Abstract
Previous studies have shown that early life stress in the form of intermittent maternal separation (MS) predisposes adult rats to develop stress-induced intestinal mucosal dysfunction and visceral hypersensitivity. However, the mechanism involved in the functional abnormalities is unclear. Our aim was to study immature animals during or shortly after exposure to MS to determine whether there are early pathophysiological changes in the gut. Sprague-Dawley rat pups were individually separated from the dam for 3 h/d from 4 to 21 d of age; nonseparated (NS) control pups remained in the home cage with the dam. On d 19–20, d 24–25, and d 29–30, blood was collected for corticosterone measurement, and colonic tissues were removed for functional and morphologic assessment. Corticosteroid levels were elevated in MS pups compared with NS, indicating that MS was indeed stressful. The distal colon demonstrated significantly enhanced ion secretion and macromolecular permeability at d 19–20 and d 24–25, returning to normal by d 29–30. Electron microscopy and bacterial culture studies indicated bacteria adhering to and penetrating into the colonic epithelium of the MS pups at all time points, while such events were rare in NS pups. The pathophysiological changes were inhibited by injecting pups sc with a corticotropin-releasing hormone (CRH) receptor antagonist daily during MS. Our studies indicate that early psychological trauma predisposes neonatal rats to develop persistent mucosal barrier dysfunction, including impaired host defense to luminal bacteria, by a mechanism involving peripheral CRH receptors.
Similar content being viewed by others
Main
Childhood psychosocial factors and long-term stress are important in the pathogenesis of certain disorders such as anxiety and depression (1). Early life stressors also increase the risk of intestinal disorders such as irritable bowel syndrome (IBS) and inflammatory bowel disease in adulthood (2). Chronic stress and abuse therefore contribute to the development of both psychological and somatic disease states (3).
In rodents, neonatal MS is a well-characterized model of early life stress that has been used to study depression and anxiety (4,5). More recently, MS has been used as an animal model in the investigation of intestinal dysfunction. Subjecting pups to daily MS during the neonatal period results in marked alterations in behavior (6,7) and physiology (8–11) in later life. MS is associated with gut inflammation in adult rats (10), which is thought to be maintained by nerve growth factor (9). In addition, exposure to early life stress affects colonic motility and induces visceral hyperalgesia both basally (12) and in response to an acute stressor in adulthood (11). Previous studies from our group (8) indicate that adult rats exposed to MS as neonates become susceptible to intestinal mucosal pathophysiology when exposed to mild acute stress. The link between early events and intestinal pathophysiology in adulthood is unclear.
The first 2 wk of life in rats are characterized by a stress hyporesponsive period, during which the neonate is unable to increase circulating glucocorticoid levels (13). Life stress, in the form of moderate periods of MS, during this stage of development results in changes in the central nervous system, accompanied by a compromised ability to control the synthesis of CRH in response to acute laboratory stressors (14). CRH may play an important role in modulating brain-gut functions in patients with irritable bowel syndrome (IBS) (15). Evidence has also shown that this neuropeptide is involved in gut hypersensitivity in rodent models of IBS (16). In adult rats exposed to acute stress, peripheral CRH receptors have been implicated in stress-induced gut changes including enhanced mucin release (17), ion secretion (18), and permeability (16,18). In addition, we previously reported (8) that the stress-induced alterations in colonic mucosal function in adult rats, maternally separated as infants, were inhibited following a single i.p. administration of a nonselective CRH receptor antagonist before stress exposure. This suggests the involvement of peripheral CRH receptors in the intestinal response of adult rats to acute stress (8). However, the mechanism by which neonatal trauma alters the vulnerability of adult rats to develop stress-induced gut pathophysiology has not been described.
Maturation of the intestinal mucosal barrier occurs in the neonatal period in rodents with the absorption of intact macromolecules being elevated at birth and decreasing with age (19). It has been found that macromolecules are more adherent to the surface of immature cells than mature cells and that transport occurs more readily in young animals, falling rapidly with gut closure (20). However, to our knowledge, colonic mucosal barrier function to antigens and microbes in rat pups has not been reported under control versus stress conditions. Our aim was to examine the immediate effects of early psychological trauma on immature intestinal mucosal function and the potential role of CRH receptors in the development of gut pathophysiology. Neonatal rats subjected to daily periods of MS demonstrated rapidly altered colonic physiology and impaired host defense to luminal bacteria. Studies using a CRH receptor antagonist injected subcutaneously implicated peripheral CRH receptors. Such changes in early life may contribute to the development of a stress-susceptible phenotype in later life.
METHODS
Animals.
Primiparous timed-pregnant Sprague-Dawley female rats were obtained from Charles-River Laboratories (St. Constant, Quebec) on gestational d 13–14. Dams were individually housed in cages lined with chip bedding on a 12:12-h light-dark cycle with free access to food and water. Day of birth was considered to be d 1. All procedures were approved by the Animal Care Committee at McMaster University.
Study design.
To examine the direct effects of MS on colonic physiology, neonatal rat pups were exposed to the separation protocol from d 4 until d 18 or 19 and killed the following day. Pups were killed at the same time each day to limit the effects of circadian rhythm. To examine whether the effects of MS were persistent, a timeline was created with some pups subjected to MS (d 4–21), weaned on d 22 and studied on d 24–25 or 29–30. Rat pups were killed by decapitation and trunk blood was collected. Colonic tissue was excised and placed on ice. Segments were mounted in Ussing chambers for functional studies. Additional segments were processed for light or electron microscopy for morphologic assessment. Body weight and colonic length were recorded. In a second set of experiments, rat pups were injected subcutaneously with a CRH receptor antagonist daily immediately before MS.
Separation protocol.
Dams and their litters (culled to 12 pups) were randomly assigned to the MS protocol or to the control nonseparated (NS) protocol. MS pups were individually separated from the dam for 3 h/d from d 4 to 21 of life (as described below), whereas NS pups remained in their home cage with the dam and left undisturbed. MS pups were removed from the home cage and placed individually into compartmentalized holding cages lined with bedding. Cages were maintained at 37 ± 0.5°C by placing them on temperature controlled heating pads. MS was performed at the same time each day to minimize the effects of circadian rhythm. Pups were weaned on d 22 and housed in small groups (three to four) until further use. All procedures were approved by the Animal Care Committee at McMaster University.
Corticosterone.
Serum was isolated from trunk blood via centrifugation and frozen at –20°C until analysis. Corticosterone was measured by radioimmunoassay (ICN, Costa Mesa, CA).
Using chamber studies.
Segments of colon (distal or proximal) were opened along the mesenteric border, cut into flat sheets and mounted in Using chambers (WP Instruments, Narco Scientific, Mississauga, Ontario), exposing 0.6 cm2 of tissue area to 8 mL of circulating oxygenated Krebs buffer (in mmol/L: 115 NaCl, 1.25 CaCl2, 1.2 MgCl2, 2.0 KH2PO4, and 25 NaHCO3, pH 7.35 ± 0.02, 37°C). Glucose (10 mmol/L) was added to the serosal buffer, and balanced by mannitol (10 mmol/L) in the mucosal buffer. Agar-salt bridges were used to monitor the potential difference across the tissue and inject the required short-circuit current (Isc). This maintains a zero potential difference as registered by automated voltage clamps. A computer system recorded Isc continuously. Baseline Isc values were obtained 15 min after the tissues were mounted. Isc, an indicator of active ion transport, was expressed in microamperes per square centimeter.
Macromolecular permeability.
Horseradish peroxidase (HRP) (44 kd) was used as a probe to examine the effects of stress on macromolecular permeability. Type VI HRP (Sigma Chemical Co., St. Louis, MO) was added (10−5 mol/L) to the luminal buffer once equilibrium was reached, 15 min following mounting. Serosal samples (500 μL) were taken at 30-min intervals for 2 h and replaced with fresh buffer. HRP activity was measured in duplicate using a modified Worthington kinetic assay as previously described (21). Phosphate buffer (containing 0.003% hydrogen peroxide and 80g/mL o-dianisidine) was added and enzymatic activity was determined based on the rate of increase in OD at 460 nm for 15 min. The flux of HRP from the mucosa to serosa was calculated as the average value of two consecutive stable flux periods (60–90 and 90–120 min). HRP flux was expressed as picomoles per square centimeter per hour.
Bacterial adherence/penetration/translocation.
Distal colonic tissue and spleen samples were collected for measurement of adherent, penetrating, and translocating bacteria. Tissue, 1- to 2-cm long pieces, was excised from rat pups, weighed, and rinsed in 10 mL of sterile PBS. Segments were cut longitudinally and vortexed three times in 1 mL of sterile saline. Pieces were then homogenized in 1 mL of sterile Triton-X 100 (0.1%) and diluted (1:2, 1:10, and 1:100). The dilutions were then spread (100 μL) on blood agar plates (PML Microbiologicals, Mississauga, ON) and incubated at 37°C. After 24 h, the plates were examined for growth and visible colonies were counted and expressed as colony-forming units (CFUs) per gram of tissue (22).
Morphology: Histology.
Distal colonic tissues were collected, fixed in formalin, embedded in paraffin, and subsequently stained with hematoxylin and eosin. Crypt length was measured via micrometer in coded sections.
Morphology: Ultrastructural studies.
Distal colonic tissues were immediately fixed in 2.5% glutaraldehyde in a 0.1 mol/L sodium-cacodylate buffer (pH 7.4) for 2 h at 22°C, rinsed with 0.05 cacodylate buffer (pH 7.6) at 4°C for 18 h, washed three times for 5 min each time, and processed for routine transmission electron microscopy (23). Ultra-thin tissue segments were cut to obtain longitudinal sections of epithelial cells and placed on copper grids. The slides were then stained with uranyl acetate and lead citrate. Observations were recorded in a blinded manner.
Myeloperoxidase (MPO) assay.
MPO is an enzyme found within the granules of neutrophils and is used as a marker for tissue inflammation (24). Tissue samples from the distal colon were collected, snap frozen in liquid nitrogen, and MPO activity was measured as previously described (25). Data are expressed as units (U)/mg tissue where 1 U is the quantity of MPO required to convert 1 μmol/L of H2O2 into water in 1 min at 22°C.
Nonselective CRH receptor antagonists.
Rat pups were injected s.c. with the nonreceptor specific CRH antagonist, α-helical CRH (9-41) (Sigma Chemical Co.; 100 μL, 250 μg/kg), daily on d 4–20, immediately before MS. This dose has been previously shown to inhibit CRH-induced barrier dysfunction and other aspects of gut pathophysiology (8,18). Saline was used as a vehicle control. The NS pups were removed from the dam and injected, then returned to the home cage.
Statistics.
Results are expressed as the mean ± SE. Groups were compared using the analysis of variance (ANOVA) and Mann-Whitney tests were used for post hoc comparisons where appropriate. Differences of p < 0.05 were considered to be significant.
RESULTS
MS did not affect body weight or colonic length.
No significant deficiencies in body weight or colonic length were found in MS versus NS pups (Table 1), indicating that the MS pups were receiving adequate nutrition and normal growth was not affected.
MS stimulated release of circulating corticosterone.
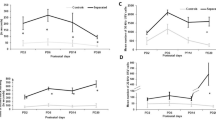
Mean corticosterone levels in serum were lower in the weaned pup groups (>22 d of age) versus the younger animals (19–20 d of age), as expected (26). However, values were consistently significantly increased (p < 0.05) in rat pups subjected to MS compared with NS controls at 19–20, 24–25, and 29–30 d (Fig. 1).
MS altered mucosal physiology in distal but not proximal colon.
Baseline Isc in the distal colon exhibited higher values than those in the proximal colon in both NS control and MS pups at the two earliest time points (Fig. 2). MS had no effect on Isc in the proximal colon (Fig. 2A), but did result in significantly (p < 0.05) elevated Isc in the distal colon (Fig. 2B) at 19–20 and 24–25 d, but not at 29–30 d.
The effect of MS on ion transport. Tissues from proximal colon (A), distal colon (B) from MS (▪) or NS (□) rat pups were studied in Ussing chambers. MS caused significant elevations in the baseline Isc in the distal colon of pups at 19–20 and 24–25 d of age compared with NS controls. There were no changes in the proximal colon. Values indicate means ± SE (n = 12–13), *p < 0.05.
HRP flux was also higher in the distal compared with the proximal colon, but only at the earliest time point (Fig. 3). MS had no effect on HRP flux in the proximal colon (Fig. 3A), but significantly (p < 0.05) increased the flux in the distal colon (Fig. 3B) at 19–20 and 24–25 d, but not at 29–30 d.
The effect of MS on macromolecular permeability. Tissues proximal colon (A) and distal colon (B), from MS (▪) or NS (□) rat pups were studied in Ussing chambers. MS significantly increased the HRP flux across the distal colon of pups at 19–20 and 24–25 d of age compared with NS controls. There were no changes in the proximal colon. Values indicate means ± SE (n = 12–13), *p < 0.05.
MS resulted in bacterial adherence and penetration into the lamina propria.
Electron microscopic sections of the distal colon from all MS pups showed the presence of bacteria adhering to the epithelium and/or penetrating into the mucosa (Fig. 4 B, D, F); however, no such organisms were identified in any sections from NS pups (Fig. 4A, C, E). Bacterial adherence and penetration were confirmed by culturing washed segments of distal colon and enumerating bacterial colonies on blood agar after 24 h of incubation. A significant increase in numbers of CFUs was found in MS compared with NS pups at days 19–20, 24–25, and 29–30 d (Table 2). Table 2 also shows that greater bacterial translocation to the spleen was identified in MS versus NS pups at d 19–20 and 24–25, but not 29–30 d of age.
Electron photomicrographs showing bacterial penetration into the distal colonic mucosa. Bacteria were identified in the epithelium (Ep) and/or lamina propria (LP) of MS pups at d 19–20, 24–25, and 29–30 (B, D, F) but not in NS pups at any time point (A, C, E). These photomicrographs are representative of those obtained in six to eight pups per group.
MS induced an increase in MPO activity.
MPO values for colonic mucosa were significantly (p < 0.05) elevated in MS versus NS pups at 19–20 d of age, with a trend toward an increase at d 24–25 (Fig. 5 A).
The effect of MS on MPO activity and crypt length. Distal colon was obtained from MS (▪) or NS (□) pups. (A) MS significantly increased the activity of MPO in the mucosa of pups at 19–20 and 24–25 d of age compared with NS controls. (B) MS significantly increased the crypt length of pups at 19–20, 24–25, and 29–30 d of age compared with NS controls. Values indicate means ± SE (12–13 pups per group), *p < 0.05.
MS caused an increase in crypt length.
Since gut inflammation can stimulate proliferation of crypt stem cells increasing the length of the crypts in the small intestine (27,28), we conducted measurements on colonic sections by light microscopy. The crypt length in the distal colon was significantly (p < 0.05) increased in MS pups compared with NS pups at all three time points (Fig. 5B).
Effects of MS on colonic mucosal function are mediated by CRH receptors.
To determine the role of CRH receptors in the effects of MS on colonic mucosal dysfunction in rat pups, the animals were injected with α-helical CRH (9-41) antagonist or vehicle daily before exposure to MS. Studies were performed only at d 19–20. Administration of the antagonist resulted in significant (p < 0.05) decreases in Isc (saline 207 ± 23; αCRH 145 ± 25 μA/cm2), HRP flux (saline 30.0 ± 9.8; αCRH 10.1 ± 5.0 pmol/cm2/h), and bacterial adherence/penetration (saline 0.96 ± 0.17; αCRH 0.17 ± 0.10 CFUs (×106)/g tissue) (eight to 13 animals per group) (Fig. 6). There was no effect of α-helical CRH on values in NS pups. The antagonist also decreased the values for circulating corticosterone in MS pups (to 18.0 ± 9.8% of saline controls) but had no significant effect in NS pups (86.8 ± 13.8% of saline controls).
DISCUSSION
Our study identifies for the first time that exposing rat pups to neonatal MS causes an immediate and long-lasting disruption of distal colonic mucosal barrier function. MS pups displayed stimulated ion secretion and enhanced macromolecular permeability both during and after the MS period. In addition, we documented altered bacterial-epithelial interactions, including increased adherence and penetration of bacteria as indicated by both imaging and culture techniques. While some aspects of barrier function returned to normal within several days, impaired host defense to microbes persisted. Our finding that administration of a CRH receptor antagonist to rat pups at the time of separation inhibited the development of barrier defects implicates CRH receptor signaling in the mechanism leading to gut pathophysiology.
Studies in neonatal rats have reported a change in the circulating levels of corticosterone during development (26). During the stress-hyporesponsive period (d 4–14), the corticosterone response is almost entirely inhibited (29). Following this period, there is a concomitant rise in corticosterone levels (d 12–14) that tapers off by approximately d 22–24, coinciding with spontaneous weaning (26). The timing of these changes is thought to serve as a cue for changes in digestive enzymes that occur in the intestine in the third postnatal week (26). Our findings in rat pups exposed to the NS protocol were consistent with this literature, with elevated serum corticosterone levels at d 19–20, decreasing to normal adult levels by d 29–30. Compared with the controls, exposure of pups to MS resulted in significantly increased levels of corticosterone, indicating that these pups did indeed experience stress as a result of the separation. In addition, the values were still elevated 10 d after MS, indicating a long-lasting effect.
In the rat, there are distinct differences between the adult and immature colon in both structure and function, with both age- and region-related changes. There is a transient appearance of villi within the proximal colon during the first two postnatal weeks with the epithelial cells resembling ileal absorptive cells, while the distal colon never develops these villi and appears to have a more simple, flat mucosa (30). The transition to adult-like epithelium occurs during the third postnatal week, where the transient villi of the proximal colon are lost and the adult structure is established (30). These events may account for functional differences between regions of colon and at specific times after birth. In addition, there are differences in innervation between the proximal and distal colon (31). Developmental studies in rats have found an age-correlated decrease in net water and electrolyte transport in the colon (region not specified), which coincides with weaning (32), and high small intestinal permeability to macromolecules postnatally that decreases with the progress of gut closure (d 24–26) (33).
Our studies demonstrated a highly elevated Isc only in the distal colon, which reached the much lower adult levels at d 29–30 of age. This trend was not apparent for macromolecular permeability in either the proximal or distal colon. However, our studies clearly demonstrated that the distal colon of the immature rat is particularly sensitive to the effects of MS, with both Isc and HRP flux being significantly increased during MS (d 19–20) and after MS (d 24–25). With respect to the barrier, the uptake of the antigen-sized protein HRP was 5-fold greater in MS pups than in NS pups. Ten days later, these values for intestinal physiology had returned to the normal range. Subsequent studies focused on the distal colon.
We found that the distal colonic barrier defect in MS pups extended to host defense against microbes. Although it is known that bacterial uptake is greater in neonates than in older animals (34), we recorded a clear difference between MS and NS rats. Electron microscopy showed bacteria penetrating between and within distal colonic epithelial cells. There appeared to be more organisms in the mucosal tissues at the two earlier time points. This was confirmed by the growth of more CFUs at 19–20 d than at 24–25 d and fewer at 29–30 d. This penetration was detrimental to the host, as indicated by the numbers of CFUs translocating to the spleen. These alterations in host defense to bacteria are unlikely to be a direct effect of elevated glucocorticoids since another study in rats (35) demonstrated that s.c. placement of a corticosterone pellet alone did not affect bacterial translocation to the blood or viscera unless combined with thermal injury.
MPO activity in the mucosa was increased, suggesting a degree of inflammatory response to the uptake of microbes/microbial products. In addition, the crypt length was increased, a finding previously associated with activation of immune cells (27,28). These findings are similar to those described for adult rats in which exposure to chronic water avoidance stress (36) induced bacterial penetration into the mucosa and mild inflammation (37).
In our previous study (8), we reported that exposure to MS in neonatal rats resulted in their vulnerability as adults to develop colonic pathophysiology in response to acute stress; such changes were abrogated by a single i.p. injection of α-helical CRH (9–41) 30 min before stress exposure. This antagonist is thought not to cross the blood-brain barrier (38), suggesting that peripheral CRH receptors were involved in the intestinal response. Therefore, we were interested in examining the possible role of CRH receptors in gut dysfunction in immature animals. MS pups injected subcutaneously daily with CRH receptor antagonist demonstrated inhibition of colonic abnormalities. This implies that peripheral CRH receptors may also play a role in the colonic mucosal changes induced by MS. Other mediators such as nerve growth factor may also be involved (9). Further studies are required to determine the sequence of biochemical events and pathways leading to gut pathophysiology as a result of neonatal psychological trauma.
In conclusion, immature rats show alterations in intestinal parameters as a direct result of early life stress. Some aspects of pathophysiology recover within a short period of time; however, other aspects of barrier dysfunction are long lasting. The period of impaired barrier function could allow enhanced penetration of antigens and/or microbes into the body, resulting in immune stimulation. In later life, stress-induced reuptake of these antigens may lead to inflammation and associated symptoms such as visceral hypersensitivity. Our study provides further evidence implicating CRH in colonic dysfunction resulting from psychological stress.
Abbreviations
- CFUs:
-
colony forming units
- CRH:
-
corticotropin-releasing hormone
- HRP:
-
horseradish peroxidase
- IBS:
-
irritable bowel syndrome
- Isc:
-
short-circuit current
- MS:
-
maternal separation
- NS:
-
nonseparated
References
Kendler KS, Kuhn JW, Prescott CA 2004 Childhood sexual abuse, stressful life events and risk for major depression in women. Psychol Med 34: 1475–1482
Lowman BC, Drossman DA, Cramer EM, McKee DC 1987 Recollection of childhood events in adults with irritable bowel syndrome. J Clin Gastroenterol 9: 324–330
Koolhaas JM, Meerlo P, De Boer SF, Strubbe JH, Bohus B 1997 The temporal dynamics of the stress response. Neurosci Biobehav Rev 21: 775–782
Sanchez MM, Ladd CO, Plotsky PM 2001 Early adverse experience as a developmental risk factor for later psychopathology: evidence from rodent and primate models. Dev Psychopathol 13: 419–449
Kuhn CM, Schanberg SM 1998 Responses to maternal separation: mechanisms and mediators. Int J Dev Neurosci 16: 261–270
Huot RL, Thrivikraman KV, Meaney MJ, Plotsky PM 2001 Development of adult ethanol preference and anxiety as a consequence of neonatal maternal separation in Long Evans rats and reversal with antidepressant treatment. Psychopharmacology (Berl) 158: 366–373
Lovic V, Gonzalez A, Fleming AS 2001 Maternally separated rats show deficits in maternal care in adulthood. Dev Psychobiol 39: 19–33
Soderholm JD, Yates DA, Gareau MG, Yang PC, MacQueen G, Perdue MH 2002 Neonatal maternal separation predisposes adult rats to colonic barrier dysfunction in response to mild stress. Am J Physiol Gastrointest Liver Physiol 283: G1257–G1263
Barreau F, Cartier C, Ferrier L, Fioramonti J, Bueno L 2004 Nerve growth factor mediates alterations of colonic sensitivity and mucosal barrier induced by neonatal stress in rats. Gastroenterology 127: 524–534
Barreau F, Ferrier L, Fioramonti J, Bueno L 2004 Neonatal maternal deprivation triggers long term alterations in colonic epithelial barrier and mucosal immunity in rats. Gut 53: 501–506
Coutinho SV, Plotsky PM, Sablad M, Miller JC, Zhou H, Bayati AI, McRoberts JA, Mayer EA 2002 Neonatal maternal separation alters stress-induced responses to viscerosomatic nociceptive stimuli in rat. Am J Physiol Gastrointest Liver Physiol 282: G307–G316
Rosztoczy A, Fioramonti J, Jarmay K, Barreau F, Wittmann T, Bueno L 2003 Influence of sex and experimental protocol on the effect of maternal deprivation on rectal sensitivity to distension in the adult rat. Neurogastroenterol Motil 15: 679–686
Vazquez DM 1998 Stress and the developing limbic-hypothalamic-pituitary-adrenal axis. Psychoneuroendocrinology 23: 663–700
Plotsky PM, Meaney MJ 1993 Early, postnatal experience alters hypothalamic corticotropin-releasing factor (CRF) mRNA, median eminence CRF content and stress-induced release in adult rats. Brain Res Mol Brain Res 18: 195–200
Fukudo S, Nomura T, Hongo M 1998 Impact of corticotropin-releasing hormone on gastrointestinal motility and adrenocorticotropic hormone in normal controls and patients with irritable bowel syndrome. Gut 42: 845–849
Tache Y, Martinez V, Wang L, Million M 2004 CRF1 receptor signaling pathways are involved in stress-related alterations of colonic function and viscerosensitivity: implications for irritable bowel syndrome. Br J Pharmacol 141: 1321–1330
Castagliuolo I, Lamont JT, Qiu B, Fleming SM, Bhaskar KR, Nikulasson ST, Kornetsky C, Pothoulakis C 1996 Acute stress causes mucin release from rat colon: role of corticotropin releasing factor and mast cells. Am J Physiol 271: G884–G892
Santos J, Saunders PR, Hanssen NP, Yang PC, Yates D, Groot JA, Perdue MH 1999 Corticotropin-releasing hormone mimics stress-induced colonic epithelial pathophysiology in the rat. Am J Physiol 277: G391–G399
Udall JN, Pang K, Fritze L, Kleinman R, Walker WA 1981 Development of gastrointestinal mucosal barrier. I. The effect of age on intestinal permeability to macromolecules. Pediatr Res 15: 241–244
Sanderson IR, Walker WA 1993 Uptake and transport of macromolecules by the intestine: possible role in clinical disorders (an update). Gastroenterology 104: 622–639
Kiliaan AJ, Saunders PR, Bijlsma PB, Berin MC, Taminiau JA, Groot JA, Perdue MH 1998 Stress stimulates transepithelial macromolecular uptake in rat jejunum. Am J Physiol 275: G1037–G1044
Kim JW, Jeon WK, Kim EJ 2005 Combined effects of bovine colostrum and glutamine in diclofenac-induced bacterial translocation in rat. Clin Nutr, in press
Yang PC, Berin MC, Yu L, Perdue MH 2001 Mucosal pathophysiology and inflammatory changes in the late phase of the intestinal allergic reaction in the rat. Am J Pathol 158: 681–690
Smith JW, Castro GA 1978 Relation of peroxidase activity in gut mucosa to inflammation. Am J Physiol 234: R72–R79
Bradley PP, Priebat DA, Christensen RD, Rothstein G 1982 Measurement of cutaneous inflammation: estimation of neutrophil content with an enzyme marker. J Invest Dermatol 78: 206–209
Henning SJ 1978 Plasma concentrations of total and free corticosterone during development in the rat. Am J Physiol 235: E451–E456
Thompson FM, Catto-Smith AG, Moore D, Davidson G, Cummins AG 1998 Epithelial growth of the small intestine in human infants. J Pediatr Gastroenterol Nutr 26: 506–512
Thompson FM, Mayrhofer G, Cummins AG 1996 Dependence of epithelial growth of the small intestine on T-cell activation during weaning in the rat. Gastroenterology 111: 37–44
Levine S 2001 Primary social relationships influence the development of the hypothalamic–pituitary–adrenal axis in the rat. Physiol Behav 73: 255–260
Colony PC, Kois JM, Peiffer LP 1989 Structural and enzymatic changes during colonic maturation in the fetal and suckling rat. Gastroenterology 97: 338–347
Hata F, Kataoka T, Takeuchi T, Yagasaki O, Yamano N 1990 Differences in control of descending inhibition in the proximal and distal regions of rat colon. Br J Pharmacol 101: 1011–1015
Finkel Y, Aperia A, Eklof AC 1985 Development of colonic fluid and electrolyte transport: influence of weaning pattern. J Pediatr Gastroenterol Nutr 4: 457–462
Henning SJ 1987 Functional Development of the Gastrointestinal Tract. In: Johnson LR (ed) Physiology of the Gastrointestinal Tract. Raven Press, New York, pp 285–297
Wenzl HH, Schimpl G, Feierl G, Steinwender G 2001 Time course of spontaneous bacterial translocation from gastrointestinal tract and its relationship to intestinal microflora in conventionally reared infant rats. Dig Dis Sci 46: 1120–1126
Jones WG, Minei JP, Richardson RP, Fahey TJ 3rd, Calvano SE, Antonacci AC, Shires GT 3rd, Shires GT 1990 Pathophysiologic glucocorticoid elevations promote bacterial translocation after thermal injury. Infect Immun 58: 3257–3261
Santos J, Benjamin M, Yang PC, Prior T, Perdue MH 2000 Chronic stress impairs rat growth and jejunal epithelial barrier function: role of mast cells. Am J Physiol Gastrointest Liver Physiol 278: G847–G854
Soderholm JD, Yang PC, Ceponis P, Vohra A, Riddell R, Sherman PM, Perdue MH 2002 Chronic stress induces mast cell-dependent bacterial adherence and initiates mucosal inflammation in rat intestine. Gastroenterology 123: 1099–1108
Baram TZ, Mitchell WG, Brunson K, Haden E 1999 Infantile spasms: hypothesis-driven therapy and pilot human infant experiments using corticotropin-releasing hormone receptor antagonists. Dev Neurosci 21: 281–289
Author information
Authors and Affiliations
Corresponding author
Additional information
This research was supported by grants from the Crohn's and Colitis Foundation of Canada and AstraZeneca Pharma Sweden.
Rights and permissions
About this article
Cite this article
Gareau, M., Jury, J., Yang, P. et al. Neonatal Maternal Separation Causes Colonic Dysfunction in Rat Pups Including Impaired Host Resistance. Pediatr Res 59, 83–88 (2006). https://doi.org/10.1203/01.pdr.0000190577.62426.45
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.pdr.0000190577.62426.45
This article is cited by
-
Maternal separation and TNBS-induced gut inflammation synergistically alter the sexually differentiated stress response in rats
BioPsychoSocial Medicine (2023)
-
Maternal separation leads to dynamic changes of visceral hypersensitivity and fecal metabolomics from childhood to adulthood
Scientific Reports (2023)
-
Dysbiosis and Alzheimer’s Disease: Cause or Treatment Opportunity?
Cellular and Molecular Neurobiology (2022)
-
Opioid Use, Gut Dysbiosis, Inflammation, and the Nervous System
Journal of Neuroimmune Pharmacology (2022)
-
Sexual dimorphism in maternally separated rats: effects of repeated homotypic stress on gastrointestinal motor functions
Experimental Brain Research (2021)