Abstract
Erythema toxicum neonatorum is a common rash of unknown etiology affecting healthy newborn infants. In this study, we postulated that the rash reflects a response to microbial colonization of the skin at birth, and that the hair follicle constitutes an “easily opened door” for microbes into the skin of the newborn. We collected microbial cultures from the skin of 69 healthy, 1-d-old infants with and without erythema toxicum to identify the colonizing flora and correlate culture results with clinical findings. We also analyzed biopsies from lesions of erythema toxicum with scanning and transmission electron microscopy in the search for microbes. Finally, each infant's body temperature was measured as a sign of acute phase response. We found that 84% of 1-d-old healthy infants, with and without erythema toxicum were colonized with coagulase-negative staphylococci. In all lesions of erythema toxicum, TEM identified cocci-like bacteria localized in the hair follicle epithelium and into recruited immune cells surrounding the hair follicle; morphology and dimension supported their identification as belonging to the genus Staphylococcus. SEM revealed 10 times more hair structures per skin surface unit in newborns compared with adults. Infants with erythema toxicum also had higher body temperature. In erythema toxicum, commensal microbes gain entry into the skin tissue, most probably through the hair canal. This triggers the local immune system and a systemic acute phase response, including an increase in body temperature. We speculate that early microbial exposure to the newborn may be important for the maturation of the immune system.
Similar content being viewed by others
Main
Erythema toxicum neonatorum is an acute, self-limiting skin manifestation that develops in 50–70% of all healthy newborn infants, particularly those born at term (Fig. 1) (1). It starts soon after birth and disappears spontaneously within a few weeks without leaving sequelae. Infants with it have papulopustules on an intense erythematous base. The presence of the rash is often a matter of concern for parents with affected newborns and may be misinterpreted by healthcare professionals, leading to unnecessary investigations and inappropriate therapies. Its etiology has been attributed to hematological, toxic, and allergic factors but still remains to be determined (2–4). Histology shows a dense inflammatory infiltrate around hair follicles, composed mostly of eosinophils, but also containing neutrophils, macrophages, and dendritic cells, as well as an up-regulation of various inflammatory mediators such as IL-1, IL-8, eotaxin, psoriasin, and nitric oxide synthases 1–3 (5–8). The rash has been suggested to reflect a response to the presence, for the first time, of microbes on the skin of the newborn infant (8).
In this study, we postulated that the skin appendages, especially the hair follicles, might act as an entry port for microbes, thus eliciting a local and systemic inflammatory response. For that purpose, we 1) examined typical lesions of erythema toxicum by SEM and TEM to identify possible microbes on and/or into the skin tissue, 2) identified the colonizing flora on the skin surface of 1-d-old healthy newborns with and without erythema toxicum by collecting microbial cultures, and 3) measured the infants' body temperature at the same postnatal time, as a marker of systemic acute phase response.
METHODS
The study was approved by the local ethics committee of Karolinska Hospital, and informed consent was obtained from all parents. It included 69 healthy, exclusively breastfed, 1-d-old infants (≥24 < 48 h), 36 girls and 33 boys, with uncomplicated deliveries at term. Birth weight was adequate for gestational age and time from rupture of the membranes to birth was <24 h in all cases (data not shown). None of the babies were bathed before sample collection. None of the mothers received antimicrobial treatment before, during, or after delivery.
Electron microscopy.
Three-millimeter punch biopsies for electron microscopy analysis were obtained from the lower leg of seven infants, six with and one without erythema toxicum, after local anesthesia as previously described (6). Biopsies from four healthy adults were also collected from corresponding regions. Biopsies were immediately fixed in 2% glutaraldehyde and 0.5% paraformaldehyde in 0.1 M sodium cacodylate buffer + 0.1 M sucrose and 3 mM CaCl2 and processed for TEM, n = 5 (9), and SEM, n = 2 (10). The biopsies were serial sectioned, i.e. ultrathin sections were collected at 20-μm intervals.
Microbial cultures.
Skin swabs for microbial cultures were collected according to hospital routine from regions with erythema toxicum and from normal skin surface, but never from the region covered by the diaper. Axillary temperature was measured with a Terumo Digital Clinical Thermometer C402/C202 (Terumo Corporation, Tokyo, Japan).
RESULTS
SEM.
Visible microbes were not found either on the surface of the lesion or on normal skin. The number of visible hair structures/mm2 was 3.5 ± 0.08 in infants (n = 2) and 0.3 ± 0.15 (mean ± SD) in adults (n = 4) (Fig. 2).
TEM.
Serial ultrathin sections revealed accumulation of inflammatory cells in the extracellular matrix surrounding a hair follicle, i.e. mostly with morphologic features of eosinophils and macrophages but also of neutrophils and mast cells. These inflammatory cells were more or less always seen in the vicinity of the capillaries. Communication between cells was often found in these areas (Fig. 3a).
TEM of an erythema toxicum lesion; the biopsy was obtained from an infant with body temperature of 38.3°C and skin culture positive for CoNS at the time of the study. (a) Overview close to a hair follicle containing capillaries, single cells with morphologic features of polymorphonuclear leukocytes (P), macrophages (M), and eosinophils (E). Note the close proximity to blood vessels in the connective tissue sheath. Macrophages communicate with other cells (arrow). (b) High magnification showing activation of endothelial cell, i.e. increased numbers of pinocytotic vesicles (arrow). Bar: a = 15 μm, b = 0.5 μm.
Endothelial cells in the capillaries were prominent and the endothelial cytoplasm contained an increased numbers of pinocytic vesicles (Fig. 3b). Isolated bacteria were found, though rarely (Fig. 4, a and b).Cocci-like bacteria (diameter, 0.91 ± 0.35 μm; n = 21, mean ± SD) were found in all ultrathin sections (three to four per biopsy) phagocytized and internalized into the hair follicle epithelium and into recruited immune cells (Fig. 4, c–f).
TEM of an erythema toxicum lesion. (a) Overview showing the hair follicle containing hair cortex (H) surrounded by epithelial cells. One cell contains bacteria in the cytoplasm (arrow). (b) High magnification of cell in (a) showing a coccus-like bacteria with pili structures in the cytoplasm of an epithelial cell. (c) Overview of connective tissue (C) and epithelial cells in the hair follicle containing a cell with bacteria in the cytoplasm (arrow). (d) Higher magnification of cell in (c). (e) A phagosome body in the cytoplasm of a macrophage/dendritic cell containing bacteria-like material (arrow). (f) Three individual bacteria in the cytoplasm of epithelial cells in the hair follicle. N, nucleus. Bar: 15 μm (a), 10 μm (c), 1 μm (b, d, e, f).
Microbial cultures.
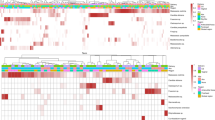
Bacteria most commonly isolated included CoNS (84%), Staphylococcus aureus (25%), Enterococcus species (19%), and α-Streptococcus (20%), with no difference noted between infants with (n = 33) and without rash (n = 36); for details see Figure 5. In 25 infants, 12 with rash and 13 without, CoNS was further typed and included mostly S. epidermidis (4 with rash and 7 without), S. hemolyticus (4 with rash and 6 without), and S. hominis, S. capitis, S. warneri, and S. lugdunensis in single cases. Direct microscopy and culture for fungi were negative in all these cases (data not shown).
Infants with rash had positive single cultures for bacteria in 33% (11/33)—nine for CoNS and one each for S. aureus and Micrococcus. Infants without the rash had single cultures in 19% (7/36), six for CoNS and one for P. agglomerans. Remaining infants harbored two to five different bacterial populations on the skin.
Body temperature.
Axillary temperature was higher in infants with the rash (37.6 ± 0.3°C, n = 33) than without the rash (37.3 ± 0.4°C, n = 36; p = 0.004, t test).
DISCUSSION
Bacteria most commonly isolated from the skin of healthy, 1-d-old infants with and without erythema toxicum included CoNS (84%), in particular S. epidermidis, S. aureus (25%), Enterococcus species (19%), and α-Streptococcus (20%). TEM revealed cocci-like bacteria with an average diameter of 0.9 μm located near or in the hair follicle epithelium and internalized into recruited immune cells in the lesions of erythema toxicum. These immune cells were located in close proximity to blood vessels and they were most prevalently eosinophils and macrophages, but also neutrophils and mast cells. The vessels were activated with numerous vacuoles in the endothelial cytoplasm. We also found that infants with erythema had significantly higher body temperature compared with infants without the rash.
CoNS are Gram-positive cocci with a diameter of 0.5–1.5 μm. They are commonly found living on human skin and mucous membranes. Staphylococci generally have a benign or symbiotic relationship with their host; however, in immunocompromised subjects they may gain entry into the host tissue and develop the lifestyle of a pathogen. This happens in preterm infants in which CoNS are a major cause of septicemia. We found that CoNS was the most frequent bacterial species growing on the skin of healthy 1-d-old infants and also the one most often growing as single culture compared with other species found, factors that may predispose this bacterial group to become invasive. However, we don't exclude that other commensal microbes, not yet identified, may be involved in erythema toxicum.
The transition from fetal to neonatal life includes the rapid colonization of microflora on skin and mucosal linings. A dynamic equilibrium of the flora with the host is established. The residential flora becomes beneficial, occupying a niche and denying access to transient, harmful, and infectious microbes, a phenomenon known as colonization resistance. Recent studies show that the skin appendages, especially the hair follicle, act as an immunologic sentinel for the skin. The follicle has a complex immunologic profile, including a complement of perifollicular immunocytes that act as the effector arm of the immune system (11). Lesions of erythema toxicum are found on the skin all over the entire body except the palms of the hands, soles of the feet, and the penis, all regions lacking hair follicles. This distinct localization, near the hair follicle, of both the inflammation and the found cocci-like microbes, strongly indicates that microbes gain access into the skin through the hair canal. Five million hair follicles cover the body of the newborn infant (12), which, in relation to the body surface, is 10 times more than in adults (Fig. 2). This, in concert with a huge, fetal adrenal DHEAS production (13, review 14) and an overproduction of sebum, seen as vernix caseosa, may facilitate the entry of microbes into the skin. During the course of our studies, we have observed that in skin biopsies of 3 mm, only one hair follicle is affected by erythema toxicum. Why some follicles become inflamed and others do not is unclear. Variation in the local microenvironment and bacterial load may be important. It may also reflect that only a limited number of microbes succeed in penetrating the tissue and/or the efficiency of the local immune system in protecting the host.
The higher body temperature of infants with rash compared with those without indicates a more powerful immunostimulation in the former. An elevation of the body temperature is part of the systemic inflammatory response to infection or tissue damage (15) and also to birth in the human newborn (16) and is believed to be a potent host defence (17).
Erythema toxicum has been studied for long time, but its etiology has remained enigmatic. Physicians of ancient Mesopotamia recognized the manifestation more than 1000 y ago, and Bartolomeus Metlinger described it in 1472 as being caused by “the unclean, noxious blood” of the mother (2). Leiner (1912) thought it due to a “toxic” gastrointestinal effect (3), and Mayerhofer (1927) interpreted it as an allergic manifestation (4). Here, we clearly show that it is due to the penetration of cocci-like microbes, probably CoNS, into the skin. We don't yet understand the meaning of this manifestation. Is it a temporary dysfunction of the hair follicle immune system and thus a failure to contain and limit the penetration of microbes into the skin? Or is it a way for the body to induce maturation of the immune system by well-orchestrated effector pathways favoring a healthy outcome in the host–microbe interplay at birth?
The present denomination of the rash—erythema toxicum—has a negative valour. And we can now say for sure that it is not toxic, but is the result of an acute, transitory attack of the commensal microflora. Therefore, we suggest a change of its actual denomination to, simply, erythema neonatorum.
Abbreviations
- CoNS:
-
coagulase-negative Staphylococcus
- SEM:
-
scanning electron microscopy
- TEM:
-
transmission electron microscopy
References
Harris JR, Schick B 1956 Erythema neonatorum. AMA J Dis Child 92: 27–33
Lehndorf H, Bartolomeus M 1951 Arch P. ediatr 68: 322–33.
Leiner C 1912 Uber eigenartige Erythemtypen und Dermatitiden des fruehen Säuglingsalters. F Deuticke, Leipzig-Wien, pp 4–15
Mayerhofer E 1927 Allergische Neugeborenen-exantheme. Arch Kinderheilk 111: 51
Freeman RG, Spiller R, Knox JM 1960 Histopathology of erythema toxicum neonatorum. Arch Dermatol 82: 586–589
Marchini G, Ulfgren AK, Loré K, Ståbi B, Berggren V, Lonne-Rahm S 2001 Erythema toxicum neonatorum: an immunohistological analysis. Pediatr Dermatol 18: 177–187
Marchini G, Lindow S, Brismar H, Ståbi B, Berggren V, Ulfgren AK, Lonne-Rahm S, Agerberth B, Gudmundsson GH 2002 The newborn infant is protected by an innate antimicrobial barrier: peptide antibiotics are present in the skin and vernix caseosa. Br J Dermatol 147: 1127–1134
Marchini G, Ståbi B, Kankes K, Lonne-Rahm S, Østergaard M, Nielsen S 2003 AQP1 and AQP3, psoriasin, and synthases 1-3 are inflammatory mediators in erythema toxicum neonatorum. Pediatr Dermatol 20: 377–384
Förster C, Mäkela S, Wärri A, Kietz S, Becker D, Hultenby K, Warner M, Gustafsson JÅ 2000 Involvement of estrogen receptor β in terminal differentiation of mammary gland epithelium. Proc Natl Acad Sci U S A 99: 15578–15583
Fang H, Edlund C, Hultenby K, Hedberg M 2002 Effects of cefoxitin on the growth and morphology of Bacteroides thetaiotaomicron strains with different cefoxitin susceptibility. Anaerobe 8: 55–61
Christoph T, Muller-Röver S, Audring H, Tobin DJ, Hermes B, Cotsarelis G, Ruckert R, Paus R 2000 The human hair follicle immune system: cellular composition and immune privilege. Br J Dermatol 142: 862–873
Paus R, Cotsarelis G 1999 Mechanisms of disease: the biology of hair follicles. New Engl J Med 12: 491–497
McNutt NS, Jones AL 1970 Observations on the ultrastructure of cytodifferentiation in the human fetal adrenal cortex. Lab Invest 22: 513–527
Irmak MK, Oztas E, Vural H 2004 Dependence of fetal hairs and sebaceous glands on fetal adrenal cortex and possible control from adrenal medulla. Med Hypotheses 62: 486–492
Baumann H, Gauldie J 1994 The acute phase response. Immunol Today 15: 74–80
Marchini G, Berggren V, Djilali-Merzoug R, Hansson LO 2000 The birth process initiates an acute phase reaction in the fetus-newborn infant. Acta Paediatr 89: 1082–1086
Kluger MJ, Kozak W, Conn CA, Leon LR, Soszynski D 1996 The adaptive value of fever. Infect Dis Clin North Am 10: 1–20
Acknowledgements
The authors thank Associate Professor Viveka Lindgren for critical advice.
Author information
Authors and Affiliations
Corresponding author
Additional information
Financial support was obtained from the Foundations Frimurarbarnhuset, Sällskapet Barnavård, and Kronprincessan Lovisas Fond.
Rights and permissions
About this article
Cite this article
Marchini, G., Nelson, A., Edner, J. et al. Erythema Toxicum Neonatorum Is an Innate Immune Response to Commensal Microbes Penetrated into the Skin of the Newborn Infant. Pediatr Res 58, 613–616 (2005). https://doi.org/10.1203/01.pdr.0000176836.27156.32
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.pdr.0000176836.27156.32
This article is cited by
-
Disrupted pathways associated with neonatal sepsis: Combination of protein-protein interactions and pathway data
BioChip Journal (2017)
-
Neonatal monocytes exhibit a unique histone modification landscape
Clinical Epigenetics (2016)
-
Kolonisation oder Infektion bei Früh- und Neugeborenen
Monatsschrift Kinderheilkunde (2014)
-
The role of the skin barrier in modulating the effects of common skin microbial species on the inflammation, differentiation and proliferation status of epidermal keratinocytes
BMC Research Notes (2013)
-
Attachment and Biofilm Forming Capabilities of Staphylococcus epidermidis Strains Isolated from Preterm Infants
Current Microbiology (2013)