Abstract
The objective of this study was to further explore previously identified effects of supplemental ribonucleotides on infant immune status as measured by antibody responses to routine infant immunizations. Infants were randomized to a milk-based formula with (FN, n = 138) or without (F, n = 147) 72 mg ribonucleotides/L. A cohort of human milk–fed (HMF, n = 192) infants was also followed. Subjects were given Haemophilus influenzae type b (Hib), diphtheria tetanus acellular pertussis, and oral poliovirus vaccinations at 2, 4, and 6 mo of age, and specific antibody responses were assessed at 2, 6, 7, and 12 mo. Growth and safety data were also monitored. Using a two-group repeated measures analysis (RMA), FN-fed infants had significantly higher poliovirus type 1 neutralizing antibody (PV-VN1) responses than F-fed infants (p = 0.045). Using three-group RMA, PV-VN1 responses in HMF infants were not different from FN-fed infants, while HMF-fed infant PV-VN1 responses were significantly higher than F-fed infants at 6 (p = 0.0004) and 12 mo (p = 0.0001). FN-fed infants had responses to Hib Farr, diphtheria, tetanus toxoid, oral poliovirus–specific IgA, and PV-VN3 not significantly different from those of F and HMF infants. Growth, gastrointestinal tolerance, and adverse events were equivalent among the three groups. The FN-associated increase in PV-VN1 response and nonstatistically significant trends toward increased Hib and diphtheria antibody responses were consistent with observations from earlier studies, indicating immune benefits of nucleotide supplementation of infant formula.
Similar content being viewed by others
Main
Infants are at higher risk for morbidity and mortality resulting from infectious diseases than older children, due in part to immaturity of the infant immune system (1,2). The mode of feeding during infancy may influence the risk of infection as breast-fed newborns have been reported to have a lower incidence of infections than formula-fed infants (2–4). It has been speculated in published reports that immune modulators in human milk could explain some of the protective effects of human milk (3,5,6).
Ribonucleotide 5′-monophosphates modulate cellular and humoral immune function in animals as has been shown from studies in which nucleotides were added to a basal animal diet low in nucleotides (7–11). Likewise, supplemental ribonucleotides increased immune responses in infants (12–16) and in malnourished children (17). In four of these studies, antigen-specific antibody responses have been used as surrogate markers to assess the influence of ribonucleotides on immune status. These data suggested that compositional changes to infant formula might augment the infant's humoral immune response.
Ribonucleotides are found in human milk (18,19) and are at much lower levels in cow's milk. Cow's milk–based infant formulas had only trace amounts of ribonucleotides before 1996. Although most formula manufacturers now add ribonucleotides, the levels and ratios of added nucleotides vary. In earlier studies, although inherent levels in unsupplemented formulas were not described, addition of relatively small amounts of ribonucleotides (19.2 mg/L) were reported to be efficacious for gut health in high-risk infant populations (20), slightly higher levels (~30 mg/L) had transient effects on natural killer cell activity (12), and no effect was observed on antibody response or lymphocyte subsets (21). Higher levels of ribonucleotides (72 mg/L) patterned after the ratios in human milk have enhanced antibody response to some routine pediatric vaccines (14,15) and modified immune cell types (22) and suggested reduced diarrheal illness in healthy Taiwanese infants (16). Thus, the benefits conferred appear to depend on both concentration and ratio of dietary ribonucleotides, and the population studied.
Antibody response to immunization requires synergistic activity of multiple immune components and is among the best surrogate measures of the integrity and functional status of the immune system. This double-blind, active treatment–controlled, randomized trial of FN was designed to verify the effect of supplemental ribonucleotides on vaccine responses, to explore effects on the development of immune cells using flow cytometric analysis, and to assess their effect on clinical morbidity. Separate reports will communicate the results of these objectives; the current article describes the vaccine response data.
METHODS
Study design.
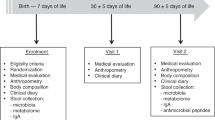
This was a 12-mo, prospective, randomized, double-blind, parallel, longitudinal study of healthy, term, formula-fed infants carried out from fall 1996 to the spring of 1998. Infants, whose mothers had chosen to formula feed before enrollment were enrolled before 8 d of age and randomized to the cow milk–based control formula (F) or the same formula supplemented with ribonucleotide 5′ monophosphates (72 mg/L) (FN, commercial SWI) ad libitum from enrollment to 12 mo of age. Infants in the nonrandomized reference group of subjects fed human milk (HMF) were enrolled concurrently before 8 d of age, and fed human milk exclusively until at least 2 mo of age. After 2 mo, infants whose parent(s) chose to wean were fed SWI not supplemented with ribonucleotides (SWI, pre-1997 commercial SWI). Therefore, the HMF group consisted of a combination of infants exclusively fed human milk, infants receiving a combination of human milk and SWI, and infants weaned to SWI. All infants were fed their assigned formula, or human milk (alone or with SWI), exclusively until 4 mo of age, after which other foods were permitted. The immunization schedule was consistent with the recommendations of the American Academy of Pediatrics (23) and subsequent changes made to the schedule (24). Blood samples were obtained at 2, 6, 7, and 12 mo of age.
Physician office visits occurred every 4 wk (± 3 d) for the duration of the study. Anthropometric measurements were taken at enrollment and at 1, 2, 4, 6, 7, and 12 mo of age as described elsewhere (25). Tolerance responses to the formulas were assessed using parent diaries for 3 d before the 1, 2, and 4-mo visits. Serious adverse events were monitored throughout the study.
Subjects.
Eligible infants were recruited from local hospitals and pediatric practices at 18 sites in 10 states (AR, CA, FL, GA, IL, LA, NC, NY, OH, and PA). Subjects had a gestational age of 37–42 wk, weighed ≥2500 g at birth, and scored ≥7 on a 5-min Apgar. Exclusions were made where there was evidence of significant organ system or metabolic disease and maternal medical history known to have adverse effects on the fetus (diabetes, preeclampsia, HIV infection, or drug abuse). Infants whose parent(s) had decided to formula feed were not eligible for the study if they had consumed colostrum or human milk. Infants that had been fed soy formula or milk-based formula supplemented with ribonucleotides were not eligible for the study. Informed consent was obtained from parent(s) or guardian(s) of each subject before participation in the trial. The consent process and clinical documentation for this study were reviewed and approved by the Internal Review Board at each study site.
Formulas.
F and FN were masked through the use of labels differing only in a numeric code. All study formulas were in the ready-to-feed form and did not require dilution. SWI was comparable to F except for minor changes in fatty acid composition, and a different protein blend (Table 1). Formulas were manufactured by Ross Products Division, Abbott Laboratories and met or exceeded nutrient levels recommended by the Committee on Nutrition of the American Academy of Pediatrics (26) and required by the Infant Formula Act of 1980 and subsequent amendments.
Immunizations and blood collection schedule.
Study sites were instructed to administer each of the injected vaccines in separate limbs according to manufacturer directions at 2, 4, and 6 mo of age. To minimize interlot variation in the immunogenicity of the vaccines, single lots of Hib polysaccharide-recombinant diphtheria toxin (CRM) vaccine (HibTITER, Lederle-Praxis, Wayne, NJ) and diptheria-tetanus-acellular pertussis (DTaP) vaccine (Tripedia, Connaught, Swiftwater, PA) were supplied to all sites. Two lots of oral trivalent polio vaccine (OPV; Orimune, Lederle, Pearl River, NY) were used. The first lot was used for the 2- and 4-mo immunizations, and the second for the 6-mo immunization. Use of study vaccine lots was verified using vaccination records. Administration of other immunizations was at physician discretion and was not a protocol deviation.
Blood samples were obtained at the 2, 6, 7 and 12 mo study office visits to 1) establish baseline antibody levels before the first immunization, 2) capture peak antigen-specific antibody response by measuring antibody titers before and 28 d after the third immunization, and 3) provide an assessment of long-term antibody responses by measuring antigen-specific titers at 12 mo of age.
Antibody and immunoglobulin determinations.
Analysis of sera for anti-Hib PRP antibody was done using a modified Farr assay as described elsewhere (27). Analyses of sera for anti-diphtheria toxoid IgG, anti-tetanus toxoid IgG, and poliovirus-specific IgA to monovalent polio vaccine MP12–97, type 1 (Statens Seruminstitut, Copenhagen, Denmark) were done using enzyme-immune assay methods previously described (15). PV-VN1 and PV-VN3 were measured as reported elsewhere (28) and are presented as the reciprocal of the highest serum dilution that inhibited visible poliovirus-induced cytopathology. Total IgE was performed using DPC Immunlite Chemiluminescent Technology (Diamond Diagnostics, Holliston, MA) and cow milk–specific IgE were assessed using Immuno CAP system fluorescence enzyme immunoassay (Kabi Pharmacia Diagnostics, Piscataway, NJ). Total serum IgG and IgA were measured by radial immunodiffusion kits (The Binding Site, San Diego, CA). Total IgG and IgA were then used to normalize antigen-specific IgG and IgA antibody titers expressing these as specific activities.
Growth and safety.
The number of visits to the physician was analyzed as an exploratory outcome. Medical personnel blinded to study products, used medical records to identify newly diagnosed conditions. Routine well visits and follow-up visits for previously diagnosed conditions were identified and excluded from the analysis. Diagnoses were categorized as otitis media, respiratory infection other than otitis media, noninfectious, and total. Visit diagnosis hierarchy was as follows: any mention of otitis media (except chronic otitis media, resolved otitis media, follow-up or recheck otitis media, etc.) resulted in the visit being categorized under otitis media. Visits in which both otitis media and another illness were diagnosed were categorized as otitis media. Mention of upper or lower respiratory tract infections, respiratory syncytial virus, cough, or congestion without otitis media resulted in classification as respiratory tract infection. Physician visits were verified by monitoring the review of each subject's medical records during routine monitoring at frequent and predetermined intervals.
Statistics.
Subjects were randomized into formula groups to maintain balance among groups within each site, using a schedule derived from a standardized SAS program (SAS Institute, Cary, NC), with permuted blocks of size 2. The randomization was stratified by gender. Sample size was based on the number of subjects required to detect differences in the Hib-Farr response reported by Pickering et al. (14). A sample size of 77 evaluable subjects per group in a two-group parallel design with one-sided alternatives was expected to give an 80% power to detect at least a 0.4 SD difference between group means for log-to-base10 transformed Hib-Farr values.
All outcomes were reported as intent-to-treat analyses except for antibody responses to OPV. PV-VN1, PV-VN3, and poliovirus-specific IgA responses were reported on an evaluable subset excluding subjects that received injected inactivated poliovirus vaccine instead of the per protocol live oral poliovirus immunization. Criteria for evaluability targeted responses to mucosal immunization (OPV) and were established before unblinding data.
Hib-Farr responses were evaluated using one-tailed tests comparing the FN group to the F group. All other comparisons were two-tailed. Comparisons of the two formula groups were specified as primary analyses in the protocol. Two-group statistical tests were considered significant at the 0.05 level. Although it is not a truly randomized comparison group, the HMF group was compared with the formula-fed groups using post hoc three-group comparisons. Group comparisons of the Hib-Farr, anti-diphtheria IgG, anti-tetanus IgG, PV-VN1, PV-VN3, and poliovirus-specific IgA were performed by fitting RMA models using SAS PROC MIXED. Site was used as a blocking factor and sites with low enrollment were combined in these assessments. Vaccine response data were transformed using base-10 logarithms before analyses. Undetectable levels were replaced by half the assay threshold value. Adjustments for multiple comparisons were made using Holm's step-down procedure (29). The smallest p value was tested at 0.05/3 = 0.0167, the intermediate p value at 0.05/2 = 0.025, and the largest p value at 0.05.
Because of the large proportion of individuals who failed to generate cow milk-protein-specific IgE (60–81%), one categorical variable (response/no response, <0.10 KU/L) was created and Cochran-Mantel-Haenszel test was performed on the derived variables by using SAS PROC FREQ to compare the feeding effect.
Growth and safety data, and the number of physician visits with each illness category while on study feeding, were compared for the three groups using Poisson regression.
RESULTS
Subjects.
A total of 477 infants (147 F, 138 FN, and 192 HMF) were enrolled, and 381 (115 F, 113 FN, and 153 HMF) completed the 12-mo study. The most common reasons for dropping from the study included intolerance (n = 23), missing visits (n = 19), and removal by the investigator (n = 9). Tolerance problems reported by parents included fussing, gas, diarrhea, and spit-up. Demographics did not significantly differ between the formula-fed groups (Table 2), but in the HMF group, maternal education level was higher and smoking less common. There were no differences in maternal parity among the three feeding groups. The proportion of HMF subjects whose milk source was exclusively HM or HM in combination with formula, respectively, was 54% and 73% at 3 mo, 35% and 60% at 5 mo, 22% and 34% at 8 mo, and 15% and 30% at 12 mo.
Compliance.
Compliance with the feeding regimen was assessed using parent diaries of formula intake completed for 3 d before specified visits, monthly interviews with the parents, review of medical records, and formula disposition records. Only four formula-fed subjects consumed a nonstudy formula for more than a total of 7 d over the first 4 mo of exclusive formula or HM feeding. Thirty-seven formula-fed infants were given nonstudy formulas before 4 mo of age; volumes were small in each case and only 4 infants were given formulas potentially containing ribonucleotides that were consumed for longer than 7 d. Fifty-two infants had nonformula foods (15 had juice, 44 had cereal, 1 had meat, 7 had vegetables, 8 had fruit) before the wk 16 visit, and no feeding group-related statistical significance was associated with these feedings. Mean ages at the blood collection time points were not different between groups and very few subjects were outside specified visit windows. Compliance with the vaccination protocol was verified using subject vaccination records and was found to exceed 93% of active subjects at all time points for HibTITER and Tripedia. Despite the use of inactivated poliovirus vaccine in some subjects, compliance to the Orimune lots provided exceeded 90% at all time points.
Serologic and immunoglobulin responses.
From 2 to 6 mo of age, mean serum PV-VN1, PV-VN3, and poliovirus-specific IgA responses increased by 12-, 43-, and 22-fold, respectively, for all three feeding groups combined (Table 3). Poliovirus-specific antibody responses continued to increase at 7 mo followed by a decline in PV-VN1 and PV-VN3 at 12 mo. Poliovirus-specific IgA responses followed a similar pattern but were little changed from 7 to12 mo of age.
Comparing differences between groups the PV-VN1 response of the FN group was significantly higher than that of the F group when analyzed by the per-protocol two-group RMA (FN > F, p = 0.045) (Table 3). When compared using a post hoc three-group RMA, and after adjustment for multiple comparisons, a statistically significant difference was observed between HMF and F at 6 and 12 mo (HMF > F, p ≤ 0.0004), whereas no statistically significant difference was seen between HMF and FN. Because of a possible effect of weaning to formula without nucleotides, a post hoc repeated measures analysis was also performed on 6-, 7-, and 12-mo data, comparing vaccine responses in exclusively HMF subjects (ExHMF) with F and FN. Results showed that ExHMF infants had significantly higher PV-VN1 titers than F (p = 0.0105), FN marginally higher than F (p = 0.0438), and FN not statistically different from ExHMF (p = 0.332). Reverse cumulative distribution curves (RCFD, data not shown) plotting the distribution of infants achieving each neutralizing antibody titer, supported these group differences. Comparison of the RCFD curves revealed statistically significant distribution differences only at 12-mo (HMF different from F, p = 0.023) using the Kolmogorov-Smirnov test (30). Consistent with this observation, an additional post hoc analysis of PV-VN1 geometric mean titers by time point confirmed that differences detected between FN and F using RMA analyses were driven primarily by the difference at 12 mo (FN > F, p = 0.0086) (Fig. 1). Formula had no consistent or significant effect on PV-VN3 responses and frequency distributions indicated no clear differences among feeding groups. Two-month RCFD curves revealed that 50% of infants had 4-fold higher maternal-derived neutralizing antibody levels against PV1 than against PV3.
Antigen-specific antibody responses at 6, 7, and 12 mo from previous study (14) (A) and current study (B) expressed as ratios (nucleotide supplemented/nonsupplemented formulas). Statistically significant and marginal differences presenting the effect of nucleotide supplementation are shown for Hib total antibody (Farr), Hib IgG (ELISA), diphtheria, and poliovirus antibody responses. Statistically significant differences (*p < 0.05, two-group comparisons; **p = 0.045, two-group RMA). Reverse cumulative distributions were different at 12 mo (¶FN > FP = 0.023). Three-group per time point analysis comparing F, FN, and HMF (†FN > F, nonstatistically significant multiplicity adjusted trend p = 0.0086 at 12 mo). Three-group RMA comparing F, FN, and ExHMF (§, FN > F, nonstatistically significant trend p = 0.0438), (‡FN>F, nonstatistically significant trend p = 0.0552). In the study by Pickering et al. (14), infants received two OPV immunizations (2 and 4 mo) whereas infants in current study received three OPV immunizations (2, 4, and 6 mo).
Poliovirus-specific IgA titers (Table 3) in FN-fed infants were lower than those in the HMF group at 6 mo of age (p = 0.0001) but reached similar levels at 7 and 12 mo. Further, PV-IgA levels in HMF infants were higher than F-fed infants at both 6 (p = 0.0066) and 12 (0.0003) mo. Although no other significant differences were detected among feeding groups at any other time points, anti-poliovirus IgA titers for the FN group were 24% and 32% higher than F levels at 7 and 12 mo. Similar nonstatistically significant trends were also observed in a post hoc analysis of 12 mo data with ExHMF > F (p = 0.0330), and FN > F (p = 0.0552).
All three groups had strong (~10-fold) antibody responses to Hib at 7 mo following the 6-mo immunizations. At 12 mo, Hib antibody titers had dropped by approximately 4-fold to levels still considered protective. Although the anti-Hib antibody titers of the F and FN groups were not significantly different, the mean anti-Hib antibody titer for the FN group was 33% and 17% higher than the F group at 6 and 7 mo, respectively, and was similar to the HMF group (Table 3). There were no clinically relevant differences detected in Hib protection rate indicators (31) (anti-Hib antibody >1.0 μg/mL at 7 mo, F, 61%, FN, 63%, HMF, 61%; anti-Hib antibody >0.15 μg/mL at 12 mo, F, 78%, FN, 83%, HMF, 82%), although a transient nucleotide-associated increase in Hib protection rate was noted at 6 mo.
Serum anti-diphtheria IgG titers followed a normal pattern of response in each of the three feeding groups (Table 3). Following the second booster immunization at 6 mo, serum anti-diphtheria responses increased approximately 5- to 6-fold 1 mo later. There were no significant differences detected between formula-fed groups, and results were similar to those of the breast-fed group. However, as seen in the Hib-Farr results, the anti-diphtheria antibody titer group means for the FN group trended nonsignificantly higher than the F group at 6 and 7 mo (Table 3, Fig. 1).
Tetanus toxoid–specific IgG responses were similar in all feeding groups with a peak response at 7 mo followed by a return to near-baseline levels by 12 mo of age (Table 3). Unlike antibody responses to diphtheria toxoid, anti-tetanus responses were slightly lower at 6 mo compared with baseline values at 2 mo. The three feeding groups had similar serum IgA and IgG levels, except at the 2-mo time point when the HMF group had higher IgG levels (data not shown). Formula and HMF groups had similar plasma cow milk–specific IgE (Table 3) and total IgE concentrations (data not shown). A small number of HMF infants weaned from human milk appeared to have high outlier values that drove trends for cow milk–specific IgE to be higher in the HMF group.
Growth and safety.
Formula-fed infants did not differ in any growth measure from entry to 4 mo of age or at 12 mo of age. Growth was comparable to that of the HMF group. Average daily formula and energy intakes were similar for F and FN. Formula tolerance including stool consistency and average daily percent of feedings with spit up, were also similar for the formula groups. As expected, the HMF group experienced more frequent yellow stools and less odoriferous stools (32). The mean number of physician visits due to infectious or noninfectious episodes (3.8 ± 0.2 and 2.0 ± 0.2, respectively) was not different between HMF and formula groups. This was also the case for the number of visits with a diagnosis of otitis media (HMF, 1.7 ± 0.2; FN, 1.6 ± 0.2; F, 1.8 ± 0.2), respiratory tract infections independent of otitis media (HMF, 1.4 ± 0.1; FN, 1.5 ± 0.2; F, 1.4 ± 0.1) and other infections. No serious adverse events attributable to feeding groups were observed.
DISCUSSION
This study was designed to increase understanding of supplemental ribonucleotide effects on the immune status of infants. The working hypothesis was that ribonucleotide supplementation supports development of the infant immune system. This hypothesis was based on infant feeding studies showing ribonucleotide-associated increases in antibody responses (14,15) and observations from animal studies (7–11).
Based on established differences in immune development between infants fed human milk and those fed formula (2), we proposed that monitoring antibody responses to pediatric vaccines might reveal differences in selected immune parameters in infants fed formulas differing in ribonucleotide concentration. Antibody responses to vaccination are used to measure integrated immune responses (33) and, in this study, were used to reflect immune status during early development. Antibody responses are end products of complex processes and interruption of any step can reduce the magnitude of response. Attribution of differences in specific antibody response to dietary ribonucleotides requires that the response not be due to differences in vaccine potency or the immunologic ability to respond to vaccine challenge. For these reasons single lots of vaccine were selected and antibody responses were measured in infants of similar ages.
Pickering et al. (14) showed that ribonucleotide fortification (72 mg/L) of cow milk–based infant formula elevated peak antibody responses to Hib PRP and diphtheria toxoid, but not to tetanus toxoid or oral poliovirus vaccine. In the current study, primary analyses revealed trends for ribonucleotide-associated elevations of antibody to Hib PRP and diphtheria toxoid that failed to reach statistical significance. Primary analyses also revealed statistically significant ribonucleotide-associated increases in PV-VN1 response. Differences between ribonucleotide effects on PV-VN1 and PV-VN3 responses may reflect lower baseline PV-VN3 titers (maternal antibody) and a more rapid response after immunization with OPV. Changes to standard vaccination practice dictated that two aspects of the Pickering et al. (14) study could not be duplicated. Whereas the original study used whole cell Bordetella pertussis vaccine (DTwP) and OPV immunization at 2 and 4 mo of age, the current study used an acellular pertussis vaccine (DTaP) and an additional OPV immunization at 6 mo of age. These changes in immunization regimen may have contributed to vaccine response differences in results between Pickering et al. (14) and the current study.
Use of acellular pertussis vaccines is associated with reduced, but protective, antibody responses to diphtheria toxoid, tetanus toxoid, and the PRP antigen in HibTITER (34,35) when compared with whole-cell pertussis vaccines. Acellular Tripedia vaccine contains less diphtheria toxoid, two isolated pertussis components in place of killed whole cell pertussis, and less alum adjuvant than the DTwP version of Tripedia used by Pickering et al. (14). The antibody response to PRP is driven by the immunogenicity of the carrier (CRM197, recombinant diphtheria toxoid) (36). Less diphtheria toxoid may have led to lower Hib carrier immunogenicity resulting in lower Hib PRP antibody responses. In addition, a general lowering of Hib antibody titers after vaccination during the last decade has been reported (37). Thus, a plausible explanation for the discordance between the current Hib PRP and diphtheria toxoid antibody responses and those previously reported is that the current responses were limited by the intensity of the vaccine-specific response itself rather than the availability of ribonucleotides.
Antibody responses to Hib PRP, diphtheria toxoid, and tetanus toxoid were substantially reduced in the current study compared with those reported earlier using similar study designs. Pickering et al. (14) and Ostrom et al. (15) reported mean ribonucleotide supplemented peak anti-Hib PRP antibody responses of 7.24 μg/mL and 6.99 μg/mL, respectively, compared with 1.89 μg/mL in the current study. Similar lower titers were also observed in diphtheria and tetanus toxoid antibody responses. Demographic descriptors and parental smoking rates were similar in the two studies and there was significant geographic overlap in the participating sites. Unfortunately, Pickering et al. (14) did not determine maternal education as a proxy for socioeconomic status. Population differences are unlikely to have accounted for the statistical discrepancies in the antibody observations made in this study and Pickering et al. (14). Considering all available information, it is likely that the known lower potency of DTaP compared with DTwP used by Pickering et al. (14) contributed to the differences observed in antibody response with supplemental ribonucleotides. Despite these differences, the data are directionally consistent for Hib-Farr responses in both studies.
The current effect of ribonucleotides on PV-VN1 response is consistent with, but not identical to, previous reports (14,15). The primary two-group RMA evaluating change over time revealed a ribonucleotide-mediated elevation in PV-VN1 response, and a post hoc three-group RMA revealed that the HMF group had a significantly higher response than the F, but not the FN group, suggesting that ribonucleotides modified the PV-VN1 response to levels more like those of the HMF group. Similarly, Ostrom et al. (15) reported that 12-mo PV-VN1 responses in infants fed ribonucleotide-supplemented soy formula were intermediate between those of HMF and control groups. Perhaps because of the inherently high polymeric ribonucleotide levels in soy formulas, no significant differences were observed in antigen-specific vaccine responses between study formulas. Consistent with the current data, Pickering et al. (14) observed higher 6-mo PV-VN1 titers in the HMF group compared with both F and FN, and the same trend at 7 and 12 mo. The Pickering study infants received only 2- and 4-mo immunizations with OPV, and is likely responsible for the inability to detect a statistically significant difference between F and HMF at 7 and 12 mo. Here, RCFD curves and post hoc per time point comparisons indicated that differences between formula groups were driven primarily by higher 12-mo PV-VN1 titers in the FN group compared with the F group. Nonsignificant trends at 6 and 7 mo, however, appeared to contribute to the group differences as determined by RMA. Trends showing a nucleotide associated effect on polio IgA titers (polio type 1 ELISA) were also observed, the highest ratio occurring at 12 mo, consistent with that of the PV-VN1 response. It is interesting that although ribonucleotides were fed for the duration of the study, the most significant change in vaccine response occurred at 12 mo. Current data suggest that the decline in PV-VN1 titers between 7 and 12 mo was slower in FN and HMF groups than that of the F group.
Pickering et al. (14) and the present study have each identified statistically significant nucleotide-mediated improvement in immune response to some vaccine antigens. Results from the two cow milk–based studies are summarized in Figure 1 as ratios of antibody responses (FN/F) to the various vaccine antigens used. Antibody response data from these studies show statistically significant nucleotide associated differences for Hib (Hib-Farr and Hib IgG ELISA) and diphtheria in study 1 (14), poliovirus VN1 responses in study 2, and other trends in both studies supportive of effects of nucleotides on immune responses. Although the studies have not indicated statistically elevated antibody response(s) to the same vaccines, consistent trends have been observed in cases when statistical significance was not detected. When examined collectively, these study results are consistent with increased immune responses in infants fed ribonucleotide-supplemented formula (Fig. 1).
Further, no differences in the number of physician visits for infection or other reasons were observed among the three groups studied, suggesting equivalent safety outcomes. With respect to otitis media, although there appear to be more published studies reporting a protective role for breast-feeding (2), approximately one-third of such studies reported no such effect (38). It is possible that study population or study design differences might explain interstudy outcome differences. Differences between currently used infant formulas and those used in past studies might also be partially responsible. Data presented here were collected only for the first year of life and it is possible that observed nucleotide associated benefits (developmental pattern of cell mediated as well as modestly improved responses to some vaccines, closer to that of breast-fed infants) could be apparent during the second year and thereafter. Finally, similar to results reported earlier (14), no differences in cow's milk-specific or total IgE levels were observed between breast-fed and formula-fed infants.
We have shown that infants fed ribonucleotide-supplemented formula have improved humoral immune responses, and shifts in T-cell populations indicative of improved immune cell maturation (22). Although the impact of ribonucleotides on infant health is not firmly established at present, it is quite possible that these improvements in immune function could influence morbidity outcomes in infants to help close the morbidity gap identified between breast- and formula-fed infants (2). No gap was identified in the infant population studied in the current report. Had the present study been performed in a different infant population, it is possible that nucleotide-supplemented formula might provide a clinical profile closer to that of the breast-fed infant relative to unsupplemented formula. In this regard, it is most interesting that significant differences in key indicators of immune function (poliovirus VN1 responses and subjects of T and NK cells) were identified not only between formula groups but also more often between breast-fed infants and those fed formula without ribonucleotides.
The mechanism by which ribonucleotides enhance immune status is unknown. The finding of enhanced T-cell immune maturation reported in infants fed FN (22) complements vaccine antigen response data and may provide insight into a possible functional role in immune function as evidenced by the increase of some antibody responses. Ribonucleotides appear to play an important role in intestinal physiology. Dietary ribonucleotides are rapidly catabolized (39) in the intestinal epithelium (40,41), are efficiently absorbed into enterocytes as nucleosides and free bases (42), and were also shown to have discernible effects on intestinal vascular blood flow (43). Immune response to OPV primarily linked with efficient functioning of gut-associated immune cell populations may have been influenced by the presence of dietary ribonucleotides. This observation may explain the effect of FN on the PV-VN1 response, and, in this regard, modification of peripheral immune responses has also been reported (11,14). As others have postulated, gut-associated immune cell function appears to be modified by dietary ribonucleotides, leading to changes in gut-associated and peripheral immune responses (44).
CONCLUSIONS
These and previous data indicate that supplemental ribonucleotides, at levels (72 mg/L) and ratios similar to those in human milk, enhance immune status in formula-fed infants when assessed by antigen-specific antibody response to immunization. This effect occurs without modification of the safety profile associated with control formula. When considered together with data reported elsewhere (11,22) evidence indicates that supplemental ribonucleotides cause shifts in the development of T-cell populations, improves infant humoral immune status, and may help provide some of the immunologic benefits associated with breast-feeding.
Abbreviations
- DTaP:
-
diphtheria tetanus acellular pertussis vaccine
- ExHMF:
-
exclusive human milk-fed
- F:
-
formula without nucleotides
- FN:
-
formula with supplemented nucleotides
- Hib PRP:
-
Hib capsular polysaccharide (polyribosylribitol phosphate)
- Hib TITER:
-
Haemophilus influenzae type b vaccine
- HMF:
-
human milk-fed
- OPV:
-
oral poliovirus vaccine
- PV-VN1:
-
poliovirus type 1 neutralizing antibody
- PV-VN3:
-
poliovirus type 3 neutralizing antibody
- RCFD:
-
reverse cumulative frequency distribution
- RMA:
-
repeated measures analysis
- SWI:
-
Similac® with iron
References
Wilson C The physiologic immunodeficiency of immaturity. In: Stiehm ER (ed) Immunologic Disorders in Infants and Children. WB Saunders, Philadelphia, pp 255–263
Dewey KG, Heinig J, Nommsen-Rivers LA 1995 Differences in morbidity between breast-fed and formula-fed infants. J Pediatr 126: 696–702
Pickering LK, Morrow AL 1993 Factors in human milk that protect against diarrheal disease. Infection 21: 355–357
Feachem RG, Koblinsky MA 1984 Interventions for the control of diarrhoeal diseases among young children: promotion of breast-feeding. Bull World Health Organ 62: 271–291
Newburg DS, Pickering LK, McCluer RH, Cleary TG 1990 Fucosylated oligosaccharides of human milk protect suckling mice from heat-stabile enterotoxin of Escherichia coli. J Infect Dis 162: 1075–1080
Hanson LA, Ahlstedt S, Andersson B, Carlsson B, Fallstrom SP, Mellander L, Porras O, Soderstrom T, Eden CS 1985 Protective factors in milk and the development of the immune system. Pediatrics 75: 172–176
Kulkarni AD, Rudolph FB, Van Buren CT 1994 The role of dietary sources of nucleotides in immune function: a review. J Nutr 124: 1442S–1446S
Carver JD, Walker WA 1995 The role of nucleotides in human nutrition. J Nutr Biochem 6: 58–72
Jyonouchi H, Sun S, Abiru T, Winship T, Kuchan MJ 2000 Dietary nucleotides modulate antigen-specific type 1 and type 2 T-cell responses in young C57bl/6 mice. Nutrition 16: 442–446
Jyonouchi H, Sun S, Winship T, Kuchan MJ 2001 Dietary ribonucleotides modulate type 1 and type 2 T-helper cell responses against ovalbumin in young BALB/cJ mice. J Nutr 131: 1165–1170
Jyonouchi H, Sun S, Winship T, Kuchan MJ 2003 Dietary ribonucleotides increase antigen-specific type 1 T-helper cells in the regional draining lymph nodes in young BALB/cJ mice. Nutrition 19: 41–46
Carver JD, Pimentel B, Cox WI, Barness LA 1991 Dietary nucleotide effects upon immune function in infants. Pediatrics 88: 359–363
Martinez-Augustin O, Boza JJ, Del Pino JI, Lucena J, Martinez-Valerde A, Gil A 1997 Dietary nucleotides might influence the humoral immune response against cow's milk proteins in preterm neonates. Biol Neonate 71: 215–223
Pickering LK, Granoff DM, Erickson JR, Masor ML, Cordle CT, Schaller JP, Winship TR, Paule CL, Hilty MD 1998 Modulation of the immune system by human milk and infant formula containing nucleotides. Pediatrics 101: 242–249
Ostrom KM, Cordle CT, Schaller JP, Winship TR, Thomas DJ, Jacobs JR, Blatter MM, Cho S, Gooch WM III Granoff DM, Faden H, Pickering LK 2002 Immune status of infants fed soy-based formulas with or without added nucleotides for 1 year: part 1: vaccine responses, and morbidity. J Pediatr Gastroenterol Nutr 34: 137–144
Yau KI, Huang CB, Chen W, Chen SJ, Chou YH, Huang FY, Kua KE, Chen M, McCue M, Alarcon PA, Tressler RL, Comer GM, Baggs G, Merritt RJ, Masor ML 2003 Effect of nucleotides on diarrhea and immune responses in healthy term infants in Taiwan. J Pediatr Gastroenterol Nutr 36: 37–43
Martinez-Augustin O, Boza JJ, Navarro J, Martinez-Valverde A, Araya M, Gil A 1997 Dietary nucleotides may influence the humoral immunity in immunocompromised children. Nutrition 13: 465–469
Leach JL, Baxter JH, Molitor BE, Ramstack MB, Masor ML 1995 Total potentially available nucleosides of human milk by stage of lactation. Am J Clin Nutr 61: 1224–1230
Thorell L, Sjoberg LB, Hernell O 1996 Nucleotides in human milk: sources and metabolism by the newborn infant. Pediatr Res 40: 845–852
Brunser O, Espinoza J, Araya M, Cruchet S, Gil A 1994 Effect of dietary nucleotide supplementation on diarrhoeal disease in infants. Acta Paediatr 83: 188–191
Pelton, SI, Barnett, ED, Cabral HJ, Klein JO 1995 Lymphocyte phenotypes in breast and formula fed infants: potential implications for regulation of response to Haemophilus polysaccharide conjugate vaccine (HCV). Abstracts of the 35th Interscience Conference on Antimicrobial Agents and Chemotherapy, pp 168
Buck RH, Thomas DL, Winship TR, Cordle CT, Kuchan MJ, Baggs GE, Schaller JP, Wheeler JG 2004 Effect of dietary ribonucleotides on infant immune status. part 2: immune cell development. Pediatr Res 56: 891–900
American Academy of Pediatrics Committee on Infectious Diseases 1996 Recommended childhood immunization schedule. Pediatrics 97: 143
Recommended childhood immunization schedule–United States 1997. MMWR Morb Mortal Wkly Rep, 46: 35–40 erratum 227
Lasekan JB, Ostrom KM, Jacobs JR, Blatter MM, Ndife LI, Gooch WM III . Cho S 1999 Growth of newborn, term infants fed soy formulas for 1 year. Clin Pediatr 38: 563–571
American Academy of Pediatrics, Committee on Nutrition 1993 Pediatric Nutrition Handbook, 3rd Ed. Elk Grove Village, IL, American Academy of Pediatrics
Granoff DM, Shackelford PG, Pandey JP, Boies EG 1986 Antibody responses to Haemophilus influenzae type B polysaccharide vaccine in relation to Km(1) and G2m(23) immunoglobulin allotypes. J Infect Dis 154: 257–264
Faden H, Modlin JF, Thoms ML, McBean AM, Ferdon MB, Ogra PL 1990 Comparative evaluation of immunization with live attenuated and enhanced-potency inactivated trivalent poliovirus vaccines in childhood: systemic and local immune responses. J Infect Dis 162: 1291–1297
Holm S 1979 A simple sequentially rejective test procedure. Scand J Stat 6: 65–70
Hollander M, Wolfe DA 1973 Nonparametric Statistical Methods. Wiley, New York 219–228
Eskola J, Ward J, Dagan R, Goldblatt D, Zepp F, Siegrist CA 1999 Combined vaccination of Haemophilus influenzae type b conjugate and diphtheria-tetanus-pertussis containing acellular pertussis. Lancet 354: 2063–2068
Lloyd B, Halter RJ, Kuchan MJ, Baggs GE, Ryan AS, Masor ML 1999 Formula tolerance in post breastfed and exclusively formula-fed infants. Pediatrics 103: E7
Wheeler JG, Steiner D 1992 Evaluation of humoral responsiveness in children. Pediatr Infect Dis J 11: 304–310
Decker MD, Edwards KM 1999 Combination vaccines. In: Plotkin S (ed) Vaccines. WB Saunders, Philadelphia pp 508–530
Giuliano M, Mastrantonio P, Giammanco A, Piscitelli A, Salmaso S, Wassilak SG 1998 Antibody responses and persistence in the two years after immunization with two acellular vaccines and one whole-cell vaccine against pertussis. J Pediatr 132: 983–988
Granoff DM, Holmes SJ, Belshe RB, Osterholm MT, McHugh JE, Anderson EL 1994 Effect of carrier protein priming on antibody responses to Haemophilus influenzae type b conjugate vaccines in infants. JAMA 272: 1116–1121
Granoff DM 2001 Assessing efficacy of Haemophilus influenzae type b combination vaccines. Clin Infect Dis 33( suppl 4) S278–S287
Paradise JL, Rockette HE, Colborn DK, Bernard BS, Smith CG, Kurs-Lasky M, Janosky JE 1997 Otitis media in 2253 Pittsburgh-area infants: prevalence and risk factors during the first two years of life. Pediatrics 99: 318–333
Edozien JC, Udo UU, Young VR, Scrimshaw NS 1970 Effects of high levels of yeast feeding on uric acid metabolism of young man. Nature 228: 180
Boza JJ, Jahoor F, Reeds PJ 1996 Ribonucleic acid nucleotides in maternal and fetal tissues derive almost exclusively from synthesis de novo in pregnant mice. J Nutr 126: 1749–1758
Rueda R, Gomez-Leon C, Gil A 2002 Ribonucleic acid hydrolysis by intestinal explants of neonatal piglets. J Pediatr Gastroenterol Nutr 35: 685–690
Salati LM, Gross CJ, Henderson LM, Saviano DA 1984 Absorption and metabolism of adenine, adenosine-5′-monophosphate, adenosine and hypoxanthine by the isolated vascularly perfused rat small intestine. J Nutr 114: 753–760
Carver JD, Saste M, Sosa R, Zaritt J, Kuchan M, Barness LA 2002 The effects of dietary nucleotides on intestinal blood flow in preterm infants. Pediatr Res 52: 425–429
Rueda R, Gil A 2000 Influence of dietary compounds on intestinal immunity. Microb Ecol Health Dis 12( suppl 2) 146–156
Acknowledgements
The authors thank the following people for technical support: Marc Masor, Ph.D., Ross Products Division, Abbott Laboratories; Howard Faden, M.D., Division of Infectious Diseases, Children's Hospital, Buffalo, NY; and Daniel M. Granoff, M.D., Children's Hospital/Oakland Research Institute, Oakland, CA. We thank Pam Newton, R.N., Tim Murphy, MS, John Lasekan, Ph.D., Peter Hu, Ph.D., Amy Bates, Joe Laco, Pete Yakimovich, and Melissa Nameth, all of Ross Products Division, Abbott Laboratories, for technical assistance. We also thank the following participant physicians: Wilson Andrews, Mark Blatter, Iqbal Choudhry, David Ferrera, William Forti, Martin Greenberg, Terry Jefferson, Susan Kerns, Jacob Lohr, Edgardo Malacaman, Michael Pichichero, Bruce Pistorius, Robert Reis, Allan Robinson, Laurie Schnell, and Michael Smith.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by grants from the Ross Products Division of Abbott Laboratories.
Rights and permissions
About this article
Cite this article
Schaller, J., Kuchan, M., Thomas, D. et al. Effect of Dietary Ribonucleotides on Infant Immune Status. Part 1: Humoral Responses. Pediatr Res 56, 883–890 (2004). https://doi.org/10.1203/01.PDR.0000145576.42115.5C
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.PDR.0000145576.42115.5C
This article is cited by
-
Composition and properties of bovine colostrum: a review
Dairy Science & Technology (2016)
-
Whey-derived valuable products obtained by microbial fermentation
Applied Microbiology and Biotechnology (2015)
-
Simultaneous Determination of Ten Nucleosides and Related Compounds by MEEKC with [BMIM]PF6 as Oil Phase
Chromatographia (2013)
-
Fermentative production of ribonucleotides from whey by Kluyveromyces marxianus: effect of temperature and pH
Journal of Food Science and Technology (2013)
-
Lactation and Neonatal Nutrition: Defining and Refining the Critical Questions
Journal of Mammary Gland Biology and Neoplasia (2012)