Abstract
Surfactant protein D (SP-D) is a collectin that plays an important role in the innate immune system. The role of SP-D in the metabolism of surfactant is as yet quite unclear. The aims of this study were to establish normal values of SP-D in the umbilical cord blood and capillary blood of mature newborn infants and to assess the influence of perinatal conditions on these levels. A total of 458 infants were enrolled in the present study. Umbilical cord blood was drawn at the time of birth and capillary blood at age 4 to 10 d. The concentration of SP-D in umbilical cord blood and capillary blood was measured by enzyme-linked immunosorbent assay. The median concentration of SP-D in umbilical cord blood was 392.1 ng/mL and was found to be influenced by maternal smoking and labor. The median concentration of SP-D in capillary blood was 777.5 ng/mL and was found to be influenced by the mode of delivery, the highest levels being observed in infants born by cesarean section. It was concluded that SP-D concentrations in umbilical cord blood and capillary blood are highly variable and depend on several perinatal conditions. Further studies are needed to elucidate the effect of respiratory distress and infection on SP-D concentrations.
Similar content being viewed by others
Main
Pulmonary surfactant is synthesized and secreted by alveolar type II epithelial cells and consists of approximately 90% lipid and 5-10% proteins (1). Four proteins, called SP-A to -D, have been identified. SP-B and SP-C have been characterized as hydrophobic polypeptides that enhance the adsorption of lipid to the surface of the alveoli, whereas SP-A and SP-D are hydrophilic and participate in the innate host defense immune system (2–4). SP-A and SP-D belong to the group of collectins, which are structurally very similar to complement protein C1q (5).
Collectins are oligomeric molecules consisting of carbohydrate recognition domains attached to collagen-like regions (5). In humans, three well-studied collectins are known at present (6). These are MBL, which is a serum protein, SP-A, and SP-D. SP-A and SP-D are mainly produced in the epithelial cells of the lungs, but SP-D is also found in epithelial cells and secretory glands in the gastrointestinal tract and in other tissues (7). SP-D plays an important role in the innate immune defense by binding to specific carbohydrate and lipid structures on the surface of microorganisms: bacteria, viral particles, fungi, and protozoa (8–11). This binding mediates effector mechanisms like aggregation, chemotaxis, mediation of phagocytosis, and permeabilization (12). Pulmonary infections in adults have been shown to cause significant changes in SP-D levels (13). Whether SP-D has a role in avoiding infections in newborn babies has to our knowledge not been investigated.
Both structural and promoter variants are known for the MBL gene, and several alleles correlate with low values of MBL in serum and lead to an increased risk of infectious diseases in otherwise healthy children (14,15). Three polymorphisms have been identified in the coding sequence of human SP-D: codons corresponding to amino acid residue 11 (Met11Thr), residue 160 (Ala160Thr), and residue 270 (Ser270Thr) in the mature protein. Two clinical studies have associated the SP-D variants of amino acid 11 with disease. The SP-D allele coding for methionine 11 has been associated with severe respiratory syncytial virus infection in infants, whereas threonine 11 has been suggested to increase susceptibility to tuberculosis (16,17). However, the connection between structural genetic variance and serum SP-D has not been investigated. We have performed a twin study comparing MBL and SP-D levels in 26 monozygotic and 36 dizygotic twins aged 6-9 y (18). The study showed a significant genetic influence on the serum levels of both MBL and SP-D, with a heritability level of approximately 90%.
Studies of amniotic fluid and lung tissue demonstrate increasing levels of SP-D with increasing gestational age (19–21). Levels of SP-A and D in amniotic fluid have therefore been suggested as markers of lung maturation (22,23). The levels of SP-A in umbilical cord blood also depend on gestational age and perinatal condition (24). However, the influence of gestational age and perinatal factors on SP-D levels has not been investigated previously.
The purpose of this study was to establish a normal range of SP-D in the umbilical cord blood and capillary blood of mature newborn infants. Furthermore, we wished to investigate the influence of perinatal factors on SP-D levels in mature newborn infants.
METHODS
Subjects.
Out of a total of approximately 3600 newborn infants born at Odense University Hospital from August 2000 to August 2001, 458 (13%) were entered into the present study. Informed consent was obtained from the parents before birth by the midwives. Infants born before 36 weeks of gestational age or infants with major anomalies were excluded. Umbilical cord blood was drawn immediately after birth. The midwives were instructed to draw blood preferably from the umbilical artery. Routinely, all newborns are seen at the local midwife center at the age of 4-10 d. Within the project, infants attending the largest midwife center in the county additionally had blood taken for SP-D measurement. The capillary blood was sampled from heel-prick. All samples were stored at −20°C until measurement of SP-D.
Methodology.
The SP-D concentrations in plasma were measured by enzyme-linked immunosorbent assay. The assay is based on pepsin-digested polyclonal rabbit anti-SP-D antibody as first-layer antibody, and monoclonal anti-SP-D antibody as detector antibody, as described earlier (13). The samples were tested in duplicates and accepted with a coefficient of variation of 5%.
Statistics.
Data were analyzed by use of the STATA program. The main purpose of the study was to determine normal values for SP-D levels in the umbilical cord blood and capillary blood of newborns, so the median values and variance were not known before the study. Our chosen sample size was therefore limited to the number of samples we could obtain during the time period of the study.
The Mann-Whitney U test was used to compare levels of SP-D between two groups and the nonparametric test for trend across ordered groups for more than two groups. The variance between SP-D levels in arterial, venous, and capillary blood was tested by use of Bland-Altman's plot with Pitman's test of difference in variance. Correlations between continuous variables and SP-D levels were analyzed by simple regression analysis. In all statistical methods, p ≤ 0.05 was considered significant. The results are expressed as medians (range) unless otherwise noted.
Ethical considerations.
Written informed consent was given for every child enrolled in the study. The study was conducted according to the Helsinki II recommendations and was approved by the Regional Committee for Research on Human Subjects in the Counties of Funen and Vejle.
RESULTS
A total of 458 infants were included in the study. Umbilical cord blood was drawn from 423 infants, and the median SP-D plasma concentration was 392.1 ng/mL (range <20-1544.7). Of the umbilical blood samples, 130 were from the artery, with median SP-D level of 359.0 ng/mL (range 88.3-1505.0). Venous umbilical blood sampling was performed in 263 cases, and the median SP-D level was significantly higher than in the arterial samples: 420.8 ng/mL (range <20-1544.7, p = 0.0013). For statistical purposes, the term “umbilical cord blood” was used for both arterial and venous samples, including 43 samples in which the label “arterial” or “venous” was missing. In 13 cases wherein both arterial and venous sampling was done, the term “umbilical cord blood” refers to arterial blood.
Capillary blood was sampled from 233 infants. The median SP-D level in capillary blood was 777.5 ng/mL (range 195.5-2669.1). This was significantly higher than in the umbilical cord blood (p < 0.00005). There was a significant correlation between the SP-D levels in umbilical cord blood and those in capillary blood (Bland-Altman, p < 0.0005). This correlation was found for both the arterial and the venous samples.
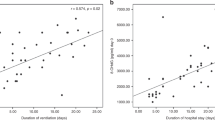
The infants' median gestational age was 40.3 weeks (range 36.0-43.4), and the median birth weight was 3600 g (range 1904-5164). We found significantly higher levels of SP-D in umbilical cord blood in the infants with lower gestational age (Fig. 1) (p < 0.005). However, regression analysis showed that the gestational age accounted for only 6.5% of the variation (p < 0.0005). There were no differences between different groups of gestational age with regard to the capillary SP-D levels. There was no correlation between birth weight and levels of SP-D in umbilical cord blood. The levels of SP-D in capillary blood decreased with increasing weight (p = 0.05).
SP-D levels in umbilical cord blood (n = 423) and capillary blood (n = 233) at different gestational ages. SP-D concentrations in umbilical cord blood were significantly lower (p < 0.005) in groups with higher gestational age. Bars indicate median (95% CI) SP-D concentration. ▪ Umbilical cord blood; □ Capillary blood.
Sixty-nine (15.6%) of the mothers had been smokers during pregnancy. The SP-D levels in umbilical cord blood (Table 1) of their infants were significantly lower than in infants of nonsmoking mothers (p = 0.025). This difference was found only in venous cord blood (p = 0.0078) and not in arterial cord blood (p = 0.989) (Table 2). The SP-D levels in umbilical cord blood (Table 1) were lower in infants born after more than 1 h of labor (p = 0.039). Ninety (19.7%) of the infants were delivered by cesarean section. The SP-D levels in umbilical cord blood did not differ according to mode of delivery, whereas the capillary SP-D (Table 3) was significantly higher in children delivered by cesarean section than in children delivered vaginally (p = 0.002). The infants delivered by cesarean section with rupture of membranes for more than 1 h had significantly lower levels of SP-D in the umbilical cord blood (p = 0.002).
Seven (1.5%) of the mothers had been treated with betamethasone on suspicion of premature labor 16-45 d before delivery. Maternal steroid treatment gave a tendency toward higher levels of SP-D in umbilical cord blood (p = 0.056) and in capillary blood. Only 4 infants had respiratory distress, and only 6 infants were treated with antibiotics on suspicion of septicemia within the first week of life. Their median SP-D level in capillary blood was almost twice as high as that of infants without respiratory distress or treatment with antibiotics, but the number was too small for statistical evaluation. None of the infants had proven septicemia.
The median age of the mothers was 29.9 y (range 18-44) at the time of delivery. The SP-D level in umbilical cord blood was lowest in the children of the youngest mothers (p = 0.04).
The capillary blood sampling was done at a median age of 6 d (range 0-11), and the SP-D level (Fig. 2) fell significantly from the time of birth (p < 0.0005).
DISCUSSION
We have in this study, to our knowledge for the first time, determined the SPD levels in umbilical cord blood and capillary blood from newborn infants. We found that the SP-D levels were highly variable, consistent with findings in healthy adult volunteers, and dependent on several maternal and perinatal conditions (13). The umbilical blood levels were found to depend on the mother's age and smoking habits, gestational age, and length of labor. Even though the study population was large (458 infants), a drawback of the study was the rather low inclusion rate of participation. However, the included infants did not differ from the whole population of mature newborn infants born during the study period with regard to gestational age, sex, and rate of cesarean section.
The capillary blood levels of SP-D were found to depend on the infants' birth weight, mode of delivery, and age at time of blood sampling. We found higher levels of SP-D in venous than in arterial umbilical cord blood, probably owing to the production of SP-D in the amniotic epithelium and choriodecidual layers (19,21). Increasing SP-D has been demonstrated in amniotic fluid with increasing gestational age (21,23). However, in these infants ≥36 wk of gestational age, we found decreasing amounts of SP-D in umbilical cord blood with increasing gestational age. This result probably reflects the decreasing amount of amniotic fluid in the fetal lungs toward term and perhaps a concomitant decrease in placental function resulting in decreasing SP-D production (25).
We found lower SP-D concentrations in umbilical cord blood of infants born after more than 1 h of labor. Uterine contractions have been reported to accelerate the secretion of pulmonary surfactant into the alveolar space and to decrease the amount of amniotic fluid by reabsorption of liquid across the pulmonary epithelium and outflow of liquid through the trachea (25–29). Three quarters of rat SP-D appears to exist in a soluble form, whereas 99% of rat SP-A exists in the form of a lipid protein complex (30). These findings may be related to the results of a clinical study of SP-A that showed elevated levels of SP-A with labor (24). These differences in SP-A and SP-D levels during labor could lead to the assumption that more SP-A is reabsorbed to plasma and more SP-D is transported by the outflow of liquid through the trachea. Furthermore, this assumption may also explain the decrease in SP-D observed in infants born by cesarean section more than 1 h after the rupture of membranes.
SP-D levels in infants with rupture of membranes for more than 1 h were not significantly lower than levels in infants without rupture of membranes before birth (p = 0.10), but a majority of the women had rupture of membranes for only a few hours (median 3 h). A study with a larger number of women with rupture of membranes for more than 24 h would be interesting because one would expect SP-D in umbilical cord blood to decrease further.
We found a trend (p = 0.056) toward increased levels of SP-D in umbilical cord blood of mothers treated with steroids, which was consistent with experimental data showing increased SP-D expression after glucocorticoid treatment both in vivo and in cultured tissue (31,32). The levels of SP-D in the lungs of newborn infants have been found to rise significantly during the first days of life (33,34). This is possibly the explanation for the high levels in capillary blood compared with umbilical cord blood.
Infection and asphyxia in neonates with respiratory distress syndrome are thought to worsen an already impaired surfactant system (35). Injury to the alveolar epithelial barrier, as seen in acute respiratory distress, will lead to increased permeability, allowing leakage of large amounts of plasma proteins into the alveolar space, and a considerable amount of alveolar surfactant components will permeate the circulation (36,37). SP-D may, because of its more hydrophilic nature, enter the vascular compartment more easily than SP-A and has therefore been suggested as a valuable plasma biomarker of lung injury (37,38). Consistently with these findings, we observed high capillary levels of SP-D in infants with respiratory distress or suspicion of infection. Mechanical ventilation of the lungs has been shown to increase SP-D production (39). Probably the pressure delivered to the lungs by the nasal continuous positive airway pressure used to treat respiratory distress has the same effect (40). The number of sick infants was limited by the scope of our present study, but an ongoing study of SP-D levels in prematurely born infants is expected to elucidate the usefulness of SP-D as a biomarker of respiratory distress syndrome and infection.
Morbidity caused by lack of SP-D has not been described in humans. In our study we found one single infant with an SP-D level <20 ng/mL. At the age of 1 year he was healthy, without any hospital visits. SP-D knockout mice show accumulation of surfactant lipids in the alveolar space, leading to emphysematous changes and increased susceptibility to infection (41,42). More clinical studies are needed to elucidate the effect in humans of low SP-D or absence of SP-D on pulmonary function and risk of infection.
Smoking during pregnancy decreases trophoblast proliferation and reduces the length of villous capillaries in the placenta, leading to diminished area for gas and nutrients exchange (43,44). Recently we have shown that SP-D is synthesized in all villous and extravillous trophoblast subpopulations in the placenta (19). In the present study, we found reduced SP-D levels in blood from the umbilical vein in smokers. This observation could have been due to reduced production or diminished transfer into the bloodstream. One could speculate whether the susceptibility of lung infections in infants of smoking mothers could be explained by these lower SP-D levels. However, the lower levels were found only in the umbilical venous blood and not in the umbilical arterial blood, which suggests that only the placental and not the fetal production of SP-D was affected.
In summary, we have in this study determined normal levels of SP-D in the blood of newborn infants born at term. Perinatal events may influence SP-D levels in opposing directions. Further studies with comparison of SP-D levels in the blood and in the mucosal tissues will be particularly interesting. Furthermore, the determination of SP-D levels in preterm infants, with their even more vulnerable innate as well as adaptive immune systems, may show more clearly the effects of variations in SP-D levels, as has been shown in experimental animals (45).
Abbreviations
- MBL:
-
mannan-binding lectin
- SP:
-
surfactant protein
- SP-D:
-
surfactant protein D
References
Crouch EC 1998 Structure, biologic properties, and expression of surfactant protein D (SP-D). Biochim Biophys Acta 1408: 278–289
Whitsett JA, Ohning BL, Ross G, Meuth J, Weaver T, Holm BA, Shapiro DL, Notter RH 1986 Hydrophobic surfactant-associated protein in whole lung surfactant and its importance for biophysical activity in lung surfactant extracts used for replacement therapy. Pediatr Res 20: 460–467
Kuroki Y, Voelker DR 1994 Pulmonary surfactant proteins. J Biol Chem 269: 25943–25946
van Golde LM 1995 Potential role of surfactant proteins A and D in innate lung defense against pathogens. Biol Neonate 67( Suppl 1): 2–17
Holmskov U, Malhotra R, Sim RB, Jensenius JC 1994 Collectins: collagenous C-type lectins of the innate immune defense system. Immunol Today 15: 67–74
Holmskov U, Thiel S, Jensenius JC 2003 Collectins and ficolins: humoral lectins of the innate immune defense. Annu Rev Immunol 21: 547–578
Madsen J, Kliem A, Tornoe I, Skjodt K, Koch C, Holmskov U 2000 Localization of lung surfactant protein D on mucosal surfaces in human tissues. J Immunol 164: 5866–5870
Lim BL, Holmskov U 1996 Expression of the carbohydrate recognition domain of bovine conglutinin and demonstration of its binding to iC3b and yeast mannan. Biochem Biophys Res Commun 218: 260–266
Reading PC, Holmskov U, Anders EM 1998 Antiviral activity of bovine collectins against rotaviruses. J Gen Virol 79( Pt 9): 2255–2263
Schelenz S, Malhotra R, Sim RB, Holmskov U, Bancroft GJ 1995 Binding of host collectins to the pathogenic yeast Cryptococcus neoformans: human surfactant protein D acts as an agglutinin for acapsular yeast cells. Infect Immun 63: 3360–3366
Reid KB 1998 Functional roles of the lung surfactant proteins SP-A and SP-D in innate immunity. Immunobiology 199: 200–207
Crouch EC 1999 Modulation of host-bacterial interactions by collectins. Am J Respir Cell Mol Biol 21: 558–561
Leth-Larsen R, Nordenbaek C, Tornoe I, Moeller V, Schlosser A, Koch C, Teisner B, Junker P, Holmskov U 2003 Surfactant protein D (SP-D) serum levels in patients with community-acquired pneumonia small star, filled. Clin Immunol 108: 29–37
Holmskov U, Jensenius JC, Tornoe I, Lovendahl P 1998 The plasma levels of conglutinin are heritable in cattle and low levels predispose to infection. Immunology 93: 431–436
Steffensen R, Thiel S, Varming K, Jersild C, Jensenius JC 2000 Detection of structural gene mutations and promoter polymorphisms in the mannan-binding lectin (MBL) gene by polymerase chain reaction with sequence-specific primers. J Immunol Methods 241: 33–42
Floros J, Lin HM, Garcia A, Salazar MA, Guo X, DiAngelo S, Montano M, Luo J, Pardo A, Selman M 2000 Surfactant protein genetic marker alleles identify a subgroup of tuberculosis in a Mexican population. J Infect Dis 182: 1473–1478
Lahti M, Lofgren J, Marttila R, Renko M, Klaavuniemi T, Haataja R, Ramet M, Hallman M 2002 Surfactant protein D gene polymorphism associated with severe respiratory syncytial virus infection. Pediatr Res 51: 696–699
Husby S, Herskind AM, Jensenius JC, Holmskov U 2002 Heritability estimates for the constitutional levels of the collectins mannan-binding lectin and lung surfactant protein D: a study of unselected like-sexed mono- and dizygotic twins at the age of 6-9 years. Immunology 106: 389–394
Leth-Larsen R, Floridon C, Nielsen O, Holmskov U 2004 Surfactant protein D in the female genital tract. Mol Hum Reprod 10: 149–154
Dulkerian SJ, Gonzales LW, Ning Y, Ballard PL 1996 Regulation of surfactant protein D in human fetal lung. Am J Respir Cell Mol Biol 15: 781–786
Miyamura K, Malhotra R, Hoppe HJ, Reid KB, Phizackerley PJ, Macpherson P, Lopez Bernal A 1994 Surfactant proteins A (SP-A) and D (SP-D): levels in human amniotic fluid and localization in the fetal membranes. Biochim Biophys Acta 1210: 303–307
Hallman M, Arjomaa P, Mizumoto M, Akino T 1988 Surfactant proteins in the diagnosis of fetal lung maturity: I. Predictive accuracy of the 35 kD protein, the lecithin/sphingomyelin ratio, and phosphatidylglycerol. Am J Obstet Gynecol 158: 531–535
Inoue T, Matsuura E, Nagata A, Ogasawara Y, Hattori A, Kuroki Y, Fujimoto S, Akino T 1994 Enzyme-linked immunosorbent assay for human pulmonary surfactant protein D. J Immunol Methods 173: 157–164
Cho K, Matsuda T, Okajima S, Matsumoto Y, Sagawa T, Fujimoto S, Kobayashi K 1999 Factors influencing pulmonary surfactant protein A levels in cord blood, maternal blood and amniotic fluid. Biol Neonate 75: 104–110
Pfister RE, Ramsden CA, Neil HL, Kyriakides MA, Berger PJ 2001 Volume and secretion rate of lung liquid in the final days of gestation and labour in the fetal sheep. J Physiol 535: 889–899
Callen P, Goldsworthy S, Graves L, Harvey D, Mellows H, Parkinson C 1979 Mode of delivery and the lecithin/sphingomyelin ratio. Br J Obstet Gynaecol 86: 965–968
Marino PA, Rooney SA 1981 The effect of labor on surfactant secretion in newborn rabbit lung slices. Biochim Biophys Acta 664: 389–396
Berger PJ, Smolich JJ, Ramsden CA, Walker AM 1996 Effect of lung liquid volume on respiratory performance after caesarean delivery in the lamb. J Physiol 492( Pt 3): 905–912
Kalache KD, Chaoui R, Marks B, Wauer R, Bollmann R 2002 Does fetal tracheal fluid flow during fetal breathing movements change before the onset of labour?. BJOG 109: 514–519
Kuroki Y, Shiratori M, Ogasawara Y, Tsuzuki A, Akino T 1991 Characterization of pulmonary surfactant protein D: its copurification with lipids. Biochim Biophys Acta 1086: 185–190
Ogasawara Y, Kuroki Y, Tsuzuki A, Ueda S, Misaki H, Akino T 1992 Pre- and postnatal stimulation of pulmonary surfactant protein D by in vivo dexamethasone treatment of rats. Life Sci 50: 1761–1767
Deterding RR, Shimizu H, Fisher JH, Shannon JM 1994 Regulation of surfactant protein D expression by glucocorticoids in vitro and in vivo. Am J Respir Cell Mol Biol 10: 30–37
Beresford MW, Shaw NJ 2003 Bronchoalveolar lavage surfactant protein a, B, and d concentrations in preterm infants ventilated for respiratory distress syndrome receiving natural and synthetic surfactants. Pediatr Res 53: 663–670
Wang JY, Yeh TF, Lin YC, Miyamura K, Holmskov U, Reid KB 1996 Measurement of pulmonary status and surfactant protein levels during dexamethasone treatment of neonatal respiratory distress syndrome. [See comments]. Thorax 51: 907–913
Konishi M, Chida S, Shimada S, Kasai T, Murakami Y, Cho K, Fujii Y, Maeta H, Fujiwara T 1992 Surfactant replacement therapy in premature babies with respiratory distress syndrome: factors affecting the response to surfactant and comparison of outcome from 1982-86 and 1987-91. Acta Paediatr Jpn 34: 617–630
Jobe A, Ikegami M, Jacobs H, Jones S, Conaway D 1983 Permeability of premature lamb lungs to protein and the effect of surfactant on that permeability. J Appl Physiol 55: 169–176
Eisner MD, Parsons P, Matthay MA, Ware L, Greene K, Acute Respiratory Distress Syndrome Network 2003 Plasma surfactant protein levels and clinical outcomes in patients with acute lung injury. Thorax 58: 983–988
Endo S, Sato N, Nakae H, Yamada Y, Makabe H, Abe H, Imai S, Wakabayashi G, Inada K, Sato S 2002 Surfactant protein A and D (SP-A, AP-D) levels in patients with septic ARDS. Res Commun Mol Pathol Pharmacol 111: 245–251
Awasthi S, Coalson JJ, Crouch E, Yang F, King RJ 1999 Surfactant proteins A and D in premature baboons with chronic lung injury (bronchopulmonary dysplasia): evidence for an inhibition of secretion. Am J Respir Crit Care Med 160: 942–949
Kamper J, Ringsted C 1990 Early treatment of idiopathic respiratory distress syndrome using binasal continuous positive airway pressure. Acta Paediatr Scand 79: 581–586
Botas C, Poulain F, Akiyama J, Brown C, Allen L, Goerke J, Clements J, Carlson E, Gillespie AM, Epstein C, Hawgood S 1998 Altered surfactant homeostasis and alveolar type II cell morphology in mice lacking surfactant protein D. Proc Natl Acad Sci U S A 95: 11869–11874
LeVine AM, Whitsett JA, Gwozdz JA, Richardson TR, Fisher JH, Burhans MS, Korfhagen TR 2000 Distinct effects of surfactant protein A or D deficiency during bacterial infection on the lung. J Immunol 165: 3934–3940
Larsen LG, Clausen HV, Jonsson L 2002 Stereologic examination of placentas from mothers who smoke during pregnancy. Am J Obstet Gynecol 186: 531–537
Shiverick KT, Salafia C 1999 Cigarette smoking and pregnancy: I. Ovarian, uterine and placental effects. Placenta 20: 265–272
Awasthi S, Coalson JJ, Yoder BA, Crouch E, King RJ 2001 Deficiencies in lung surfactant proteins A and D are associated with lung infection in very premature neonatal baboons. Am J Respir Crit Care Med 163: 389–397
Acknowledgements
The authors thank Ivan Iachine for statistical assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by grants from Direktør Ib Henriksens Foundation, Dagmar Marshalls Foundation, Gudrun Krauses Mindelegat, Overlægerådets legatudvalg, and Fonden for lægevidenskabelig forskning at Odense University Hospital
Rights and permissions
About this article
Cite this article
Dahl, M., Juvonen, P., Holmskov, U. et al. Surfactant Protein D in Newborn Infants: Factors Influencing Surfactant Protein D Levels in Umbilical Cord Blood and Capillary Blood. Pediatr Res 58, 908–912 (2005). https://doi.org/10.1203/01.PDR.0000181379.72900.EC
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.PDR.0000181379.72900.EC