken to investigate the growth status of Taiwanese children with constipation and to further evaluate the influence of constipation on growth status during a 24-wk medical treatment. The effect of constipation-relief by medication on the growth status in children was also investigated and discussed.
PATIENTS AND METHODS
Patients.
During a 4-y period (July 2002–June 2006), we prospectively conducted a long-term (24 wk) medical treatment in children aged between 1 and 15 y with constipation and tried to evaluate the consequence of constipation on growth status in children. Constipation is diagnosed when a child has hard stools or has difficult defecation or frequency of defecation less than three times in a week for more than 1 mo. Patients with known gastrointestinal disease such as gastroesophageal reflux disease, celiac disease, inflammatory bowel disease, cardiopulmonary disease, liver disease, renal disease, genetic diseases, endocrinal disease, or who have received abdominal surgeries were excluded. Patients with acute illness such as enteritis, pneumonia, urinary tract infection, or prolonged symptoms (>1 wk) of respiratory tract infection during study periods, which may influence the consequence of appetite and growth, were excluded from the study. Those age-matched healthy children who visited the nutrition clinic for dietary, growth, and nutrition assessment with regular survey for growth for more than 24 wk were enrolled as control. The result of growth status, and gastric emptying data of the control children were used as control data for comparison.
Interventions.
Before intervention, growth velocities (height and weight increment) were obtained for 2 wk before entering the study. All the subjects were assigned medical treatment and follow-up visits every 2 wk at clinic for 24 wk. Medical treatment and protocol assigned was oral magnesium oxide 10–15 mg/kg/dose three times per day, the dosage of magnesium oxide was tapered to twice or once per day if complete relief of constipation during 2 wk observation was achieved. Those children with fair or poor medical response of constipation at 12 wk received further advanced medications for the next 12 wk. The advanced medication assigned included stimulants (sennoside 7.5–15 mg once per day) or osmotic laxatives (rectal enema). The dosage of stimulants was tapered to half dose per day if complete relief of constipation in 2 wk was achieved.
Assessment for growth status.
The investigated clinical features included change of appetite, growth status, and body mass index (BMI). Appetite evaluated was based on 3-d dietary records performed by the patient's family. The investigated growth status included z-scores of height-for-age, weight-for-age, and BMI made at baseline, 12 wk, and 24 wk. The difference of growth velocity (height and weight gain) between patients with different status of improvement of constipation was evaluated. The Department of Health of Taiwan, R.O.C in June 1999, conducted the evaluated growth charts. Height-for-age z-score, weight-for-age z-score, and BMI-for-age z-score were computed according to the statue percentile on growth charts.
The result of medical treatment on constipation was evaluated by the symptoms observed each 2 wk. The period of assessment of efficacy of medical treatment on constipation was 12 wk. A “good response” of treatment for constipation was obtained if the children had a duration of symptoms <40% of the observation period. A “poor response” of constipation was obtained if the children had a duration of symptoms >40% of observation period.
The change of appetite was assessed twice; first assessment was between dietary records at first 2 wk and last 2 wk of the 12 wk (1–12 wk). The second assessment was between first 2 wk and last 2 wk of the next 12 wk (13–24 wk). Children with an increase of appetite were defined as having marked increase >20% of daily intake volume of major foods originated from carbohydrate and/or protein: rice, milk, meat, etc.
Data collection and statistical analysis.
The data consisting of the change of height, weight, height-for-age z-score, weight-for-age z-score, and BMI-for-age z-score at baseline, 12 wk, and 24 wk were obtained from the records of charts reviewed. The correlation of change of growth status with medical response on constipation and appetite was statistically evaluated. Those patients with fair or poor medical response after 12-wk medical therapy received advanced medication for the next 12 wk, and the correlation of growth status with appetite was further statistically evaluated. Continuous data were expressed as the average ± SD (SD). The data were analyzed using a statistical system (SAS). We used student t test for continuous variables and Mantel-Haenszel χ2 test for categorical data. A p < 0.05 was considered significant.
The study was evaluated and approved by Research Committee of Chang Gung Memorial Hospital (#96117). All the participants proved written informed consent.
RESULTS
Demographic and clinical characteristics.
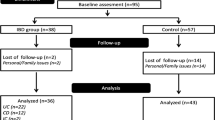
The study included 3025 enrolled children. One hundred thirty-eight cases with prolonged illness of upper respiratory tract infection, 126 cases with enteritis, 26 cases with bronchitis, 13 cases with pneumonia, 176 cases without compliance of medical treatment, and 120 cases had loss of follow-up were excluded during the study period. Finally, there were 2426 children entered into the study who completed the medical treatment and the 24-mo observation. The population in each age group were 1–3 y, 445 cases (18.3%); 4–6 y, 601 cases (24.8%); 6–9 y, 519 cases (21.4%); 10–12 y, 405 cases (16.7%); and 13–15 y, 456 cases (18.8%). The demographic data and clinical characteristics of these children are shown in Table 1. The enrolled control consisted of 683 children (349 boys, 334 girls). Mean age of these children was 7.26 ± 3.91 y, which was similar to the age of the studied patients (7.31 ± 3.65 y) (p = 0.558, student t test).
Growth status at baseline, 12 wk, and 24 wk.
Table 2 demonstrate growth status (weight, height, and BMI) at baseline, 12 wk, and 24 wk in the patients and control. Comparing to the data in the healthy controls, statistically lower height, weight, height-for-age z-score, weight-for-age z-score, BMI-value, and BMI-for-age z-score were found in the studied patients (all p < 0.001, student t test). Secure increments of height, weight, height-for-age z-score, weight-for-age z-score, and BMI-for-age z-score found at 12 wk and 24 wk (Table 2). The average increment of height and weight in the studied patients were 1.55 ± 0.34 cm and 0.93 ± 0.21 kg between baseline and 12 wk, and 1.53 ± 0.35 cm and 0.86 ± 0.20 kg between baseline and 24 wk. The differences of height-for-age and weight-for-age z-scores were statistically significant between baseline and 12 wk and between baseline and 24 wk (all p < 0.001, student t test). Significant differences of BMI value and BMI-for-age z-score were found between baseline and 12 wk and between baseline and 24 wk (all p < 0.001, χ2 analysis and student t test).
In the healthy controls, average values of height-for-age z-score, weight-for-age z-score, BMI value and BMI-for-age z-score of the healthy control were all approaching to zero (= 50 percentile of statue status on growth chart). The average increment of height and weight were 1.41 ± 0.26 cm and 0.80 ± 0.18 kg between baseline and 12 wk, and 1.39 ± 0.26 cm and 0.81 ± 0.19 kg between baseline and 24 wk, respectively.
In comparison to the data of the control, more increment of height and weight were found in the studied patients after 12 and 24 wk (all p < 0.001, student t test).
Change of constipation status at baseline, 12 wk, and 24 wk.
About 1377 cases (56.8%) had good improvement of constipation after 12-wk of intervention, 127 of 1377 cases (9.2%) had poor improvement of constipation during 13–24 wk. About 1049 cases (43.2%) had poor improvement of constipation after 12 wk of intervention. After advanced medical treatment during 13–24 wk, 613 cases (58.4%) showed good improvement of constipation.
Correlation of growth to different medical responses on constipation.
Table 3 shows the correlation of growth status with different medical response (12 wk) of constipation. Compared with the growth velocity before intervention, the growth velocity on height and weight both increased after 12-wk intervention. More significant increment of height, weight, BMI, height-for-age z-score, weight-for-age z-score, and BMI-for-age z-score were found in those patients with good medical response (1377 cases) than in those with fair or poor medical responses (1049 cases) (p < 0.001, <0.001, 0.002, 0.017, <0.001, and 0.005). Compared with the data of the control, significantly more increment in height and weight were demonstrated in the patients with good medical response after 12-wk intervention (both p < 0.001, student t test), whereas less increment in height and weight was found in the patients with poor medical response, and the difference in weight gain was significant (p < 0.001, student t test).
Table 4 analyzes the correlation of growth status in children with advanced medication during 13–24 wk. Those 1049 patients with fair or poor responses received further advanced medications. More significant increment of height, weight, BMI, height-for-age z-score, weight-for-age z-score, and BMI-for-age z-score were found in patients with good medical response than in patients with poor medical responses (p < 0.001, <0.001, 0.019, 0.035, 0.008, and 0.041) (Table 4). Compared with the control data, significantly more increment in height and weight were demonstrated in the patients with continual good medical response after 24-wk intervention (both p < 0.001, student t test), whereas significantly less increment in height and weight was found in the patients who required advanced medical treatment (both p < 0.001, student t test).
Correlation of growth with change of appetite.
A total of 1333 (54.9%) and 1775 (73.2%) cases had an increase of appetite at 12 wk and 24 wk. As shown in Table 5, significant increase of height, and weight was found in those patients with increase of appetite at 12 wk (both p < 0.001), and those with increase of appetite at 24 wk (both p < 0.001).
DISCUSSION
Growth expressed as rate of change in weight and height (velocity) are assessed by comparing indices against the reference population. In assessing the growth status of individual children, plotting a child's weight and height over time allows assessment of the child's own growth curve in relation to a reference population. Commonly used derived indices for growth include weight-for-height, weight-for-age, and height-for-age measurements. Pediatric growth charts have been extensively used by pediatricians, nurses, and parents to track the growth of infants, children, and adolescents worldwide. If the growth charts are computerized together with regional databases, they will provide necessary growth data for descriptive health surveys (7). Growth charts are commonly used to identify sick children or children that have other causes for growth disturbances (7). New World Health Organization pediatric growth charts conducted by a multicenter study affirm that growth charts can be used to assess children everywhere, regardless of ethnicity, socio-economic status, and nutrition (8). BMI, calculated as weight (kg) or height (2) (m2), is commonly used as an obesity index and has recently been recommended as an indicator of surveying overweight and nutritional status in children after infancy (9–11).
The present study was undertaken to investigate the growth status of Taiwanese children with constipation, and further evaluates the impact of constipation on growth status during a 12-wk and 24-wk medical therapy. Not like a previous observation indicated that chronic severe constipation was more prone to obese children (12), children with constipation in our series were prone to be malnourished. Misra et al. (12) indicated an association between chronic severe constipation and being overweight by comparing 101 overweight and constipated children with 100 normal controls. In their study, the overweight ones were significantly male predominant (70.45%) and showed significantly increased incidence of psychological or behavior disorders in comparison with the control group. In our study, those patients with psychological or behavior disorders were excluded. We have observed overweight or obese patients in our series, but patients with overweight or obesity were less commonly seen than those underweight or malnourished ones. In our series, near 5% of patients were in overweight (>90 percentile) or obese status, whereas near 25% of patients were underweight (<10% percentile) or malnourished. Results from the present study indicate that those children who experienced poor medical response remained more growth stunted than those with good response to treatment. Otherwise, the study also found that effective medical control of constipation resulted in increase of growth even after adjusting medical treatment. Growth deficits and reduced body weight may be caused by low protein, low energy, and/or low mineral intakes.
The mechanism of the impact of constipation on growth retardation has only minimally been evaluated to date. As expected from previous reports, chronic constipation may negatively influence growth (13,14). Constipation may be a contributing factor to poor growth in children with nocturnal enuresis (15). A previous study observed that constipation might impair appetite (16). Constipation adversely affects nutritional status by causing feelings of mild to severe abdominal discomfort, bloating, and nausea that leads to a loss of appetite (17). In a children study, fecal mass in the rectum and abdominal pain were markedly reduced and appetite improved after daily supplementation of polyethylene glycol (0.5 g/d/kg) (18). Based upon the detailed history of our patients, the majority of those children with poor growth status was found to have poor or decreased appetite before entering the study. Our results showed that those patients with increased appetite significantly had better increment in height and weight, suggesting increase of appetite may contribute to better growth in children with constipation. Growth deficits and reduced body weight during constipation in children may be caused by low protein, low energy, and/or low mineral intakes.
Our findings demonstrate the effective medical treatment to assist in maintaining appropriate rates of increase in BMI during constipation in children, and their known benefits for gastrointestinal health. We conclude that a long-term constipation may have a negative effect on the growth in children, but with long-term medication, restoration of normal growth is achievable.
References
Baker SS, Liptak GS, Colletti RB, Croffie JM, Di Lorenzo C, Ector W, Nurko S 1999 Constipation in infants and children: evaluation and treatment. J Pediatr Gastroenterol Nutr 29: 612–626
Rasquin-Weber A, Hyman PE, Cucchiara S, Fleisher DR, Hyams JS, Milla PJ, Staiano A 1999 Childhood functional gastrointestinal disorders. Gut 45: II60–II68
Loening Baucke V 2005 Prevalence, symptoms and outcome of constipation in infants and toddlers. J Pediatr 146: 359–363
Haynes L, Atherton D, Clayden G 1997 Constipation in epidermolysis bullosa: successful treatment with a liquid fiber-containing formula. Pediatr Dermatol 14: 393–396
Fowler AJ, Moskowitz DG, Wong A, Cohen SP, Williams ML, Heyman MB 2004 Nutritional status and gastrointestinal structure and function in children with ichthyosis and growth failure. J Pediatr Gastroenterol Nutr 38: 164–169
Chitkara DK, Bredenoord AJ, Cremonini F, Delgado-Aros S, Smoot RL, El-Youssef M, Freese D, Camilleri M 2004 The role of pelvic floor dysfunction and slow colonic transit in adolescents with refractory constipation. Am J Gastroenterol 99: 1579–1584
Gelander L 2006 Children's growth: a health indicator and a diagnostic tool. Acta Paediatr 95: 517–518
WHO Multicentre Growth Reference Study Group 2006 WHO Child growth standards based on length/height, weight and age. Acta Paediatrica Suppl 450: 76–85
Daley AJ, Copeland RJ, Wright NP, Roalfe A, Wales JK 2006 Exercise therapy as a treatment for psychopathologic conditions in obese and morbidly obese adolescents: a randomized, controlled trial. Pediatrics 118: 2126–2134
Faith MS, Dennison BA, Edmunds LS, Stratton HH 2006 Fruit juice intake predicts increased adiposity gain in children from low-income families: weight status-by-environment interaction. Pediatrics 118: 2066–2075
Speakman JR, Walker H, Walker L, Jackson DM 2005 Associations between BMI, social strata and the estimated energy content of foods. Int J Obes (Lond) 29: 1281–1288
Misra S, Lee A, Gensel K 2006 Chronic constipation in overweight children. JPEN J Parenter Enteral Nutr 30: 81–84
Baer MT, Harris AB 1997 Pediatric nutrition assessment: identifying children at risk. J Am Diet Assoc 97: S107–S115
White JL, Malcolm R, Roper K, Westphal MC Jr Smith C 1981 Psychosocial and developmental factors in failure to thrive: one- to three-year follow-up. J Dev Behav Pediatr 2: 112–114
Moffatt ME 1997 Nocturnal enuresis: a review of the efficacy of treatments and practical advice for clinicians. J Dev Behav Pediatr 18: 49–56
Allman S, Haynes L, MacKinnon P, Atherton DJ 1992 Nutrition in dystriophic epidermolysis bullosa. Pediatr Dermatol 9: 231–238
Poulsen I, Rahm Hallberg I, Schroll M 2006 Nutritional status and associated factors on geriatric admission. J Nutr Health Aging 10: 84–90
Dupont C, Leluyer B, Amar F, Kalach N, Benhamou PH, Mouterde O, Vannerom PY 2006 A dose determination study of polyethylene glycol 4000 in constipated children: factors influencing the maintenance dose. J Pediatr Gastroenterol Nutr 42: 178–185
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Chao, HC., Chen, SY., Chen, CC. et al. The Impact of Constipation on Growth in Children. Pediatr Res 64, 308–311 (2008). https://doi.org/10.1203/PDR.0b013e31817995aa
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e31817995aa
This article is cited by
-
The use of polyethylene glycol as a maintenance treatment of functional constipation in children living in Egypt
Egyptian Pediatric Association Gazette (2023)
-
The relationship between functional constipation and overweight/obesity in children: a systematic review and meta-analysis
Pediatric Research (2023)
-
Functional constipation induces bladder overactivity associated with upregulations of Htr2 and Trpv2 pathways
Scientific Reports (2021)