Abstract
Oxygen fluctuation patterns in preterm infants who develop retinopathy of prematurity (ROP) are varied and poorly represented in animal models. We examined the hypothesis that clustered (CL) episodes of hypoxia during hyperoxia results in a more severe form of oxygen-induced retinopathy (OIR) than dispersed episodes. Rat pups were exposed to alternating cycles of 1) 50% O2 with three CL episodes of 12% O2 every 6 h; or 2) 50% O2 with one episode of 12% O2 every 2 h, for 7 (P7) or 14 (P14) days postnatal age. Pups were killed after hyperoxia, or placed in room air (RA) until P21. RA littermates were killed at P7, P14, and P21. Systemic and ocular vascular endothelial growth factor (VEGF), soluble VEGFR-1 (sVEGFR-1), insulin-like growth factor I (IGF-I), and growth hormone were examined. All hyperoxia-exposed retinas had evidence of neovascularization. Animals in the CL group had a more severe form of OIR at P21 evidenced by vascular tufts, leaky vessels, retinal hemorrhage, and vascular overgrowth. These characteristics were associated with low body weight; high systemic and ocular VEGF; and low systemic and high ocular sVEGFR-1 and IGF-I. These data suggest that preterm infants who experience CL fluctuations in Pao2 during supplemental O2 therapy are at a higher risk for severe ROP.
Similar content being viewed by others
Main
Retinopathy of prematurity (ROP) continues to be a significant long-term morbidity in very low birth weight (VLBW) preterm infants (<1500 g) who experience numerous alterations in their O2 saturations (1,2). Although strict management of O2 exposure with careful monitoring of O2 saturation has been shown to be successful in controlling the disease (3), infants who experience the greatest fluctuations in their Pao2 seem to be at a higher risk for the development of threshold ROP (4). This is corroborated by animal studies which show a greater degree of retinal neovascularization in variable O2 levels (80/40%) compared with constant levels (80%) with further studies showing greater vascular pathology in cycles of hyperoxia/hypoxia (50/10%) compared with variable hyperoxia alone (80/40%) (5,6). Most of these studies have used models of hyperoxia with hypoxia lasting 12–24 h (5–9), but ill VLBW infants experience O2 fluctuations on the order of minutes, not hours.
Utilizing an experimental O2 model of brief, 2-min episodes of hypoxia dispersed (DP) every 2 h, we have demonstrated upregulation of retinal vascular endothelial growth factor (VEGF), VEGF receptor-2 (VEGFR-2), and severe neovascularization before recovery in room air (RA) (Coleman et al., 2007, unpublished data) suggesting that retinal VEGF upregulation, changes in vascular morphology, and neovascularization may be initiated before weaning from O2 therapy in VLBW infants who experience frequent apnea and variability in O2 saturations. Those previous findings contrast with the current hypothesis for the etiology of ROP and provide direct evidence for the onset of retinal neovascularization before weaning from O2 therapy. Further, we observed that VLBW infants who experience clustered (CL), consecutive apnea and desaturations appear to be more susceptible to the development of severe ROP. This enabled us to hypothesize that brief, CL episodes of hypoxia during prolonged hyperoxia would result in a more severe form of oxygen-induced retinopathy (OIR) than brief, evenly DP episodes of hypoxia.
MATERIALS AND METHODS
All experiments were approved by the Memorial Health Services Institutional Animal Care and Use Committee, Long Beach, CA. Animals were managed according to the ARVO Statement for the Use of Animals in Ophthalmic and Visual Research, the United States Department of Agriculture, the Guide for the Care and Use of Laboratory Animals, and the American Veterinary Medical Association.
Experimental design.
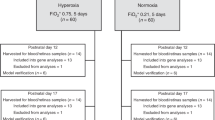
Certified infection-free, timed-pregnant Sprague Dawley rats were purchased from Charles River Laboratories (Wilmington, MA) at 19 d gestation. The animals were housed in an animal facility with a 12-h-day/12-h-night cycle and provided standard laboratory diet and water ad libitum. Within approximately 5 h of birth, newborn rat pups delivering on the same day were pooled and randomly assigned to expanded litters of 17 pups/litter. The expanded litter size was used to simulate relative postnatal malnutrition in ill VLBW infants. Rat pups raised in large litters have been shown to develop more severe abnormal neovascularization (10). One dam remained with the same litter for the entire study. Each pup was weighed and measured for linear growth (crown to rump) before experimentation. On the day of birth, or postnatal day 1 (P1), the OIR groups were placed in specialized chambers for hyperoxia/hypoxia cycling. The hyperoxia/hypoxia cycles consisted of 50% O2 followed by brief episodes of hypoxia (12% O2) for 2 min for a total of 12 cycles per day. These hypoxic episodes were spaced in one of two ways. In the DP group, the cycles were evenly spaced every 2 h throughout the day. In the CL group, three episodes of hypoxia were grouped, each 10 min apart, followed by hyperoxia to complete 6 h. These OIR models were modified from a previously validated model (5–9). Hypoxia of 12% O2 was used due to the extended time period needed to reach 10% and the desire to keep the hypoxic episodes brief. To reach 12% O2 required 2 min, but to reach 10% O2 required a total of 5 min. The O2 concentration remained at 12% for 2 min. Previous work by Werdich et al. (9) showed that hypoxia of 12.5% O2 was significant enough to cause retinal pathology. Nine groups were studied. Two groups were exposed to DP or CL hyperoxia/hypoxia cycling for 7 d from P1 to P7 (7D-O2 DP and 7D-O2 CL); two groups were exposed to DP or CL hyperoxia/hypoxia cycling for 14 d from P1 to P14 (14D-O2 DP and 14D-O2 CL); two groups were exposed to DP or CL hyperoxia/hypoxia cycling for 14 d (P1 to P14), then allowed to recover in RA until P21 (21D-O2 DP and 21D-O2 CL); and three groups of age-matched control littermates in expanded litters of 17 pups/litter, were raised in RA from P1 to P7 (7D-RA), P1 to P14 (14D-RA), or P1 to P21 (21D-RA).
Hyperoxia/hypoxia cycling.
On the day of birth (P1), all hyperoxia-exposed litters were placed with the dams into specialized O2 chambers (BioSpherix, NY) attached to an oxycycler. The oxycycler sensed O2 inside the chamber and infused nitrogen to reduce O2 and O2 to raise it. Oxygen content inside the chamber was continuously monitored and recorded on a Dell Computer. The animals remained undisturbed except during the bedding change, which occurred every 3 d, during a 50% O2 cycle, and lasted no more than 3 min. The chamber was optimized for gas efficiency and provided adequate ventilation for the animals in a controlled atmosphere. Carbon dioxide in the chamber was continuously monitored and controlled with the use of a built-in fan and soda lime. Humidity in the chamber was also continuously monitored and controlled.
Fluorescein-dextran perfusion.
To determine retinal vascular development, computer-digitized images of fluorescein-dextran stained retinas from five rats in each group were examined. The rats were anesthetized with intraperitoneal sodium pentobarbital (40 mg/kg IP) and a median sternotomy was performed. The left ventricle was perfused with 1 mL of 4% phosphate buffered formaldehyde containing 50 mg of 2 × 106 molecular weight fluorescein-dextran (Sigma Chemical Co., St. Louis, MO). The eyes were enucleated and placed in 4% paraformaldehyde for at least 2 h before removal of the retina. The retinas were flattened by making four incisions and mounted with glycerol-gelatin. The flat-mounted retinas were viewed by fluorescence microscopy and the images were saved on a computer using SPOT software (Diagnostic Instruments, Inc., Sterling Heights, MI), Olympus BH-2 microscope (McBain Instruments, Chatsworth, CA) and Dell Optiplex GX280 computer (Dell Computer Corporation, Dallas, TX). Images of the retinas were digitized at 640 × 480 pixels and 4.0× magnification.
Sample collection.
Both eyes from 12 rats in each group were enucleated and rinsed in ice-cold phosphate-buffered saline (pH 7.4) on ice. Enucleation was performed with the use of iris forceps and scissors for separation of the eyes from the surrounding connective tissue, nerves, and muscle. The vitreous fluid was aspirated using a 0.5 mL insulin syringe and placed on ice in sterile Eppendorf tubes. Vitreous fluid was pooled for a total of five samples per group. None of the vitreous fluid samples were contaminated with blood. The retinas were then excised under a dissecting microscope, placed in sterile polypropylene tubes, and frozen. To obtain enough tissue, retinas were pooled and a total of five samples were assayed per group. Each sample contained vitreous or retina from 4–5 eyes. Blood samples were collected in sterile Eppendorf tubes following decapitation, placed on ice and allowed to clot for 30 min before processing. The tubes were centrifuged at 3000 rpm for 20 min for collection of serum. Vitreous and serum samples were stored in −20°C and retinal samples were stored in −80°C until assay.
Assays.
On the day of the assay, retinas were homogenized on ice, centrifuged at 5000 rpm at 4°C for 20 min, and then filtered. VEGF and soluble VEGFR-1 (sVEGFR-1); and growth hormone (GH) and insulin-like growth factor I (IGF-I) levels in serum, undiluted vitreous fluid and retinal homogenates were assayed using commercially available sandwich immunoassay kits for rat/mouse from R & D Systems, Minneapolis, MN, and Diagnostic Systems Laboratories, Webster, TX, respectively, according to the manufacturer's protocol. Growth factor levels in the retinal homogenates were standardized using total cellular protein levels.
Total cellular protein levels.
A 10 μL portion of the retinal homogenate was used for total cellular protein levels using the Bradford method (Bio-Rad, Hercules, CA) with BSA as a standard. The protein assay was carried out on the same day as the assays for growth factors.
Statistical analysis.
One-way analysis of variance was used to determine differences among the groups for normally distributed data, and Kruskal-Wallis test was used for nonnormally distributed data following Bartlett's test for equality of variances. Post hoc analysis was performed using the Tukey and Student-Newman-Keuls tests for significance. Significance was set at p < 0.05 and data are reported as mean ± SEM, where applicable. All analyses were two-tailed and performed using SPSS (SPSS, Inc. Chicago IL).
RESULTS
Effects on growth.
Body weight was lower in both 7D oxygen-exposed groups compared with their RA air littermates with no differences in linear growth. At P14, only the CL group had a significantly lower body weight, while linear growth remained comparable. In contrast, at P21, both body weight and linear growth were lower in the CL group (Table 1). Figure 1 represents the DP and CL models used in the study.
Total VEGF.
VEGF levels (pg/mL: serum and vitreous, pg/mg protein: retina) were significantly elevated in all compartments in the CL groups compared with both the DP hypoxia groups and RA controls (Fig. 2A–C). At P7, serum VEGF in the CL group (278.1 ± 18.9) was more than twice that of the DP group (122.8 ± 9.6, p < 0.001) or RA (146.1 ± 8.9, p < 0.001), whereas in the vitreous (488.6 ± 141.5 vs. 45.3 ± 3.3, 154.7 ± 17.2, p < 0.05) and retina (137.8 ± 19.2 vs. 15.9 ± 6.7, 4.7 ± 0.8, p < 0.001) there were multiple fold increases in VEGF in the CL group. These large increases continued in the 14D groups. Serum VEGF in the CL group (172.1 ± 3.8) was 10-fold that of either the DP group (14.9 ± 1.1, p < 0.001) or RA controls (17 ± 2.5, p < 0.001) while the retina showed 20–40 fold differences (15.7 ± 1.3, 6 ± 0.8, p < 0.001). In addition, at 14 d, the DP hypoxia group showed a significant increase in the vitreous VEGF level (397.9 ± 19.7) compared with RA (235.5 ± 23.6, p < 0.05) while the CL hypoxia group showed a significant increase over both groups (864.4 ± 56, p < 0.001). After RA recovery, there was a highly significant increase in VEGF in the serum (126.8 ± 8.1 vs. 18.3 ± 1.3, 10.9 ± 1.5, p < 0.001), vitreous (229.5 ± 36.2 vs. 153.3 ± 19.4, 116.4 ± 9.3, p < 0.05), and retina (163.3 ± 31.5 vs. 27.7 ± 3.4, 12.1 ± 2.1, p < 0.01) of the CL hypoxia groups vs. both the DP group and the RA controls.
Effects of brief dispersed vs. clustered hypoxia during hyperoxia on serum (A), vitreous fluid (B), and retinal (C) VEGF protein levels. The open bar represents the room air (RA) groups; the lined bar represents the O2-dispersed group (DP); and the solid bar represents the O2-clustered group (CL). Data are expressed as mean ± SEM (n = 12 samples/group for serum; n = 5 samples/group for vitreous fluid and retina). **p < 0.01 vs. RA.
sVEGFR-1.
Figure 3A shows that after 7 d of cyclic O2 exposure, a significant increase was seen in the serum level of sVEGFR-1 in the DP group (465.4 ± 63.4) compared with both the CL group (269.6 ± 28.2, p < 0.01) and RA (243 ± 51, p < 0.01). The retinal levels were also decreased in both experimental groups (DP 380.3 ± 115.9, CL 220.2 ± 27.4) compared with RA (1370.3 ± 94.5, p < 0.001), while no differences were noted in the vitreous fluid (Figs. 3B and C). There were no significant differences in any compartments at P14 (data not shown). After RA recovery, there was a decrease in the serum sVEGFR-1 in the CL group (217.6 ± 15.8) compared with both the DP group (654 ± 90, p < 0.01) and RA (530.1 ± 51.3, p < 0.01) (Fig. 3A). At this same time, the vitreous showed a highly significant increase in the sVEGFR-1 level in the CL group (2641.4 ± 288.3) compared with the DP and control groups (1092.1 ± 331.3, 661.7 ± 210.1, p < 0.01), while a nonsignificant decrease was noted in the retina (Figs. 3B and C).
Effects of brief, dispersed (DP) vs. clustered (CL) hypoxia during hyperoxia on serum (A and D), vitreous fluid (B and E), and retinal (C and F) sVEGFR-1 protein levels at 7 and 21 d postnatal age, respectively. Data are expressed as mean ± SEM (n = 12 samples/group for serum; n = 5 samples/group for vitreous fluid and retina). **p < 0.01 vs. RA.
Insulin-like growth factor-1.
Significant decreases were seen in the serum level of IGF-1 in all the CL hypoxia groups compared with the other two groups (data not shown). In the 7D-O2 CL and 14D-O2 CL groups, the levels of IGF-1 were nearly half of that seen in either the DP hypoxic group or RA (7D-O2: 261.8 ± 26.7 vs. 455.8 ± 17.7 and 405.2 ± 32.9, p < 0.01; 14D-O2: 226.55 ± 27.6 vs. 445.5 ± 26 and 403.3 ± 21.2, p < 0.001). No significant changes were noted in the vitreous or retina (data not shown). After RA recovery, both experimental groups showed a substantial decrease in serum IGF-1 levels compared with the RA groups (Fig. 4A). The DP hypoxic group had less than half the IGF-1 level seen in the RA group (441 ± 29.8 vs. 1039.9 ± 114.8, p < 0.05) whereas the CL group showed a highly significant decrease compared with both the DP group and RA (174.6 ± 17.5, p < 0.001). No changes were noted in the vitreous fluid IGF-I levels among the groups (Fig. 4B). Retinal IGF-I levels were elevated in the CL group compared with the DP and RA groups (13.1 ± 1.3 vs. 8.2 ± 0.4 and 7.7 ± 0.6, p < 0.05) as shown in Figure 4C.
Effects of brief, dispersed (CP) vs. clustered (CL) hypoxia during hyperoxia on serum (A), vitreous fluid (B), and retinal (C) IGF-I protein levels at 21 d postnatal age. Data are expressed as mean ± SEM (n = 12 samples/group for serum; n = 5 samples/group for vitreous fluid and retina). *p < 0.05; **p < 0.01 vs. RA.
Growth hormone.
There were no significant differences in GH in the serum, vitreous, or retina among any of the groups (Table 1).
Retinal vascularization.
The RA control rats showed the normal progression of vessels extending toward the periphery and increasing capillary density, followed by remodeling of the capillary beds with pruning of the capillary tree around large vessels from day 7 (Fig. 5A) to day 14 (Fig. 5B) and day 21 (Fig. 5C). There was preservation of the avascular zone between the peripheral retina and the ciliary body. In contrast, there was evidence of abnormal vascular morphology in the hyperoxia-exposed groups. The DP 7D-O2 group showed vessel leakage and vascular tufts (Fig. 5D) and the DP 14D-O2 groups showed vascular overgrowth extending into the avascular zone (Fig. 5E). Following RA recovery, there was evidence of severe tortuosity, dilatation, and advanced neovascularization in the 21D-O2 DP group (Fig. 5F). These vessels bypassed the avascular zone and grew into the ciliary bodies. These findings of abnormal vessel morphology were more striking in the CL hypoxia group. In the CL 7D-O2 group (Fig. 5G), there was a severe delay in vascular growth with the persistence of primordial vessels, which are normally gone by 3 d of postnatal life in rats. By P14 (Fig. 5H), the vessels showed severe dilation and tortuosity with areas of hemorrhage. After RA recovery, the retinas were severely overgrown and disorganized, obliterating the avascular zone (Fig. 5I).
Fluorescein-dextran stained retinas from room air (RA) controls and oxygen-exposed rats. Retinas from RA controls at P7 (A), P14 (B), and P21 (C) show normal vasculature. Retinas from rat pups exposed to 50/12% dispersed hypoxic cycling for 7 d (D) show vascular tufts and leaky vessels (arrow). Retinas from rat pups exposed to 50/12% clustered hypoxic cycling for 7 d (G) show persistence of immature, primordial vessels (arrow). Retinas from rat pups exposed to 50/12% dispersed hypoxic cycling for 14 d (E) show vascular overgrowth, dilatation, and some tortuosity (arrow). Retinas from rat pups exposed to 50/12% clustered hypoxic cycling for 14 d (H) had severe OIR evidenced by leaky vessels, hemorrhage, and vessel dilatation (arrows). Retinas from rat pups exposed to 50/12% dispersed hypoxic cycling for 14 d with 7 d of RA recovery (F) show vascular overgrowth, dilatation, and tortuosity (arrow) consistent with “plus disease.” Retinas from rat pups exposed to 50/12% clustered hypoxic cycling for 14 d with 7 d of RA recovery (I) show leaky vessels, hemorrhage, and persistence of immature, primordial vessels (arrows). Images of the retinas were digitized at 640 × 480 pixels and 4.0× magnification.
DISCUSSION
The present study demonstrated that CL episodes of hypoxia were associated with a more severe form of OIR, thereby proving our hypothesis that brief, CL episodes of hypoxia during prolonged hyperoxia would result in a more severe form of OIR than brief, evenly DP episodes of hypoxia. The most interesting finding was the effect of CL hypoxia on VEGF protein levels, which was consistently elevated in all compartments. VEGF is a potent mitogen specific for endothelial cells and is essential for normal retinal vascular development (11,12). Previous studies have examined the effect of hypoxia on retinal VEGF expression as well as the link between VEGF upregulation and neovascularization (7,9,13–15). Work by McColm et al. (7) found that repeated fluctuations in O2 resulted in upregulation of retinal VEGF to a greater extent than a single episode. Our results are consistent with, and confirm those findings. Furthermore, our data suggest that the O2 fluctuations also contribute to VEGF upregulation such that grouping of desaturations with minimal time for recovery leads to a more exaggerated response. This may be due to decreased VEGF protein turnover during the periods of hyperoxia or may be caused by upregulation of transcription or translation of VEGF mRNA by CL hypoxia, leading to increased VEGF production. Our animal model is consistent with the reported clinical findings that VLBW infants who are clinically unstable have a higher risk of ROP. Although the exact mechanism for differences in physiologic consequences between the two OIR models remains unclear, we speculate that it may be due to differences in exposure time of the retina to hypoxia at a given time point. In the CL group, the retinas remained hypoxic for a longer period of time.
VEGF exerts its angiogenic effects through its membrane receptors, VEGFR-1 and VEGFR-2 (16). A cDNA encoding an alternatively spliced soluble form of VEGFR-1 (sVEGFR-1) binds VEGF with high affinity and inhibits VEGF-induced angiogenesis (17). Work by Aiello et al. (15) showed a 50% reduction in retinal neovascularization when sVEGFR-1-like chimeric proteins were injected into the vitreous of animals with retinal ischemia. These proteins are large and were thought to be unable to diffuse into retinal tissue, thus limiting their inhibitory effects. More recent work by Rota et al. (18) showed an even greater reduction in neovascularization (97.5%) when sVEGFR-1 was injected into the vitreous of rats with oxygen-induced injury. In the present study, retinal sVEGFR-1 levels were suppressed in both OIR models after 7 d of hyperoxia/hypoxia cycling, an effect that was not reflected in the serum or vitreous fluid. Interestingly, vitreous fluid sVEGFR-1 levels progressively increased with advancing age and were significantly higher in the CL hypoxia group reflecting elevations of VEGF. This calls into question whether VEGF regulation by endogenous sVEGFR-1 is developmentally regulated and therefore would have been permissive to the development of neovascularization at such at early point in postnatal life, much earlier than has been previously thought in the current two-phase view of ROP. In fact, the lack of an increase of sVEGFR-1 in the experimental groups is consistent with the findings of severe progressive neovascularization in all O2-exposed groups. By the time an increase in sVEGFR-1 was seen in the recovering CL hypoxia group, there would have been no effect on neovascularization since sVEGFR-1 has been shown to have no effect on preexisting retinal vessels (18). These data provide further support that the onset of OIR may occur before RA recovery.
IGF-1 is involved in normal vascular development and its deficiency has been correlated to pathologic findings in retinal vascularization (19). Low serum IGF-1 levels in VLBW preterm infants have been shown to be as strong a risk factor for ROP as gestational age and birth weight (20). This is thought to be due to the interaction between IGF-1 and VEGF. Low IGF-I levels contribute to poor vascular growth and a hypoxic maturing avascular retina, which eventually leads to increased VEGF production and neovascularization (20,21). Our data showed that IGF-1 was suppressed only in the serum, did not increase later in postnatal life, and continued to be low despite the presence of severe neovascularization. We previously showed that the ontogeny of IGF-1 in the developing retina is compartment-specific and that there is no correlation between the IGF-1 levels in the serum and in the retina (22). Thus, we believe that the low IGF-1 levels seen in the serum of the CL hypoxia group are not causative of the neovascularization since no significant changes were seen in the ocular compartment. This leads us to speculate that the low serum IGF-1 levels may be a consequence of low body weight and gestational age rather than a causal factor for ROP.
It has been suggested that GH may be of importance for angiogenesis (23,24). This is thought to be due to the effect of GH on IGF-1 with decreased GH levels leading to decreased IGF-1 synthesis (23). However, newborns are known to be in a state of GH resistance and this state may be exaggerated in ill preterm infants who are also at risk for ROP (25). In our study, severe neovascularization in all O2-exposed groups was not associated with changes in GH levels at any time or in any compartment, shedding doubt on a role for GH in OIR. The evidence of a support for our primary hypothesis is in the appearance of the retinal vasculature which demonstrated that upregulation of VEGF in response to CL hypoxia is marked and leads to characteristics similar to that seen in “plus disease.” These characteristics appear to emerge before recovery in RA. This could potentially explain the inability of supplemental O2 given during the recovery phase in the STOP-ROP trial to prevent ROP since the factors leading to neovascularization were already upregulated (26). Most previous studies have drawn conclusions based on the collection of serum data, the only media available in human studies. Since neovascularization results in the production of weak, leaky neovessels, it would be reasonable to speculate that a breakdown in the blood-ocular barrier would allow differences between the compartments to equalize. However, the present study demonstrates that this is only true for VEGF and not sVEGFR-1, IGF-I, or GH, suggesting increased VEGF production.
In summary, we have shown that clustering episodes of hypoxia results in a more severe form of OIR than DP episodes; characteristics consistent with “plus disease” emerge as early as during phase 1; endogenous sVEGFR-1 production may be age-dependent; and compartment-specific differences in sVEGFR-1, IGF-I, and GH persist in OIR. The implications of these findings are that VLBW infants who experience CL episodes of hypoxia during prolonged hyperoxia are at a higher risk for severe ROP. Because of possible compartmental-specific differences, caution is emphasized when anti-growth factor therapies are proposed for the treatment of OIR.
Abbreviations
- CL:
-
clustered
- DP:
-
dispersed
- OIR:
-
oxygen-induced retinopathy
- P:
-
postnatal age (days)
- RA:
-
room air
- ROP:
-
retinopathy of prematurity
- SPSS:
-
statistical package for social science
- sVEGFR-1:
-
soluble vascular endothelial growth factor receptor-1
- VEGFR-2:
-
vascular endothelial growth factor receptor-2
- RA:
-
room air
- VLBW:
-
very low birth weight (<1500 g)
References
Hameed B, Shyamanur K, Kotecha S, Manktelow BN, Woodruff G, Draper ES 2004 Trends in the incidence of severe retinopathy of prematurity in a geographically defined population over a 10-year period. Pediatrics 113: 1653–1657
Gibson DL, Sheps SB, Uh SH, Schechter MT, McCormick AQ 1990 Retinopathy of prematurity-induced blindness: birth weight-specific survival and the new epidemic. Pediatrics 86: 405–412
Chow LC, Wright KW, Sola A, CSMC Oxygen Administration Study Group 2003 Can changes in clinical practice decrease the incidence of severe retinopathy of prematurity in very low birth weight infants?. Pediatrics 111: 339–345
York JR, Landers S, Kirby RS, Arbogast PG, Penn JS 2004 Arterial oxygen fluctuation and retinopathy of prematurity in very-low-birth-weight infants. J Perinatol 24: 82–87
Penn JS, Tolman BL, Henry MM 1994 Oxygen-induced retinopathy in the rat: relationship of retinal nonperfusion to subsequent neovascularization. Invest Ophthalmol Vis Sci 35: 3429–3435
Penn JS, Henry MM, Tolman BL 1994 Exposure to alternating hypoxia and hyperoxia causes severe proliferative retinopathy in the newborn rat. Pediatr Res 36: 724–731
McColm JR, Geisen P, Hartnett ME 2004 VEGF isoforms and their expression after a single episode of hypoxia or repeated fluctuations between hyperoxia and hypoxia: relevance to clinical ROP. Mol Vis 10: 512–520
Penn JS, McCollum GW, Barnett JM, Werdich XQ, Koepke KA, Rajaratnam VS 2006 Angiostatic effect of penetrating ocular injury: role of pigment epithelium-derived factor. Invest Ophthalmol Vis Sci 47: 405–414
Werdich XQ, McCollum GW, Rajaratnam VS, Penn JS 2004 Variable oxygen and retinal VEGF levels: correlation with incidence and severity of pathology in a rat model of oxygen-induced retinopathy. Exp Eye Res 79: 623–630
Holmes JM, Duffner LA 1996 The effect of postnatal growth retardation on abnormal neovascularization in the oxygen-exposed neonatal rat. Curr Eye Res 15: 403–409
Stone J, Itin A, Alon T, Pe'er J, Gnessin H, Chan-Ling T, Keshet E 1995 Development of retinal vasculature is mediated by hypoxia-induced vascular endothelial growth factor (VEGF) expression by neuroglia. J Neurosci 15: 4738–4747
Ferrara N 2000 Vascular endothelial growth factor and the regulation of angiogenesis. Recent Prog Horm Res 55: 15–35
Cunningham S, McColm JR, Wade J, Sedowofia K, McIntosh N, Fleck B 2000 A novel model of retinopathy of prematurity simulating preterm oxygen variability in the rat. Invest Ophthalmol Vis Sci 41: 4275–4280
Aiello LP, Northup JM, Keyt BA, Takagi H, Iwamoto MA 1995 Hypoxic regulation of vascular endothelial growth factor in retinal cells. Arch Ophthalmol 113: 1538–1544
Aiello LP, Pierce EA, Foley ED, Takagi H, Chen H, Riddle L, Ferrara N, King GL, Smith LE 1995 Suppression of retinal neovascularization in vivo by inhibition of vascular endothelial growth factor (VEGF) using soluble VEGF-receptor chimeric proteins. Proc Natl Acad Sci USA 92: 10457–10461
Gille H, Kowalski J, Li B, LeCouter J, Moffat B, Zioncheck TF, Pelletier N, Ferrara N 2001 Analysis of biological effects and signaling properties of Flt-1 (VEGFR-1) and KDR (VEGFR-2). A reassessment using novel receptor-specific vascular endothelial growth factor mutants. J Biol Chem 276: 3222–3230
Ferrara N, Davis-Smyth T 1997 The biology of vascular endothelial growth factor. Endocr Rev 18: 4–25
Rota R, Riccioni T, Zaccarini M, Lamartina S, Gallo AD, Fusco A, Kovesdi I, Balestrazzi E, Abeni DC, Ali RR, Capogrossi MC 2004 Marked inhibition of retinal neovascularization in rats following soluble-flt-1 gene transfer. J Gene Med 6: 992–1002
Hellstrom A, Perruzzi C, Ju M, Engstrom E, Hard AL, Liu JL, Albertsson-Wikland K, Carlsson B, Niklasson A, Sjodell L, LeRoith D, Senger DR, Smith LE 2001 Low IGF-1 suppresses VEGF-survival signaling in retinal endothelial cells: direct correlation with clinical retinopathy of prematurity. Proc Natl Acad Sci USA 98: 5804–5808
Hellstrom A, Engstrom E, Hard AL, Albertsson-Wikland K, Carlsson B, Niklasson A, Lofqvist C, Svensson E, Holm S, Ewald U, Holmstrom G, Smith LE 2003 Postnatal serum insulin-like growth factor I deficiency is associated with retinopathy of prematurity and other complications of premature birth. Pediatrics 112: 1016–1020
Smith LE, Shen W, Perruzzi C, Soker S, Kinose F, Xu X, Robinson G, Driver S, Bischoff J, Zhang B, Schaeffer JM, Senger DR 1999 Regulation of vascular endothelial growth factor-dependent retinal neovascularization by insulin-like growth factor-1 receptor. Nat Med 5: 1390–1395
Modanlou HD, Gharraee Z, Hasan J, Waltzman J, Nageotte S, Beharry KD 2006 Ontogeny of VEGF, IGF-1 and GH in neonatal rat serum, vitreous fluid, and retina from birth to weaning. Invest Ophthalmol Vis Sci 47: 738–744
Smith LE, Kopchick JJ, Chen W, Knapp J, Kinose F, Daley D, Foley E, Smith RG, Schaeffer JM 1997 Essential role of growth hormone in ischemia-induced retinal neovascularization. Science 276: 1706–1709
Hikino S, Ihara K, Yamamoto J, Takahata Y, Nakayama H, Kinukawa N, Narazaki Y, Hara T 2001 Physical growth and retinopathy in preterm infants: involvement of IGF-I and GH. Pediatr Res 50: 732–736
Radetti G, Bozzola M, Paganini C, Valentini R, Gentili L, Tettoni K, Tato L 1997 Growth hormone bioactivity and levels of growth hormone, growth hormone-binding protein, insulin-like growth factor I, and insulin-like growth factor-binding proteins in premature and full-term newborns during the first month of life. Arch Pediatr Adolesc Med 151: 170–175
STOP-ROP Multicenter Study Group 2000 Supplemental therapeutic oxygen for prethreshold retinopathy of prematurity (STOP-ROP), a randomized, controlled trial. I: primary outcomes. Pediatrics 105: 295–310
Author information
Authors and Affiliations
Additional information
This work was supported by a grant from the Memorial Medical Center Foundation, Long Beach, CA.This paper was presented, in part, at the 2007 annual Western Society for Pediatric Research, Carmel, CA and the 2007 annual American Pediatric Society-Society for Pediatric Research meeting, Toronto, Canada.
Rights and permissions
About this article
Cite this article
Coleman, R., Beharry, K., Brock, R. et al. Effects of Brief, Clustered Versus Dispersed Hypoxic Episodes on Systemic and Ocular Growth Factors in a Rat Model of Oxygen-Induced Retinopathy. Pediatr Res 64, 50–55 (2008). https://doi.org/10.1203/PDR.0b013e31817307ac
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e31817307ac
This article is cited by
-
Neonatal intermittent hypoxia, fish oil, and/or antioxidant supplementation on gut microbiota in neonatal rats
Pediatric Research (2022)
-
Renal biomarkers of acute kidney injury in response to increasing intermittent hypoxia episodes in the neonatal rat
BMC Nephrology (2021)
-
Comparison of coenzyme Q10 or fish oil for prevention of intermittent hypoxia-induced oxidative injury in neonatal rat lungs
Respiratory Research (2021)
-
Pharmacologic synergism of ocular ketorolac and systemic caffeine citrate in rat oxygen-induced retinopathy
Pediatric Research (2016)
-
The relationship between patterns of intermittent hypoxia and retinopathy of prematurity in preterm infants
Pediatric Research (2012)