Abstract
Zinc (Zn) treatment given together with acute ethanol in early pregnancy has previously been demonstrated to protect against physical birth abnormalities in mice. The current study examined whether this Zn treatment (s.c. injection) can also prevent the more subtle cognitive impairments caused by ethanol exposure in early pregnancy. Pregnant C57BL/6J dams were injected with saline (0.85% wt/vol NaCl) or 25% ethanol (0.015 mL/g body weight) intraperitoneally at 0 and 4 h on gestational d (GD) 8. ZnSO4 (2.5 μg Zn/g at 0 h) treatment was administered by s.c. injection immediately following ethanol treatment. Offspring were randomly selected from litters for each of the three treatment groups and were tested at 55 and 70 d of age using a cross-maze water escape task for spatial learning and memory impairments consecutively. No differences were observed between treatments for the spatial learning task. However, young adult mice exposed to ethanol in utero demonstrated impaired spatial memory, with a decrease in correct trials and increased escape latency and incorrect entry measurements, compared with saline-treated controls. In comparison, offspring given s.c. Zn treatment at the time of ethanol exposure were not cognitively impaired, performing at the same level as control mice in the cross-maze escape task. These findings indicate that critically timed Zn administration can limit spatial memory impairments caused by ethanol exposure in early pregnancy.
Similar content being viewed by others
Main
The teratogenic nature of ethanol has been well documented in humans and experimental animals (1–3). Consumption of ethanol during pregnancy can produce an array of physical abnormalities, including prenatal and/or postnatal growth deficiency and craniofacial dysmorphology (4). However, cognitive and behavioral impairments, such as deficits in attention, learning, and memory (5) are much more commonly observed in children exposed prenatally to ethanol and hence are more significant and costly to both the individual and community. These outcomes result from diverse maternal drinking patterns, ranging from the episodic "binge" of large quantities of ethanol over a short time period to chronic ethanol intake.
The mechanisms involved in ethanol-related abnormalities are unclear. Although it is likely that many factors are involved, several lines of evidence support fetal Zn deficiency as a major contributing factor to ethanol teratogenicity. First, an adequate supply of Zn to the fetus is critical during pregnancy (6). In rodents, there are similarities in fetal outcome between prenatal Zn deficiency and prenatal ethanol exposure. These include increased fetal resorptions, low birth weight, and birth abnormalities (7–10). These effects are potentiated during organogenesis (GD 7–12 in rodents, weeks 3–9 in humans), a period during early pregnancy critical for development and cell differentiation.
Second, studies in rats (11) and in our laboratory using mice demonstrate that acute ethanol exposure in early pregnancy causes fetal Zn deficiency via the induction of the Zn binding protein metallothionein (MT) I and II in the maternal liver. Following increased expression of MT, Zn is sequestered by MT and redistributed to the liver, causing plasma Zn concentrations to decrease by up to 65% over 16 h. This limitation in fetal Zn supply from the maternal plasma is associated with an increased incidence of physical abnormalities in ethanol-treated MT+/+ mice (27%) compared with saline-treated mice (6.4%). Furthermore, ethanol-treated MT knockout (MT−/−) mice that cannot express MT exhibited a low incidence of abnormalities (2.2%), due to the absence of a MT-induced Zn deficiency (12). The involvement of Zn deficiency is further supported by findings that the transfer of 65Zn to the fetus was significantly impaired and the total fetal zinc reduced, after alcohol exposure in MT+/+ mice (13) and rats (11), but not in MT−/− mice (13). In addition, s.c. Zn treatment at the time of ethanol exposure on GD8 prevents the physical abnormalities caused by ethanol by increasing plasma Zn concentrations up to fivefold during the period of transient Zn deficiency (14). This raises the critical question addressed in the present study of whether s.c. Zn treatment can also prevent cognitive impairments caused by ethanol consumption during early pregnancy. Although the central nervous system (CNS) is only in the very early stages during organogenesis, studies have shown that ethanol exposure during this period can result in behavioral impairments (15–17) as well as alterations in brain structure (16,18). The etiology of these cognitive impairments, such as spatial learning and memory deficits, which have been demonstrated in humans (19,20) and experimental animals (15,16,21), are yet to be associated with impaired maternal Zn homeostasis, as previously demonstrated with physical abnormalities.
Studies have shown associations between maternal Zn status and fetal neurodevelopment. Zn is critical for many processes involved in CNS development, such as neurogenesis, neuronal migration, and synaptogenesis and its deficiency could interfere with neurophysiological development (22–24). In humans, mild maternal Zn deficiency, assessed by serum and hair Zn, is associated with an increased frequency of neural tube defects, which may subsequently impair brain development (25). Zn deprivation in immature animals has been demonstrated to impair behavior, including learning, attention, and memory (26) similar to the effects of prenatal ethanol exposure. Studies have previously investigated low Zn status as a potential mediator of ethanol-related brain dysfunction and have shown that Zn supplementation with ethanol throughout pregnancy in rats results in increased cerebral weight and cerebral RNA content compared with ethanol alone. An increase in metabolic activity in the fetal hippocampus following Zn supplementation further indicated possible protection from impaired brain development (27). Furthermore, Zn repletion (20 mg Zn/d) in children (6–9 y) has been shown to improve performance in reasoning and visual recognition (28). This evidence supports a central role for Zn in cognitive development and relates to maternal factors that may influence this.
To establish whether prenatal Zn treatment can protect against spatial learning and memory deficits caused by early prenatal ethanol exposure, offspring were tested for cognitive impairments using a water-cross maze. Mice were exposed to ethanol on GD8 of pregnancy, which occurs during the critical period of organogenesis and corresponds approximately with the third week in human pregnancy. This is a time where women are more likely to unknowingly expose the fetus to alcohol, as they often do not know they are pregnant until the middle of the first trimester.
METHODS
Animals and mating procedure.
C57BL/6J mice were purchased from Institute of Medical and Veterinary Science (Adelaide, Australia). Mice were maintained at 22°C, subject to a 12-h light/dark cycle and were given unrestricted access to water and a commercial, nonpurified diet (Milling Industries, Adelaide, Australia), except when indicated during treatment. Mating was carried out by pairing females (aged 9–14 wk) with a proven male in separate cages. Females were examined every morning for the presence of a vaginal plug. Confirmation of a plug was designated as GD1, at which time females were separated from males and housed individually until the time of experimentation. All experimental procedures were approved by the Institute of Medical and Veterinary Science Animal Ethics Committee.
GD8 ethanol and Zn treatment: Spatial learning and memory testing.
Pregnant dams were assigned to one of three treatment groups: 1) saline, 2) ethanol, or 3) ethanol + Zn. On GD8, mice were injected with saline (0.85% wt/vol NaCl) or 25% ethanol in 0.85% saline vol/vol (0.015 mL/g) intraperitoneally at 0 and 4 h. The dose of ethanol administered results in a maximal blood alcohol concentration at 350 mg/dL, 30 min after the injection, which then declines 100 mg/dL/h for the next 3.5 h (12). Immediately after the first ethanol injection, the third group of mice was given an additional 250 μL s.c. injection in the nape of the neck of ZnSO4 in saline (2.5 μg Zn/g). An s.c. Zn injection gives an immediate and consistently reproducible increase in plasma Zn that peaks four- to fivefold normal 2 h after injection and declines to more than 50% of this at 4 h, returning to normal levels (14 μmol/L) by 12 h. We have found no evidence that these plasma Zn levels have a detrimental affect on pregnancy outcome (14). Food was removed after the first injection and returned after the second. Beginning on GD 19, cages were inspected twice daily for pups. The day that pups were found was noted as postnatal day (PN) 1 and litter size was recorded. All litters were culled to a maximum of eight pups. Pups were weaned at PN 21 and housed according to sex and treatment until testing. During the week before behavioral testing, offspring were inspected for any obvious physical abnormalities that could influence spatial performance in the maze (e.g. eyes partly or completely fused closed, which could impair their ability to view spatial cues required for spatial learning). Ten to 12 pups with no severe eye abnormalities (55 d of age) were randomly selected for each gender per treatment for behavioral testing (saline: 12 male and 12 female; ethanol: 12 male and 12 female; and ethanol + Zn: 12 male and 10 female). Mice were also handled every day for a week before testing to acclimatize them to their surroundings, including the presence of the experimenter. Mice were tested in two batches over a month.
Behavioral apparatus.
The protocol used was a modified place learning task that has been successfully used in mice (15). The apparatus consisted of a clear plastic cross maze (arm length = 26 cm, width = 20 cm) placed in a circular pool of water (1 m diameter, 23°C). A 90-cm high wall covered in black plastic incompletely surrounded the pool. The water was made opaque by powdered milk to conceal an escape platform (EP), which was submerged 0.5 cm below the surface of the water. The EP was located in the distal half of the east arm. Constant visual (spatial) cues were placed around the maze and were provided by various objects around the room and by the experimenter who always stood at the south arm.
Habituation (PN55).
During a habituation trial with no EP placed in the pool, the animals were allowed to swim for 60 s.
Acquisition/learning (PN56-60).
Mice were given a 5-d training period in which they were required to learn the position of the submerged EP from the other three (north, south, west) arms that did not contain the EP. Each mouse was given six daily trials (two blocks of three trials separated by a 30-min rest), in which each of the three arms were chosen as a starting point in a semirandomized pattern (twice daily). For each trial, the mouse was placed in the distal end of an arm facing the wall and allowed 60 s to reach the EP, where it remained for 10 s. Mice that did not climb onto the EP in the given time were placed on the EP for 10 s. The mouse was then placed in a cage for 10 s and subsequent trials were continued.
Long-term retention/memory (PN70-71).
Ten days after acquisition, animals were tested over 2 d of trials for long-term retention of the EP position, placed in its initial position during place learning.
Data were recorded for each mouse on their escape latency (i.e. time taken to swim to the platform), number of correct trials (i.e. if a mouse found the platform on the first attempt), and number of incorrect entries/reentries (i.e. the number of times that a mouse went into an arm that did not contain the EP). The three observations of spatial learning and memory were determined for each mouse (22–24 mice per treatment group) six times per day over 5 d of learning and 2 d of memory assessment. Approximately 720 measurements for learning and 288 measurements for memory were obtained for each treatment group. Only one operator was used to manually collect the cognitive data throughout the assessment period to reduce variation in data collection.
Statistical analysis.
One-way analysis of variance (ANOVA) was used to analyze litter size and body weight. Escape latency was analyzed by repeated measures ANOVA using generalized linear model (Minitab Statistics Software, Minitab Inc., State College, PA). Tukey's post hoc test was used to test for significance. Correct trials, which return a binary number (yes/no, whether they went directly to the escape platform), were analyzed using a generalized linear model assuming a binomial distribution and a logit link, given by logit (p) = log (p/1 − p). The data were presented as predicted proportions (the number of correct trials/the total number of trials). Incorrect entries were analyzed using a generalized linear model that assumes a Poisson distribution and were transformed using log (μ). The incorrect entry data were presented as means. Significant interactions and main effects were tested using Wald and deviance tests, respectively, which are approximately χ2 distributed. If a factor or interaction was found to be statistically significant, least significant difference (LSD) tests were used to determine where significant differences were occurring. Results are presented as mean ± standard of the mean (SEM) where applicable. Differences were considered to be significant at p < 0.05.
RESULTS
Litter size and body weights: Behavioral testing.
Table 1 summarizes the data for litter size and body weight of animals randomly selected for behavioral testing. On the day of birth (which usually occurred on GD 20), ethanol treatment had no effect on litter size compared with controls and was not different from ethanol + Zn. However, ethanol + Zn had larger litter sizes than controls (Table 1). Pups' weights were analyzed on postnatal d 7 (mean, 3.55 ± 0.11 g), d 14 (mean, 6.76 ± 0.17 g), and at d 21 (weaning) (mean, 7.78 ± 0.27 g), and no differences were found between the mean weights at these ages between treatment groups. At the time of behavioral testing when offspring were approximately 55 d old, all females randomly selected were of similar weight but weighed significantly less than males. Saline- and ethanol-treated males were lighter than ethanol + Zn-treated males (Table 1).
Spatial learning.
The escape latency, correct trials and incorrect entries/re-entries scores for each of the 5 d of spatial learning are shown in Figure 1. Mice from all treatment groups learnt the place-learning task, indicated by a reduction in the time taken to find the platform, a decrease in incorrect entries, and an increase in number of correct trials across the 5 d of testing. An effect of day was demonstrated for each of these parameters when correct trials, escape latency and incorrect entries were combined from all three treatments. There was no difference in performance between treatment groups on any day of testing, with all mice learning the place-task to the same level on the last day of training (Fig. 1).
Spatial learning: The effect of treatment on correct trials, incorrect entries and escape latency. Correct trial (A), incorrect entry (B), and escape latency (C) data over 5 d of spatial learning testing for offspring exposed to saline (♦), ethanol (▪), or ethanol + Zn (▴) on GD 8. Correct trials are presented as predicted proportions (i.e. the number of correct trials/total observations for each treatment). Escape latency and incorrect entries/reentries are presented as means ± SEM. Each point is the treatment group mean of the sums of six daily trials for each mouse; 22 to 24 mice were used per treatment. Correct trials increased and incorrect entries and escape latency decreased for each treatment over the 5 d of testing.
When all male data were compared with all female data independent of treatment group, an effect of gender (p < 0.05) was demonstrated for escape latency scores with females taking longer to find the platform than males (sex effect p < 0.05; female, 10.00 ± 0.29; male, 11.03 ± 0.31). There was no sex-treatment interaction. Furthermore, males did not differ from females in correct trial or incorrect entry scores. Therefore, data for males and females were combined to increase the sample size for comparison between treatments.
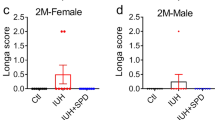
Long-term retention (spatial memory).
The escape latency, correct trial, and incorrect entry scores over the combined 2 d of testing for the three treatment groups are shown in Table 2. Deviance tests demonstrated that prenatal ethanol exposure impaired performance in the spatial memory test, with offspring taking significantly longer to find the platform and having more incorrect entries and fewer correct trials compared with saline treatment. In comparison, offspring treated prenatally with Zn at the time of ethanol exposure performed to the level as saline offspring in terms of shorter escape latencies, more correct trials, and fewer incorrect entries compared with ethanol-treated offspring (Table 2).
An effect of gender (p < 0.05) was demonstrated for each of the parameters over the 2 d of memory testing. Female offspring combined from all treatment groups took longer to find the platform than males. Furthermore, they also had fewer correct and more incorrect entries compared with males. However, there was no sex/treatment interaction, indicating that for any given treatment, there was no difference between the male or female data. An effect of day (p < 0.05) was demonstrated, with mice finding the escape platform more quickly on the first day of memory testing than on the second. However, there was no difference between the 2 d for correct trials and incorrect entries (Table 2).
DISCUSSION
The present study demonstrates that acute ethanol exposure to pregnant mice on GD 8 causes impairments in spatial memory in offspring tested at 55 d of age. Furthermore, s.c. Zn treatment of the mother at the time of ethanol exposure limited these cognitive impairments as assessed by our cross-maze protocol. This is evidenced by the fact that offspring exposed prenatally to ethanol and s.c. Zn treatment performed at the same level as the saline-treated offspring for all parameters measured in the cross-maze memory task.
The present study supports earlier findings that prenatal ethanol exposure impairs performance on spatial tasks (15,16,21). A similar study using the same cross-maze task in which C57BL/6 mice were exposed to ethanol on GD 9 demonstrated spatial memory impairments in aging but not in young mice (15). The fact that we detected impairments in young mice may be due to differences in testing procedure. For example, Dumas and Rabe (15) gavaged mice with one dose of ethanol, compared with two intraperitoneal injections administered in the present study, which we have found to cause 27% physical birth abnormalities per litter in offspring (12). The dose, administration technique, and day of insult in this study may therefore impair brain function to the extent that it is detectable in young mice. Furthermore, the period between learning the escape task and memory testing was 14 d shorter in our study, and this may have been a more favorable time frame to determine memory differences. Another study in which acute ethanol exposure was administered to pregnant rats on GD 8 similarly demonstrated spatial memory deficits in young rats, but only in females (16). Although a sex treatment effect was not found in the present study, females from all treatments took significantly longer to locate the platforms than males and is possibly attributable to their smaller body size.
It has been shown that ethanol consumption during pregnancy can also result in eye abnormalities (1,10,12,14) and motor impairments (3). It can be argued that these abnormalities may affect performance in the spatial navigation task. However, in the present study, we removed pups with any obvious eye impairments, as was also done by Dumas and Rabe (15). Furthermore, any undetectable eye abnormalities were unlikely to be an influence, as ethanol-exposed offspring demonstrated consistent learning of the place task similar to control offspring, which requires intact vision for processing of spatial cues. Starting the mice in a different arm for each trial and selecting these in a semi-random pattern ensured that they did not learn the escape platform position based on previous swimming pathways. Impaired swimming ability was also unlikely to cause deficits in spatial memory, as the time taken (escape latency) for all ethanol-treated offspring to locate the platform did not differ from that of normal mice.
This is the first study to demonstrate that prenatal Zn treatment limits cognitive impairments caused by early prenatal ethanol exposure on GD 8. Because of this, it is possible that the mechanisms by which ethanol in early pregnancy caused cognitive impairments are related to Zn metabolism. We have previously shown that ethanol exposure on GD 8 causes the induction of MT in the mother's liver. This leads to a decrease in the fetal Zn supply in the plasma for over 16 h as Zn is drawn into the liver (12). Zn is essential for many critical processes in brain development, such as the generation of neurons, migration of neurons to an appropriate location where they mature to their full form and function, and synaptogenesis in late pregnancy (22). A transient limitation in fetal Zn supply caused by ethanol exposure may impair critical stages in early neuronal development. In support of this, ethanol exposure during organogenesis has been demonstrated to inhibit neuronal differentiation and proliferation (29) and cause apoptosis in cell populations, such as the developing neural plate and primitive streak (30). Suppression of normal neural stem cell development has been similarly demonstrated by a deficiency of dietary Zn throughout pregnancy (31,32). This could interfere with subsequent developmental stages (migration or differentiation), leading to major structural changes in the brain. This might explain why others have shown that structures that begin to develop several days after ethanol exposure, such as the hippocampus (an area important for learning and memory) (33), are affected by ethanol (16,18). Anatomical changes in the hippocampus, including reduced numbers of neurons and abnormal arrangement of hippocampal mossy fibers, have been associated with alcohol exposure during pregnancy (18,33,34). Further research is required with MT−/− mice to demonstrate whether the spatial memory impairments caused by ethanol are associated with an MT-induced Zn deficiency, as previously demonstrated with physical abnormalities (12–14).
Regardless of the mechanism involved, administration of Zn at the time of ethanol exposure limited impairments in spatial memory. Although it is unclear how Zn treatment limited these defects, there are several possible mechanisms by which exogenous Zn may have had a protective effect. We have hypothesized that prenatal Zn treatment replenishes the fetal Zn supply, which is transiently depleted due to the induction by alcohol of MT in the mother's liver. As the s.c. Zn injection administered increases plasma Zn levels 5-fold that of normal (14), it is likely that this could offset the sequestration of Zn by induced levels of MT in the mother's liver and maintain relatively normal plasma Zn levels in the period immediately following ethanol exposure. However, the possibility that Zn has MT-independent effects on the developing brain cannot be overlooked. Zn is not only essential for growth and development but is also involved in antiapoptotic pathways (35–37). Thus, Zn treatment might promote cell survival, as shown when given with other teratogenic agents (36), to compensate for the alcohol-related brain disturbances, rather than directly limiting the actions of alcohol. Further studies are therefore warranted to determine whether Zn prevents alcohol-related structural damage by presumably limiting the transient Zn deficiency caused by MT induction or whether it independently stimulates the development of brain structure and function.
CONCLUSION
We have demonstrated that s.c. Zn treatment at the time of prenatal ethanol exposure in early pregnancy limits the adverse effects on spatial memory in young adult mice. Application of a binge-drinking model is highly relevant to the clinical setting where four to six drinks in one session in the first 3 to 9 wk of pregnancy (often before a woman knows she is pregnant) places the fetus at considerable risk. Furthermore, maintenance of appropriate Zn nutrition during pregnancy is critical for normal fetal development. Dietary intake of Zn is often lower than the recommended levels and when coupled with ethanol intake can have severe adverse consequences on the fetus. Our findings emphasize the importance of Zn for fetal brain development. Furthermore, they suggest that exogenous Zn may either offset ethanol-induced Zn deficiency or act through an independent mechanism to limit the effects of ethanol on brain development. Understanding the mechanism by which ethanol causes teratogenicity is important to consider possible intervention strategies. Further studies would be valuable to determine whether dietary Zn supplementation at different stages of pregnancy can protect against ethanol teratogenicity and furthermore to identify strategies for protecting against other teratogens that elicit an inappropriate maternal MT response early in pregnancy.
Abbreviations
- EP:
-
escape platform
- GD:
-
gestational day
- MT:
-
metallothionein
- PN:
-
postnatal day
- Zn:
-
zinc
References
Becker HC, Diaz-Granados JL, Randall CL 1996 Teratogenic actions of ethanol in the mouse: a minireview. Pharmacol Biochem Behav 55: 501–513
Dreosti IE 1993 Nutritional factors underlying the expression of the fetal alcohol syndrome. Ann N Y Acad Sci 678: 193–204
Streissguth AP, Landesman-Dwyer S, Martin JC, Smith DW 1980 Teratogenic effects of alcohol in humans and laboratory animals. Science 209: 353–361
Clarren SK, Smith DW 1978 The fetal alcohol syndrome. Lamp 35: 4–7
Mattson SN, Riley EP 1998 A review of the neurobehavioral deficits in children with fetal alcohol syndrome or prenatal exposure to alcohol. Alcohol Clin Exp Res 22: 279–294
Vallee BL, Falchuk KH 1993 The biochemical basis of zinc physiology. Physiol Rev 73: 79–118
Beach RS, Gershwin ME, Hurley LS 1982 Reversibility of development retardation following murine fetal zinc deprivation. J Nutr 112: 1169–1181
Dreosti IE, Buckley RA, Chem HC, Record IR 1986 The teratogenic effect of zinc deficiency and accompanying feeding patterns in mice. Nutr Res 6: 159–166
Randall CL, Taylor WJ 1979 Prenatal ethanol exposure in mice: teratogenic effects. Teratology 19: 305–311
Sulik KK, Johnston MC, Webb MA 1981 Fetal alcohol syndrome: embryogenesis in a mouse model. Science 214: 936–938
Taubeneck MW, Daston GP, Rogers JM, Keen CL 1994 Altered maternal zinc metabolism following exposure to diverse developmental toxicants. Reprod Toxicol 8: 25–40
Carey LC, Coyle P, Philcox JC, Rofe AM 2000 Maternal ethanol exposure is associated with decreased plasma zinc and increased fetal abnormalities in normal but not metallothionein-null mice. Alcohol Clin Exp Res 24: 213–219
Carey LC, Coyle P, Philcox JC, Rofe AM 2000 Ethanol decreases zinc transfer to the fetus in normal but not metallothionein-null mice. Alcohol Clin Exp Res 24: 1236–1240
Carey LC, Coyle P, Philcox JC, Rofe AM 2003 Zinc supplementation at the time of ethanol exposure ameliorates teratogenicity in mice. Alcohol Clin Exp Res 27: 107–110
Dumas RM, Rabe A 1994 Augmented memory loss in aging mice after one embryonic exposure to alcohol. Neurotoxicol Teratol 16: 605–612
Minetti A, Arolfo MP, Virgolini MB, Brioni JD, Fulginiti S 1996 Spatial learning in rats exposed to acute ethanol intoxication on gestational day 8. Pharmacol Biochem Behav 53: 361–367
Vigliecca NS, Ferreyra Moyano H, Molina JC 1986 Acute prenatal alcohol exposure in rats: a behavioral study. Acta Physiol Pharmacol Ther Latinoam 36: 463–472
Diaz Perez H, Espinosa Villanueva J, Marchado Salas J 1991 Behavioral and hippocampal morphological changes induced by ethanol administered to pregnant rats. Ann N Y Acad Sci 625: 300–304
Streissguth AP, Sampson PD, Olson HC, Bookstein FL, Barr HM, Scott M, Feldman J, Mirsky AF 1994 Maternal drinking during pregnancy: attention and short-term memory in 14-year-old offspring? a longitudinal prospective study. Alcohol Clin Exp Res 18: 202–218
Uecker A, Nadel L 1998 Spatial but not object memory impairments in children with fetal alcohol syndrome. Am J Ment Retard 103: 12–18
Matthews DB, Simson PE 1998 Prenatal exposure to ethanol disrupts spatial memory: effect of the training-testing delay period. Physiol Behav 64: 63–67
Bhatnagar S, Taneja S 2001 Zinc and cognitive development. Br J Nutr 2: S139–S145
Frederickson CJ, Suh SW, Silva D, Frederickson CJ, Thompson RB 2000 Importance of zinc in the central nervous system: the zinc-containing neuron. J Nutr 130: 1471S–1483S
Pfeiffer CC, Braverman ER 1982 Zinc, the brain and behavior. Biol Psychiatry 17: 513–532
Srinivas M, Gupta DK, Rathi SS, Grover JK, Vats V, Sharma JD, Mitra DK 2001 Association between lower hair zinc levels and neural tube defects. Indian J Pediatr 68: 519–522
Golub MS, Keen CL, Gershwin ME, Hendrickx AG 1995 Developmental zinc deficiency and behavior. J Nutr 125: 2263S–2271S
Tanaka H, Inomata K, Arima M 1983 Zinc supplementation in ethanol-treated pregnant rats increases the metabolic activity in the fetal hippocampus. Brain Dev 5: 549–554
Sandstead HH, Penland JG, Alcock NW, Dayal HH, Chen XC, Li JS, Zhao F, Yang JJ 1998 Effects of repletion with zinc and other micronutrients on neuropsychologic performance and growth of Chinese children. Am J Clin Nutr 68: 470S–475S
Jing H, Li Y 2004 Effects of ethanol on mouse embryonic brain development and heat shock protein 73 expression. Toxicol In Vitro 18: 601–607
Dunty WC Jr, Chen SY, Zucker RM, Dehart DB, Sulik KK 2001 Selective vulnerability of embryonic cell populations to ethanol-induced apoptosis: implications for alcohol-related birth defects and neurodevelopmental disorder. Alcohol Clin Exp Res 25: 1523–1535
Wang FD, Bian W, Kong LW, Zhao FJ, Guo JS, Jing NH 2001 Maternal zinc deficiency impairs brain nestin expression in prenatal and postnatal mice. Cell Res 11: 135–141
Rogers JM, Taubeneck MW, Daston GP, Sulik KK, Zucker RM, Elstein KH, Jankowski MA, Keen CL 1995 Zinc deficiency causes apoptosis but not cell cycle alterations in organogenesis-stage rat embryos: effect of varying duration of deficiency. Teratology 52: 149–159
Berman RF, Hannigan JH 2000 Effects of prenatal alcohol exposure on the hippocampus: spatial behavior, electrophysiology, and neuroanatomy. Hippocampus 10: 94–110
West JR, Hodges CA, Black AC Jr 1981 Prenatal exposure to ethanol alters the organization of hippocampal mossy fibers in rats. Science 211: 957–959
Allington C, Shamovsky IL, Ross GM, Riopelle RJ 2001 Zinc inhibits p75NTR-mediated apoptosis in chick neural retina. Cell Death Differ 8: 451–456
Fernandez EL, Gustafson AL, Andersson M, Hellman B, Dencker L 2003 Cadmium-induced changes in apoptotic gene expression levels and DNA damage in mouse embryos are blocked by zinc. Toxicol Sci 76: 162–170
Truong-Tran AQ, Carter J, Ruffin RE, Zalewski PD 2001 The role of zinc in caspase activation and apoptotic cell death. Biometals 14: 315–330
Acknowledgements
The authors gratefully acknowledge the work of Kathryn Dowling from Biometrics SA for the statistics performed on the maze data.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by funding from the University of Adelaide.
Rights and permissions
About this article
Cite this article
Summers, B., Rofe, A. & Coyle, P. Prenatal Zinc Treatment at the Time of Acute Ethanol Exposure Limits Spatial Memory Impairments in Mouse Offspring. Pediatr Res 59, 66–71 (2006). https://doi.org/10.1203/01.pdr.0000190573.23893.13
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.pdr.0000190573.23893.13
This article is cited by
-
14-3-3ζ deficient mice in the BALB/c background display behavioural and anatomical defects associated with neurodevelopmental disorders
Scientific Reports (2015)
-
Locomotor hyperactivity in 14-3-3ζ KO mice is associated with dopamine transporter dysfunction
Translational Psychiatry (2013)
-
Neurodevelopmental and neuropsychiatric behaviour defects arise from 14-3-3ζ deficiency
Molecular Psychiatry (2012)