Abstract
Insulin treatment of prepubertal children with insulin-dependent diabetes improves body protein balance by decreasing the rate of protein degradation without stimulating protein synthesis. However, insulin also causes hypoaminoacidemia, so the inability of insulin to stimulate protein synthesis may have been limited by substrate availability. We investigated the ability of insulin to stimulate protein synthesis in growing pubertal children who were given sufficient amino acids to counter insulin-induced hypoaminoacidemia. Protein metabolism in six pubertal children with type 1 diabetes was assessed from leucine kinetics during a primed, 6-h infusion of l-[1-13C]leucine. The children were studied in the postabsorptive state during a basal (insulin withdrawn) period and during the infusion of 0.83 mU · kg−1 · min−1 human regular insulin. Amino acids and glucose were given with insulin to prevent hypoaminoacidemia and hypoglycemia. Net leucine balance was significantly higher with insulin than in the basal state, the result of decreased protein degradation but also decreased protein synthesis. The data suggest that insulin alone does not increase protein synthesis in pubertal children with type 1 diabetes.
Similar content being viewed by others
Main
An association between protein catabolism and diabetes has been known for centuries. The Greek physician Aretaeus the Cappadocian described diabetes as a condition that causes “melting of flesh” into urine (1). Insulin treatment reverses the negative nitrogen balance associated with diabetes and increases lean body mass (2). Thus, it is widely accepted that insulin plays a major role in the regulation of protein metabolism.
In vitro and in vivo (animal and human) data regarding the mechanism of the anabolic effect of insulin are inconsistent and contradictory. In vitro studies suggest that insulin stimulates protein synthesis and inhibits protein degradation in muscle (3,4). In vivo animal studies indicate that insulin is capable of stimulating muscle protein synthesis in young, rapidly growing animals but not in adult animals (5–8). Studies of whole-body protein metabolism in adult humans with type 1 diabetes suggest that insulin only decreases protein breakdown but plays no role in increasing protein synthesis (9–12). In contrast to animals, insulin also failed to stimulate whole-body protein synthesis in prepubertal children with type 1 diabetes (13).
All of the above studies were carried out in the postabsorptive (fasting) state, when insulin infusion results in the reduction in the concentration of circulating amino acids (14,15). The inability of insulin to stimulate protein synthesis has been attributed to the limitation of protein synthesis by the low circulating concentration of amino acids that occurs with insulin administration in the fasting state. Consequently, several studies in adults were designed to evaluate the effect of insulin supplementation on protein metabolism during concomitant amino acid supplementation. These studies demonstrated an effect of insulin on decreasing proteolysis and increasing leucine oxidation; however, the effect of insulin on protein synthesis is less clear. Two studies in patients with insulin-dependent diabetes (16,17) showed an increase in protein synthesis, whereas the third study (18) failed to confirm this finding. Two studies in healthy control subjects (19,20) indicated an increase in whole-body protein synthesis when insulin and amino acids were infused, whereas the third study (21) did not confirm this finding. Furthermore, a study that was conducted in individuals with type 2 diabetes to assess protein kinetics over a 24-h period, including both fasting and feeding, suggested that the anabolic effect of insulin was provided through decreased protein degradation rather than increased protein synthesis (22).
In view of the studies in animals suggesting greater sensitivity to insulin in young, growing animals relative to mature animals, we undertook a study to investigate the role of insulin in regulating protein metabolism in pubertal children who have type 1 diabetes and were given insulin with sufficient amino acids to prevent hypoaminoacidemia. In this study, we assessed the effects of insulin with concomitant amino acid administration on whole-body protein determined from the kinetics of i.v. administered l-[1-13C]leucine.
METHODS
Human subjects.
Six pubertal male adolescents with type 1 diabetes were studied. Three were on continuous insulin infusion pumps with lys-pro insulin (Humalog), and three were on s.c. insulin injections with short- (lys-pro insulin, Humalog) and intermediate-acting insulin (NPH, Humulin N). Patient characteristics are described in Table 1. The study was performed in the Clinical Research Center, and the protocol was approved by the Committee of Research Involving Human Subjects, the institutional review board at the State University of New York at Stony Brook, New York. Written consent was obtained from parents, and assent from the patient after the purpose, nature, and potential risks of the study were explained.
Study protocol.
Patients were admitted to the General Clinical Research Center on the day preceding the study. For patients who were on s.c. insulin injections, the last dose of intermediate- and short-acting insulin was administered 24 and 12 h, respectively, before the beginning of the study. For patients who were on continuous s.c. insulin infusions, the infusion was discontinued 2 h before study. All patients were studied after an overnight fast.
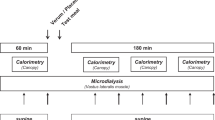
For assess whole-body protein kinetics, l-[1-13C]leucine was infused as previously described (23). The study consisted of 180 min of basal period (−180 to 0 min), when only tracer (l-[1-13C]leucine) was infused, and 180 min of infusion period (0–180 min), when insulin and amino acids were infused continuously along with l-[1-13C]leucine tracer.
On the morning of study, a vein of the left forearm was cannulated and used for the infusion of l-[1-13C]leucine, insulin, glucose, and amino acid. A vein of the opposite hand was cannulated in a retrograde manner, and the hand was maintained warm for arterialized venous blood sampling (24). This site was also used for frequent glucose monitoring.
At −180 min, a priming dose of l-[1-13C]leucine (6 μmol/kg; Mass Trace, Woburn, MA) was administered followed by a continuous infusion (6 μmol · kg−1 · h−1) throughout the study period by means of Harvard pump (Harvard Apparatus, South Natick, MA). After 180 min of basal period, a continuous i.v. infusion of human regular insulin was started at 0.05 units · kg−1 · h−1 (0.83 mU · kg−1 · min−1) along with an amino acid solution (8.5% FreAmine III; B. Braun Medical, Irvine, CA) at 6.72 mg · kg−1 · h−1 N (containing leucine infused at 31 μmol · kg−1 · h−1) for an additional 180 min. Blood glucose concentration was monitored every 15 min during the 3 h of insulin infusion by a Beckman glucose analyzer (Beckman Instruments, Fullerton, CA), and potato starch–derived 10% dextrose solution was prepared to administer if necessary to prevent hypoglycemia. This source of dextrose has a low natural abundance of 13C glucose as opposed to corn-derived dextrose, which is enriched with 13C glucose as a result of the photosynthetic pathway of corn (25). Thus, this source of dextrose would not contribute to the abundance of 13CO2 in expired breath assumed to be oxidation of tracer (13C leucine). Only one patient required infusion of dextrose and only in the last 10 min of the study period.
Arterialized venous blood samples were collected before the start of tracer infusion and at −45, −30, −15, and 0 min during the last hour of the basal period and during the insulin and amino acid infusion at 135, 150, 165, and 180 min for the determination of 13C leucine, α-ketoisocaproate (KIC) enrichment, and amino acid concentration. At the same time period, samples of expired air were collected into evacuated glass vacutainer tubes for the determination of 13CO2 isotopic enrichment. Blood samples were collected before the start of tracer infusion (−180 min), at the end of the basal period (0 min), and periodically during the insulin infusion for determination of insulin concentration. The rate of CO2 production was determined by respiratory gas exchange using a ventilated hood (Delta Track Respiratory Gas Monitor, Yorba Linda, CA) on multiple occasions during the basal and infusion periods.
Analytical determination.
Plasma glucose was measured at the bedside with a glucose oxidase method and a Beckman II glucose analyzer. Plasma insulin was determined by RIA with kits from Diagnostic Products Corp. (Los Angeles, CA).
The enrichment of l-[1-13C]leucine and KIC from the plasma was measured as described previously (26). Briefly, the enrichments of l-[1-13C]leucine and 13C-KIC were determined with a VG MD 800 quadrupole gas chromatography mass spectrometry (Fisons MD 800, San Jose, CA) after conversion to the tertiary butyldimethylsilyl and quinoxalinol tertiary butyldimethylsilyl derivatives, respectively. The abundance of 13CO2 in breath was measured by gas isotope ratio–mass spectrometry at the General Clinical Research Center at the University of Vermont with a VG SIRA II Isotope Ratio Mass Spectrometer (Middlewich, Cheshire, UK) as described previously (27). Plasma amino acid concentrations were determined by HPLC.
Calculations.
All kinetic data were calculated at near steady-state conditions of [13C]leucine and [13C]KIC isotopic enrichment in the plasma and 13CO2 isotopic enrichment in expired air achieved during the last hour of the basal and infusion periods. All calculations were based on the mean values of KIC isotopic enrichment in the plasma and of 13CO2 production in the expired air at the steady state. Plasma α-KIC, a transaminated product of leucine, is used because the plasma enrichment of α-KIC closely resembles that of intracellular [13C]leucine (28). Data were analyzed with a stochastic model as described in detail previously (23,26,29–31). Endogenous leucine flux (Q) was calculated with the equation
Q (μmol · kg−1 · h−1 leucine) = i Ei/Ep where i is the amount of leucine infused (6 μmol · kg−1 · h−1), Ei is the tracer isotopic enrichment [in moles % excess (MPE)], and Ep is the leucine (or KIC) isotopic enrichment in the plasma (in MPE). The contribution of infused leucine was subtracted from Q to obtain endogenous flux. The rate of leucine oxidation was derived from the rate of expired 13CO2 (μmol · kg−1 · h−1), and the plasma KIC enrichment was obtained with a correction of incomplete recovery of body bicarbonate (23). Nonoxidative leucine disposal (NOLD; or protein synthesis) and leucine derived from protein degradation were calculated from Q with the equation (Q) = NOLD + oxidation = protein degradation + leucine intake. Leucine intake was the amount of leucine provided by the amino acid infusion (31 μmol · kg−1 · h−1). Net leucine balance, an index of net protein accretion or anabolism, was calculated as protein degradation − protein synthesis (NOLD).
The enrichment of plasma leucine is known to be higher than the enrichment of leucine at the site of protein synthesis and leucine oxidation. The enrichment of KIC has been used in the calculation of leucine kinetics, because it is more likely to represent the enrichment of leucine within the tissue, as suggested by Matthews et al. (28). A recent study reported that the enrichment of KIC in muscle tissue was higher than that of leucyl-tRNA (32). This would mean that the rates of protein synthesis based on KIC enrichment underestimate the true rate of protein synthesis.
Statistics.
Two-tailed paired t test was used to compare data in the basal and infusion periods. Data are expressed as mean ± SEM. The mean value of KIC enrichment during the last hour of both the basal and the infusion periods was used for calculations of leucine kinetics. p < 0.05 was considered significant.
RESULTS
With the withdrawal of insulin, the concentration of plasma glucose was elevated and the concentration of serum insulin was low in all patients. The changes in plasma glucose (six patients) and insulin (four patients) during the infusion of insulin are shown in Fig. 1. In one patient, insulin levels were determined only at the beginning and the end of the insulin infusion. Data from this patient were included in the estimate of changes in insulin levels, but the data are not shown in Fig. 1. A second patient had insulin antibodies. In this patient, insulin levels were determined after precipitation of insulin antibodies, followed by acid treatment to release insulin free of circulating antibodies (ARUP Laboratories, Salt Lake City, UT). As expected, when insulin was infused, plasma glucose decreased significantly [from 20 ± 3.3 mM (360 ± 59 mg/dL) to 10 ± 0.83 mM (180 ± 15 mg/dL; p < 0.001] and plasma insulin concentration increased (from 3.99 ± 1.75 to 58.3 ± 8.52 μU/lm; p < 0.001).
Change in plasma glucose and insulin concentrations. Plasma concentrations of glucose (mg/dL; n = 6) and insulin (FU/mL; n = 4) in pubertal children with type 1 diabetes. All patients were withdrawn from insulin (see “Study Protocol”). From 0 to 180 min, patients received an i.v. infusion of 0.83 mU · kg−1 · min−1 regular insulin with an amino acid mixture (8.5% FreAmine III) that supplied 6.72 mg · kg−1 · h−1 N. Plasma glucose and insulin were determined as described in “Methods.”
Under basal (insulin withdrawn) conditions, the total plasma amino acid concentration was 2075 ± 362 μM, whereas branched-chain amino acid (BCAA) were 537 ± 89 μM (Table 2). During the infusion of insulin and amino acids, total and BCAA were 2200 ± 234 and 476 ± 50 μM, respectively, both of which were not significantly different from the basal period (p = 0.17 for total and 0.57 for BCAA). With regard to individual amino acids, alanine, glycine, phenylalanine, and tryptophan increased by 27.3, 36.5, 26.5, and 33.9% (p = 0.05, 0.018, 0.017, and 0.006), respectively, whereas leucine and tyrosine were decreased by 20 and 25.9% (p = 0.036 and 0.016), respectively.
Steady state for [13C]leucine and KIC isotopic enrichment in the plasma (Fig. 2) and 13CO2 isotopic enrichment in expired air were achieved during the last hour of the basal and the infusion periods. None of the values for enrichment of KIC during the last hour of infusion was significantly different (ANOVA, p = 0.6). The [13C]leucine and KIC isotopic enrichment were significantly different from each other both in the basal state (4.45 ± 0.14 versus 4.14 ± 0.19 MPE; p = 0.005) and during the infusion of amino acids (4.64 ± 0.16 versus 4.31 ± 0.16; p = 0.008) with the ratio of KIC to [13C]leucine enrichment 0.93 ± 0.17 and 0.93 ± 0.16 during the basal and infusion periods, respectively.
Time-related changes in plasma [13C]leucine and KIC isotopic enrichment during the basal and infusion periods. [13C]leucine and KIC enrichments were determined with gas chromatography–mass spectrometry as described in “Methods.” The data are displayed as the mean MPE with SEM for six patients who received 6 Fmol · kg−1 · min−1 [13C]leucine. Samples that were taken before l-[13C]leucine infusion were used to determine the natural abundance of [13C]leucine. The basal period and the period of insulin + amino acid infusion were as described in the legend to Fig. 1.
The enrichment of plasma KIC was used in the calculation of leucine kinetics, but the conclusions would be similar if the assessment were based on the enrichment of plasma leucine. Parameters of protein metabolism assessed from l-[1-13C]leucine kinetics including leucine appearance (protein degradation), nonoxidative leucine disappearance (protein synthesis), and leucine oxidation during insulin withdrawal from adolescents with type 1 diabetes and during infusion of insulin and amino acids are shown in Fig. 3 and Table 3. The rate of protein degradation in the basal (insulin withdrawn) state was 138 ± 7.3 μmol · kg−1 · h−1, and the rate of NOLD (protein synthesis) was 107 ± 6.7 μmol · kg−1 · h−1. With the infusion of insulin and amino acids, the rate of both protein degradation and protein synthesis decreased significantly. The rate of protein degradation declined 27 ± 1% to 101 ± 5.3 μmol · kg−1 · h−1 (p < 0.001 versus basal), and the rate of protein synthesis was decreased by 23.5 ± 3.8% to 82.5 ± 7.0 μmol · kg−1 · h−1 (p < 0.001 versus basal). The rate of leucine oxidation in the insulin-withdrawn basal state (31.2 ± 1.7 μmol/kg/h) increased to 49.7 ± 1.9 μmol · kg−1 · h−1 (p = 0.002) with the infusion of insulin and amino acids. Leucine balance (protein degradation − NOLD) was negative in the basal state (−31.2 ± 1.66 μmol/ · kg−1 · h−1), and although there was a significant improvement in leucine balance with the infusion of insulin and amino acids, leucine balance was still negative (−18.9 ± 2.04 μmol · kg−1 · h−1; p = 0.01).
Leucine kinetics in adolescents with type 1 diabetes during insulin withdrawal and insulin replacement. NOLD, leucine appearance, leucine oxidation, and leucine balance were calculated from the enrichment of plasma [13C]KIC, 13CO2, and CO2 production as described in “Methods.” The data are expressed as μmol · kg−1 · h−1 leucine. The basal period (gray; without infusion of insulin) and the period of insulin + amino acid infusion (black) were as described in the legend to Fig. 1. Differences between the basal period and the infusion of insulin + amino acid period were statistically significant, **p < 0.001, *p < 0.01.
Ideally, the intracellular leucyl-t-RNA specific activity should be used for calculations of protein synthesis. As this measurement is very invasive for multiple measurements in adolescents and samples of multiple tissues for measurements of whole-body protein metabolism, the enrichment of plasma KIC often has been taken to represent the enrichment of leucine at the site of amino acid oxidation and protein synthesis (28). We also analyzed the data using plasma leucine enrichment for the calculations. The changes in NOLD or protein synthesis (96.6 ± 3.7 versus 72.7 ± 6.4 μmol · kg−1 · h−1; p = 0.002) and protein degradation (128 ± 4.3 versus 91.6 ± 4.4; p < 0.001) with infusion of insulin and amino acids were similar when the data were calculated from the enrichment of plasma leucine.
DISCUSSION
This study demonstrates a suppression in endogenous protein degradation in growing male adolescents who were given insulin with a simultaneous infusion of amino acids. The patients of this study were on stable insulin regimens (see Table 1) before the withdrawal of insulin for the study, and all but one were growing at pubertal growth rates. The height and weight velocities are shown in Table 1. From the mean weight gain of 5.6 ± 1.4 kg/y, it is possible to estimate the daily protein accretion in these patients. Assuming body weight to be 15% protein for this age group (33), the increase in protein is ~2.3 g/d.
Previous studies in adults who had type 1 diabetes and were studied during insulin withdrawal and insulin infusion had suggested that insulin failed to stimulate protein synthesis but rather reduced the rate of protein degradation (17,18,34,35). Similarly, a study in young (mean age 10 y) patients with type 1 diabetes showed a similar effect of insulin infusion, namely, a decreased rate of protein degradation (13). This also occurred in the present study despite the provision of additional amino acids. It is interesting that in all of these studies and in the present study, the rate of protein synthesis (or NOLD) decreased during the infusion of insulin. Although diminished protein degradation contributed to an improvement in protein balance, patients were not in positive protein balance during the infusion of insulin (10,13,16–18,35). Our findings concur with these previous studies, even with an infusion of amino acid substrate.
This result is in contrast to studies in animals demonstrating a stimulation in the rate of protein synthesis in muscle with the provision of insulin to normal, fasted animals (6) and a reduction in the rate of protein synthesis in muscle of diabetic animals (36). This paradoxic difference between the animal and human studies has been explained in two ways. One way is the contrast between growth and maturity. An ability of young, growing animals to increase protein synthesis in response to insulin, that declines with age, has been reported frequently (8,37–39). It perhaps is not surprising that the adolescent human is less responsive to the effect of insulin than a growing animal. The sensitivity of protein metabolism to the effect of insulin in younger humans (e.g. infants) may be higher than that of adolescents. However, one study in prepubertal children demonstrated no effect of insulin on protein synthesis (13).
An alternative hypothesis for the decline in protein synthesis observed with the provision of insulin to insulin-withdrawn individuals is that insulin is unable to stimulate protein synthesis as a result of a lack of available substrate. Because the rate of protein degradation is reduced by insulin, there is a reduction in the amount of amino acids available for the synthesis of protein. Confirmation of this hypothesis has been provided by studies in which amino acids were given along with insulin. In the studies of adults who had type 1 diabetes and were given amino acids along with insulin, there was a demonstrable increase in protein synthesis (16,17). However, unlike the present study, in which the aim was to prevent the decline in plasma amino acid levels during the infusion of insulin, in both the study of Inciostro et al. (16) and the study of Luzi et al. (17), amino concentrations in plasma were significantly increased (1.5- to 2-fold) during the insulin and amino acid infusion periods. Thus, it seems apparent that at high enough concentrations, amino acids are able to enhance the sensitivity of protein synthesis to insulin in individuals with type 1 diabetes. However, the concentrations required seem to be higher than the amino acid levels present in the postabsorptive state. In contrast to studies in individuals with diabetes, normal, healthy adults did respond to insulin with an increase in protein synthesis when amino acids were maintained at fasting levels (40).
In is unclear in the present study whether the failure of protein synthesis to respond to insulin might have been due to the fall in plasma leucine concentration between the basal state and during insulin infusion. Although amino acids, particularly leucine, have been shown to stimulate protein synthesis (41–47), this effect is observed at plasma concentrations of leucine that are significantly higher than postprandial levels. Clearly, leucine at levels comparable to those achieved during feeding, or higher, can stimulate protein synthesis, but what about levels of leucine that are lower than fasting levels? Is it possible that lower levels of leucine, such as the ~25% decline in plasma concentration observed in the current study, can inhibit protein synthesis? In this regard, a study reported by Kobayashi et al. (48) is particularly relevant. Although the study assessed muscle protein synthesis rather than protein synthesis in the whole body and was conducted in growing pigs, the study demonstrated that reduced levels of plasma amino acids (from hemodialysis) reduced rates of protein synthesis (48). Although similar studies have not been carried out in growing humans, the data in the present study on whole-body protein synthesis are consistent with the hypothesis that leucine levels lower than those present during fasting are associated with reduced levels of protein synthesis.
It would be most interesting to see whether lower levels of leucine in the adolescent, in the absence of insulin, are accompanied by lower levels of protein synthesis. It would also be interesting to see whether provision of higher levels of amino acids to adolescents with type 1 diabetes would result in sensitivity to insulin that was greater than that observed in adults with type 1 diabetes.
CONCLUSION
In conclusion, our study confirms that the primary effect of insulin in humans is to inhibit proteolysis. No evidence of the ability of insulin to stimulate protein synthesis was apparent in these adolescents, even when amino acids were infused with insulin to prevent the hypoaminoacidemia resulting from inhibition of protein degradation during insulin infusion. A suggestion of dependence of whole-body protein synthesis on plasma leucine concentrations, consistent with the study of Kobayashi et al. (48) in growing pigs, was observed in the present study of growing adolescents. The improvement in leucine balance that was observed with the provision of insulin was due to a reduction in the rate of protein degradation that exceeded the decline in the rate of protein synthesis. The study suggests that positive leucine balance requires higher levels of amino acids, perhaps particularly leucine, than were achieved in the present study. The exact nature of the dependence of protein synthesis on both insulin and amino acid levels, particularly leucine, in the adolescent human remains to be delineated.
Abbreviations
- BCAA:
-
branched-chain amino acids
- KIC:
-
ketoisocaproate
- MPE:
-
moles % excess
- NOLD:
-
nonoxidative leucine disposal
- Q:
-
endogenous leucine flux
References
Reed J 1954 Aretaeus, the Cappadocian. Diabetes 3: 419–421
Walsh CH, Soler NG, James H, Harvey TC, Thomas BJ, Fremlin JH, Fitzgerald MG, Malins JM 1976 Studies in whole body potassium and whole body nitrogen in newly diagnosed diabetics. Q J Med 45: 295–301
Jefferson L 1980 Role of insulin in the regulation of protein synthesis. Diabetes 29: 487–496
Flaim K, Copenhaver ME, Jefferson LS 1980 Effects of diabetes on protein synthesis in fast-and slow-twitch rat skeletal muscle. Am J Physiol 239: E88–E95
Baillie AG, Garlick PJ 1991 Responses of protein synthesis in different skeletal muscles to fasting and insulin in rats. Am J Physiol 260: E891–E896
Garlick PJ, Fern M, Preedy VR 1983 The effect of insulin infusion and food intake on muscle protein synthesis in postabsorptive rats. Biochem J 210: 669–676
Jefferson LS, Li JB, Rannels SR 1977 Regulation by insulin of amino acid release and protein turnover in the perfused rat hemicorpus. J Biol Chem 252: 1476–1483
Wray-Cahen D, Nguyen HV, Burrin DG, Beckett PR, Fiorotto ML, Reeds PJ, Wester TJ, Davis TA 1998 Response of skeletal muscle protein synthesis to insulin in suckling pigs decreases with development. Am J Physiol 275: E602–E609
Nair KS, Ford GC, Halliday D 1987 Effect of intravenous insulin treatment on in vivo whole body leucine kinetics and oxygen consumption in insulin deprived type 1 diabetic patients. Metabolism 36: 491–495
Pacy PJ, Nair KS, Ford C, Halliday D 1989 Failure of insulin infusion to stimulate fractional muscle protein synthesis in type 1 diabetic patients. Anabolic effect of insulin and decreased proteolysis. Diabetes 38: 618–624
Pacy PJ, Bannister PA, Halliday D 1991 Influence of insulin on leucine kinetics in the whole body and across the forearm in post-absorptive insulin dependent diabetic (type 1) patients. Diabetes Res 18: 155–162
Robert JJ, Beaufrere B, Koziet J, Desjeux JF, Bier DM, Young VR, Lestradet H 1985 Whole body de novo amino acid synthesis in type 1 (insulin-dependent) diabetes studied with stable-isotope labeled leucine, alanine and glycine. Diabetes 34: 67–73
Vogiatzi MG, Nair KS, Beckett PR, Copeland KC 1997 Insulin does not stimulate protein synthesis acutely in prepubertal children with insulin-dependent diabetes mellitus. J Clin Endocrinol Metab 82: 4083–4087
Felig P, Wahren J, Sherwin R, Palaiologos G 1977 Amino acid and protein metabolism in diabetes mellitus. Arch Intern Med 137: 507–513
Fukagawa NK, Minaker KL, Rowe JW, Goodman MN, Matthews DE, Bier DM, Young VR 1985 Insulin-mediated reduction of whole body protein breakdown. Dose-response effects on leucine metabolism in postabsorptive men. J Clin Invest 76: 2306–2311
Inchiostro S, Biolo G, Bruttomesso D, Fongher C, Sabadin L, Carlini M, Duner E, Tiengo A, Tessari P 1992 Effects of insulin and amino acid infusion on leucine and phenylalanine kinetics in type 1 diabetes. Am J Physiol 262: E203–E210
Luzi L, Castellino P, Simonson DC, Petrides AS, DeFronzo RA 1990 Leucine metabolism in IDDM. Role of insulin and substrate availability. Diabetes 39: 38–48
Bennet WM, Connacher AA, Jung RT, Stehle P, Rennie MJ 1991 Effects of insulin and amino acids on leg protein turnover in IDDM patients. Diabetes 40: 499–508
Castellino P, Luzi L, Simonson DC, Haymond M, DeFronzo RA 1987 Effect of insulin and plasma amino acid concentrations on leucine metabolism in man. Role of substrate availability on estimates of whole body protein synthesis. J Clin Invest 80: 1784–1793
Tessari P, Inchiostro S, Biolo G, Trevisan R, Fantin G, Marescotti MC, Iori E, Tiengo A, Crepaldi G 1987 Differential effects of hyperinsulinemia and hyperaminoacidemia on leucine-carbon metabolism in vivo. Evidence for distinct mechanisms in regulation of net amino acid deposition. J Clin Invest 79: 1062–1069
Flakoll PJ, Kulaylat M, Frexes-Steed M, Hourani H, Brown LL, Hill JO, Abumrad NN 1989 Amino acids augment insulin's suppression of whole body proteolysis. Am J Physiol 257: E839–E847
Gougeon R, Marliss EB, Jones PJ, Pencharz PB, Morais JA 1998 Effect of exogenous insulin on protein metabolism with differing nonprotein energy intakes in type 2 diabetes mellitus. Int J Obes Relat Metab Disord 22: 250–261
Melville S, McNurlan MA, McHardy KC, Broom J, Milne E, Calder AG, Garlick PJ 1989 The role of degradation in the acute control of protein balance in adult man: failure of feeding to stimulate protein synthesis as assessed by L-[1–13C]leucin infusion. Metabolism 38: 248–255
Copeland KC, Kenney FA, Nair KS 1992 Heated dorsal hand vein sampling for metabolic studies: a reappraisal. Am J Physiol 263: E1010–E1014
Borel MJ, Buchowski MS, Turner EA, Goldstein RE, Flakoll PJ 1998 Protein turnover and energy expenditure increase during exogenous nutrient availability in sickle cell disease. Am J Clin Nutr 68: 607–614
Garlick PJ, McNurlan MA, McHardy KC, Calder AG, Milne E, Fearns LM, Broom J 1987 Rates of nutrient utilization in man measured by combined respiratory gas analysis and stable isotopic labelling: effect of food intake. Hum Nutr Clin Nutr 41: 177–191
Toth MJ, MacCoss MJ, Poehlman ET, Matthews DE 2001 Recovery of (13)CO(2) from infused [1-(13)C]leucine and [1,2-(13)C(2)]leucine in healthy humans. Am J Physiol 281: E233–E241
Matthews DE, Schwarz HP, Yang RD, Motil KJ, Young VR, Bier DM 1982 Relationship of plasma leucine and alpha-ketoisocaproate during a L-[1–13C]leucine infusion in man: a method for measuring human intracellular leucine tracer enrichment. Metabolism 31: 1105–1112
Matthews DE, Motil KJ, Rohrbaugh DK, Burke JF, Young VR, Bier DM 1980 Measurement of leucine metabolism in man from a primed, continuous infusion of L-[1–3C]leucine. Am J Physiol 238: E473–E479
Motil KJ, Matthews DE, Bier DM, Burke JF, Munro HN, Young VR 1981 Whole-body leucine and lysine metabolism: response to dietary protein intake in young men. Am J Physiol 240: E712–E721
Waterlow JC, Garlick PJ, Millward DJ 1978 Protein Turnover in Mammalian Tissues and in the Whole Body. North-Holland, Amsterdam, p 804
Toffolo G, Albright R, Joyner M, Dietz N, Cobelli C, Nair KS 2003 Model to assess muscle protein turnover: domain of validity using amino acyl-tRNA vs. surrogate measures of precursor pool. Am J Physiol 285: E1142–E1149
Ellis KJ, Shypailo RJ, Abrams SA, Wong WW 2000 The reference child and adolescent models of body composition. A contemporary comparison. Ann N Y Acad Sci 904: 374–382
Pacy PJ, Halliday D 1989 Muscle protein synthesis in steroid-induced proximal myopathy: a case report. Muscle Nerve 12: 378–381
Nair KS 1995 Muscle protein turnover: methodological issues and the effect of aging. J Gerontol A Biol Sci Med Sci 50: 107–112
Pain VM, McNurlan MA, Albertse EC, Clemens MJ, Garlick PJ 1978 Effect of streptozotocin diabetes on protein synthesis in the liver, kidney and intestinal mucosa of young rats. Proc Nutr Soc 37: 104A
Baillie AG, Garlick PJ 1992 Attenuated responses of muscle protein synthesis to fasting and insulin in adult female rats. Am J Physiol 262: E1–E5
Davis TA, Fiorotto ML, Nguyen HV, Reeds PJ 1993 Enhanced response of muscle protein synthesis and plasma insulin to food intake in suckled rats. Am J Physiol 265: R334–R340
Davis TA, Fiorotto ML, Beckett PR, Burrin DG, Reeds PJ, Wray-Cahen D, Nguyen HV 2001 Differential effects of insulin on peripheral and visceral tissue protein synthesis in neonatal pigs. Am J Physiol 280: E770–E779
Chevalier S, Gougeon R, Kreisman SH, Cassis C, Morais JA 2004 The hyperinsulinemic amino acid clamp increases whole-body protein synthesis in young subjects. Metabolism 53: 388–396
Anthony JC, Anthony TG, Kimball SR, Vary TC, Jefferson LS 2000 Orally administered leucine stimulates protein synthesis in skeletal muscle of postabsorptive rats in association with increased eIF4F formation. J Nutr 130: 139–145
Anthony JC, Yoshizawa F, Anthony TG, Vary TC, Jefferson LS, Kimball SR 2000 Leucine stimulates translation initiation in skeletal muscle of postabsorptive rats via a rapamycin-sensitive pathway. J Nutr 130: 2413–2419
Greiwe JS, Kwon G, McDaniel ML, Semenkovich CF 2001 Leucine and insulin activate p70 S6 kinase through different pathways in human skeletal muscle. Am J Physiol 281: E466–E471
Liu Z, Jahn LA, Long W, Fryburg DA, Wei L, Barrett EJ 2001 Branched chain amino acids activate messenger ribonucleic acid translation regulatory proteins in human skeletal muscle, and glucocorticoids blunt this action. J Clin Endocrinol Metab 86: 2136–2143
Liu Z, Jahn LA, Wei L, Long W, Barrett EJ 2002 Amino acids stimulate translation initiation and protein synthesis through an Akt-independent pathway in human skeletal muscle. J Clin Endocrinol Metab 87: 5553–5558
Paddon-Jones D, Sheffield-Moore M, Zhang XJ, Volpi E, Wolf SE, Aarsland A, Ferrando AA, Wolfe RR 2004 Amino acid ingestion improves muscle protein synthesis in the young and elderly. Am J Physiol 286: E321–E328
Wang X, Campbell LE, Miller CM, Proud CG 1998 Amino acid availability regulates p70 S6 kinase and multiple translation factors. Biochem J 334: 261–267
Kobayashi H, Borsheim E, Anthony TG, Traber DL, Badalamenti J, Kimball SR, Jefferson LS, Wolfe RR 2003 Reduced amino acid availability inhibits muscle protein synthesis and decreases activity of initiation factor eIF2B. Am J Physiol 284: E488–E498
Acknowledgements
We thank the young men and their families who gave up their time to participate in this study. We also thank the nursing and Core Laboratory staff of the Stony Brook General Clinical Research Center, especially George Casella for the mass spectrometry and Dawn Sasvary for the measurement of insulin. We also thank Joan Kavanaugh for once again preparing an excellent manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was supported by grants from the National Institutes of Health M01 RR00109 to the University of Vermont and M01RR 10710 to the State University of New York at Stony Brook.
Rights and permissions
About this article
Cite this article
Godil, M., Wilson, T., Garlick, P. et al. Effect of Insulin with Concurrent Amino Acid Infusion on Protein Metabolism in Rapidly Growing Pubertal Children with Type 1 Diabetes. Pediatr Res 58, 229–234 (2005). https://doi.org/10.1203/01.PDR.0000169976.20029.64
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.PDR.0000169976.20029.64
This article is cited by
-
Differential control of muscle mass in type 1 and type 2 diabetes mellitus
Cellular and Molecular Life Sciences (2015)
-
The Effect of Oral Leucine on Protein Metabolism in Adolescents with Type 1 Diabetes Mellitus
International Journal of Pediatric Endocrinology (2010)
-
Blood amino acids concentration during insulin induced hypoglycemia in rats: the role of alanine and glutamine in glucose recovery
Amino Acids (2007)