Abstract
Endotoxin [lipopolysaccharide (LPS)] from Gram-negative bacteria is found in amniotic fluid in intrauterine infections that associate with the risk for spontaneous premature birth, bronchopulmonary dysplasia (BPD), and respiratory distress syndrome. Toll-like receptor 4 (TLR4) is the signaling receptor for LPS. The aim was to investigate the primary inflammatory response in mice shortly after administration of LPS to the dam (14 and 17 d of pregnancy), to the newborn, or into the amniotic fluid. The expression levels of TLR4, IL-1, tumor necrosis factor-α, IL-6, IL-10, macrophage inflammatory protein-2, and IL-1 receptor 1 were studied with ribonuclease protection assay. In addition, TLR4 protein was analyzed with Western blotting. The fetal membranes expressed TLR4 mRNA and protein and showed an acute cytokine response to LPS when LPS was administrated into the amniotic fluid. There was distinct ontogeny in the responsiveness of fetal lung to LPS: on fetal day 14 (term 20 d), both the expression of TLR4 and the acute cytokine response were undetectable 5 h after LPS; they became detectable by fetal day 17. TLR4 and the cytokine response further increased after birth. In maternal lung, the TLR4 expression was strongest and up-regulated in parallel with the induction of the cytokines. We propose that TLR4 controls the magnitude of the LPS-induced cytokine response during the perinatal period.
Similar content being viewed by others
Main
Intrauterine infection and intrauterine inflammatory response syndrome are associated with preterm birth and bronchopulmonary dysplasia (BPD) in premature infants. Among the predisposing conditions, urinary tract infections and infections that affect the abdominal organs are often caused by Gram-negative bacteria. The onset of premature birth is associated with increased endotoxin and cytokine concentrations in amniotic fluid and inflammation in fetal membranes (1,2).
The infection is detected by the host organism by recognizing specific structures produced only by microorganisms. These elements are called pathogen-associated molecular patterns (PAMPs) (3,4). Recognition of PAMPs is an innate mechanism that is mediated by specific pattern recognition receptors, which activate the acute inflammatory response. Lipopolysaccharide (LPS; also known as endotoxin) is one of the best known PAMPs. It is a constituent of the cell wall of Gram-negative bacteria that starts a complex cascade of events in inflammatory cells, particularly in monocytes and macrophages. This leads to the production of endogenous mediators, including the primary proinflammatory cytokines IL-1 and tumor necrosis factor-α (TNF-α), and a number of other mediators that are induced in various cells (5–7).
A principal LPS signaling receptor is a recently characterized transmembrane pattern recognition receptor, Toll-like receptor 4 (TLR4) (8–11). TLR4 is a member of the mammalian Toll/IL-1 receptor family that is homologous to the Drosophila Toll family, which controls the dorsoventral patterning in the embryo and the antimicrobial response in the adult fly (12,13). Mammalian TLR4 functions as a CD14-associated signal transducer of inflammation that recognizes and distinguishes LPS and some other classes of pathogens on inflammatory cells. Activation of TLR4 initiates the proinflammatory signaling cascade that produces the cytokine response that is involved in the innate immunity and acts to bridge innate and adaptive immunity by inducing various co-stimulatory effector molecules (14–18). Most cytokines have a short half-life in the circulation, being produced in large quantities in activated phagocytes. They interact with specific target cells and participate in generation of an appropriate antimicrobial response. In addition, some cytokines are constitutive and may be needed for continued cell growth, differentiation, and survival. Overproduction of inflammatory cytokines may lead to shock and organ injury (19).
The aims of the present study were to determine whether administration of LPS to the dam, into the amniotic fluid, or to the newborn results in acute primary cytokine response and whether tissues involved in the oxygen uptake (placenta-fetal membranes, lung) are affected. Because TLR4 expression has been suggested to correlate with the intensity of the LPS-induced innate immune response in vitro, we hypothesized that the TLR4-expression in tissues may be a factor controlling the cytokine response.
METHODS
Animals.
All experiments were approved by the Animal Research Committee of the University of Oulu. Female DBA/2 mice were mated, and the day of the vaginal plug was designated as day 0. At days 14 and 17 of pregnancy, known with a precision of ±12 h, the mice received an i.p. injection of 1.2 mg/kg (n = 4 dams) or 2.4 mg/kg LPS (n = 4 dams; E. coli LPS, serotype 055:B5; Sigma Chemical Co. Chemical Co, St. Louis MO). The newborn mice (aged 12–24 h; n = 10) received an s.c. injection of either PBS or 2.4 mg/kg LPS. In another set of experiments, PBS or 0.25 μg of LPS was given to the amniotic sac [intra-amniotic (i.a.)]. These dams were anesthetized on day 14 or day 17 of pregnancy, uterine horns were exposed, and LPS was given i.a. as previously described (20). Five hours after each injection, the mice were killed with cervical dislocation. The maternal and fetal lungs, the placenta, and the fetal membranes as well as the lungs of the newborn mice were harvested.
RNA analysis.
To investigate the acute response to LPS at the molecular level in maternal, newborn, and fetal tissues, we examined the mRNA expression levels of TLR4 and the proinflammatory cytokines IL-1α, IL-1β, IL-6, and TNF-α; the anti-inflammatory cytokine IL-10; the chemokine macrophage inflammatory protein-2 (MIP-2); and the IL-1 signaling receptor (IL-1R1) with ribonuclease protection assay (RPA).
The 303-bp TLR4 probe was synthesized from linearized plasmid pmTLR4-1 generated by reverse transcriptase–PCR from adult mouse lung. The sense primer sequence was 5′-GCAAAGTCCCTGATGACATT-3′, and the antisense primer sequence was 5′-CCAATAGGGAAGCTTTCTA-3′, corresponding to the nucleotides 155 to 174 and 440 to 458 of mouse TLR4 cDNA (GenBank AF110133). The TLR4 RPA probe synthesis reaction contained the linearized template, each NTP and α-32P-UTP (Amersham Biosciences, Buckinghamshire, UK), dithiothreitol, transcription buffer, RNase inhibitor, and T7 RNA polymerase (Promega, Madison, WI). DNA was digested from the mixture after 1 h of synthesis at 37°C with DNase-free RNase. The TLR4 probe was purified with PAGE-urea gel (21), followed by further purification with phenol-chloroform extraction and ethanol precipitation.
Total cellular RNA was isolated from tissues with Trizol reagent (Gibco BRL, Life Technologies, Grand Island, NY) according to the manufacturer's instructions. The RPA was performed with the RiboQuant-RPA kit (Pharmingen, San Diego, CA). The radiolabeled antisense RNA probe was synthesized of a custom template set (Pharmingen) according to the manufacturer's instructions. The custom template mix and the TLR4 probe were dissolved and mixed together. The precipitate was dissolved in the hybridization buffer, and the probe was added to 10 μg of total RNA to be analyzed. After overnight hybridization at 56°C, the unprotected RNA was digested with RNase A and RNase T1 mixture, and the protected RNA fragments were purified with phenol extraction and ethanol precipitation. Electrophoresis was carried out on a 5% denaturing polyacrylamide gel. The bands were quantified with a PhosphorImager scanner (Quantity one, BioRad, Hercules, CA), and the results were normalized to the housekeeping gene L32.
Protein analysis.
The goat anti-human TLR4 antibody C-18 for protein analysis was purchased from Santa Cruz Biotechnology (Santa Cruz, CA). The tissues were homogenized in extraction buffer [10 mM Tris (pH 7.5); 0.25 M saccharose; 1 mM EDTA; 5 mM benzamidine; and 2 mM PMSF that contained 10 μg/mL pepstatin A, aprotinin, leupeptin, and chymostatin] and centrifuged at low speed to collect the supernatant. Ten or 20 μg of each protein sample was resolved in 8% SDS-polyacrylamide gel and electrotransferred onto nitrocellulose membrane Protran BA83 (Schleicher & Schuell, Dassel, Germany). The membranes were blocked at 4°C overnight in 5% skim milk powder-TBS-T (Tris-buffered saline that contained 0.1% Tween 20) and incubated with the primary antibody in TBS-T for 1 h at room temperature followed by washes with TBS-T and incubation with horseradish peroxidase–conjugated anti-goat IgG (Santa Cruz). The blot was developed with the ECL-Plus system (Amersham Biosciences) according to the manufacturer's instructions.
Statistics.
The levels of mRNA, normalized to the housekeeping gene L32, were expressed as means (±SE) for convenience. The changes in the expression levels as a response to LPS were shown as fold increase to control (vehicle) level. The statistical significance was analyzed using nonparametric independent samples test. Significance was accepted at p < 0.05.
RESULTS
To evaluate LPS responsiveness, we monitored the LPS- or vehicle-treated pregnant mice for systemic signs of inflammatory disease. In preliminary experiments, two different concentrations of LPS (1.2 and 2.4 mg LPS/kg) and two different challenging times (5 or 12 h) were used. Within 4 h after the LPS challenge, the mice developed symptoms of fever, ruffled hair, and lethargy. There were no spontaneous abortions or fetal deaths within 5 h. The higher dose of LPS (2.4 mg/kg) and short time interval of 5 h were chosen to establish a primary inflammatory response, minimizing the secondary maternal response that is likely to interfere with the intrauterine response.
Pulmonary response to endotoxin.
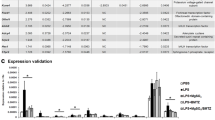
Maternal lung responded acutely and promptly to LPS by up-regulating cytokine mRNAs (Fig. 1). The pulmonary expression levels of the proinflammatory cytokines IL-1β, TNF-α, and IL-6 increased 11.5-, 7.5-, and 4-fold, respectively, whereas the expression level of the chemokine MIP-2 increased 15.5-fold. The increases of IL-1β, TNF-α, and MIP-2 were statistically significant. In addition, IL-1R1, IL-10, and IL-1α were up-regulated ∼2-fold during LPS challenge. The cytokine expression pattern of newborn lung was similar to the adult lung, except that the 5-fold increase in the expression level of IL-1α was stronger than in adult lung. In the newborn animals, LPS increased the pulmonary expression levels of IL-1β, TNF-α, and MIP-2 by 14.4-, 5-, and 16.5-fold, respectively. All of these increases were statistically significant.
Cytokine expression profiles of fetal, newborn, and maternal lungs. The dams (i.p., n = 4) and newborn mice (s.c., n = 10) received injections of PBS or 2.4 mg/kg LPS. The tissues were harvested 5 h later for RNA isolation, and the mRNAs were analyzed using RPA. The levels of IL-1α, IL-1β, IL-6, TNF-α, MIP-2, IL-10, and IL-1R were normalized to L32 and expressed as means (±SE) for convenience. The changes in the expression levels as a response to LPS are shown as fold increase to the control (vehicle) level (horizontal line). Significance, shown with asterisks, was accepted at p < 0.05.
In the very premature lung of the 14-d-old fetus, no constitutional expression of proinflammatory cytokines or chemokines or induction of their expression after LPS exposure was detected (data not shown). In the 17-d-old fetal lung, the increase in cytokine expression was moderate and not statistically significant: the up-regulation of IL-1α, IL-1β, IL-6, TNF-α, and MIP-2 was 2-, 3.5-, 2-, 2-, and 4-fold, respectively. No IL-10 expression could be detected, and the strong constitutional expression of IL-1R1 was not influenced by i.a. LPS. Administration of LPS did not result in any detectable increase in the expression of cytokines of the fetal lung (data not shown).
Responsiveness of placenta and fetal membranes to i.p. and i.a. LPS.
The intensity of cytokine response in placenta and fetal membranes was dependent on the site of LPS administration. The placental tissue expressed constitutive levels of IL-1α, TNF-α, and IL-1R1 (Fig. 2). LPS challenge i.p. induced the expression levels of IL-1α, IL-1β, MIP-2, and TNF-α 1.5-, 1.5-, 4-, and 2.5-fold, respectively. No IL-6 or IL-10 expression could be detected. LPS i.a. induced the placental IL-1β and MIP-2 5.5- and 14.5-fold but TNF-α only 1.5-fold. IL-10 increased 2.0-fold, and IL-6 increased 1.5-fold. However, because of high variation, none of these changes was statistically significant.
Cytokine expression profiles of placenta and fetal membranes at 17 gestational days. The dams received i.p. injections of PBS (n = 4) or 2.4 mg/kg LPS (n = 4); alternatively, PBS (n = 4) or 0.25 μg of LPS (n = 5) was administrated into the amniotic fluid (i.a.). The tissues were harvested 5 h later for RNA, and the mRNAs were analyzed using RPA. The levels of IL-1α, IL-1β, IL-6, TNF-α, MIP-2, IL-10, and IL-1R were normalized to L32 and expressed as means (±SE) for convenience. The changes in the expression levels as a response to LPS are shown as fold increase to the control (vehicle) level (horizontal line). Significance, shown with asterisks, was accepted at p < 0.05. Note that the scale for the fetal membranes (i.a.) is twice the scale of other tissues.
In fetal membranes, the expression of IL-1R1 was constitutional and noninducible (Fig. 2). The i.p. LPS administration had minor effects on the cytokine expression levels of the fetal membrane. On the contrary, the i.a. LPS challenge resulted in up-regulation of the proinflammatory mediators IL-1α, IL-1β, IL-6, and TNF-α and chemokine MIP-2 10.5-, 21-, 5-, 12-, and 28-fold, respectively. All of these increases were statistically significant. Anti-inflammatory cytokine IL-10 mRNA also tended to increase 2.5-fold.
TLR4 expression in the lung, placenta, and fetal membranes.
TLR4 mRNA was expressed in maternal lung, and there was a minor increase by the LPS challenge (Fig. 3). Newborn lung also expressed TLR4, but the expression was not affected by the LPS challenge (Fig. 3). In fetal lung, TLR4 mRNA was not detected at day 14 of gestation (data not shown); however, by day 17, the expression had initiated (Fig. 3). The LPS challenge did not change the expression levels in fetal or newborn lung. In placenta, low basal TLR4 expression was detected and no increase in expression was seen after the LPS administration (Fig. 3). The fetal membranes expressed TLR4, and there was a small, statistically nonsignificant increase during the i.a. LPS challenge (Fig. 3).
Expression of TLR4 mRNA in fetal, newborn, and maternal lungs and in placenta and fetal membranes at 17 gestational days. The dams and newborn mice received i.p. injections of PBS (n = 4) or 2.4 mg/kg LPS (n = 4). In other experiments, PBS (n = 4) or 0.25 μg of LPS (n = 5) was administrated into the amniotic fluid (i.a.). The tissues were harvested 5 h later for mRNA analysis by RPA. The data were normalized to L32 and expressed as means (±SE) for convenience. The changes in the expression levels as a response to LPS are shown as fold increase to the control (vehicle) level (horizontal line).
TLR4 protein in the lung, placenta, and fetal membranes.
Low quantities of TLR4 protein were detectable in fetal lung at day 17. Pulmonary TLR4 in newborn pups was higher than that in fetuses, whereas TLR4 protein in the adult lung was distinctly highest, reflecting the ontogeny of TLR4 mRNA expression. No detectable changes in Western blots were evident after the LPS challenge (Fig. 4).
TLR4 protein in fetal, newborn, and maternal lungs and in placenta and fetal membranes. The dams and newborn mice received i.p. injections of PBS (n = 4) or 2.4 mg/kg LPS (n = 4), and the tissues were collected 5 h later for Western analysis. Twenty micrograms of total protein was loaded on to the SDS-PAGE gel. After transfer onto a nitrocellulose membrane, TLR4 protein was detected using polyclonal antibody (C-18). The results shown are representative of four analyses.
TLR4 signal was weak in Western blots from placenta at 17 gestational days (Fig. 4). In contrast, the fetal membranes from 17 d of pregnancy contained more TLR4 protein. There was no detectable increase in TLR4 protein within 5 h after the LPS challenge (Fig. 4).
DISCUSSION
The present study was undertaken to investigate the primary cytokine response after the introduction of a large dose of LPS into the maternal compartment (22) or into the amniotic fluid. The maternal, placental, and fetal compartments showed remarkable differences in the magnitude of the cytokine response. In contrast to a barely detectable response to LPS in fetal lung, the cytokine responses in maternal lung and in fetal membranes were strong. The present results indicate that the expression of TLR4 correlates with the magnitude of acute cytokine response in different tissues. During perinatal development, there are similarities between the expression patterns of TLR4 and TLR2 (23), the signaling receptors for Gram-negative and Gram-positive bacteria, respectively. The distal signaling pathways of these two TLRs also reveal similarities (17).
In mice of the DBA/2 strain, the expression of TLR4, as measured using RPA, became clearly detectable in fetal lung by day 17, increased toward term, and further increased after birth, confirming the previous results using quantitative PCR in mice of the FVB strain (23). Because in fetal lung, LPS had no acute influence on the expression of TLR4, the genetic regulation of this predominantly macrophage-associated protein may be linked to factors that control the quantity, pulmonary distribution, and differentiation of macrophages (24,25). In accordance with the observed low expression of TLR4, 17-d-old fetal lung responded poorly to the LPS challenge. The acute cytokine response was distinct in the newborn lung, reflecting the perinatal increase in TLR4 protein.
The lack of acute fetal lung response to the LPS challenge suggests that a very immature lung from day 14 either is inert against acute inflammatory stimuli or responds by a TLR4-independent mechanism. However, the finding of a prominent fetal pulmonary cytokine response 1 to 7 d after an i.a. injection of LPS in premature ovine pregnancy (26) suggests that the responsiveness to LPS is inducible in fetal lung. We propose that some of the mediators induced by LPS are responsible for priming the inflammatory responsiveness. It is feasible to assume that cytokines from the fetal membranes accumulate into the amniotic fluid that is mixed with the fetal lung fluid during fetal breathing movements (27,28). Cells that localize on the lining of the future airways either have constitutional TLR4 signaling or may develop TLR4 expression upon contact with the amniotic fluid. Analogously, the cytokines in the amniotic fluid (presumably IL-1) may gain access to the lung via the airways, increasing the components of the surfactant system in the future alveoli (29).
That both very premature ovine and human fetuses develop a prominent pulmonary cytokine response to toxins from microbes (26,30,31) indicates either species difference in the ontogeny of pulmonary innate response or that the time window required for activation of the immune response is longer than used here, allowing the secondary inflammatory response to take place. It may be argued that fetal mice that undergo surgery fail to distribute i.a. LPS to future airways by fetal breathing movements. However, in a similar setting the fetuses had an intracardiac cytokine response, indicating the availability of LPS in the fetal compartment (20). Very premature infants with severe pneumonia at birth also demonstrated low levels of IL-1β and TNF-α in lung effluent and a low level of inducible nitric oxide synthase enzyme in airway cells (32). These inflammatory activities increase remarkably during the next few days as the recovery from severe respiratory failure takes place. A gestational increase in LPS responsiveness was evident in human macrophages from the airways (33).
Besides TLR4, CD14 and MD-2 are required for activation of TLR4 (34). Adaptor proteins, including MyD88, are required for signal transduction after the activation of TLR4 (35). MD-2 null mice do not respond to LPS, and as studied in embryonic fibroblasts, TLR4 remained within the Golgi region and did not appear in plasma membrane (36). In addition to the signaling receptor for LPS, other components of the signaling pathway (37), including the adapter proteins that modulate the quality and the quantity of the inflammatory signal (35), may be rate limiting in perinatal development of the cytokine response.
In premature newborn infants who develop BPD, the cytokine response, judged on the basis of the proinflammatory cytokines in airway specimens, is abnormally high, suggesting dysregulation of the innate immune response (38). The present study provides the first preliminary evidence of the importance of TLR as a modulator of the degree of cytokine responsiveness during the perinatal period. Apart from striking differences in the magnitude of cytokine responsiveness and the expression of the signaling receptor of LPS, there were differences in the pattern of inducible cytokines. The paucity of anti-inflammatory IL-10 in fetal and placental tissues was in contrast with the induction of IL-10 in adult lung that, however, did not reach statistical significance. IL-10 as an anti-inflammatory cytokine in acute macrophage response and as a response element of TH-2 cells has been implicated as a potential antidote in inflammatory diseases. In very premature infants who develop BPD, the high proinflammatory cytokine response and lack of an anti-inflammatory cytokine response, particularly that of IL-10 (39), may sensitize the lung to oxidants and proteases (38).
Chorioamnionitis is an established risk factor for BPD (30). As shown here, the fetal membranes possessed a strong TLR4 signal and gave a robust acute cytokine response after i.a. but not after maternal LPS. The fetal membranes thus may be partially protected from endotoxin in the maternal compartment. In the present study, the fetal membranes and the adult lung tended to show an increase of TLR4 expression, whereas in the other tissues studied, particularly in fetal and neonatal lung, TLR4 expression was not affected by acute exposure to LPS. As studied using mouse peritoneal macrophages, the expression levels of TLR4 are acutely down-regulated by its ligand (40). Induction of TLR possibly may lead to excessive cytokine response observed in BPD in some susceptible infants. The mechanisms that cause the range of changes in TLR4 expression levels, induced by its ligand (40) (present study), remain unknown.
Spontaneous premature births in human pregnancies are commonly associated with intrauterine infection and inflammation, as indicated by the proinflammatory cytokines, microbes (41), and LPS (42) in the amniotic fluid. The fetal membranes implicated in the progression of premature labor are capable of an acute innate cytokine response after LPS. The cytokines generated by the placenta and fetal membranes induce the synthesis of prostaglandins and other mediators that are required for the onset and progression of labor (41). The lack of an appropriately responding innate immune system required for pathogen elimination in the premature infant could be partly responsible for the susceptibility to infections and inflammatory disease. Recently, an allele of TLR4 that results in altered responsiveness to LPS was associated with a predisposition to spontaneous premature birth (43). We propose that activation of TLRs in placenta (23,44) and in fetal membranes, resulting in proinflammatory responses in placenta, fetal membranes, and fetal lung, are among important early steps that lead to inflammatory disease of the fetus and to premature birth.
Abbreviations
- BPD:
-
bronchopulmonary dysplasia
- i.a.:
-
intra-amniotic
- IL-1R1:
-
IL-1 receptor 1
- LPS:
-
lipopolysaccharide (endotoxin)
- MIP:
-
macrophage inflammatory protein
- PAMP:
-
pathogen-associated molecular pattern
- RPA:
-
ribonuclease protection assay
- TLR:
-
Toll-like receptor
- TNF:
-
tumor necrosis factor
References
Romero R, Sirtori M, Oyarzun E, Avila C, Mazor M, Callahan R, Sabo V, Athanassiadis AP, Hobbins JC 1989 Infection and labor. V. Prevalence, microbiology, and clinical significance of intraamniotic infection in women with preterm labor and intact membranes. Am J Obstet Gynecol 161: 817–824
Romero R, Gomez R, Ghezzi F, Yoon BH, Mazor M, Edwin SS, Berry SM 1998 A fetal systemic inflammatory response is followed by the spontaneous onset of preterm parturition. Am J Obstet Gynecol 179: 186–193
Medzhitov R, Janeway CA Jr 1997 Innate immunity: impact on the adaptive immune response. Curr Opin Immunol 9: 4–9
Anderson KV 2000 Toll signaling pathways in the innate immune response. Curr Opin Immunol 12: 13–19
Rietschel ET, Brade H 1992 Bacterial endotoxins. Sci Am 267: 54–61
Wright SD 1999 Toll, a new piece in the puzzle of innate immunity. J Exp Med 189: 605–609
Beutler B 2003 Innate immune responses to microbial poisons: discovery and function of the Toll-like receptors. Annu Rev Pharmacol Toxicol 43: 609–628
Poltorak A, He X, Smirnova I, Liu MY, Huffel C, Du X, Birdwell D, Alejos E, Silva M, Galanos C, Freudenberg M, Ricciardi-Castagnoli P, Layton B, Beutler B 1998 Defective LPS signaling in C3H/HeJ and C57BL/10ScCr mice: mutations in Tlr4 gene. Science 282: 2085–2088
Qureshi ST, Lariviere L, Leveque G, Clermont S, Moore KJ, Gros P, Malo D 1999 Endotoxin-tolerant mice have mutations in Toll-like receptor 4 (Tlr4). J Exp Med 189: 615–625
Hoshino K, Takeuchi O, Kawai T, Sanjo H, Ogawa T, Takeda Y, Takeda K, Akira S 1999 Cutting edge: Toll-like receptor 4 (TLR4)-deficient mice are hyporesponsive to lipopolysaccharide: evidence for TLR4 as the Lps gene product. J Immunol 162: 3749–3752
Takeuchi O, Hoshino K, Kawai T, Sanjo H, Takada H, Ogawa T, Takeda K, Akira S 1999 Differential roles of TLR2 and TLR4 in recognition of gram-negative and gram-positive bacterial cell wall components. Immunity 11: 443–451
Rock FL, Hardiman G, Timans JC, Kastelein RA, Bazan JF 1998 A family of human receptors structurally related to Drosophila Toll. Proc Natl Acad Sci USA 95: 588–593
Medzhitov R, Preston-Hurlburt P, Janeway CA Jr 1997 A human homologue of the Drosophila Toll protein signals activation of adaptive immunity. Nature 388: 394–397
Zhang G, Ghosh S 2001 Toll-like receptor-mediated NF-κB activation: a phylogenetically conserved paradigm in innate immunity. J Clin Invest 107: 13–19
Ghosh S, May MJ, Kopp EB 1998 NF-kappa B and Rel proteins: evolutionarily conserved mediators of immune responses. Annu Rev Immunol 16: 225–260
May MJ, Ghosh S 1998 Signal transduction through NF-kappa B. Immunol Today 19: 80–88
Akira S 2003 Toll-like receptor signaling. J Biol Chem 278: 38105–38108
Fukao T, Koyasu S 2003 PI3K and negative regulation of TLR signaling. Trends Immunol 24: 358–363
Nicola NA 1994 An introduction to the cytokines. In: Nicola NA (ed) Guidebook to Cytokines and Their Receptors. Oxford University Press, New York, pp 1–8
Rounioja S, Räsänen J, Glumoff V, Ojaniemi M, Mäkikallio K, Hallman M 2003 Intra-amniotic lipopolysaccharide leads to fetal cardiac dysfunction. A mouse model for fetal inflammatory response. Cardiovasc Res 60: 156–164
Sambrook T, Fritsch EF, Maniatis T 2001 Molecular cloning: a laboratory manual. Cold Spring Harbor Laboratory Press, New York, pp 7.63–7.74
Kohmura Y, Kirikae T, Kirikae F, Nakano M, Sato I 2000 Lipopolysaccharide (LPS)-induced intra-uterine fetal death (IUFD) in mice is principally due to maternal cause but not fetal sensitivity to LPS. Microbiol Immunol 44: 897–904
Harju K, Glumoff V, Hallman M 2001 Ontogeny of Toll-like receptors Tlr2 and Tlr4 in mice. Pediatr Res 49: 81–83
Sorokin SP, McNelly NA, Hoyt RF Jr 1994 Exogenous cytokines enhance survival of macrophages from organ cultured embryonic rat tissues. Anat Rec 240: 398–406
Trapnell BC, Whitsett JA 2002 Gm-CSF regulates pulmonary surfactant homeostasis and alveolar macrophage-mediated innate host defense. Annu Rev Physiol 64: 775–802
Kramer BW, Moss TJ, Willet KE, Newnham JP, Sly PD, Kallapur SG, Ikegami M, Jobe AH 2001 Dose and time response after intraamniotic endotoxin in preterm lambs. Am J Respir Crit Care Med 164: 982–988
Newnham JP, Moss TJ, Kramer BW, Nitsos I, Ikegami M, Jobe AH 2002 The fetal maturational and inflammatory responses to different routes of endotoxin infusion in sheep. Am J Obstet Gynecol 186: 1062–1068
Hallman M, Lappalainen U, Bry K 1997 Clearance of intra-amniotic lung surfactant: uptake and utilization by the fetal rabbit lung. Am J Physiol 273: L55–L63
Bry K, Lappalainen U, Hallman M 1997 Intraamniotic interleukin-1 accelerates surfactant protein synthesis in fetal rabbits and improves lung stability after premature birth. J Clin Invest 99: 2992–2999
Watterberg KL, Demers LM, Scott SM, Murphy S 1996 Chorioamnionitis and early lung inflammation in infants in whom bronchopulmonary dysplasia develops. Pediatrics 97: 210–215
Bry K, Hallman M, Teramo K, Waffarn F, Lappalainen U 1997 Granulocyte-macrophage colony-stimulating factor in amniotic fluid and in airway specimens of newborn. Pediatr Res 41: 105–109
Aikio O, Vuopala K, Pokela ML, Hallman M 2000 Diminished inducible nitric oxide synthase expression in fulminant early-onset neonatal pneumonia. Pediatrics 105: 1013–1019
Blahnik MJ, Ramanathan R, Riley CR, Minoo P 2001 Lipopolysaccharide-induced tumor necrosis factor-alpha and IL-10 production by lung macrophages from preterm and term neonates. Pediatr Res 50: 726–731
Shimazu R, Akashi S, Ogata H, Nagai Y, Fukudome K, Miyake K, Kimoto M 1999 MD-2, a molecule that confers lipopolysaccharide responsiveness on Toll-like receptor 4. J Exp Med 189: 1777–1782
O'Neill LA, Fitzgerald KA, Bowie AG 2003 The Toll-IL-1 receptor adaptor family grows to five members. Trends Immunol 24: 286–289
Nagai Y, Akashi S, Nagafuku M, Ogata M, Iwakura Y, Akira S, Kitamura T, Kosugi A, Kimoto M, Miyake K 2002 Essential role of MD-2 in LPS responsiveness and TLR4 distribution. Nat Immunol 3: 667–672
Takeda K, Kaisho T, Akira S 2003 Toll-Like Receptors. Annu Rev Immunol 21: 335–376
Jobe AH, Bancalari E 2001 Bronchopulmonary dysplasia. Am J Respir Crit Care Med 163: 1723–1729
Jones CA, Cayabyab RG, Kwong KY, Stotts C, Wong B, Hamdan H, Minoo P, deLemos RA 1996 Undetectable interleukin (IL)-10 and persistent IL-8 expression early in hyaline membrane disease: a possible developmental basis for the predisposition to chronic lung inflammation in preterm newborns. Pediatr Res 39: 966–975
Nomura F, Akashi S, Sakao Y, Sato S, Kawai T, Matsumoto M, Nakanishi K, Kimoto M, Miyake K, Takeda K, Akira S 2000 Cutting edge: endotoxin tolerance in mouse peritoneal macrophages correlates with down-regulation of surface toll-like receptor 4 expression. J Immunol 164: 3476–3479
Gomez R, Ghezzi F, Romero R, Munoz H, Tolosa JE, Rojas I 1995 Premature labor and intra-amniotic infection. Clinical aspects and role of the cytokines in diagnosis and pathophysiology. Clin Perinatol 22: 281–342
Romero R, Roslansky P, Oyarzun E, Wan M, Emamian M, Novitsky TJ, Gould MJ, Hobbins JC 1988 Labor and infection. II. Bacterial endotoxin in amniotic fluid and its relationship to the onset of preterm labor. Am J Obstet Gynecol 158: 1044–1049
Lorenz E, Hallman M, Marttila R, Haataja R, Schwartz DA 2002 Association between the Asp299Gly polymorphisms in the Toll-like receptor 4 and premature births in the Finnish population. Pediatr Res 52: 373–376
Holmlund U, Cebers G, Dahlfors AR, Sandstedt B, Bremme K, Ekstrom ES, Scheynius A 2002 Expression and regulation of the pattern recognition receptors Toll-like receptor-2 and Toll-like receptor-4 in the human placenta. Immunology 107: 145–151
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was supported by the Finnish Academy, the Biocenter Oulu, and the Foundation for Pediatric Research.
Rights and permissions
About this article
Cite this article
Harju, K., Ojaniemi, M., Rounioja, S. et al. Expression of Toll-Like Receptor 4 and Endotoxin Responsiveness in Mice during Perinatal Period. Pediatr Res 57, 644–648 (2005). https://doi.org/10.1203/01.PDR.0000156212.03459.A9
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.PDR.0000156212.03459.A9
This article is cited by
-
Novel Toll-like receptor-4 antagonist (+)-naloxone protects mice from inflammation-induced preterm birth
Scientific Reports (2016)
-
Toll-like receptor-4 in human and mouse colonic epithelium is developmentally regulated: a possible role in necrotizing enterocolitis
Pediatric Research (2015)
-
Postnatal development and LPS responsiveness of pulmonary adenosine receptor expression and of adenosine-metabolizing enzymes in mice
Pediatric Research (2014)
-
Differential effects of cytokines and corticosteroids on Toll-like receptor 2 expression and activity in human airway epithelia
Respiratory Research (2009)