Abstract
Hydrophobic bile acids are implicated in the pathogenesis of cholestatic liver disorders through mechanisms involving oxidative stress and mitochondrial dysfunction. Antioxidants ameliorate bile acid–induced cytotoxicity in rat hepatocyte suspensions. The purpose of the current study was to evaluate the potential protective role of β-carotene (βC), a putative fat-soluble antioxidant that is reduced in patients with cholestasis, against bile acid–induced hepatotoxicity. In freshly isolated rat hepatocyte suspensions that were exposed to the toxic hydrophobic bile acid glycochenodeoxycholic acid (100 or 500 μM), βC (100 μM) decreased generation of reactive oxygen species by >50%, similar to the inhibition afforded by β-tocopherol. Commensurate with this antioxidant effect, 100 μM βC also protected hepatocytes against both glycochenodeoxycholic acid–induced cellular necrosis and apoptosis, which was associated with reduction in caspase 3 activation, inhibition of mitochondrial cytochrome c release in rat hepatocytes, and prevention of the mitochondrial permeability transition in both liver mitochondria and rat hepatocytes. A lower concentration of βC (50 μM) produced similar antioxidant and anti-apoptotic protection but with less inhibition against cell necrosis, suggesting that the higher concentration of βC may have conferred additional cytoprotection not directly related to its antioxidant function. These results demonstrate that the antioxidant effects of βC may provide hepatoprotection against cholestatic liver injury by preventing bile acid–induced oxidative stress and mitochondrial perturbations.
Similar content being viewed by others
Main
The preventive roles of dietary antioxidants, such as vitamin E (including tocopherols and tocotrienols) and ascorbic acid, have been evaluated extensively as potential protective agents toward several diseases or conditions in humans, including cancer, heart disease, and cataractogenesis (see Refs. 1 and 2 for overviews). The mechanism of protection afforded by these agents is generally consistent with their antioxidant activities, although inhibition of cellular mediators, including protein kinases and eicosanoids, have also been implicated (3, 4). In addition to these antioxidant vitamins, β-carotene (βC) may function as a physiologically relevant antioxidant along with its well-defined role as a precursor to vitamin A (for review, see Ref. 5). However, despite the seminal report by Burton and Ingold (6), who found that βC functioned as an efficient antioxidant in chemical systems, recent large-scale human studies with the carotenoid have been disappointing. For example, βC failed to protect human subjects against lung cancer and coronary artery disease (7, 8). Consequently, the Panel on Dietary Antioxidants and Related Compounds of the Food and Nutrition Board of the Institute of Medicine determined that βC does not meet the definition of a dietary antioxidant and that βC supplementation should not be recommended (9). In contrast to the studies that evaluated βC's role in the prevention of cancer and atherosclerosis, few studies have addressed the potential protective effects of βC in hepatobiliary diseases. Recent reports show that 1) βC is malabsorbed in various hepatobiliary diseases (10–12); 2) serum βC levels are very low in adults with the cholestatic liver disorders (CLD), primary biliary cirrhosis, and primary sclerosing cholangitis (12) and in children with cholestasis (13); and 3) antioxidant therapy improved symptoms in patients with cholestasis in a recent pilot study (14). Thus, a lack of adequate βC may play a role in potentiating liver injury in CLD.
Recent studies from our laboratory demonstrate in both in vivo and in vitro models that oxidative stress is a key mediator for the hepatic injury observed in CLD. These diseases, characterized by an impairment of bile flow or secretion that results in increased concentrations of bile constituents within the liver and subsequent hepatotoxicity, include biliary atresia, neonatal hepatitis, progressive familial intrahepatic cholestasis, a variety of metabolic liver disorders, cystic fibrosis, and primary sclerosing cholangitis in childhood. Because treatment for many of these disorders is inadequate, liver transplantation is frequently required in affected children and adults (15). One primary factor implicated in cholestasis is the accumulation of hydrophobic bile acids within the liver (16), which have been demonstrated to be toxic to freshly isolated and cultured hepatocytes, liver mitochondria, and whole animals (17–20). Hepatocytes that are exposed to lower concentrations of hydrophobic bile acids (≤100 μM) typically undergo apoptotic cell death (20, 21), whereas at higher concentrations, these compounds promote cell necrosis through oxidative stress, ATP depletion, hepatocyte swelling, and disruption of the plasma membrane (17, 20). Both modes of bile acid–induced cell death are believed to be important in the pathogenesis of CLD through generation of oxidative stress (17, 22).
Mechanistic studies of bile acid–induced apoptosis and/or necrosis have also focused attention on induction of the mitochondrial permeability transition (MPT) as a critical event preceding cell death (19, 23–25). The MPT is characterized by large-amplitude swelling and loss of the electrochemical potential across the inner mitochondrial membrane caused by opening of a megachannel (MPT pore) spanning both the inner and the outer mitochondrial membranes (26, 27). Upon induction of the MPT, several intermembranous space proteins are released into cytosol, including the pro-apoptotic signal cytochrome c and several inhibitors of apoptosis (28). Of particular interest are findings correlating increased generation of reactive oxygen species (ROS) with stimulation of the MPT by bile acids (19, 22, 25), most likely via the oxidative modification of MPT pore proteins (29). Commensurate with their ability to inhibit the MPT and cytochrome c release from mitochondria, antioxidants such as α-tocopherol (α-TH), ebselen, and idebenone also reduce bile acid–induced cellular necrosis and apoptosis in rat hepatocytes (17, 25).
Because βC has been proposed as an antioxidant and levels of βC are low in cholestatic liver injury, the current study was performed to determine the potential antioxidant and cytoprotective effects of βC toward glycochenodeoxycholic acid (GCDC)-induced hepatocyte toxicity by addressing the following questions that are relevant to the pathogenesis of CLD:1) Can βC function as an antioxidant in rat hepatocytes that are exposed to a bile acid–induced oxidative stress?2) Can βC prevent bile acid–induced hepatocyte cytotoxicity?3) What are the mechanisms responsible for the cytoprotective effects afforded by βC against bile acid–induced hepatotoxicity?
METHODS
All chemicals were obtained in reagent-grade quality from suppliers. BSA-fraction V (BSA) and alcohol-soluble digitonin were obtained from Calbiochem (La Jolla, CA, U.S.A.). GCDC (Na+salt) and βC (type 1) were obtained from Sigma Chemical Co. (St. Louis, MO, U.S.A.). 2,7-dichlorofluorescin diacetate (DCF-DA) was purchased from Eastman Kodak Co. (Rochester, NY, U.S.A.), and the fluorescent probe JC-1 was purchased from Molecular Probes (Eugene, OR, U.S.A.). R,R,R-(α-TH) was obtained from Fisher Scientific (Pittsburgh, PA, U.S.A.). All other reagents unless stated were reagent grade or better.
Isolation of rat hepatocytes and liver mitochondria.
Humane care was given to all experimental animals, and this study was approved by the Institutional Animal Care and Use Committee of the University of Colorado Health Sciences Center. Hepatocytes were isolated by a recirculating collagenase technique from 175- to 225-g male Sprague Dawley rats (Sasco, Inc., Omaha, NE, U.S.A.) maintained on a 12-h light-dark cycle and fed standard laboratory rat diet, as previously described (17). Initial hepatocyte viability measured by trypan blue exclusion was always >94%. Freshly isolated hepatocytes were resuspended in a Krebs Ringers HEPES (KRH) buffer containing 0.2% BSA (KRH/BSA) to a concentration of ∼1 × 106/mL and preincubated for 30 min at 37°C with βC (50 or 100 μM, dissolved in DMSO), 100 μM α-TH, or both 100 μM βC and α-TH to determine whether the antioxidant effects were additive or synergistic. After the preincubation period, 100 or 500 μM GCDC was added and hourly aliquots of cell suspension were removed to determine their effects on ROS generation, cell necrosis, and apoptosis. For immunoblot analysis, aliquots were withdrawn after 3 h of incubation.
Measurement of ROS generation in rat hepatocytes.
For determining whether βC could function as an antioxidant in this model, generation of ROS was measured by spectrofluorescence using the hydroperoxide detecting probe DCF-DA as previously described in detail (17). Briefly, hepatocytes were preloaded with DCF-DA for 30 min at 37°C before the addition of antioxidants. After an additional 30-min preincubation with antioxidants, hepatocytes were exposed to GCDC (100 or 500 μM) for 4 h and hourly aliquots were removed for analysis of ROS by measuring 2′7′-dichlorofluorescein (DCFein) fluorescence at 490-nm excitation and 520-nm emission. Results were expressed as picomoles per 106 cells based on a standard curve using DCFein.
Determination of hepatocyte apoptosis and necrosis.
Hepatocyte apoptosis was quantified by determining the percentage of hepatocytes with nuclear morphologic changes of apoptosis detected by fluorescence microscopy of 4′6-diamidino-2-phenylindole–stained fixed hepatocytes, as previously described (21). Necrosis was determined by the release of lactate dehydrogenase activity from cells, as previously described (21), and expressed as the percentage of total cellular activity released into the media.
Immunoblot analysis of cytochrome c release and caspase 3 activation.
To determine the extent of mitochondrial cytochrome c release in isolated rat hepatocytes that were exposed to GCDC and βC, we used the protocol of selective digitonin permeabilization as originally described by Leist et al. (30) and as modified by Qiao et al. (31). Briefly, after 3 h of incubation with 100 μM GCDC with or without antioxidants, 4–6 × 106 cells were pelleted by centrifugation, washed once with KRH buffer (no BSA), and recentrifuged to obtain hepatocyte pellets. Hepatocytes were resuspended in a cell permeability buffer containing 75 mM NaCl, 8 mM Na2HPO4, 1 mM NaH2PO4, 1 mM EDTA, and 250 mM sucrose (pH 7.4) containing 350 μg/mL digitonin for 30 s and centrifuged at 13,000 × g for 1 min. The cytosolic supernatant fraction was collected, and protein concentration was determined by Lowry et al. (32). Approximately 15–25 μg of protein was loaded onto a 12% SDS-PAGE and transferred to nitrocellulose membrane and probed with 1–2 μg/mL purified mouse anti–cytochrome c MAb (BD Biosciences, San Diego, CA, U.S.A.). Cytochrome c was detected colorimetrically with stabilized 3,3′,5,5′-tetramethylbenzidine (Promega, Madison, WI, U.S.A.) and quantified by densitometry using UN-SCAN-IT gel software (Silk Scientific, Orem, UT, U.S.A.).
For caspase 3 immunoblotting, a cytosolic fraction was obtained as follows: 2 × 106 cells were pelleted by centrifugation, washed once with KRH buffer (no BSA), and recentrifuged to obtain hepatocyte pellets. Cells were lysed by the addition of 200–300 μL of 3-[3-cholamidopropyl)dimethyl, ammonio]-1-propanesulfonate Cell Extract Buffer (Cell Signaling Technology, Beverly, MA, U.S.A,) containing 5 mM DTT and 1 mM phenylmethylsulfonyl fluoride. The cell suspension was subjected to three freeze–thaw cycles before centrifugation at 13,000 × g for 5 min. The supernatants were collected, and protein concentration was determined by the Bradford assay (33). Electrophoresis and analysis were carried out as described for cytochrome c except that 50–100 μg of protein was loaded onto 12% SDS-PAGE, and the blots were incubated with 1:50 dilution of mouse monoclonal anti–caspase 3 (Santa Cruz Biotechnology, Santa Cruz, CA, U.S.A.). Equal loading was confirmed in selected experiments by also probing blots against a 1:5000 dilution of anti-actin MAb followed by a 1:2000 dilution of goat anti-mouse IgM-specific horseradish peroxidase (Oncogene Research Products, Boston, MA, U.S.A.).
Flow cytometry.
Flow cytometric analysis was performed to determine the effect of βC on GCDC-induced MPT in freshly isolated hepatocytes, as previously described in detail (34). Briefly, freshly isolated hepatocytes were pretreated with 50–100 μM βC for 30 min before exposure to 100 μM GCDC for 4 h. Hourly aliquots of cells were removed, loaded with 7.6 μM JC-1 or 3 μM propidium iodide (PI) for 15 min at 22°C in the dark, and washed with KRH buffer at 4°C before flow cytometry on a Becton Dickinson FACS Calibur (Becton Dickinson Immunocytometry Systems, San Jose, CA, U.S.A.) using CELLQuest software. In actively respiring mitochondria, JC-1 aggregates form and the intensity of their fluorescence at 590 nm is proportional to the mitochondria mitochondrial electrochemical gradient (Δψ) and indicative of a closed MPT pore (βC alone had no effect on JC-1 fluorescence). Approximately 10,000 cells were analyzed for each time point and treatment. The fluorescence of JC-1 aggregates was determined only in live cells (as determined by PI staining) by gating on hepatocytes that showed no uptake of PI.
Measurement of the MPT.
Rat liver mitochondria were isolated by differential centrifugation of liver homogenate through a Percoll gradient, and the MPT assay was performed as previously described in detail (22). Briefly, hepatic mitochondria (1.5–3.0 mL) in respiration buffer [125 mM sucrose, 100 mM NaCl, 10 mM MOPS (pH 7.4) treated with 1% Chelex-100] were incubated at 25°C for 5 min alone or in the presence of 10–250 μM βC. After the preincubation period, 100 μM CaCl2, 5 mM sodium succinate, and 5 μM rotenone (in dimethylformamide) were added to mitochondria, and the absorbance at 540 nm was monitored for 5 min. The MPT was then induced by the addition of 100 μM GCDC, and absorbance was monitored continuously for an additional 5 min.
Statistical analysis.
Mean and SEM were calculated for each time point. Comparisons among groups were performed by ANOVA and the Scheffe test or t test when appropriate. P < 0.05 was considered statistically significant.
RESULTS
β-carotene reduces GCDC-stimulated ROS generation.
Because the antioxidative function of βC in biologic systems is controversial (35), we first undertook an evaluation of the effect of βC on ROS generation under conditions of excess hydrophobic bile acids that may exist in the cholestatic liver. Freshly isolated rat hepatocyte suspensions that were exposed to either 100 or 500 μM GCDC generated increased ROS (hydroperoxides) in a time-dependent manner when compared with untreated cells (Fig. 1a and b). Pretreatment with βC led to a >50% reduction in ROS generation in GCDC-exposed hepatocytes at 4 h and was not dose dependent. The effects of βC were compared with that observed with α-TH, an antioxidant previously demonstrated to inhibit ROS generation in rat hepatocytes and liver mitochondria that were exposed to GCDC (17, 22). Figure 1c indicates that the antioxidative potencies of βC and α-TH were identical in preventing ROS generation in rat hepatocytes that were exposed to 100 μM GCDC and that no additive or synergistic effects were observed when the antioxidants were combined.
βC prevents generation of ROS in isolated rat hepatocytes that were exposed to GCDC. Hepatocytes (106/mL) were loaded with 10 μM DCF-DA for 30 min at 37°C and, where indicated, preincubated for an additional 30 min with βC (50–100 μM) or vehicle before the addition of either 100 μM (a) or 500 μM (b) GCDC. (c) The antioxidative effect of 100 μM βC was compared with that of 100 μM α-TH alone or in combination. Hourly aliquots were removed, and ROS generation was determined by fluorescence of DCFein, as described in “Methods.” Results are expressed as mean ± SEM of at least four separate experiments.
βC protects rat hepatocytes against GCDC-induced cell necrosis and apoptosis.
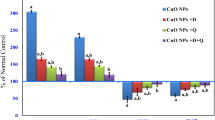
We next sought to determine whether the observed antioxidative effect of βC was associated with cytoprotection against GCDC-induced necrosis and apoptosis. To assess the effects of varying concentrations of βC on GCDC-induced cell necrosis, rat hepatocyte suspensions were exposed to either 100 or 500 μM GCDC, and cell necrosis was quantified by release of lactate dehydrogenase from cells. By 4 h of incubation (Fig. 2a and b), GCDC caused significant cell necrosis at both GCDC concentrations when compared with untreated cells (14 ± 1% for control versus 35 ± 2% for 100 μM GCDC versus 47 ± 4% for 500 μM GCDC). Preincubation of cells with 100 μM βC protected hepatocytes against cellular necrosis, whereas the lower concentration of βC (50 μM) protected hepatocytes against 100 μM GCDC but not 500 μM of the bile acid. When cells were exposed to 100 μM GCDC, a significant increase in protection was afforded by the combination of 100 μM βC and 100 μM α-TH compared with 100 μM βC or α-TH alone (Fig. 2c).
βC inhibits GCDC-induced cellular necrosis in isolated rat hepatocytes. Hepatocytes were preincubated for 30 min at 37°C with βC (50–100 μM) or vehicle before the addition of either 100 μM (a) or 500 μM (b) GCDC to promote cell necrosis. (c) The antioxidative effect of 100 μM βC was compared with that of 100 μM α-TH alone or in combination. Hourly aliquots were removed for determination of cell necrosis (% lactate dehydrogenase release), as described in “Methods.” Results are expressed as mean ± SEM of at least four separate experiments.
Isolated rat hepatocytes that are exposed to 100 μM GCDC undergo significant apoptosis by 2 h, which continues to increase by 4 h of incubation (Fig. 3; 43% of GCDC-treated cells versus 1% untreated cells at 4 h). Pretreating hepatocytes with 50 μM βC reduced bile acid–induced apoptosis by approximately 50% at 2 h and 35% at 4 h; 100-μM βC concentration was associated with somewhat better protection against apoptosis at 4 h. Pretreating cells with 100 μM α-TH led to a similar reduction of GCDC-induced apoptosis as that produced by 100 μM βC; 100 μM βC combined with α-TH had a mild additive protective effect (data not shown).
βC inhibits GCDC-induced apoptosis in isolated rat hepatocytes. Hepatocytes were preincubated for 30 min at 37°C with βC (50–100 μM), α-TH, or vehicle before the addition of 100 μM GCDC to induce cell apoptosis. Hourly aliquots were removed for determination of apoptosis as assessed by the percentage of cells with nuclear morphologic changes observed under fluorescence microscopy, as described in “Methods.” Results are expressed as mean ± SEM of at least four separate experiments.
Inhibition by βC of GCDC-induced MPT in liver mitochondria.
Induction of the MPT by a variety of toxic agents is believed to be a critical step in mediating cell death by necrotic and apoptotic pathways. GCDC (100 μM) led to a rapid decrease in absorbance of liver mitochondria at 540 nm, representative of mitochondrial swelling and induction of the MPT. βC exerted a dose-dependent inhibition of the MPT in this model (Fig. 4a). The MPT was verified by the complete inhibition of the GCDC-induced mitochondrial swelling by preincubation with cyclosporin A. A comparison of the dose-dependent effects of βC and α-TH on GCDC-induced MPT (Fig. 4b) shows that the profile of MPT inhibition afforded by each of the antioxidants is nearly identical.
Dose-dependent inhibition by βC of GCDC-induced MPT in liver mitochondria. Suspensions of liver mitochondria were preincubated with 0–250 μM βC or α-TH, or 1 μM cyclosporin A (CsA) for 5 min before the addition of 100 μM GCDC to induce the MPT. Mitochondrial swelling was measured spectrophotometrically as a reduction in absorbance at 540 nm over 5 min. (a) A typical tracing demonstrates the dose-dependent inhibition of MPT induced by 100 μM GCDC in liver mitochondria and the complete blockage of MPT by CsA. (b) The dose-dependent protection against GCDC-induced MPT by βC and α-TH is shown. MPT is expressed as the change in absorbance during the 5 min of exposure of mitochondria to 100 μM GCDC Results are expressed as mean ± SEM of at least four separate experiments.
Effect of βC on GCDC-induced cytochrome c release and caspase 3 levels.
The suppression of bile acid–induced hepatocyte apoptosis by βC suggests that the carotenoid may alter critical steps in the induction of hepatocyte apoptosis. Therefore, we determined the effect of βC on two important events in the execution of hepatocytes apoptosis, release of cytochrome c from mitochondria and activation of caspase 3 (Fig. 5). Examination of postmitochondrial supernatant from hepatocytes that were treated with 100 μM GCDC indicated that exposure to GCDC for 3 h stimulated release of cytochrome c from mitochondria when compared with untreated hepatocytes (Fig. 5a). Pretreating cells with 100 μM βC, 100 μM α-TH, or the combination abrogated release of cytochrome c from mitochondria. To determine the effect of antioxidants on GCDC-stimulated caspase 3 activation, we analyzed the amount of procaspase 3 levels in cytosol of hepatocytes by immunoblotting (Fig. 5b). Results from these experiments demonstrated that procaspase 3 in cells exposed to 100 μM GCDC for 3 h was reduced, indicative of caspase 3 activation (Fig. 5b). Pretreating hepatocytes with βC, α-TH, or the combination prevented the reduction of procaspase levels, concomitant with protection against apoptosis (Fig. 3). Similar loading of lanes with cytosol was indicated by the immunoblots for β–actin (Fig. 5c).
βC and α-TH prevent GCDC-induced cytochrome c release and caspase 3 activation in rat hepatocytes. The effects of βC (100 μM), α-TH (100 μM), both antioxidants, or no treatment (control-C) on GCDC-induced cytochrome c release from mitochondria into cytosol of hepatocytes (a) and caspase 3 activation (b) were determined after 3 h of incubation, as described in “Methods.” Samples of cytosol from hepatocytes were immunoblotted against mouse anti–cytochrome c MAb in a or mouse anti–caspase 3 MAb in b. In selected experiments, blots that were probed with anti–caspase 3 antibodies were stripped and reprobed with anti-actin antibodies (c) to demonstrate similar loading. Results shown are representative of at least two separate experiments.
βC prevents GCDC-induced mitochondrial depolarization in rat hepatocytes.
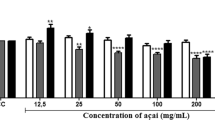
Induction of the MPT is associated with increased oxidative stress in hepatocytes that were treated with hydrophobic bile acids. Inasmuch as βC reduced ROS generation and inhibited the MPT in isolated mitochondria, we next determined whether βC affected the MPT in live hepatocytes. To measure MPT in intact cells, we assessed mitochondrial Δψ in isolated hepatocytes by flow cytometric analysis using the probe JC-1 (Fig. 6). Exposure of hepatocytes to 100 μM GCDC caused a significant decrease in fluorescence of JC-1 aggregates in hepatocytes at 2 h, indicative of reduction of mitochondrial Δψ and opening of the MPT pore. Pretreating cells with 50–100 μM βC significantly prevented the reduction in JC-1 aggregate fluorescence at 3 and 4 h. These results demonstrate that βC blocked the MPT concurrent with inhibition of ROS generation and reduced activation of caspase 3 and inhibition of apoptosis.
The effect of βC on GCDC-induced collapse of mitochondrial Δψ in rat hepatocytes. Isolated rat hepatocytes were exposed to 100 μM GCDC in the absence or presence of 50–100 μM βC. Hourly aliquots were removed, loaded with JC-1 and PI for 15 min at 22°C, and washed with KRH buffer before fluorescence determination at 590 nm for JC-1. JC-1 aggregate fluorescence in live cells (PI-negative), which represents an intact mitochondrial Δψ, was significantly reduced by 2 h of incubation with GCDC (red line) compared with untreated cells (black line). Preincubation of hepatocytes with either 50 μM βC (blue line) or 100 μM βC (green line) prevented the GCDC-induced reduction in JC-1 aggregate fluorescence, indicating that the bile acid–induced mitochondrial depolarization was inhibited by βC. βC alone failed to affect JC-1 aggregate fluorescence when compared with control cells (data not shown). The horizontal bar indicates the percentage of the population of cells exhibiting the designated fluorescence. Results shown are representative of at least two separate experiments.
DISCUSSION
Results from the current study using an in vitro model of cholestatic liver injury demonstrate that βC, a carotenoid of nutritional and physiologic significance, protects rat hepatocyte suspensions from hydrophobic bile acid–induced cell apoptosis by a mechanism consistent with its putative antioxidant activity. Concentrations of βC in human liver vary widely, with its concentration in nonsupplemented individuals ranging from 6 to 25 nmol/g liver (35, 36). Assuming 140,000 × 106 hepatocytes/g wet weight of liver, with 5 μL of water per 106 hepatocytes (37), the range of liver concentrations of βC are converted to 9–36 μM. However, in hepatobiliary disorders, concentrations of liver and serum βC are substantially decreased (10, 12, 13, 36). Therefore, the concentrations of βC chosen in this study are close to the range of normal values, particularly when considering the accelerated time course needed to achieve intracellular βC concentrations in isolated hepatocyte incubations.
The antioxidative effect and cytoprotection afforded by βC in these experiments were nearly identical to that of α-TH, an antioxidant previously reported to protect rat hepatocytes from bile acid–induced cell death (17, 18). The anti-apoptotic effect of βC was further characterized by demonstrating inhibition of both caspase 3 activation and loss of mitochondrial Δψ in cells that were exposed to the toxic bile acid and significant reduction of the MPT in liver mitochondria incubated with the bile acid. Taken together, these results support an antioxidative and anti-apoptotic role of βC under conditions that may exist in the cholestatic liver.
The cytoprotective effects of βC reported in this study provide evidence that βC may protect mammalian cells that are subjected to oxidative stress–dependent apoptosis. Although the antioxidative function of βC in vivo is a source of considerable controversy (38, 39), there is extensive evidence that βC functions as an antioxidant under a variety of in vitro conditions. In the original study by Burton and Ingold (6), βC prevented peroxidation of methyl linoleate in a unique manner when compared with previously characterized mechanisms of other antioxidants. The hypothesized mechanism of βC anti-oxidant protection against lipid oxidation was that of a chain-breaking antioxidant by efficient trapping of peroxyl radicals resulting in generation of lipid hydroperoxides. As hydrophobic bile acids have been shown to increase generation of hydroperoxides (17, 19), it is possible that βC functioned as an antioxidant in the current study by protecting membrane lipids from propagating oxidative damage through termination of peroxyl radical-mediated reactions. Inhibition of DCFein fluorescence, a measurement of intracellular peroxide generation, by βC would support this antioxidative mechanism. A second, less likely explanation for the reduction of ROS generation by βC was its role as a quencher of electronically excited singlet oxygen (40, 41). Although studies have reported generation of singlet oxygen in hepatocytes (42), no evidence exists that this photochemically generated intermediate is produced in bile acid–treated hepatocytes under the conditions used in this study (which did not use photosensitizing agents).
At the higher concentration of βC used in this study (100 μM), we observed a significant inhibition of GCDC-induced generation of ROS, reduction of cellular apoptosis, and reduced cell necrosis. It is interesting that when a lower concentration of the carotenoid was examined (50 μM), we observed nearly identical antioxidant and anti-apoptotic protection to that of the higher dose but a lesser degree of protection against cellular necrosis. A similar observation was noted when comparing the effects of a combination of βC and α-TH (100 μM each) toward ROS generation (Fig. 1c) and cellular necrosis (Fig. 2c), where the combination failed to decrease ROS generation further yet provided increased protection against necrosis, suggesting that once a maximal level of antioxidant protection is achieved, increased potentiation against cellular necrosis continued. Explanations for the increased cytoprotection conferred by 100 μM βC include 1) possible nonantioxidant functions for the carotenoid (43), 2) increased concentrations of the carotenoid or a retinoid metabolite (44), and 3) increased intra- or extracellular effects that increase cell stabilization against necrotic cell death. Such findings are not surprising given the myriad of structural and metabolic events implicated in bile acid–induced necrotic cell death, including alterations in Ca+2 homeostasis, ATP depletion, and activation of cellular proteolytic pathways (45). These data suggest that pathways involved in bile acid–induced hepatocyte apoptosis, such as activation of caspases and mitochondrial release of cytochrome c into the cytosol, may be more sensitive to cellular redox status compared with processes that are observed during necrosis.
The current finding of a potent anti-apoptotic effect of βC in a normal cell model is in contrast to studies using tumor cell models. For example, a study with human adenocarcinoma cells found that βC at concentrations up to 100 μM exhibited pro-oxidative and pro-apoptotic effects including decreased expression of the anti-apoptotic protein BCL-2 (46). βC's differential effects between freshly isolated rat hepatocytes and cultured tumor cells can be explained by a variety of experimental and biologic factors. First, tumor cells have an antioxidant defense mechanism and redox status that contrast with those of normal cells (47). In addition, the uptake and metabolism of βC can differ greatly depending on the cell type and mode of βC administration (44, 48). Other properties of βC (or other related carotenoids) that may contribute to its anti-apoptotic effects include an antiproliferative effect (49), stimulation of gap junctional communications (50), and regulation of cellular detoxification systems (51). Finally, the metabolism of βC to retinoids (48, 50) cannot be disregarded as a contributing factor to βC's observed anti-apoptotic effects. However, induction of gene transcription by retinoids through binding of nuclear receptor complexes would not likely occur in the short time frame of the current study using freshly isolated (not cultured) hepatocytes.
The protective role of βC in the current study is supportive of the hypothesis that oxidant stress is a crucial step in the pathogenesis of bile acid–induced toxicity. Many laboratories have linked generation of an oxidant stress to pro-apoptotic events in liver mitochondria and intact hepatocytes (19, 22). For example, we have demonstrated that GCDC induced the MPT in liver mitochondria and stimulated the release of cytochrome c from mitochondria into cytosol and loss of mitochondrial Δψ in hepatocytes (22, 25), all of which were blocked by antioxidants. These findings, now extended with the current results with βC, clearly implicate oxidative stress and mitochondrial dysfunction in the pathogenesis of bile acid–induced cytotoxicity. Although the evidence herein supports a role for the antioxidant effect of βC in this cytoprotection, as stated above, one cannot discount the possibility that βC also possesses nonantioxidant functions that are also operative.
In summary, the current study provides additional evidence that oxidative stress and mitochondrial dysfunction play critical roles in bile acid–induced hepatocyte toxicity, an important mediator of hepatocyte injury in the cholestatic liver (52). Moreover, the results demonstrate for the first time that βC can prevent biochemical and morphologic evidence of cell necrosis and apoptosis in rat hepatocyte suspensions that are exposed to toxic, hydrophobic bile acids. The protection afforded by this nutrient was consistent with its role as an antioxidant of biologic importance. Consideration of using βC in humans, as was recently done in a pilot study with patients with CLD (14), must take into account the possible adverse effects of the compound under certain circumstances. Questions of potential toxicity of βC have arisen during intervention studies in which βC supplementation in long-term cigarette smokers was associated with increased susceptibility to lung cancer and coronary artery disease (7, 8). Lieber's laboratory has also provided evidence in both cells and baboons suggesting that a toxic interaction may arise between βC and ethanol administration, perhaps by a mechanism involving common metabolic detoxification pathways (53, 54). Nevertheless, additional studies into the mechanisms and relevance of βC as a potential hepatoprotective agent in childhood cholestasis are warranted.
Abbreviations
- α-TH:
-
α-tocopherol
- βC:
-
β-carotene
- CLD:
-
cholestatic liver disorders
- DCF-DA:
-
dichlorofluorescin diacetate
- DCFein:
-
2′7′-dichlorofluorescein
- GCDC:
-
glycochenodeoxycholic acid
- KRH:
-
Krebs Ringers HEPES
- MPT:
-
mitochondrial permeability transition
- PI:
-
propidium iodide
- ROS:
-
reactive oxygen species
- Δψ:
-
mitochondrial electrochemical gradient
References
Frei B 1994 Natural Antioxidants in Human Health and Disease. Academic Press, San Diego
Sies H 1997 Antioxidants in Disease Mechanisms and Therapy, Vol 38, Advances in Pharmacology. Academic Press, San Diego
Gopalakrishna R, Gundimeda U 2002 Antioxidant regulation of protein kinase C in cancer prevention. J Nutr 132: 3819S–3823S.
Toivanen JL 1987 Effects of selenium, vitamin E and vitamin C on human prostacyclin and thromboxane synthesis in vitro. Prostaglandins Leukot Med 26: 265–280.
Olson JA 1999 Carotenoids. In: Shils ME, Olson JA, Shike M, Ross AC (eds) Modern Nutrition in Health and Disease, 9th Ed. Williams & Wilkins, Baltimore, 525–542.
Burton GW, Ingold KU 1984 β-Carotene: an unusual type of lipid antioxidant. Science 224: 569–573.
Alpha-Tocopherol, β-Carotene Cancer Prevention Study Group 1994 The effect of vitamin E and beta carotene on the incidence of lung cancer and other cancers in male smokers. N Engl J Med 330: 1029–1035
Kritharides L, Stocker R 2002 The use of antioxidant supplements in coronary heart disease. Atherosclerosis 164: 211–219.
Dietary reference intakes for vitamin C, vitamin E selenium, and carotenoids A Report of the Panel on Dietary Antioxidants and Related Compounds, Subcommittees on Upper Reference Levels of Nutrients and of Interpretation and Use of Dietary Reference Intakes 2000 Food and Nutrition Board, Institute of Medicine, National Academy Press Washington, DC
Leo MA, Ahmed S, Aleynik SI, Siegel JH, Kasmin F, Lieber CS 1995 Carotenoids and tocopherols in various hepatobiliary conditions. J Hepatol 23: 550–556.
Phillips JR, Angulo P, Petterson T, Lindor KD 2001 Fat-soluble vitamin levels in patients with primary biliary cirrhosis. Am J Gastroenterol 96: 2745–2750.
Floreani A, Baragiotta A, Martines D, Naccarato R, Dodorico A 2000 Plasma antioxidant levels in chronic cholestatic liver diseases. Aliment Pharmacol Ther 14: 353–358.
Sokol RJ, Devereaux MW, Gumpricht E 2001 Inhibition of bile acid-induced mitochondrial permeability transition by dietary antioxidants. Hepatology 34: 277A( abstr)
Watson JP, Jones DE, James OF, Cann PA, Branble MG 1999 Case report: oral antioxidant therapy for the treatment of primary biliary cirrhosis: a pilot study. J Gastroenterol Hepatol 14: 1034–1040.
Starzl TE, Demetros AJ, Van Thiel D 1989 Liver transplantation (1). N Engl J Med 321: 1014–1022.
Bove KE, Daugherty CC, Tyson W, Mireau G, Heubi JE, Balistreri WF, Setchell KD 2000 Bile acid synthetic defects and liver disease. Pediatr Dev Pathol 3: 1–16.
Sokol RJ, Winklhofer-Roob BM, Devereaux MW, McKim JM 1995 Generation of hydroperoxides in isolated rat hepatocytes and hepatic mitochondria exposed to hydrophobic bile acids. Gastroenterology 109: 1249–1256.
Sokol RJ, McKim JM, Goff MC, Ruyle SZ, Devereaux MW, Han D, Packer L, Everson G 1998 Vitamin E reduces oxidant injury to mitochondria and the hepatotoxicity of taurochenodeoxycholic acid in the rat. Gastroenterology 114: 164–174.
Rodrigues CM, Fan G, Ma X, Kren BT, Steer CJ 1998 A novel role for ursodeoxycholic acid in inhibiting apoptosis by modulating mitochondrial membrane perturbation. J Clin Invest 101: 2790–2799.
Patel T, Bronk SF, Gores GJ 1994 Increases of intracellular magnesium promote glycodeoxycholate-induced apoptosis in rat hepatocytes. J Clin Invest 94: 2183–2192.
Gumpricht E, Devereaux MW, Dahl RH, Sokol RJ 2000 Glutathione status of isolated rat hepatocytes affects bile acid-induced cellular necrosis but not apoptosis. Toxicol Appl Pharmacol 164: 102–111.
Sokol RJ, Straka MS, Dahl R, Devereaux MW, Yerushalmi B, Gumpricht E, Elkins N, Everson G 2001 Role of oxidant stress in the permeability transition induced in rat hepatic mitochondria by hydrophobic bile acids. Pediatr Res 49: 519–531.
Botla R, Spivey JR, Aguilar H, Bronk SF, Gores GJ 1995 Ursodeoxycholate (UDCA) inhibits the mitochondrial membrane permeability transition induced by glycochenodeoxycholate: a mechanism of UDCA cytoprotection. J Pharmacol Exp Ther 272: 930–938.
Gores GJ, Miyoshi H, Botla R, Aguilar HI, Bronk SF 1998 Induction of the mitochondrial permeability transition as a mechanism of liver injury during cholestasis: a potential role for mitochondrial proteases. Biochim Biophys Acta 1366: 167–175.
Yerushalmi B, Dahl R, Devereaux MW, Gumpricht E, Sokol RJ 2001 Bile acid-induced rat hepatocyte apoptosis is inhibited by antioxidants and blockers of the mitochondrial permeability transition. Hepatology 33: 616–626.
Crompton M 1999 The mitochondrial permeability transition pore and its role in cell death. Biochem J 341: 233–249.
Pastorino JG, Snyder JW, Serroni A, Hoek JB, Farber JL 1993 Cyclosporin and carnitine prevent the anoxic death of cultured hepatocytes by inhibiting the mitochondrial permeability transition. J Biol Chem 268: 13791–13798.
Ott M, Robertson JD, Gogvadze V, Zhivotovsky B, Orrenius S 2002 Cytochrome c release from mitochondria proceeds by a two-step process. Proc Natl Acad Sci U S A 99: 1259–1263.
Kowaltowski AJ, Castilho RF, Vercesi AE 2001 Mitochondrial permeability transition and oxidative stress. FEBS Lett 495: 12–15.
Leist M, Volbracht C, Fava E, Nicotera P 1998 1-Methyl-4-phenylpyridinium induces autocrine excitotoxicity, protease activation, and neuronal apoptosis. Mol Pharmacol 54: 789–801.
Qiao L, Studer E, Leach K, McKinstry R, Gupta S, Decker R, Kukreja R, Valerie K, Nagarkatt P, El Deiry W, Molkentin J, Schmidt-Ullrich R, Fisher PB, Grant S, Hylemon PB, Dent P 2001 Deoxycholic acid (DCA) causes ligand-independent activation of epidermal growth factor receptor (EGFR) and FAS receptor in primary hepatocytes: inhibition of EGFR/mitogen-activated protein kinase-signaling module enhances DCA-induced apoptosis. Mol Biol Cell 12: 2629–2645.
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ 1951 Protein measurement with the Folin-phenol reagent. J Biol Chem 193: 265–275.
Bradford MM 1976 A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem 72: 248–254.
Gumpricht E, Dahl RH, Yerushalmi B, Devereaux MW, Sokol RJ 2002 Nitric oxide ameliorates hydrophobic bile acid-induced apoptosis in isolated rat hepatocytes by non-mitochondrial pathways. J Biol Chem 277: 25823–25830.
Tanumihardjo SA, Furr HC, Amedee-Manesme O, Olson JA 1990 Retinyl ester (vitamin A ester) and carotenoid composition in human liver. Int J Vitam Nutr Res 60: 307–313.
Leo MA, Rosman AS, Lieber CS 1993 Differential depletion of carotenoids and tocopherol in liver disease. Hepatology 17: 977–986.
Berry MN, Edwards AM, Barritt GJ 1991 Biochemical properties. In: Burdon RH, van Knippenberg (eds) Isolated Hepatocytes: Preparation, Properties, and Applications. Elsevier Science Publishing Co., New York, 121–178.
Crabtree DV, Adler AD 1997 Is beta-carotene an antioxidant? Med H. ypotheses 48: 183–187.
Rice-Evans CA, Sampson J, Bramley PM, Holloway DE 1997 Why do we expect carotenoids to be antioxidants in vivo? Free Radic R. es 26: 381–398.
Foote CS, Denny RW 1968 Chemistry of singlet oxygen VII quenching by β-carotene. J Am Chem Soc 90: 6233–6235.
Liebler DC 1993 Antioxidant reactions of carotenoids. Ann N Y Acad Sci 691: 20–31.
Cadenas E, Wefers H, Sies H 1981 Low-level chemiluminescence of isolated hepatocytes. Eur J Biochem 119: 531–536.
Stahl W, Ale-Agha N, Polidori MC 2002 Non-antioxidant properties of carotenoids. Biol Chem 383: 553–558.
Williams AW, Boileau TW, Clinton SK, Erdman JW 2000 βeta-carotene stability and uptake by prostate cancer cells are dependent on delivery vehicle. Nutr Cancer 36: 185–190.
Spivey JR, Bronk SF, Gores GJ 1993 Glycochenodeoxycholate-induced lethal hepatocellular injury in rat hepatocytes. Role of ATP depletion and cytosolic free calcium. J Clin Invest 92: 17–24.
Palozza P, Calviello G, Serini S, Maggiano N, Lanza P, Ranelletti FO, Bartoli GM 2001 β-Carotene at high concentrations induces apoptosis by enhancing oxyradical production in human adenocarcinoma cells. Free Radic Biol Med 30: 1000–1007.
Cheeseman KH, Emery S, Maddix SP, Slater TF, Burton GW, Ingold KU 1988 Studies on lipid peroxidation in normal and tumour tissues. The Yoshida rat liver tumour. Biochem J 250: 247–252.
Wei RR, Wamer WG, Lambert LA, Kornhauser A 1998 β-Carotene uptake and effects on intracellular levels of retinol in vitro. Nutr Cancer 30: 53–58.
Carpenter K, Hardwick SJ, Albarani V, Mitchinson MJ 1999 Carotenoids inhibit DNA synthesis in human aortic smooth muscle cells. FEBS Lett 447: 17–20.
Stahl W, Sies H 2001 Effects of carotenoids and retinoids on gap junctional communication. Biofactors 15: 95–98.
Kessova IG, Leo MA, Lieber CS 2001 Effect of beta-carotene on hepatic cytochrome P-450 in ethanol-fed rats. Alcohol Clin Exp Res 25: 1368–1372.
Greim H, Czygan P, Schaffner F, Popper H 1973 Determination of bile acids in needle biopsies of human liver. Biochem Med 8: 280–286.
Ni R, Leo AM, Zhao J, Lieber CS 2001 Toxicity of beta-carotene and its exacerbation by acetaldehyde in HepG2 cells. Alcohol Alcohol 36: 281–285.
Leo MA, Kim CI, Lowe N, Lieber CS 1992 Interaction of ethanol with beta-carotene: delayed blood clearance and enhanced hepatotoxicity. Hepatology 15: 883–891.
Acknowledgements
Presented in part at the 52nd Annual Meeting of the American Association for the Study of Liver Diseases, Dallas, TX, November 2001 [Hepatology 2001;34:277A(abstr)].
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported in part by grants from the National Institutes of Health (RO1 DK-38446) and the Abby Bennett Liver Research Fund.
Rights and permissions
About this article
Cite this article
Gumpricht, E., Dahl, R., Devereaux, M. et al. β-Carotene Prevents Bile Acid-Induced Cytotoxicity in the Rat Hepatocyte: Evidence for an Antioxidant and Anti-Apoptotic Role of β-Carotene In Vitro. Pediatr Res 55, 814–821 (2004). https://doi.org/10.1203/01.PDR.0000117845.23762.6B
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.PDR.0000117845.23762.6B
This article is cited by
-
Melatonin and metformin co-loaded nanoliposomes efficiently attenuate liver damage induced by bile duct ligation in rats
Naunyn-Schmiedeberg's Archives of Pharmacology (2024)
-
Protection of human colon epithelial cells against deoxycholate by rottlerin
Apoptosis (2008)