Abstract
Intragastric fat digestion was investigated by analyzing the products of lipolysis and the gastric lipase (HGL) levels of premature infants fed with a formula enriched with medium chain triglycerides (MCT) and those of infants fed with human milk. Infants were fed using a gastric tube and the gastric contents were aspirated twice a day for 5 d, before and at various times after gavage feeding. HGL levels were measured using the pHstat technique. After extraction, lipids were separated and quantified using thin-layer chromatography coupled to a flame ionization detector. Fatty acid methyl esters were analyzed by gas chromatography. HGL concentration increased during digestion, reaching 77.4 ± 43.1 μg/mL (around 75% of those recorded in adults). Mean HGL output was 115 ± 43 μg for 3 h and the overall intragastric lipolysis was 6.1 ± 2.6%. Although the formula was enriched with octanoic and decanoic acid, the main fatty acids released in the stomach were palmitic (C16:0, 17.03 ± 0.23% wt/wt) and oleic (C18:1 n-9, 28.23 ± 1.26% wt/wt) acid. Similar results were obtained with infants fed with human milk. MCT supplementation has no quantitative or qualitative effects on the intragastric lipolysis, which is not higher in premature infant than in adults.
Similar content being viewed by others
Main
It is generally recognized that the exocrine pancreas has a poor secretory capacity during the neonatal period in comparison with adults (1,2). The pancreatic lipase contents of the duodenum are not increased by the ingestion of a meal, and the pool of bile salts is very low at birth (3,4). Some mechanisms probably develop to compensate for the low contribution of the pancreatic enzymes to fat digestion in the infant. For instance, the contribution of BSSL present in the mother's milk and HGL to fat digestion is thought to be higher in newborn infants than at later stages in development (5). It has been established that HGL appears in the fundic mucosa of human fetus at around the 11 wk of gestation, and that its level then gradually increases until the same level as that recorded in adults is reached at around the third month of life (6). Gastric lipolysis is essential to newborns fed with human milk, because the membrane of milk fat globules prevents the TG from being hydrolyzed by pancreatic lipase and BSSL. The fatty acids released by HGL play an important role in triggering the activity of pancreatic lipase by changing the “quality” of the lipid-water interface (7). Although the qualitative role of HGL has been clearly established, the quantitative contribution of this lipase to fat digestion has not yet been exactly determined. Some authors did not find any significant differences in HGL levels between premature infants and adults (8,9).
In adults, intragastric lipolysis by HGL can release 10–25% of the fatty acids present in ingested TG (10,11). HGL is still active in the duodenal contents (10) and has all the characteristics required to act both in the stomach and the intestine: it is stable in a wide pH range (1.5–7) (12) and it is not inhibited by bile salts (11). Several studies have suggested that HGL might play a more important role in patients with exocrine pancreatic insufficiency (13,14). It was recently confirmed that the HGL output increased 3- to 4-fold in adults with chronic pancreatitis (15).
It has been assumed for many years that HGL was specific of short- and medium-chain fatty acids (MCFA) and might therefore play a major role in the efficacy of infant formulas enriched with MCT. These formulas contain 20–40% wt/wt MCFA versus total fat, whereas human milk contains only around 10% MCFA. One of the theoretical reasons for MCT enrichment is related to the better absorption of MCFA, which is less dependent on bile salts than that of LCFA. In addition, MCFA can be directly absorbed through the gastric mucosa and transported via the portal vein. It was reported that these formulas improve the weight gain in comparison with human milk (16), but it was not actually proved that the weight gain was due to the MCT supplementation (16,17).
The aim of the present study was to determine the qualitative and quantitative contributions of HGL to intragastric lipolysis in the premature infant, focusing in particular on the digestion of a MCT-enriched infant formula.
METHODS
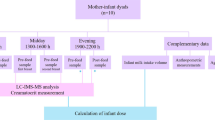
Premature infants and clinical protocol.
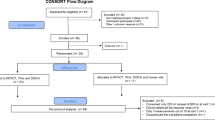
Premature infants were included in the study after the clinical protocol entitled “Lipolyse gastrique chez le nouveau-né premature” was accepted by the ethical committee of Marseille Medicine University (CCPPRB 2), France, on January 9, 2004, and their parents had given informed written consent. Recruitment of patients allowed the enrollment of 11 subjects, most of them (n = 9) being fed with an infant formula (PreGallia, Laboratoire Gallia, Villefranche sur Saone, France). Only two newborns were fed with human milk, precluding any statistical comparisons between the two groups.
Premature infants were fed every 3 h with a gastric tube placed before each meal. In each experiment (i.e. one per day for 5 d), the total gastric contents were aspirated twice, just before gavage feeding (t = 0) and again at a given time after the end of the gavage (15, 30, 60, 90, 120, or 180 min). When the second aspiration occurred before 180 min, the same volume of milk or infant formula was given a second time to the baby. Using this procedure, it was possible to measure the variations with time in gastric volume, pH, HGL activity/concentration, lipolysis product concentration and lipolysis level.
Handling of samples.
One-milliliter gastric samples were mixed with 1 mL glycerol and 40 μL of protease inhibitors [1 pellet of Complete inhibitor mix (Roche Molecular Biochemicals, Indianapolis, IN) in 2 mL purified water], and were stored at –20°C.
Lipase activity measurements.
HGL activities were measured using the pHstat technique and tributyrin substrate (10). The specific activity of BSSL (45 U/mg of enzyme) is much lower (3.4%) than that of HGL (1300 U/mg of pure enzyme) under these assay conditions. Lipase activity was expressed in international units (1 U = 1 μmol of butyric acid released per minute). Using the known specific activity of HGL, it was possible to deduce the active HGL concentration (μg/mL) from the enzyme activity measurements (U/mL).
Calculation of the GE rate of milk.
The GE rate of milk was estimated from the amounts of total fatty acids remaining in the stomach, which were used as meal markers, assuming the emulsified milk lipids and the water phase to be simultaneously emptied. At a given time, the GE rate (%) was calculated as follows:
Math

where TG0 are the amounts (mmol) of TG initially present in the ingested milk or infant formula, and TGt, DGt, MGt, and FFAt are the amounts of residual TG, diglycerides, monoglycerides, and FFA present in the gastric contents at time t.
Calculation of residual meal volume (VR) in gastric contents.
Math

where V0 is the initial meal volume.
Calculation of pyloric outputs.
At a given time (t), the amounts of HGL present in the stomach were calculated as follows:
Math

where Vg(t) is the gastric content volume and [HGLg](t) is the concentration of HGL in gastric contents. The HGL pyloric output during the time period [t1, t2] was calculated from the mean HGL amounts in gastric contents and the fraction of GE during this time period as follows:
Math

The overall pyloric output during the whole digestion period was obtained by summing up the pyloric outputs calculated for each time period (0–15, 15–30, 30–60, 60–90, 90–120, and 120–180 min). Similar calculations were performed to estimate the pyloric outputs of each lipolysis product.
Lipid extraction and quantitative analysis of TG, DG, MG, and FFA.
Lipid extraction from 1-mL gastric sample was performed immediately after collection with 5 mL chloroform-methanol (2:1 vol/vol) and quantitative analysis of TG, DG, MG, and FFA was performed using thin-layer chromatography (TLC) coupled to a flame ionization detector as previously described (15). The mass detection data were converted into mmoles using the average molar masses (g/mol) calculated from the fatty acid composition of either PreGallia infant formula (TG: 776; DG: 548; MG: 320; FFA: 246) or human milk (TG: 832; DG: 585; MG: 339; FFA: 265).
Quantitative and qualitative analysis of FFA by gas chromatography.
TG, DG, MG, and FFA were separated using preparative TLC after spotting 500 μL of the lipid extracts onto a silica plate (Merck, Darmstadt, Germany) using an Linomat IV (Camag. Muttenz, Switzerland) automated sample spotter. After separation and identification of each class of lipids, each lipid band was recovered separately by scraping the silica, and the lipids were extracted once with 2–3 mL of heptane-diethyl ether 55-45 vol/vol, and then twice with 2–3 mL of acetone. The total organic phases were pooled and filtered and the solvent was evaporated under a nitrogen flow. Fatty acids from each sample were transformed into methyl esters (FAME) and analyzed by gas chromatography as previously described (18).
Calculation of lipolysis levels.
At a given time and a given molar composition of lipids (TG, DG, MG, FFA) present in the gastric contents, the instantaneous lipolysis level can be estimated from the percentage level of FFA versus total acyl chains present in residual glycerides and FFA as follows:
Math

The overall gastric lipolysis occurring during 3 h in the stomach was calculated from the sum of the pyloric lipolysis product outputs and the residual lipolysis products remaining in the stomach according to (10).
RESULTS
Premature infant population.
The nine premature infants fed with PreGallia infant formula were born at 29 + 1 wk (range, 27–31 wk) and their mean weight at birth was 1525 ± 546 g. At the beginning of the study, their mean age was 34.3 ± 1.8 wk and their mean weight was 1924 ± 284 g. The two premature infants fed with human milk were born at 32 + 4 and 32 + 5 wk, and their weight at birth was 1730 and 1770 g, respectively. They were 34 + 4 and 34 + 3 wk old and they weighed 1850 and 1770 g, respectively, at the beginning of the study.
Human milk, infant formula, lipid contents, and fat intake during a meal.
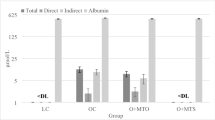
The human milk used here contained 20.5 ± 4.9 g/L TG. At each gavage, newborns were fed with 40 mL milk containing 0.82 ± 0.2 g TG. The five main fatty acids present were lauric (C12:0, 9.08 ± 1.90% wt/wt), myristic (C14:0, 10.25 ± 2.06% wt/wt), palmitic (C16:0, 22.77 ± 1.31% wt/wt), oleic (C18:1 n-9, 26.95 ± 2.03% wt/wt), and linoleic (C18:2 n-6, 15.27 ± 0.38% wt/wt) acid (Fig. 1A).
The PreGallia formula contained 34.5 ± 1.4 g/L TG, which were enriched with 25% wt/wt MCT with respect to the total TG. Infants were fed with 43 ± 8 mL formula containing 1.50 ± 0.33 g TG. The five main fatty acids present were caprylic (C8:0, 12.73 ± 1.00% wt/wt), capric (C10:0, 11.35 ± 0.76% wt/wt), palmitic (C16:0, 17.97 ± 0.40% wt/wt), oleic (C18:1 n-9, 22.67 ± 0.57% wt/wt), and linoleic (C18:2 n-6, 18.69 ± 0.51% wt/wt) acid (Fig. 1B).
Low amounts of omega-3 α-linolenic (C18:3 n-3), eicosapentaenoic (EPA, C20:5 n-3), and docosahexanoic (DHA, C22:6 n-3)) acids were detected in both human milk and the PreGallia infant formula (Fig. 1).
pH Levels of gastric contents.
After ingestion of the PreGallia formula, the pH levels of gastric contents decreased regularly from pH 7.0 to pH 3.35 ± 0.87 (1.67–4.80) after 180 min (Fig. 2). Similar changes in gastric pH levels were found to occur in the case of human milk (Fig. 2).
Gastric content volume and gastric emptying.
Changes with time in the gastric content volume were determined by aspirating the gastric contents at various times of the milk digestion from 0 to 180 min (Fig. 3). The mean half GE time was found to be 17 ± 5 min using total fatty acids as markers. The difference between residual meal and total gastric content volumes showed that the contribution of the gastric secretion was significant: 32%, 28%, and 43% vol/vol at t = 30, 60, and 90, respectively.
HGL concentrations.
HGL concentration increased during digestion (Fig. 4), reaching maximum levels amounting to around 75% of the maximum levels recorded in healthy adults (77.4 ± 43.1 versus 100–120 μg/mL) at t = 180 min.
The total amounts of HGL secreted (115 ± 43 μg) during the digestion of PreGallia formula were estimated from HGL pyloric output (89 ± 21 μg) and residual amounts of HGL present in the gastric contents at t = 180 min (49 ± 44 μg). The total amounts of HGL secreted during the digestion of the mother's milk with which two infants were fed were 100 and 175 μg.
Intragastric lipolysis. With the PreGallia formula, the instantaneous rates of lipolysis in gastric contents increased fast during the first 15–30 min of digestion and then more slowly, reaching a maximum value of 18 ± 4% in residual gastric contents after 180 min (Fig. 5). The rates of lipolysis measured in two experiments performed with the mother's milk were not significantly different and reached maximum values of 23.0% and 18.2%, respectively. The overall lipolysis that occurred in the stomach during 180 min was calculated from the sum of the pyloric output and the residual gastric contents of lipolysis products and was found to be 6.1 ± 2.6%. The total rates of intragastric lipolysis measured with the two newborn infants fed with mother's milk were slightly higher (10.3 and 11.2%, respectively), possibly due to the presence of active BSSL in maternal milk. BSSL cannot hydrolyze native milk fat globules on its own, but a low rate of hydrolysis by HGL is known to trigger lipolysis by BSSL (5). Another explanation may be that milk fat globules in mother's milk are better substrates than those present in the formula due to different physical properties.
Qualitative analysis of lipolysis products.
Gas chromatography analysis of FAME was performed to determine the fatty acid composition of the various lipid species present in the gastric contents when the rates of lipolysis reached significant levels (16.7 ± 1.6% with PreGallia and 19.1 ± 4.7% with human milk), during the 90–180 min time period. Although the PreGallia infant formula was enriched with octanoic and decanoic acid (Fig. 1), the main fatty acids released in the stomach were palmitic (C16:0, 17.03 ± 0.23% wt/wt) and oleic (C18:1 n-9, 28.23 ± 1.26% wt/wt) acid (Fig. 6B). As shown in Figure 6A, similar results were obtained with newborns fed with human milk (C16:0, 24.78 ± 6.15% wt/wt; C18:1 n-9, 27.14 ± 3.30% wt/wt). Interestingly, the proportion of free caprylic acid (C8:0) released from the infant formula was not much higher than that obtained with human milk (5.52 ± 1.18% wt/wt versus 3.48 ± 1.53% wt/wt, Fig. 6, A and B). Since the proportions of C8:0 and C10:0 present in FFA might have been underestimated due to inefficient MCFA extraction or the direct absorption of these FFA in the stomach, we analyzed the changes in the C8:0 and C10:0 levels occurring in the other lipid species. In comparison with the FFA composition of the TG initially present in the infant formula (TG0), it can be seen from Figure 6 B that the proportions of C8:0 and C10:0 decreased in the residual TG but remained similar in DG and MG, which confirms that most of the MCFA remained esterified and were not released by HGL.
DISCUSSION
Gastric pH variations, gastric secretion, and consequences for determining GE rates in premature infants.
The pH levels of the infants' gastric contents decreased after ingestion of the meal as the result of gastric acid secretion, reaching a minimum pH value of 3.35 ± 0.87 under fasting conditions. This value is similar to those reported in previous studies on newborns (8,19). These pH values suggest either a high buffering capacity of the meal or that the gastric acid secretion levels are not very high in premature infants and contribute very little to the overall volume of the gastric contents during the digestion period. This assumption was adopted in some previous studies in which GE was calculated from the changes in total gastric volume with time. A half-emptying time of around 30 min was thus obtained in experiments with various milks (8,20). Using total gastric volume as the sole basis, the mean half-emptying time was found to be around 25 min in our experiments. The GE rate was also calculated, however, using the total milk fatty acids as meal marker. Although TG can be converted into lipolysis products in the stomach, fatty acids will be either associated with residual TG, DG, and MG or FFA. Only short- and medium-chain FFA can be absorbed in the stomach, but since the overall gastric lipolysis levels are low in the stomach, the possibility that a loss of mass may have occurred due to the absorption of these FFA in the stomach can be neglected. Moreover, the results of FAME analysis showed that significant amounts of MCFA released into the stomach were recovered from the FFA fraction (Fig. 6). Based on the assumption that the decrease with time in the global mass of the fatty acids present in the stomach was due to GE, a mean half-emptying time of 17 ± 5 min was obtained. This value was lower than that given by the overall change in gastric volume. These results indicate that the contribution of gastric secretion should not be overlooked in premature infants.
HGL secretion in premature infants and gastric lipolysis.
High rates of HGL secretion were expected to occur in premature infants because of these infants' relatively low pancreatic enzyme secretion, but their HGL levels were actually found to be lower than in adults. Other authors using a different lipase assay did not find any significant differences between HGL levels of premature infants and adults (8,9). As previously observed by Fredrikzon et al. (19), HGL concentration in gastric contents was found here to increase with time after milk ingestion. During the whole digestion period, the HGL mass output (115 ± 43 μg) was 100- to 200-fold lower than in healthy adults (11).
The newborns' intragastric lipolysis levels were found to be similar to those recorded in adults (11). The overall rate of intragastric lipolysis observed with the infant formula (6.1 ± 2.6%) during the whole digestion period was also found to be in the same range as that recorded in adults fed with a mixed liquid-solid test meal [9.3 ± 6.3%, (21); 7.3 ± 5.9%, (15)].
Similar release of MCFA upon lipolysis of MCT-enriched infant formula and human milk.
MCFA were expected to be among the main fatty acids released from the PreGallia infant formula into the stomach. The infant formula tested here is obtained by mixing MCT (25% wt/wt) with other types of TG mainly composed of LCFA esterified at the various glycerol positions. MCT are made from tropical oils such as palm kernel and coconut oils, which contain large amounts of caprylic (C8:0) and capric (C10:0) acids esterified at the various glycerol positions. This distribution of MCFA and the high stereospecificity of gastric lipase (70–90%) for the hydrolysis of the ester bound at the sn-3 position of TG (22) probably explain why all the MCFA in the infant formula are not directly accessible to HGL and why C8:0 and C10:0 accounted for only 7.86 ± 2.55% of the FFA released when the rate of lipolysis reached 16.7 ± 1.6%. In human milk TG, MCFA are less abundant (C8:0 + C10:0 = 2.17 ± 0.31% versus 24.08 ± 1.76% wt/wt in infant formula) but they mainly occur at the sn-3 glycerol position. As a result, C8:0 and C10:0 accounted for 4.08 ± 1.59% of the FFA released when the rate of lipolysis reached 19.1 ± 4.7%. Enriching infant formula with MCT therefore has no noteworthy effects on the release of MCFA in the stomach, since fatty acid distributions in the TG of human milk and infant formula differ. These different stereospecific TG structures and fatty acid profiles have been analyzed in a recent article by Straarup et al. (23).
LCFA are the main FFA released in the stomach.
FAME analysis showed that palmitic (C16:0) and oleic (C18:1 n-9) acid were the main FFA released in the stomach by HGL, both in infants fed with human milk and those fed with the MCT-enriched infant formula. Although a similar finding was also made in some previous studies after 30 min of digestion (24,25), these results are in contradiction with the generally held idea that HGL or other preduodenal lipases preferentially hydrolyze ester bonds with short acyl chains. This apparent specificity was deduced from early experiments in which milk was used as a substrate for lingual or gastric lipase. As mentioned previously, these lipases display a high stereospecificity for the hydrolysis of ester bonds at the sn-3 position of glycerol. Because short- and medium-chain fatty acids mainly occur at this position in milk TG (26,27), they were found to be the first fatty acid released during digestion (24,25). However, oleic acid is the main fatty acid occurring in the sn-3 position in milk TG (26,27) and it is therefore not surprising that this fatty acid is the FFA that is the most abundantly released into the stomach when the rates of lipolysis are increasing. A more surprising finding was the fact that oleic acid is also the main fatty acid released from MCT-enriched infant formula. As mentioned previously, this can be explained, however, by the distribution of the fatty acids present in TG and the high stereospecificity of HGL.
Our results might seem to be contradictory to those obtained in earlier studies on milk fat digestion in rats, showing that MCFA are the main fatty acids released into the stomach by lingual lipase (28,29). Rat milk naturally contains much higher levels of MCFA than human milk (35% wt/wt C8:0–C12:0) and these MCFA mostly occur at the sn-3 position in rat milk TG. This is not so in the case of MCT-enriched infant formulas.
CONCLUSION
MCT supplementation of infant formula has no quantitative or qualitative effects on intragastric lipolysis, which is not higher in premature infant than in adults. The most important part of dietary TG digestion occurs, however, in the small intestine, where MCT might induce differences in residual glyceride lipolysis and fat absorption. We investigated intragastric lipolysis here using the tube that is normally used to feed newborns, and it is not possible to investigate duodenal lipolysis in the same way. It is therefore difficult to establish the contribution to lipolysis of the various lipases present in the intestine and their respective activities toward MCT.
The fact that HGL mainly releases LCFA in the stomach is probably essential for pancreatic secretion to occur, even in very low levels, and for pancreatic lipase to subsequently act. LCFA, particularly oleic acid, are known to trigger the secretion of cholecystokinin (CCK), which in turns triggers exocrine pancreatic secretion (30). Because the cells producing CCK are located in the upper part of the duodenum, the first fatty acids released by HGL are probably important factors triggering CCK release. Moreover, the LCFA released by HGL trigger the lipolytic activity of pancreatic lipase on milk fat globules, which are not a good substrate for the latter lipase alone (7). The release of long-chain FFA by HGL in the stomach therefore seems to be a physiologic prerequisite for complete digestion to occur. Fortunately, the enrichment of infant formulas with MCT does not seem to impair this physiologic process.
Abbreviations
- BSSL:
-
bile salt-stimulated lipase
- C16:0:
-
palmitic acid
- C18:1:
-
oleic acid
- CCK:
-
cholecystokinin
- DG:
-
diglyceride
- FAME:
-
fatty acid methyl ester
- GE:
-
gastric emptying
- HGL:
-
human gastric lipase
- LCFA:
-
long-chain fatty acid
- MCFA:
-
medium-chain fatty acid
- MCT:
-
medium-chain triglyceride
- MG:
-
monoglyceride
- TG:
-
triglyceride
References
Zoppi G, Andreotti G, Pajno-Ferrara F, Njai DM, Gaburro D 1972 Exocrine pancreas function in premature and full term neonates. Pediatr Res 6: 880–886
Fredrikzon B, Olivecrona T 1978 Decrease of lipase and esterase activities in intestinal contents of newborn infants during test meals. Pediatr Res 12: 631–634
Watkins JB, Ingall D, Szczepanik P, Klein PD, Lester R 1973 Bile-salt metabolism in the newborn. Measurement of pool size and synthesis by stable isotope technic. N Engl J Med 288: 431–434
Murphy GM, Signer E 1974 Bile acid metabolism in infants and children. Gut 15: 151–163
Bernback S, Blackberg L, Hernell O 1990 The complete digestion of human milk triacylglycerol in vitro requires gastric lipase, pancreatic colipase-dependent lipase, and bile salt-stimulated lipase. J Clin Invest 85: 1221–1226
Sarles J, Moreau H, Verger R 1992 Human gastric lipase: ontogeny and variations in children. Acta Paediatr 81: 511–513
Bernbäck S, Bläckberg L, Hernell O 1989 Fatty acids generated by gastric lipase promote human milk triacylglycerol digestion by pancreatic colipase-dependent lipase. Biochim Biophys Acta 1001: 286–291
Armand M, Hamosh M, Mehta NR, Angelus PA, Philpott JR, Henderson TR, Dwyer NK, Lairon D, Hamosh P 1996 Effect of human milk or formula on gastric function and fat digestion in the premature infant. Pediatr Res 40: 429–437
Armand M, Hamosh M, Dipalma JS, Gallagher J, Benjamin SB, Philpott JR, Lairon D, Hamosh P 1995 Dietary fat modulates gastric lipase activity in healthy humans. Am J Clin Nutr 62: 74–80
Carrière F, Barrowman JA, Verger R, Laugier R 1993 Secretion and contribution to lipolysis of gastric and pancreatic lipases during a test meal in humans. Gastroenterology 105: 876–888
Lengsfeld H, Beaumier-Gallon G, Chahinian H, De Caro A, Verger R, Laugier R, Carrière F 2004 Physiology of gastrointestinal lipolysis and therapeutical use of lipases and digestive lipase inhibitors. In: Müller G, Petry S (eds) Lipases and Phospholipases in Drug Development. Wiley, Weinheim, 195–229.
Ville E, Carriere F, Renou C, Laugier R 2002 Physiological study of pH stability and sensitivity to pepsin of human gastric lipase. Digestion 65: 73–81
Roulet M, Weber AM, Paradis Y, Roy CC, Chartraud L, Lasalle R, Morin CL 1980 Gastric emptying and lingual lipase activity in cystic fibrosis. Pediatr Res 14: 1360–1362
Moreau J, Bouisson M, Balas D, Ravaud A, Stupnik S, Buscail L, Vaysse N, Ribet A 1990 Gastric lipase in alcoholic pancreatitis. Comparison of secretive profiles following pentagastrin stimulation in normal adults and patients with pancreatic insufficiency. Gastroenterology 99: 175–180
Carrière F, Grandval P, Renou C, Palomba A, Priéri F, Giallo J, Henniges F, Sander-Struckmeier S, Laugier R 2005 Quantitative study of digestive enzyme secretion and gastrointestinal lipolysis in chronic pancreatitis. Clin Gastroenterol Hepatol 3: 28–38
Schanler RJ, Shulman RJ, Lau C 1999 Feeding strategies for premature infants: beneficial outcomes of feeding fortified human milk versus preterm formula. Pediatrics 103: 1150–1157
Hamosh M, Bitman J, Liao TH, Mehta NR, Buczek RJ, Wood DL, Grylack LJ, Hamosh P 1989 Gastric lipolysis and fat absorption in preterm infants: effect of medium-chain triglyceride or long-chain triglyceride-containing formulas. Pediatrics 83: 86–92
Villeneuve P, Pina M, Montet D, Graille J 1995 Determination of lipase specificities through the use of chiral triglycerides and their racemics. Chem Phys Lipids 76: 109–113
Fredrikzon B, Hernell O 1977 Role of feeding on lipase activity in gastric contents. Acta Paediatr Scand 66: 479–484
Siegel M, Lebenthal E, Topper W, Krantz B, Li PK 1982 Gastric emptying in prematures of isocaloric feedings with differing osmolalities. Pediatr Res 16: 141–147
Carriere F, Renou C, Ransac S, Lopez V, De Caro J, Ferrato F, De Caro A, Fleury A, Sanwald-Ducray P, Lengsfeld H, Beglinger C, Hadvary P, Verger R, Laugier R 2001 Inhibition of gastrointestinal lipolysis by Orlistat during digestion of test meals in healthy volunteers. Am J Physiol Gastrointest Liver Physiol 281: G16–G28
Carrière F, Rogalska E, Cudrey C, Ferrato F, Laugier R, Verger R 1997 In vivo and in vitro studies on the stereoselective hydrolysis of tri- and diglycerides by gastric and pancreatic lipases. Bioorg Med Chem 5: 429–435
Straarup EM, Lauritzen L, Faerk J, Hoy Deceased CE, Michaelsen KF 2006 The stereospecific triacylglycerol structures and fatty acid profiles of human milk and infant formulas. J Pediatr Gastroenterol Nutr 42: 293–299
Patton JS, Rigler MW, Liao H, Hamosh P, Hamosh M 1982 Hydrolysis of triacylglycerol emulsions by lingual lipase. A microscopic study. Biochim Biophys Acta 712: 400–407
Hamosh M, Bitman J, Liao T, Mehta NR, Buczek RJ, Wood DL, Grylack LJ, Hamosh P 1989 Gastric lipolysis and fat absorption in preterm infants: effect of medium chain triglyceride or long chain triglyceride containing formulas. Pediatrics 83: 86–92
Myher JJ, Kuksis A, Steiner G 1984 Milk fat structure of a patient with type 1 hyperlipidemia. Lipids 19: 673–682
Winter CH, Hoving EB, Muskiet FA 1993 Fatty acid composition of human milk triglyceride species. Possible consequences for optimal structures of infant formula triglycerides. J Chromatogr 616: 9–24
Staggers JE, Fernando-Warnakulasuriya GJ, Wells MA 1981 Studies on fat digestion, absorption, and transport in the suckling rat. II. Triacylglycerols: molecular species, stereospecific analysis, and specificity of hydrolysis by lingual lipase. J Lipid Res 22: 675–679
Fernando-Warnakulasuriya GJ, Staggers JE, Frost SC, Wells MA 1981 Studies on fat digestion, absorption, and transport in the suckling rat. I. Fatty acid composition and concentrations of major lipid components. J Lipid Res 22: 668–674
Hildebrand P, Petrig C, Burckhardt B, Ketterer S, Lengsfeld H, Fleury A, Hadvary P, Beglinger C 1998 Hydrolysis of dietary fat by pancreatic lipase stimulates cholecystokinin release. Gastroenterology 114: 123–129
Acknowledgements
The authors thank Nathalie Barouh and Bruno Barrea (CIRAD, Montpellier, France) for their technical assistance.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Roman, C., Carriere, F., Villeneuve, P. et al. Quantitative and Qualitative Study of Gastric Lipolysis in Premature Infants: Do MCT-Enriched Infant Formulas Improve Fat Digestion?. Pediatr Res 61, 83–88 (2007). https://doi.org/10.1203/01.pdr.0000250199.24107.fb
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.pdr.0000250199.24107.fb
This article is cited by
-
Fatty acid composition and phospholipid types used in infant formulas modifies the establishment of human gut bacteria in germ-free mice
Scientific Reports (2017)
-
The impact of lactoferrin with different levels of metal saturation on the intestinal epithelial barrier function and mucosal inflammation
BioMetals (2016)
-
Pancreatic lipase–related protein 2 digests fats in human milk and formula in concert with gastric lipase and carboxyl ester lipase
Pediatric Research (2013)
-
Digested formula but not digested fresh human milk causes death of intestinal cells in vitro: implications for necrotizing enterocolitis
Pediatric Research (2012)
-
Development of the Digestive System—Experimental Challenges and Approaches of Infant Lipid Digestion
Food Digestion (2012)