Abstract
A novel therapeutic strategy for phenylketonuria (PKU) has been initiated in Japan. A total of 12 patients who met the criteria for tetrahydrobiopterin (BH4)-responsive hyperphenylalaninemia (HPA) with a mutant phenylalanine hydroxylase (PAH) (EC 1.14.16.1) gene were recruited at 12 medical centers in Japan between June 1995 and July 2001. Therapeutic efficacy of BH4 was evaluated in single-dose, four-dose, and 1-wk BH4 loading tests followed by long-term BH4 treatment, and also examined in relation to the PAH gene mutations. The endpoints were determined as the percentage decline in serum phenylalanine from initial values after single-dose (>20%), four-dose (>30%), and 1-wk BH4 (>50%) loading tests. Patients with mild PKU exhibiting decreases in blood phenylalanine concentrations of >20% in the single-dose test also demonstrated decreases of >30% in the four-dose test. The 1-wk test elicited BH4 responsiveness even in patients with poor responses in the shorter tests. Patients with mild HPA, many of whom carry the R241C allele, responded to BH4 administration. No clear correlation was noted between the degree of decrease in serum phenylalanine concentrations in the single- or four-dose tests and specific PAH mutations. The 1-wk test (20 mg/kg of BH4 per day) is the most sensitive test for the diagnosis of BH4-responsive PAH deficiency. Responsiveness apparently depends on mutations in the PAH gene causing mild PKU, such as R241C. BH4 proved to be an effective therapy that may be able to replace or liberalize the phenylalanine-restricted diets for a considerable number of patients with mild PKU.
Similar content being viewed by others
Main
HPA results from the deficiency of PAH enzyme activity or its cofactor, BH4. In 1999, Kure et al.(1) reported four patients with PAH deficiency who showed a decrease in blood phenylalanine elevations after BH4 loading. BH4 is known to normalize blood phenylalanine in BH4 deficiency, but not in PKU. However, Shintaku et al.(2) found that 5 patients of 15 with mild HPA (serum phenylalanine <20 mg/dL) showed a gradual decrease of serum phenylalanine at 24 h with BH4 loading, although no patient with classical PKU (serum phenylalanine ≥20 mg/dL) responded to BH4. We examined 12 patients with BH4-responsive PAH deficiency discovered by PKU screening and evaluated the responses in the BH4 loading tests in terms of specific PAH mutations. The results have important implications for diagnosis and treatment of patients with BH4-responsive PAH deficiency.
PATIENTS AND METHODS
The 12 HPA patients detected by neonatal PKU screening (Table 1) had normal amount of pteridine in urine or serum before BH4 loading, and also had normal dihydropteridine reductase activity according to the test using the Guthrie card. Blood phenylalanine concentrations at screening were in the range of 2.0–12.0 mg/dL. All patients were diagnosed with mild PKU, and were given the phenylalanine-restricted diets. The criterion standard was administered between June 1995 and July 2001 at 12 medical centers in Japan.
An oral BH4 (Suntory, Tokyo, Japan) loading test was performed after demonstrating serum phenylalanine concentrations >6 mg/dL upon instituting a normal diet, which was maintained during loading tests. In the single-dose BH4 loading test, BH4 (10 mg/kg) was administered before breakfast; blood samples were collected at 0, 4, 8, and 24 h after loading. In the four-dose BH4 loading test, BH4 was administered at doses of 10, 10, 5, and 5 mg/kg at 0, 24, 36, and 48 h, respectively. Blood samples were obtained at 0, 4, 8, 24, and 52 h after loading. In the 1-wk BH4 loading test, BH4 was administered for 1 wk at 20 mg/kg in 3 p.o. daily. Blood samples were obtained before loading and after 4 and 7 d. Long-term BH4 administration was started at 10–20 mg/kg into three doses daily; the dose was adjusted with the goal of maintaining serum phenylalanine concentrations between 2 and 4 mg/dL with a normal diet. Blood samples were obtained before administration, then weekly during the first month, and subsequently every 2 wk or month. All BH4 loading tests and long-term BH4 administration were performed after informed consent and approval of the institutional review board.
Serum phenylalanine concentrations were determined by using an automated amino acid analyzer (L-8800; Hitachi, Tokyo, Japan). Serum pteridine was measured by HPLC (LC-10; Shimazu, Kyoto, Japan) after iodine oxidation. Dihydropteridine reductase activity was measured in Guthrie card specimens as described previously (3).
Genomic DNA was prepared from white blood cells using a phenol/chloroform extraction method. Each exon and its flanking intron region were amplified with a pair of human PAH-specific oligonucleotide primers (one primer being biotinylated) using a PCR. The amplified products were purified to single-stranded DNA using streptavidin-coated M280 magnetic beads (Dynal, Oslo, Norway). The purified single-stranded DNA was sequenced by the dye terminator method using an ABI PRISM 310 genetic analyzer (PerkinElmer Instruments, Norwalk, CT, U.S.A.).
RESULTS
Single-dose BH4 loading test.
In eight patients (cases 1, 2, 5–8, 10, and 11) with initial serum phenylalanine concentrations of at least 9.84 mg/dL, serum phenylalanine decreased gradually by 20–60% of their initial values between 4 and 24 h after BH4 loading (Tables 2 and 3). Among cases 3, 4, and 9, with initial values of approximately 5 mg/dL, cases 3 and 9 showed the above pattern, decreasing by more than 50% of the initial phenylalanine values. Case 4 failed to show a decrease in serum phenylalanine during the loading test. Thus, the degrees of decline of serum phenylalanine in a single-dose BH4 loading test were greater than 20% in 10 of 11 patients. This test was not performed in case 12.
Four-dose BH4 loading test.
Case 4 showed a gradual decrease after 8 h, with a 37.4% decline in serum phenylalanine in 52 h (Tables 2 and 3). Case 5 showed a similar response to the single-dose case. The four doses were no more effective than one in this case. The decline in serum phenylalanine induced by the four-dose BH4 loading test was >30% in seven (cases 1–4, 6, 8, and 12) of eight patients, ranging from 35% to 59%. This test was omitted in some patients.
One-week BH4 administration test.
In six patients (cases 1–5 and 8) BH4 was administered at 20 mg/kg/d for 1 wk (Tables 2 and 3). In cases 2 and 4, the 1-wk BH4 administration was initiated immediately after the four-dose BH4 loading test without waiting for an increase in serum phenylalanine. Values from the single-dose BH4 loading test in case 2 and the four-dose BH4 loading test in case 4 therefore were used as the baseline for calculating degree of decline with the 1-wk administration in these cases. In case 8, the 1-wk BH4 administration was carried out immediately by returning the patient to a normal diet, because low-phenylalanine diet therapy had been maintained until that time. Taking the value for the four-dose BH4 loading as a baseline, the degree of further decline was calculated. As a result, serum phenylalanine concentrations in cases 3 and 5 decreased by more than 50%. The serum phenylalanine decline in case 1 was the largest observed, being >44.7% at 15 mg/kg of BH4/d for 1 wk. Serum phenylalanine levels decreased to 3 mg/dL or less in cases 2 and 4, with degree of reduction representing more than 50% compared with the preloading values in the single-dose or the four-dose BH4 loading test. In case 8, the serum phenylalanine level before the 1-wk BH4 loading test was 0.56 mg/dL within the normal range, however, during this test, serum phenylalanine kept the level as almost stable as 4 mg/dL. This level did not increase under the free diet and the degree of reduction showed more than 50% compared with the preloading values in the four-dose BH4 loading test.
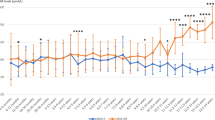
Long-term BH4 therapy.
In case 1, BH4administration at 12.2 mg/kg/d kept serum phenylalanine at <4 mg/dL with a normal diet modified only by use of phenylalanine-free milk (Table 3). Subsequently, case 1 developed normally. Cases 2 and 3 had serum phenylalanine levels below 4 mg/dL on a normal diet under BH4 administration at 16.4 and 7.9 mg/kg per day, respectively. They had started the BH4 treatment early, and developed normally. Cases 4 and 5 had started the BH4 treatment at 2 y of age and kept their serum phenylalanine levels below 4 mg/dL on a normal diet by BH4 mono-therapy, and showed normal mental development. In case 4, compliance with the low phenylalanine diet resulted in a reduced caloric intake and stunted body development. After the introduction of BH4 treatment, the caloric intake recovered and the body development resumed normally.
In case 6, the compliance with the low phenylalanine diet had been poor, resulting in serum phenylalanine above 10 mg/dL. BH4 treatment was initiated at 5 mg/kg per day and then increased gradually, based on serum phenylalanine concentrations.
Cases 7 and 9 had received BH4 treatment from the beginning in the neonatal period, and both showed a good response in the single-dose BH4 loading test. Blood phenylalanine values were controlled by BH4 either given alone or combined with a restricted-phenylalanine diet. BH4 monotherapy has been pursued in case 9 for more than 4.5 y, resulting in normal physical and mental development. In case 10, BH4 administration was discontinued for 1 y due to parental constraints, leading to high serum phenylalanine concentrations. BH4 treatment was resumed after this hiatus, but unfortunately this treatment was stopped after 11 mo, again by the parental request. Cases 8 and 12 were treated with a low-phenylalanine diet without BH4 administration. The way of treatment in case 11 after BH4 loading test was unknown. Notably, no side effects were identified in the BH4-treated cases.
Among 12 patients with BH4-responsive PAH deficiency, 8 patients achieved their target serum phenylalanine values with BH4 alone or in combination with a phenylalanine-restricted diet, resulting in normal development. In addition, BH4 greatly improved patients' compliance and reduced the mental and physical burden upon both patients and families. The effectiveness, safety, and advantages of BH4 thus were confirmed in treatment of BH4-responsive PAH deficiency.
Mutations in the PAH gene.
The results of gene mutation analysis are listed in Table 3. All but two patients were heterozygous, and two different mutation types were identified. The R241C mutation was detected in 8 (cases 1, 4, 5, 7, 8, 10, 11, and 12) of 12 patients. Interestingly, two patients (cases 4 and 11) were homozygous for this mutation. The PAH R241C mutant has been reported showing 25% of the activity of wild-type PAH in a COS cell expression analysis (4).
Among the six compound heterozygotes, T278I, P281A, R111X, and R413P were detected in the other alleles. These four mutations are detected in classical PKU and result in nonfunctional PAH alleles (5, 6). Nevertheless, eight cases with the R241C allele showed low blood phenylalanine concentrations (7.0 mg/dL on average) in neonatal mass-screening. In cases 2 and 6, P407S was detected in one allele and R158W and R252W in the other allele. Case 9 had A373T and IVS4–1g>a alleles. Mutant PAH molecules with P407S and A373T possess residual activity, like R241C (1). However, PAH alleles with R252W, R158W, and IVS4–1g>a have no activity, thus resembling the R413P allele. Two patients with the P407S allele (cases 2 and 6) showed essentially high blood phenylalanine concentrations (10–16 mg/dL) in neonatal mass-screening.
No clear correlation was evident between the PAH mutations and the degree of decline of serum phenylalanine in the single- or four-dose BH4 loading test. In all cases, blood phenylalanine concentrations decreased gradually after BH4 administration. However, based on the results above, R241C, P407S, A132V, and A373T alleles represented the causes of mild HPA, whereas R413P, R252W, R158W, and IVS4–1g>a alleles resulted in severe HPA. Patients with mild HPA, many of whom had the R241C allele, responded to BH4 administration.
DISCUSSION
Among patients with mild HPA, characterized by serum phenylalanine concentrations below 20 mg/dL, a subset has shown a gradual decrease in serum phenylalanine concentrations over 1 d after BH4 administration (1, 2, 7–15). These patients showed no abnormalities in BH4 metabolism but had mutations in the PAH gene. Thus, a likely mechanism for BH4 responsiveness would involve the mutant PAH molecules with a high Michaelis-Menten constant (Km) for BH4, requiring a higher BH4 concentration (1, 2, 7–15). Furthermore, BH4 might stabilize the mutant PAH molecules, considering that some of the missense mutations rendered the PAH molecule unstable, leading to a shorter half-life; this could account for the gradual nature of the effect. In either case, PAH activity should increase in response to exogenous BH4.
Accordingly, the four-dose BH4 loading test and the 1-wk trial administration were performed in patients showing decreases in blood phenylalanine in the single-dose BH4 loading test. The four-dose test was used to confirm a decline of phenylalanine in serum. The high-dose, 1-wk trial administration (20 mg/kg/d) was intended to increase the diagnostic accuracy and predict the effectiveness of the long-term treatment.
We found that patients with a decrease >20% in serum phenylalanine levels in the single-dose BH4 loading test showed a similar decrease in the four-dose test. The mean degree of lowering in the single-dose test was 40% in Japan, about half of the reduction seen in Europe; the standard dose of BH4 is 10 mg/kg in Japan, half of the 20 mg/kg dose used in Europe. These results indicated that the response to a BH4 load was dose dependent. Although case 5 showed no enhancement of effect by the four-dose BH4 administration, it showed a significant decrease in serum phenylalanine levels in the 1-wk BH4 loading test. The 1-wk trial administration confirmed BH4 effects in responsive patients, but also showed an effect in patients without any clear responsiveness in single- or four-dose BH4 loading tests. These results indicated that BH4 responsiveness becomes evident slowly, and in some cases it must be taken several days to lower blood phenylalanine. Lässker et al.(7) reported that two patients with no response to BH4 (7.5 mg/kg) in a loading test showed a marked decrease in plasma phenylalanine after 5 d of BH4 administration (10 mg/kg). Moreover, although the BH4 dose (20 mg/kg) in the 1-wk trial administration was higher than the usual therapeutic dose used in BH4 deficiency in Japan, it may represent the optimal dose in BH4-responsive PAH deficiency, considering that 20 mg/kg is used in European countries with only minimal side effects (diarrhea and vomiting). Information from our 1-wk trial BH4 administration is helpful in dose-setting for the long-term treatment. More generally, the 1-wk BH4 administration is highly important in the differential diagnosis and treatment planning in BH4-responsive HPA.
Our genetic analyses and those reported by others indicated that BH4 responsiveness is greatly determined by mutations in the PAH gene, such as R241C. Spaapen et al. (8) reported four patients with BH4-responsive PAH deficiency; one patient with R241C/A403V mutations showed a rapid response in a combined phenylalanine and BH4 loading test, resulting in normalization of plasma phenylalanine within 8 h. Mutant PAH molecules with R241C and A403V mutations were found to have respective residual activities of 25% and 32% of wildtype PAH activity. However, Trefz et al. (9) reported one mild PKU patient with E390G/IVS10–11g>a—a missense mutation permitting some enzyme activity and another mutation precluding activity—who showed BH4 responsiveness. They concluded that a patient with mild PKU with one mutation, resulting in limited activity, may show the BH4 reactivity even if the other mutation abolishes activity. Mutant PAH molecules with Y414C, the most common mild PKU mutation in Northern and Western Europe (4), have residual activity resembling that with R241C. Steinfeld et al. (10) reported that a patient homozygous for Y414C showed a 72% decline in serum phenylalanine in a single-dose BH4 loading test (20 mg/kg). Nuoffer et al. (11) described a patient with Y414C/del194 mutations and a similar response to a BH4 load of 20 mg/kg. On the other hand, Lindner and co-workers (12) found that three patients with the same genotype (Y414C/R408W) showed differing responses in a single-dose BH4 loading test (20 mg/kg). Blood phenylalanine levels decreased to the normal range in one patient, but not in the other two patients, despite normal BH4 absorption; the authors concluded that BH4 responsiveness in PAH deficiency is at least partly independent of PAH genotype. Although the first mutation, Y414C, has some residual activity (4), R408W is a known null mutation that completely abolishes enzyme activity on the affected allele and is associated with only minimal amounts of PAHimmunoreactive protein according to in vitro expression studies (16). Therefore, the mutant PAH molecule with Y414C/ R408W catalyzed the phenylalanine-hydroxylation reaction at a lower rate than that seen in a Y414C homozygote, rendering BH4 responsiveness in patients with Y414C/R408W more variable than in Y414C homozygote. Although no clear correlation was seen between the degrees of lowering of the serum phenylalanine in the BH4 loading test and PAH mutations, at least one mild PKU mutation or missense mutation was found in patients with BH4 responsiveness. Erlandsen and Stevens (13) indicated that these mutations can be located in the cofactor-binding regions or in those that closely interact with the cofactor-binding regions. However Blau and Trefz (14) reported that a patient with BH4 responsiveness had the homozygous L48S mutation in the PAH gene that has located in the regulatory domain (exon 1–5). Muntau et al. (15) classified seven mutations (P314S, Y417H, V177M, V245A, A300S, E390G, and IVS4–5C->G) as probably associated with responsiveness to BH4, six mutations (A403V, F39L, D415N, S310Y, R158Q, and I65T) as potentially associated, and four mutations (Y414C, L48S, R261Q, and I65V) as inconsistently associated with this phenotype, and stated that mutations connected to BH4 responsiveness were predominantly in the catalytic domain of the protein and were not directly involved in cofactor binding. Therefore, the mechanism underlying BH4 responsiveness in PAH deficiency is still incompletely understood.
Discovery of BH4-responsive PAH deficiency has signifi- cant clinical implications. Sufficient amounts of BH4 easily could be given to treat this disorder, inasmuch as serum phenylalanine concentrations were controlled to within 4 mg/dL by BH4 monotherapy or by BH4 combined with relatively mild dietary phenylalanine restriction. A rigorous restricted- phenylalanine diet involves a great deal of long-term effort for patients and their families. BH4 treatment of responsive patients can eliminate or reduce the need for phenylalanine- restriction. Accurate diagnosis of BH4 responsiveness therefore is very important. In this study, BH4 responsiveness appeared to be regulated by mild PKU mutations in PAH gene, and was affected by the dose and administration period of BH4. Based on our genetic analysis, the rate of R241C or P407S mutations among BH4-responsive PAH deficiency is 83% in Japan. Thus, gene analysis should be performed on all HPA patients. One-week BH4 administration at 20 mg/kg/d was the most sensitive test for diagnosis of BH4-responsive PAH de- ficiency, and this additional test should be performed in all PKU patients who show more than a 20% decrease of blood phenylalanine in a single-dose BH4 loading test, or who have R241C or P407S mutations.
Treatment with BH4 (5–20 mg/kg/d) is a new and effective pharmacotherapy that can replace a restricted-phenylalanine diet in some mild PKU patients. BH4 has already been marketed as an approved drug for BH4 deficiency. The rate of BH4-responsive PAH deficiency among PKU is about 10% in Japan, and is apparently higher than that of BH4 deficiency. Nevertheless, BH4 is not yet approved for BH4-responsive PAH deficiency, and effects of high doses of BH4 have not been examined in large numbers of patients. Caution and careful observation of clinical changes will be necessary to successfully bring BH4 treatment to the clinic for this indication.
Abbreviations
- PKU:
-
phenylketonuria
- BH4:
-
tetrahydrobiopterin
- PHA:
-
hyperphenylalaninemia
- PAH:
-
phenylalanine hydroxylase
References
Kure S, Hou DC, Ohura T, Iwamoto H, Suzuki S, Sugiyama N, Sakamoto O, Fujii K, Matsubara Y, Narisawa K 1999 Tetrahydrobiopterin-responsive phenylalanine hydroxylase deficiency. J Pediatr 135: 375–378
Shintaku H, Asada M, Sawada Y, Yamano T 2000 Tetrahydrobiopterin-responsive hyperphenylalaninemia without biopterin deficiency. Pteridines 11: 83–84
Arai N, Narisawa K, Hayakawa H, Tada K 1982 Hyperphenylalaninemia due to dihydropteridine reductase deficiency: diagnosis by enzyme assays on dried blood spots. Pediatrics 70: 426–430
Okano Y, Eisensmith RC, Dasovich M, Wang T, Guttler F, Woo SL 1991 A prevalent missense mutation in Northern Europe associated with hyperphenylalaninaemia. Eur J Pediatr 150: 347–352
Okano Y, Asada M, Kang Y, Nishi Y, Hase Y, Oura T, Isshiki G 1998 Molecular characterization of phenylketonuria in Japanese patients. Hum Genet 103: 613–618
Takahashi K, Kure S, Matsubara Y, Narisawa K 1992 Novel phenylketonuria mutation detected by analysis of ectopically transcribed phenylalanine hydroxylase mRNA from lymphoblast. Lancet 340: 1473
Lässker U, Zschocke J, Blau N, Santer R 2002 Tetrahydrobiopterin responsiveness in phenylketonuria. Two new cases and a review of molecular genetic findings. J Inherit Metab Dis 25: 65–70
Spaapen LJ, Bakker JA, Velter C, Loots W, Rubio-Gozalbo ME, Forget PP, Dorland L, De Koning TJ, Poll-The BT, Ploos van Amstel HK, Bekhof J, Blau N, Duran M, Rubio-Gonzalbo ME 2001 Tetrahydrobiopterin-responsive phenylalanine hydroxylase deficiency in Dutch neonates. J Inherit Metab Dis 24: 352–358
Trefz FK, Aulela-Scholz C, Blau N 2001 Successful treatment of phenylketonuria with tetrahydrobiopterin. Eur J Pediatr 160: 315
Steinfeld R, Kohlschutter A, Zschocke J, Lindner M, Ullrich K, Lukacs Z 2001 Tetrahydrobiopterin-responsiveness associated with common phenylalaninehydroxylase mutations distant from the tetrahydrobiopterin binding site. J Inherit Metab Dis 24: 29
Nuoffer JM, Töny B, Romstad A, Blau N 2001 A patient with phenylketonuria successfully treated with tetrahydrobiopterin. J Inherit Metab Dis 24: 29
Lindner M, Haas D, Mayatepek E, Zschocke J, Burgard P 2001 Tetrahydrobiopterin responsiveness in phenylketonuria differs between patients with the same genotype. Mol Genet Metab 73: 104–106
Erlandsen H, Stevens RC 2001 A structural hypothesis for BH4 responsiveness in patients with mild forms of hyperphenylalaninaemia and phenylketonuria. J Inherit Metab Dis 24: 213–230
Blau N, Trefz FK 2002 Tetrahydrobiopterin-responsive phenylalanine hydroxylase deficiency: possible regulation of gene expression in a patient with the homozygous L48S mutation. Mol Genet Metab 75: 186–187
Muntau AC, Roschinger W, Habich M, Demmelmair H, Hoffmann B, Sommerhoff CP, Roscher AA 2002 Tetrahydrobiopterin as an alternative treatment for mild phenylketonuria. N Engl J Med 347: 2122–2132
DiLella AG, Marvit J, Brayton K, Woo SL 1987 An amino-acid substitution involved in phenylketonuria is in linkage disequilibrium with DNA haplotype 2. Nature 327: 333–336
Acknowledgements
The authors thank Tomoko Kajita for expert technical assistance. We also thank Dr. Toshiaki Oura, Dr. Keiya Tada, and Dr. Ichiro Matsuda for critically reviewing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shintaku, H., Kure, S., Ohura, T. et al. Long-Term Treatment and Diagnosis of Tetrahydrobiopterin-Responsive Hyperphenylalaninemia with a Mutant Phenylalanine Hydroxylase Gene. Pediatr Res 55, 425–430 (2004). https://doi.org/10.1203/01.PDR.0000111283.91564.7E
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.PDR.0000111283.91564.7E
This article is cited by
-
Tetrahydrobipterin-responsive phenylalanine hydroxylase deficiency
Journal of Human Genetics (2019)
-
The neonatal tetrahydrobiopterin loading test in phenylketonuria: what is the predictive value?
Orphanet Journal of Rare Diseases (2016)
-
Correlation between genotype and the tetrahydrobiopterin-responsive phenotype in Chinese patients with phenylketonuria
Pediatric Research (2015)
-
Tetrahydrobiopterin responsiveness in phenylketonuria: prediction with the 48-hour loading test and genotype
Orphanet Journal of Rare Diseases (2013)
-
Testing for Tetrahydrobiopterin Responsiveness in Patients with Hyperphenylalaninemia due to Phenylalanine Hydroxylase Deficiency
Advances in Therapy (2013)