Abstract
Several data indicate a connection between Chlamydophila pneumoniae infection and asthma. Although C. pneumoniae is a common cause of infection, not all infected patients develop asthma. This suggests that certain individuals may be genetically predisposed to the chronic effects of C. pneumoniae infection on airway functions. We investigated the possible modifying effect of different polymorphisms on C. pneumoniae infection and on the susceptibility to asthma in 318 children, among those 144 had asthma and 174 had no asthmatic symptoms. C. pneumoniae–specific antibodies were measured by ELISA. Tumor necrosis factor-α (TNFα), monocyte chemoattractant protein-1 (MCP-1), and RANTES (regulated on activation normal T cell expressed and secreted) genotypes were determined by PCR–restriction fragment length polymorphism (RFLP). There were no significant differences in the percentage of children positive for C. pneumoniae–specific antibodies between cases and controls. None of the genotypes was associated with altered susceptibility to C. pneumoniae infection. Among asthmatic children carrying the TNFα –308A allele, there were significantly more patients positive for C. pneumoniae–specific IgG, than among control children carrying the same allele (20.1% versus 9.2% of asthmatic versus control children, respectively; p = 0.002; odds ratio = 3.52 (1.52–7.53); p = 0.005). This study indicates the possible roles of polymorphisms in the immune system in the susceptibility to asthma in children infected with C. pneumoniae.
Similar content being viewed by others
Main
Asthma is a chronic disease of the airways characterized by increased bronchial responsiveness to a variety of stimuli. Previous studies suggest that asthma is a multifactorial disease influenced by genetic and environmental factors (1).
Chlamydophila pneumoniae is a common respiratory pathogen, and, although many infections are believed to be asymptomatic, a growing body of evidence implicates an association between C. pneumoniae infection and asthma in some individuals (2,3). It has been estimated that most people have two or three C pneumoniae infections during their lifetime (4), which raises the question, why do some experience asthmatic symptoms and others not? As several data indicate, genetic factors must play a role in the susceptibility to the disease and influence the lower respiratory response to C. pneumoniae infection.
TNFα is a proinflammatory cytokine that is found in increased concentrations in asthmatic airways (5). The large and stable interindividual differences in TNFα production indicate a genetic background. Wilson et al. (6) raised considerable interest with their report that the –308A allele in the promoter region is transcribed in vitro at seven times the rate of the −308G allele.
MCP-1 (or CCL2) may play a significant role in asthma because of its ability to induce mast cell activation and leukotriene C4 release into the airway, which directly induces airway hyperresponsiveness (7). A biallelic A/G polymorphism in the MCP-1 distal gene regulatory region at position −2518 has been found that affects the level of MCP-1 expression in response to an inflammatory stimulus (8).
RANTES, or CCL5, is one of the most extensively studied chemokines in allergic and infectious diseases (9). A polymorphism in the RANTES promoter region (–403 G/A) have been found affecting the transcription of the RANTES gene (10).
C. pneumoniae has been shown to induce TNFα, MCP-1, and RANTES expression in various systems, and, conversely, several data indicate that these molecules influence the host defense against the bacterium (11–13). Given this reciprocal interaction, and the roles of C. pneumoniae, TNFα, MCP-1, and RANTES in asthma, it might be hypothesized that polymorphisms, which influence the level of these molecules, might have an effect on the infection and/or the susceptibility to asthma in patients infected with C pneumonia. To test this hypothesis, we compared the prevalence of different infection status of children with different genotypes and investigated the role of C. pneumoniae infection in children with asthma comparing them with healthy controls and studied the modifying effect of these polymorphisms on the susceptibility to the disease.
METHODS
Subjects.
The asthmatic children attended the Allergic Outpatient Consultation of the Budai Children's Hospital. All the asthmatic children had specialist physician–diagnosed asthma with the following characteristics: 1) recurrent breathlessness and expiratory dyspnea requiring treatment; 2) physician diagnosed wheeze; and 3) reversibility of the wheezing and dyspnea by bronchodilator treatment measured as forced expiratory volume 1 s (FEV1) by a spirometer (piston) (14). Altogether, 185 asthmatic patients were enrolled in the study. After clinical and laboratory investigation, 41 patients were excluded from the further investigation. Exclusion criteria included medication within the last 6 wk for other diseases than asthma, positivity for C. trachomatis or C psittaci, or apparent viral or bacterial infection. After the exclusion 144 asthmatic children remained in the study.
All the asthmatics (or their parents) were instructed to record accurately for 2 wk their symptoms, treatment, and twice-daily (in the evening and in the morning) peak expiratory flow (PEF). If the patient is younger than 5 y old, the determination of lung function tests (PEF or FEV1) is usually not possible. In that case, the diagnosis of the disease was made according to the other symptoms. Asthma severity was classified according to Global Initiative for Asthma guidelines (15,16) (detailed description of our classification of asthma severity is in ref. 16). Some clinical and biologic characteristics of the asthmatic patients are presented in Table 1.
The control children were randomly selected from outpatients from the Orthopaedic Department in the Budai Children's Hospital. One or two control patients were matched to one asthmatic patient. Matching criteria included age, ethnicity and sex. Altogether 232 controls were recruited for the investigation. After clinical and laboratory investigation 58 patients were excluded from the study. Exclusion criteria included medication within the last 6 wk, positivity for C. trachomatis or C psittaci, lung function test value less than 80% of the predicted value for that person, apparent viral or bacterial infection. Subjects in the control group had mild musculoskeletal alterations like pes planus or scoliosis. After the exclusion 174 healthy children (Table 1) participated in the study.
Informed parental consent was obtained for each patient and control and the study was approved by the Institutional Review Board of Budai Children's Hospital. The investigation conforms to the principles outlined in the Declaration of Helsinki.
All children were from Budapest and most of them belonged to the Hungarian Caucasian population. Approximately, 5% of the children were of Gypsy origin (6 asthmatics and 8 controls), which rate is similar to that of in the general population of Budapest.
Laboratory analysis.
Total Genomic DNA was extracted from white blood cells using QIAamp DNA Blood Midi Kit of QIAGEN GmbH (Hilden, Germany).
The RANTES –403 genotype was determined using an RsaI site introduced with a mismatch into the PCR primer next to the G-A transition. Amplification with the primers RANTES –581S: 5′-CAC AAG AGG ACT CAT TCC AAC TCA-3′ and RANTES –376AS: 5′-GTT CCT GCT TAT TCA TTA CAG ATC GTA-3′, which has a guanine instead of a thymine (underlined) generated a 206 bp product. Digestion with RsaI yields 180 and 26 bp fragments when G is at position –403. The products were separated in 3% agarose gel, stained with ethidium bromide.
The MCP-1 –2518 genotype was determined with a PCR–restriction fragment length polymorphism (RFLP) assay using a PvuII site affected by the G/A polymorphism. Amplification with the primers MCP417S: 5′-TCT CTC ACG CCA GC ACT GAC C-3′ and MCP650AS: 5′-GAG TGT TCA CAT AGG CTT CTG-3′ generated a 234 bp product. Digestion with PvuII yields 159 and 75 bp fragments when G is at position −2518. The products were separated in 3% agarose gel, stained with ethidium bromide.
The TNFα –308 polymorphism was determined by DNA amplification by PCR using the primers: TNFA1: ATC TGG AGG AAG CGG TAG TG; and TNFM1: AAT AGG TTT TGA GGG CCA TG. The PCR products were digested at 37°C with NcoI and separated in 4% agarose gel, stained with ethidium bromide.
All genotypes were determined at least twice. Only those genotypes were accepted, when at least two genotypings gave the same results.
C. pneumoniae–specific IgA and IgG were determined from serum used Sero CP-IgA, IgG protein ELISA (Savyon Diagnostics, Ashdod, Israel) according to the manufacturer's instruction. Serum was designated as positive if the cut-off index (COI) was >1.1. C. trachomatis or C psittaci were determined by ELISA with SeroFIA C. psittaci, SeroFIA C. trachomatis kits by Savyon Diagnostic Ltd.
Total serum IgE levels and specific IgE levels to more than 100 allergens were determined by the Pharmacia CAP System (Pharmacia Diagnostics AB, Uppsala, Sweden). IgE levels were defined as high in subjects whose total serum IgE exceeded 100 kU/L, and specific IgE was considered positive in those having detectable allergen-specific IgE (>0.35 kU/L). Atopy was defined by positive skin prick test to at least one allergen (wheal diameter 3 mm greater than saline control) and/or positive total or specific IgE levels.
Statistical methods.
Allele frequencies were calculated by allele counting. Data were analyzed using MedCalc 5.0 (MedCalc Software, Belgium), SPSS 11.0 (SPSS Inc.), and Arlequin 1.1 (Genetics and Biometry Lab, University of Geneva) programs. Hardy-Weinberg equilibrium was tested by using a χ2 goodness-of-fit test. χ2 test was used to test for differences in allele distribution between the groups. Confidence intervals were calculated at the 95% level. It has earlier been suggested that the response to the C. pneumoniae infection is influenced by sex (4). Furthermore, the age, especially in childhood, may also have substantial impact on the immune response. To minimize the effect of these two potentially confounding factors, the results were adjusted for age and sex by multiple logistic regression analysis. In some analyses, genotype*serology interaction test was also included. To account for multiple testing, we used the Bonferroni correction and considered significant only those results for which p < 5.6 × 10−3.
RESULTS
Table 2 shows the number and percentage of children positive for C. pneumoniae–specific antibodies in the two groups. There were no significant differences in the proportion of patients positive for any C. pneumoniae–specific antibodies between asthmatic and control children. Furthermore, there were no differences between sexes in the infection status in any groups of children (data not shown).
It has been suggested that IgG positivity indicates that the probands have had C. pneumoniae infection in the past and the presence of short-lived specific IgA antibodies to C. pneumoniae can be associated with both acute and chronic infection (persistent levels of IgA). Potentially chronic or recurrent infection with C. pneumoniae may be identified when IgG positivity is combined with IgA positivity. According to this latter definition 29 asthmatic (20.1%) and 37 control (21.3%) had chronic or recurrent C. pneumoniae infection among our patients. The two groups did not differ statistically in this respect either (Table 2).
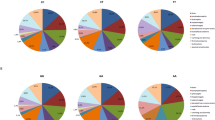
The Table 3 shows the genotype distribution and the prevalence of the polymorphisms in asthmatic and control patients. All genotypes in all samples were determined. The results were overall in “Hardy-Weinberg” equilibrium. As we have described previously the prevalence of the −2518G allele in the gene regulatory region of the MCP-1 is significantly higher in the asthmatic children than in the controls [33.3% versus 21.0% in asthmatic versus control patients, respectively; p < 0.001; OR = 1.88(1.32–2.69)]. Detailed description of the analysis of the connection between asthma and the MCP-1 –2518 polymorphism is presented in ref. 16.
No significant differences were observed in the genotype and allele frequencies of the RANTES and TNFα promoter polymorphisms between the two groups (Table 3).
No significant difference between C. pneumoniae–seropositive and –seronegative individuals in the frequencies of the polymorphisms was revealed. None of the genotypes was associated with altered susceptibility to C. pneumoniae infection (data not shown).
To evaluate the modifying effect of the three polymorphisms on the susceptibility to asthma in C. pneumoniae infection, children were stratified according to their genotypes, and the asthmatic and control children were compared on the basis of their infection status. Logistic regression analysis for the association between the prevalence of different C. pneumoniae–specific antibodies and asthma in children with different genotypes is presented in Table 4.
Among asthmatic children carrying the TNFα −308A allele, there were significantly more patients positive for C. pneumoniae–specific IgG, than among control children carrying the same allele [20.1% versus 9.2% of asthmatic versus control children, respectively; p = 0.002; odds ratio (95% confidence interval) (OR (95% CI)) = 4.08 (1.75–9.52)]. The results remained significant after adjusting for age and sex [p = 0.005; OR (95% CI) = 3.52 (1.52–7.53) (Table 4)]. These results were confirmed by an interaction test regarding C. pneumoniae IgG positivity*TNFα −308A allele interaction for asthma susceptibility, which gave similar results [p = 0.005; OR (95% CI) = 4.16 (1.83–9.61)]. These results indicate that C. pneumoniae–specific IgG positivity is associated with asthma, when only children carrying the TNFα −308A alleles are considered.
In contrast, comparing asthmatic children homozygous for the wild-type TNFα –308 allele (G/G) with control children with identical genotype, there were less asthmatic patients positive for C. pneumoniae–specific IgG than among control children (24.3% versus 39.1% of asthmatic versus control children, respectively; p = 0.01; OR (95% CI) = 0.49 (0.23–0.81)), although the p value was slightly higher than the Bonferroni corrected p value (p = 5.6 × 10−3).
There were no significant differences between asthmatic and control children when the TNFα −308 genotypes and C. pneumoniae–specific IgA or the combined IgA + IgG positivity were considered. The MCP-1 –2518 and the RANTES −403 polymorphisms did not influence the asthma risk associated with C. pneumoniae in this context (Table 4).
To further evaluate the role of these polymorphisms in the susceptibility to asthma among children infected with C. pneumoniae, the prevalence of the different genotypes in subjects positive for C. pneumoniae–specific antibodies was compared in asthmatics and controls. Logistic regression analysis for the association between the prevalence of different genotypes and asthma in children positive for C. pneumoniae–specific antibodies is presented in Table 5.
The distribution of the TNFα −308 genotypes differed significantly between asthmatic and control children who were positive for C. pneumoniae–specific IgG. The proportion of children with the rare TNFα allele was higher in asthmatics than in healthy controls comparing it with children with the G/G genotype [45.3% and 54.7% of asthmatics versus 19.0% and 81.0% of controls had G/A + A/A versus G/G genotypes, respectively; adjusted OR (95% CI) = 3.31 (1.62–6.88); p = 0.005].
The distribution of the MCP-1 –2518 genotypes differed also significantly between asthmatic and control children with C. pneumoniae–specific IgG positivity [65.8% and 34.2% of asthmatics versus 37.8% and 62.2% of controls had A/G + G/G versus A/A genotypes, respectively; OR (95% CI) = 2.84 (1.43–5.87); p = 0.001]. However, carrying alone the MCP-1 −2518G allele increases the susceptibility for developing asthma, thus it must be investigated, whether C. pneumoniae positivity is associated with an additional risk in G allele carriers? Although carrying the G allele is associated with a higher OR in C. pneumoniae IgG positive individuals than in G carriers in the whole population [OR (95% CI) = 1.88 (1.32–2.69)], our analysis revealed that these differences were not statistically significant.
Investigating the effect of RANTES –403A allele in C. pneumoniae–positive individuals showed that children with chronic or recurrent C. pneumoniae infection (IgG + IgA positivity) had a high OR for developing asthma comparing them to children with RANTES –403 G/G genotype and similar infection status [OR (95% CI) = 4.32 (1.19–15.56)], since the proportion of children with the rare RANTES allele was higher in asthmatics than in healthy controls comparing it with children with the G/G genotype (34.5% and 65.5% in asthmatics versus 10.8% and 89.2% in controls; had G/A + A/A versus G/G genotypes, respectively) but the p value (p = 0.03) did not reach the Bonferroni corrected level of significance (p = 5.6 × 10−3).
To assess the effect of chronic C. pneumoniae infection on the severity of asthma in this population we compared the prevalence of children with different C. pneumoniae positivity in groups with intermittent and moderate asthma. According to our results the two groups did not differ significantly from each other in this respect. The two groups did not show significant difference either, when seropositivity and TNFα, MCP-1, or RANTES variant alleles were considered (data not shown).
One hundred and twelve (77.8%) asthmatic and 35 (20.1%) control patients were atopic. The C. pneumoniae infection, the investigated polymorphisms and their combinations were not associated with atopy.
DISCUSSION
Our study shows that C. pneumoniae–specific IgG positivity is associated with asthma, when children carrying the TNFα –308A allele are considered. Furthermore, children infected with C. pneumoniae in the past (IgG positivity) carrying the TNFα –308A allele have considerably higher risk of developing asthma than children with similar infection status carrying normal genotypes.
It must be noted, however, that retrospective case-control studies such as ours may suffer from several biases, which may lead to false-positive and to false-negative results. We have matched our patient and control groups for age, sex and ethnicity to reduce this possibility. In addition, we applied the Bonferroni correction for multiple comparisons to reduce the type one error. It is also important to mention that there was no patient with severe asthma in our population thus it is possible that the conclusion of this study may not be applied to those with severe asthma.
A causal association between C. pneumoniae and asthma is biologically plausible, based on the observations that asthma is a chronic inflammatory disease of the airways and that Chlamydia species are known to produce chronic inflammatory damage in target organs. C. pneumoniae is a common cause of infection, but clearly, not all infected patients develop asthma. This suggests that certain individuals may be genetically predisposed to the chronic effects of C. pneumoniae infection on airway function, or be genetically susceptible to infection, rendering them more likely to be persistently infected.
Bacterial infection of resident airway cells, such as epithelial cells or macrophages, produces a cascade of cytokines and chemokines that recruit and activate immune cells involved in bacterial destruction. However, these immune cells may also lead to inflammation and tissue damage (17). Several studies have indicated that C. pneumoniae infection induces the expression of several cytokines and chemokines, among others TNFα, MCP-1, and RANTES, all of them are implicated in the pathomechanism of asthma (5,10,16).
TNFα has been shown to play an important role in immunity to bacterial infection, including chlamydiae (13). There is evidence that TNFα plays a role in vivo in host defence against chlamydiae, but, due to indirect effects, it can also delay the clearance of the bacteria (18). TNFα is also an important modulator in the chronic inflammatory process of asthma. In murine models of asthma, either a deficiency in TNFα receptors, chronic treatment with a TNFα antibody or induction of a TNFα autoantibody, results in marked attenuation of antigen induced airway inflammation (19,20). In addition, inhalation of TNFα in both rodents (21) and normal (22) or asthmatic humans (23) leads to the development of airway hyperresponsivity accompanied by airway neutrophilia. The TNFα −308A allele has been tested in 19 published studies so far, and an association between the A allele and asthma was reported in seven of these studies (24). In one additional study, an extended haplotype in the TNFα and lymphotoxin genes was found to be associated with asthma susceptibility and an increased frequency of transmission from parents of the G allele to their child with asthma was shown (24). Our study failed to detect an association between this promoter polymorphism and asthma. But the difference between the asthmatic and control children became significant when subjects stratified according to TNFα −308 genotypes and C. pneumoniae–specific IgG were considered. According to these results C. pneumoniae infection may lead to the development of asthma in genetically predisposed children carrying TNFα −308A allele. Naturally, a reverse scenario is also feasible. Asthmatic children with TNFα −308A allele are prone to developing a chronic C. pneumoniae infection, which could then propagate the asthma process. Although our results that the TNFα −308A allele together with past (IgG positivity) and not the chronic or recurrent (IgA, or IgG + IgA positivity) infection associates with the increased susceptibility to asthma does not support this hypothesis, prospective studies are needed to determine the exact role of this genotype-environment interaction in the disease. It must be noted, however, that those with C. pneumoniae antibodies probably have had past infection, but the converse is not necessarily true. In fact, the persistence of antibodies may be directly related to the rate of immune clearance of chlamydophila. Therefore, it cannot be assumed that those without antibodies have not had C. pneumoniae infection. This can reduce the power of this study and might offer an explanation to the findings with regard to past versus chronic/recurrent infection.”
The exact role of the TNFα −308A allele is quite controversial in this process. Several studies have indicated that the allele is associated with increased TNFα transcription (6,25). In this case, increased TNFα expression might be associated with an increased susceptibility to inflammation. C. pneumoniae infection is also linked to chronic inflammatory damage in the infected organs. The coincidence of the –308A allele and the C. pneumoniae infection might make individuals more susceptible to developing asthma. Additionally, C. pneumoniae infection might provoke higher TNFα expression in individuals carrying the 308A allele increasing the risk of asthma. However, others have stated that the −308A allele does not up-regulate the TNFα level (24,26). Earlier we have shown that the TNFα −308 allele is part of an extended ancient haplotype (haplotype 8.1) and is in close linkage disequilibrium with the hemolytically inactive complement C4A*Q0 allele located approximately 430 kb from the TNFα gene on chromosome 6 (27,28). The complement system plays a principal role in the defence against bacterial infection. Therefore, it can be assumed that carriers of the silent C4A*Q0 allele have an impaired capacity to eliminate or mitigate C. pneumoniae infection increasing the risk for developing chronic conditions like asthma. Naturally, it is also possible that genes linked with these alleles are also involved, since there are other candidate genes in close vicinity, including the MHC genes, lymphotoxin-α and β (related to TNFα), heat shock protein 70 (putative role in autoimmune inflammation), leukocyte-specific transcript-1 (involved in macrophage activation), and several other genes with still uncertain or unknown functions.
The high OR (4.32) for C. pneumoniae IgG + IgA positive children carrying the RANTES −403A allele for developing asthma is also an interesting result. Although the p value did not reach the level of significance because of the Bonferroni correction, it must be noted that this correction is known to be conservative and thus “overcorrected” the raw p values. Regarding the important role of RANTES in both asthma and C. pneumoniae infection, investigation of higher number of patients should be needed to explore the exact biologic role of this polymorphism in this process.
We have found no associations between atopy and the C. pneumoniae infection, the investigated polymorphisms and their combinations. It must be noted, however, that the control population is significantly less atopic than the asthmatic population, and because the nonasthmatic atopic children are too few to involve in a valuable statistical analysis, it cannot be excluded that the observed associations are influenced by the difference in the prevalence of atopy between the asthmatic and control patients. Investigation of higher number of nonasthmatic atopic patients may explore the exact role of the interaction between C. pneumoniae infection and the TNFα polymorphism in these diseases (study is in progress).
These results are in good correlation with the findings of Conway et al., who investigated patients with scarring trachoma caused by infection with Chlamydia trachomatis and detected higher prevalence of the TNFα −308A allele in patients than in controls (29). Our paper is also in line with some recent reports, which investigate the role of genetic variations in the immune systems (30,31). The effects of these variations are usually modest and insufficient to cause disease when taken individually. However, they might induce significant phenotypic differences when they become involved in gene-by-gene and/or gene-by-environmental interaction.
In conclusion, this article presents an association between a promoter polymorphism of the TNFα gene, C. pneumoniae infection, and development of asthma. Additionally, this study highlights the possible roles of polymorphisms in the immune system in response to bacterial infection.
Abbreviations
- MCP-1:
-
monocyte chemoattractant protein-1
- RANTES:
-
regulated on activation normal T cell expressed and secreted
References
Ober C, Thompson EE 2005 Rethinking genetic models of asthma: the role of environmental modifiers. Curr Opin Immunol 17: 670–678
Johnston SL, Martin RJ 2005 Chlamydophila pneumoniae and Mycoplasma pneumoniae: A role in asthma pathogenesis?. Am J Respir Crit Care Med 172: 1078–1089
Pasternack R, Huhtala H, Karjalainen J 2005 Chlamydophila (Chlamydia) pneumoniae serology and asthma in adults: a longitudinal analysis. J Allergy Clin Immunol 116: 1123–1128
Grayston JT, Campbell LA, Kuo CC, Mordhorst CH, Saikku P, Thom DH, Wang SP 1990 A new respiratory tract pathogen: Chlamydia pneumoniae strain TWAR. J Infect Dis 161: 618–625
Howarth PH, Babu KS, Arshad HS, Lau L, Buckley M, McConnell W, Beckett P, Al Ali M, Chauhan A, Wilson SJ 2005 Tumour necrosis factor (TNFalpha) as a novel therapeutic target in symptomatic corticosteroid dependent asthma. Thorax 60: 1012–1018
Wilson AG, Symons JA, McDowell TL, McDewitt HO, Duff GW 1997 Effects of a polymorphism in the human tumor necrosis factor alpha promoter on transcriptional activation. Proc Natl Acad Sci U S A 94: 3195–3199
Campbell EM, Charo IF, Kunkel SL, Strieter RM, Boring L, Gosling J, Lukacs NW 1999 Monocyte chemoattractant protein-1 mediates cockroach allergen-induced bronchial hyperreactivity in normal but not CCR2–/– mice: The role of mast cells. J Immunol 163: 2160–2167
Rovin BH, Lu L, Saxena R 1999 A novel polymorphism in the MCP-1 gene regulatory region that influences MCP-1 expression. Biochem Biophys Res Commun 259: 344–348
Lukacs NW, Strieter RM, Warmington K, Lincoln P, Censue SW, Kunkel SL 1997 Differential recruitment of leukocyte populations and alteration of airway hyperreactivity by C-C family chemokines in allergic airway inflammation. J Immunol 158: 4398–4404
Nickel RG, Casolaro V, Wahn U, Beyer K, Barnes KC, Plunkett BS, Freidhoff LR, Sengler C, Plitt JR, Schleimer RP, Caraballo L, Naidu RP, Levett PN, Beaty TH, Huang SK 2000 Atopic dermatitis is associated with a functional mutation in the promoter of the C-C chemokine RANTES. J Immunol 164: 1612–1616
Rodriguez N, Fend F, Jennen L, Schiemann M, Wantia N, Prazeres da Costa CU, Durr S, Heinzmann U, Wagner H, Miethke T 2005 Polymorphonuclear neutrophils improve replication of Chlamydia pneumoniae in vivo upon MyD88-dependent attraction. J Immunol 174: 4836–4844
Dechend R, Gieffers J, Dietz R, Joerres A, Rupp J, Luft FC, Maass M 2003 Hydroxymethylglutaryl coenzyme A reductase inhibition reduces Chlamydia pneumoniae-induced cell interaction and activation. Circulation 108: 261–265
Gerard HC, Wang Z, Whittum-Hudson JA, El-Gabalawy H, Goldbach-Mansky R, Bardin T, Schumacher HR, Hudson AP 2002 Cytokine and chemokine mRNA produced in synovial tissue chronically infected with Chlamydia trachomatis and C. pneumoniae. J Rheumatol 29: 1827–1835
American Thoracic Society 1995 Standardization of spirometry, 1994 Update. American Thoracic Society. Am J Respir Crit Care Med 152: 1107–1136
NHLBI/WHO Workshop Report 1995. Global strategy for asthma management and prevention. National Institutes of Health. National Heart, Lung, and Blood Institute, Bethesda, MD. Publication No. 95-3659: 144–168.
Szalai C, Kozma GT, Nagy A, Bojszkó Á, Krikovszky D, Szabó T, Falus A 2001 Polymorphism in the gene regulatory region of MCP-1 is associated with asthma susceptibility and severity. J Allergy Clin Immunol 108: 375–381
Verkerk MS, Visseren FL, Paul Bouter K, Diepersloot RJ 2003 Acute-phase response of human hepatocytes after infection with Chlamydia pneumoniae and cytomegalovirus. Eur J Clin Invest 33: 720–725
Perry LL, Su H, Feilzer K, Messer R, Hughes S, Whitmire W, Caldwell HD 1999 Differential sensitivity of distinct Chlamydia trachomatis isolates to IFN-gamma-mediated inhibition. J Immunol 162: 3541–3548
Rudmann DG, Moore MW, Tepper JS, Aldrich MC, Pfeiffer JW, Hogenesch H, Tumas DB 2000 Modulation of allergic inflammation in mice deficient in TNF receptors. Am J Physiol Lung Cell Mol Physiol 279: L1047–L1057
Zuany-Amorim C, Manlius C, Dalum I, Jensen MR, Gautam A, Pay G, Mouritsen S, Walker C 2004 Induction of TNF-alpha autoantibody production by AutoVac TNF106: a novel therapeutic approach for the treatment of allergic diseases. Int Arch Allergy Immunol 133: 154–163
Tavernier J, Pauwels RA 1992 Tumor necrosis factor causes bronchial hyperresponsiveness in rats. Am Rev Respir Dis 145: 332–336
Thomas PS, Yates DH, Barnes PJ 1995 Tumor necrosis factor-alpha increases airway responsiveness and sputum neutrophilia in normal human subjects. Am J Respir Crit Care Med 152: 76–80
Thomas PS, Heywood G 2002 Effects of inhaled tumour necrosis factor alpha in subjects with mild asthma. Thorax 57: 774–778
Randolph AG, Lange C, Silverman EK, Lazarus R, Weiss ST 2005 Extended haplotype in the tumor necrosis factor gene cluster is associated with asthma and asthma-related phenotypes. Am J Respir Crit Care Med 172: 687–692
Louis E, Franchimont D, Piron A, Gavaert Y, Schaaf-Lafontaine N, Roland S, Mahieu P, Malaise M, De Groote D, Louis R, Belaiche J 1998 Tumor necrosis factor gene polymorphism influences TNF-alpha production in lipopolysaccharide-stimulated whole blood cell culture in healthy humans. Clin Exp Immunol 113: 401–406
Knight JC, Keating BJ, Rockett KA, Kwiatkowski DP 2003 In vivo characterization of regulatory polymorphisms by allele-specific quantification of RNA polymerase loading. Nat Genet 33: 469–475
Szalai C, Fust G, Duba J, Kramer J, Romics L, Prohaszka Z, Csaszar A 2002 Association of polymorphisms and allelic combinations in the tumour necrosis factor-alpha-complement MHC region with coronary artery disease. J Med Genet 39: 46–51
Vatay A, Yang Y, Chung EK, Zhou B, Blanchong CA, Kovacs M, Karadi I, Fust G, Romics L, Varga L, Yu CY, Szalai C 2003 Relationship between complement components C4A and C4B diversities and two TNFA promoter polymorphisms in two healthy Caucasian populations. Hum Immunol 64: 543–552
Conway DJ, Holland MJ, Bailey RL, Campbell AE, Mahdi OS, Jennings R, Mbena E, Mabey DC 1997 Scarring trachoma is associated with polymorphism in the tumor necrosis factor alpha (TNF-alpha) gene promoter and with elevated TNF-alpha levels in tear fluid. Infect Immun 65: 1003–1006
Nagy A, Kozma GT, Keszei M, Treszl A, Falus A, Szalai C 2003 The development of asthma in children infected with Chlamydia pneumoniae is dependent on the modifying effect of mannose-binding lectin. J Allergy Clin Immunol 112: 729–734
Lazarus R, Vercelli D, Palmer LJ, Klimecki WJ, Silverman EK, Richter B, Riva A, Ramoni M, Martinez FD, Weiss ST, Kwiatkowski DJ 2002 Single nucleotide polymorphisms in innate immunity genes: abundant variation and potential role in complex human disease. Immunol Rev 190: 9–25
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was supported by OTKA (National Scientific Research Fund, grants T031887, T046372, and TS/2 044707) and a János Bolyai Research Grant.
Rights and permissions
About this article
Cite this article
Tölgyesi, G., Keszei, M., Ungvári, I. et al. Involvement of TNFα –308A Promoter Polymorphism in the Development of Asthma in Children Infected With Chlamydophila pneumoniae. Pediatr Res 60, 543–548 (2006). https://doi.org/10.1203/01.pdr.0000242298.24089.52
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.pdr.0000242298.24089.52
This article is cited by
-
The Regulated upon Activation Normal T-cell Expressed and Secreted (RANTES) −28C/G and −403G/A Polymorphisms and Asthma Risk: A Meta-analysis
Molecular Diagnosis & Therapy (2014)
-
The −308 G/A polymorphism in TNF-α gene is associated with asthma risk: an update by meta-analysis
Journal of Clinical Immunology (2011)
-
Asthma from a pharmacogenomic point of view
British Journal of Pharmacology (2008)