Abstract
Inhaled nitric oxide (NO) is increasingly used in the treatment of pulmonary hypertension, despite its potential toxicity and the risk of life-threatening rebound pulmonary hypertension upon its discontinuation. We investigated whether i.v. dipyridamole, a cGMP phosphodiesterase inhibitor, increased the effects of inhaled NO and prevented rebound pulmonary hypertension. In 14 anesthetized and mechanically ventilated piglets, pulmonary hypertension was induced with U-46619, a thromboxane A2 analogue. Response to NO and rebound pulmonary hypertension were evaluated without and with i.v. dipyridamole. Low-dose dipyridamole (10 μg/kg/min) increased cardiac output and augmented the effects of inhaled NO on pulmonary vascular resistance, with marginal additive effect on mean pulmonary artery pressure. Pulmonary vascular resistance decreased from 904 to 511 (20 parts per million NO) (p < 0.0005) and 358 dyne s cm−5 (20 parts per million NO + dipyridamole) (p < 0.001 versus NO alone), and mean pulmonary artery pressure decreased from 29.0 to 20.5 (p < 0.0001) and 19.3 mm Hg (NS versus NO), respectively. Mean arterial pressure decreased from 85 to 74 mm Hg (dipyridamole + NO) (p < 0.01). High-dose dipyridamole (100 μg/kg/min) with inhaled NO reduced pulmonary vascular resistance to 334 dyne s cm−5 but also decreased mean arterial pressure to 57 mm Hg. Eight piglets developed rebound pulmonary hypertension. Two died of acute right ventricular failure and, in five, rebound pulmonary hypertension was prevented by low-dose dipyridamole. In conclusion, low-dose i.v. dipyridamole augments the effects of inhaled NO on right ventricular afterload with moderate changes in systemic hemodynamics, and can prevent rebound pulmonary hypertension.
Similar content being viewed by others
Main
NO is a potent endothelium-derived relaxing factor that exerts its vasodilating action through stimulation of soluble guanylyl cyclase and subsequent increase in cGMP in the vascular smooth muscle cell (1–3), where it is rapidly hydrolyzed by cGMP-specific phosphodiesterases (PDE 5) (4, 5). Since its introduction as a selective pulmonary vasodilator, inhaled NO (5, 6) has been used in a variety of pathologies associated with PHT, including adult respiratory distress syndrome, persistent PHT of the newborn, and in adult and neonatal cardiac surgery (7–10). Despite these beneficial effects, two major problems are a cause for concern. First, the safety of long-term inhalation of NO has not been fully elucidated. The maximal exposure limit of 25 ppm NO for 8 h a day, set by the Occupational Safety and Health Administration (11), may not be safe in patients with PHT who are receiving NO continuously for a prolonged period and who, additionally, are likely to have an abnormal pulmonary circulation. Second, severe rebound PHT on sudden withdrawal of inhaled NO has been described previously (12, 13).
Because cGMP phosphodiesterase (PDE 5) inhibitors induce pulmonary vasodilation (14–16), we investigated whether dipyridamole, a clinically available cGMP phosphodiesterase inhibitor, could enhance the effects of inhaled NO in experimentally induced PHT in piglets. This could result in lower concentrations of inhaled NO to be effective and may consequently reduce potential toxicity associated with NO inhalation. We also hypothesized that increased plasma cGMP levels, expected as a result of dipyridamole infusion, could prevent rebound PHT on withdrawal of inhaled NO.
METHODS
The experiments were performed in accordance with institutional guidelines for animal research.
Animal Selection and Surgical Procedures
Fourteen healthy piglets (age 5–6 wk; weight 10–12.5 kg) were studied under general anesthesia. None of the piglets had any sign of pulmonary or other infection.
Thirty minutes before induction of anesthesia, the piglets were premedicated with azaperone (8 mg/kg intramuscularly). General anesthesia was induced with i.v. sodium thiopental (10 mg/kg) and pancuronium (0.15 mg/kg) injected in an ear vein. The animals were intubated and mechanically ventilated (fraction of inspired oxygen 0.40 and arterial Pco2 5.3–6 kPa). Anesthesia was maintained with propofol (160–200 μg/kg/min), sufentanil (0.03 μg/kg/min), and pancuronium (7 μg/kg/min).
After surgical incision, a 20-gauge catheter (Vygon, Ecouen, France) was introduced into the right carotid artery and positioned in the aorta for blood pressure monitoring and sampling of cGMP and arterial blood gases (288 Blood Gas System, Chiron, Emeryville, CA, U.S.A.). Pulmonary artery pressures and CO were measured with a 5F thermodilution catheter (Baxter Healthcare, Deerfield, IL, U.S.A.) introduced via the right external jugular vein. The left external jugular vein was cannulated with a 5F three-lumen catheter (William Cook Europe ApS, Bjaeverskov, Denmark) for measurement of central venous pressure and administration of dipyridamole and i.v. fluids. U-46619 was administered via a 20-gauge catheter (Vygon) positioned in a femoral vein. ECG and invasive blood pressures were monitored with an HP 78304 A monitor (Hewlett Packard, Palo Alto, CA, U.S.A.). The animals were positioned on a heated water pad to maintain rectal temperature between 38.5 and 39.5°C.
Delivery of Inhaled NO
Medical-grade NO from a 1000 ppm NO cylinder (BOC, Guildford, Surrey, U.K.) was delivered before the ventilator via a nitrogen rotameter to obtain inspiratory concentrations of 2.5, 5, 10, and 20 ppm. Inhaled NO and NO2 concentrations were continuously monitored with a fast response chemiluminescence analyzer (NOX 4000, Seres, Aix-en-Provence, France) at the level of the endotracheal tube.
Drug Preparation
A stock solution of U-46619 (10 mg/mL, Pharmacia, Peapack, NJ, U.S.A.) was stored at −20°C. Immediately before the experiments, 0.5 mg of U-46619 was dissolved in 50 mL of Ringer lactate. Dipyridamole (10 mg/2 mL, Boehringer Ingelheim, Ingelheim, Germany) was diluted in 0.9% saline to a final concentration of 0.25 mg/mL (part A) and 1 mg/mL (part B) in the second protocol.
Measurement of Plasma cGMP
Plasma cGMP concentrations were determined in eight piglets using 125I RIA (Immunotech, Biocode, Liege, Belgium). For each cGMP measurement, 1 mL of blood was sampled from the arterial line and cooled in ice. Within 5 min, the samples were centrifuged during 10 min in a cooled (4°C) centrifuge (Hettich Universal 16 R, Hettich-Zentrifugen, Tuttlingen, Germany) at 2500 ×g. Plasma was separated and stored at −20°C until the assay was performed. Plasma cGMP concentrations were measured using competitive binding of sample and known amounts of 125I-labeled cGMP for a specific antibody. All samples were determined in duplicate and intra- and interassay quality were controlled by measuring a known amount of cGMP. Plasma cGMP concentrations are expressed as picomoles per milliliter plasma.
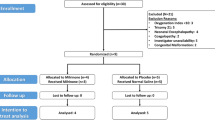
Experimental Protocol 1: Response to Inhaled NO
After 20 min of stable baseline conditions, an infusion of a potent pulmonary vasoconstrictor U-46619, a stable endoperoxide analogue of thromboxane A2 (9,11-dideoxy-9α,11α-epoxymethanoprostaglandin F2α) was titrated at a rate of 0.03–0.06 μg/kg/min to increase MPAP to 170–180% of baseline values. When MPAP was stable for 10 min, incremental doses of inhaled NO (2.5, 5, 10, and 20 ppm) were delivered over 5 min for each concentration and hemodynamic measurements were performed at each NO concentration. CO was measured as the average of two determinations after injection of 5 mL normal saline at room temperature. Thereafter, NO was discontinued and MPAP was recorded every minute over 10 min to detect rebound PHT, which was defined as an elevation of at least 20% above values obtained with U-46619. After this 10-min period, the infusion of U-46619 was discontinued for 20 min to allow the right ventricle to recover from the high afterload and to prevent right ventricular dysfunction.
Experimental Protocol 2: Response to Inhaled NO with Intravenous Dipyridamole
Twenty minutes after the end of protocol 1, MPAP was increased again with U-46619, as in protocol 1.
Part A.
Intravenous dipyridamole was infused at 10 μg/kg/min in the 12 surviving piglets and continued throughout the experiment. Hemodynamic measurements were performed at 5 and 10 min, after which protocol 1 was repeated. Again, a 10-min NO-free period was repeated to monitor rebound PHT while dipyridamole was continued.
Part B.
Fifteen minutes after NO was stopped, dipyridamole was increased to 100 μg/kg/min. Again, the response to inhaled NO was repeated. In this experiment, however, dipyridamole was not continued until the end of the experiment, but stopped together with the last dose of NO (Fig. 1).
Plasma cGMP concentrations were measured in eight piglets at baseline, during infusion of U-46619, during dipyridamole infusion (10 and 100 μg/kg/min), and 20 min after the high-dose dipyridamole (100 μg/kg/min) was stopped.
Statistical Analysis
Data are presented as means ± SD. Statistical analysis was performed with SigmaStat (SPSS Science, Chicago, IL, U.S.A) using two-way ANOVA for repeated measures for analysis within and between groups. A p value < 0.05 was considered significant.
RESULTS
Two piglets died of acute right ventricular failure resulting from extreme rebound PHT after withdrawal of inhaled NO at the end of protocol 1, and consequently did not receive a dipyridamole infusion. Data obtained from these animals were not used for statistical analysis. All 12 surviving piglets completed the entire study protocol. All data shown comprise these 12 piglets, except when mentioned otherwise. NO2 concentrations were <0.3 ppm at all times, and a 5% difference between the delivered and the aimed NO concentration was considered acceptable.
Protocol 1
Infusion of U-46619 increased MPAP from 16.6 ± 1.6 to 29.0 ± 2.6 mm Hg (p < 0.0001) and PVR from 353 ± 76 to 904 ± 183 dyne s cm−5 (p < 0.0001). MAP increased from 74 ± 14 to 90 ± 14 mm Hg (p < 0.001), SVR increased from 2671 ± 772 to 3548 ± 779 dyne s cm−5 (p < 0.001), and CO decreased from 2.1 ± 0.2 to 1.9 ± 0.2 L/min (NS).
Inhaled NO significantly decreased both MPAP and PVR at all concentrations (Table 1) without changes in systemic hemodynamic parameters. There were no significant changes in central venous pressure and pulmonary capillary wedge pressure (PcwP) during the experiment. The response to inhaled NO showed 5, 10 and 20 ppm NO to be more effective than 2.5 ppm both for MPAP and PVR, whereas only 20 ppm was significantly different from 5 ppm (Fig. 2). Rebound PHT occurred in six of the surviving twelve piglets within 2 min after NO was discontinued, with a peak after 5 min. MPAP (n = 6) increased from 29.8 ± 2.9 mm Hg to 36.8 ± 4.7 (p < 0.04) and 41.0 ± 4.8 mm Hg (p < 0.001) at 2 and 5 min, respectively (Fig. 3).
Response to inhaled NO (protocol 1 and 2A): effects on MPAP (mm Hg) and PVR (dyne s cm−5). NO in ppm. Dip 10, dipyridamole 10 μg/kg/min. Data are mean ± SD (n = 12). Control: data from protocol 1. Dip: data from protocol 2a. For MPAP: *p < 0.001 vs 2.5 NO, †p < 0.01 vs 5 NO, §p < 0.01 vs 2.5 NO + Dip 10, °p < 0.01 vs 5 NO + Dip 10, **p < 0.0001 vs baseline. For PVR: *p < 0.01 vs 2.5 NO, †p < 0.05 vs 5 NO, §p < 0.01 vs 2.5 NO + Dip 10, °p < 0.05 vs 5 NO + Dip, **p < 0.0001 vs baseline.
Protocol 2
Part A.
Restarting the infusion of U-46619 resulted in a MPAP of 29.7 ± 2.6 mm Hg and a PVR of 966 ± 246 dyne s cm−5. Ten minutes of i.v. dipyridamole (10 μg/kg/min) reduced MPAP and PVR, but also MAP and SVR with a concomitant increase in CO. Heart rate increased from 126 ± 18 to 138 ± 27 beats/min (NS) after 10 min of dipyridamole infusion. Addition of inhaled NO further decreased PVR to levels below those obtained with inhaled NO alone (at all NO concentrations) without further alterations in systemic hemodynamics, except for an additional increase in CO (Table 1).
In five of the six piglets with rebound PHT in protocol 1, dipyridamole infusion completely prevented rebound PHT (Fig. 3). In one piglet, dipyridamole failed to prevent rebound PHT. In this animal, MPAP increased from 33 to 43 mm Hg 6 min after withdrawal of NO, but decreased to 37 mm Hg 10 min after NO discontinuation.
Part B.
Dipyridamole at 100 μg/kg/min reduced both MPAP and PVR, but also induced a profound systemic vasodilation and increased CO. Furthermore, HR increased significantly from 126 ± 18 before the high-dose dipyridamole infusion to 149 ± 19 beats/min (p < 0.02). However, most of the HR increase occurred during the NO withdrawal period, irrespective of whether dipyridamole was administered or not. Filling pressures decreased slightly, but the changes were not statistically significant. Central venous pressure and PcwP decreased from 6.2 ± 3.0 to 5.6 ± 2.4 (NS) and from 7.2 ± 1.8 to 7.1 ± 2.2 mm Hg (NS). Inhalation of NO further reduced MPAP and PVR without major changes in systemic hemodynamics, except a further increase in CO (Table 2). None of the animals experienced rebound PHT, despite simultaneous cessation of i.v. dipyridamole infusion and inhalation of NO, not even 20 min after both drugs were discontinued, suggesting prolonged protection of dipyridamole against rebound PHT. In fact, MPAP remained significantly lower versus U-46619.
Plasma cGMP concentrations (n = 8) increased from baseline values of 11.7 ± 2.1 to 15.3 ± 3.5 (p < 0.006) and 16.5 ± 5.1 (p < 0.05) pmol/mL at 10 and 100 μg/kg/min dipyridamole, respectively (Fig. 4). Even 20 min after dipyridamole and NO administration were stopped, these high cGMP levels were maintained at 15.6 ± 4.9 pmol/mL (p < 0.05).
DISCUSSION
NO produced by pulmonary vascular endothelial cells is an important modulator of pulmonary vascular tone (17, 18). Because PHT may be associated with attenuated endogenous NO production (18, 19) and persistent or increased cGMP phosphodiesterase activity (16), the combination of NO with a cGMP phosphodiesterase inhibitor might reduce the effective dose of NO and limit potential toxicity related to NO inhalation (20, 21). Although the experimental PDE 5 inhibitor zaprinast (generic name) is slightly more potent than dipyridamole (4) and has already been used to enhance the effects of inhaled NO (22, 23), we preferred to study dipyridamole because it is an approved, inexpensive drug that has been clinically available for more than 30 y. If dipyridamole potentiates the effects of inhaled NO without compromising the systemic circulation, it can be useful in the setting of PHT in neonates and infants after surgery for congenital heart disease.
Our study shows that low-dose i.v. dipyridamole (10 μg/kg/min) is not a selective pulmonary vasodilator, but reduces MPAP and PVR, with a significant reduction in SVR but a clinically acceptable decrease in MAP (Table 1). Whereas inhaled NO (protocol 1) significantly vasodilates pulmonary blood vessels (MPAP −29%, PVR −43%, 20 ppm NO), dipyridamole in combination with inhaled NO (protocol 2A) further decreases PVR (−29%, for 20 ppm NO), without significant effect on MPAP (−6%) (Table 1). Whether this reflects enhanced pulmonary vasodilation or is merely the result of general vasodilation by dipyridamole is difficult to assess from our data. Although dipyridamole itself increases CO, most probably as a result of systemic vasodilation, the addition of inhaled NO to i.v. dipyridamole further increases CO, with a small decrease in MPAP and an unchanged MAP, suggesting true additional pulmonary vasodilation (Table 1). This increase in CO can probably be attributed to a decrease in right ventricular afterload with maintained coronary perfusion, resulting in improved right ventricular function.
Although in the present study 100 μg/kg/min dipyridamole (protocol 2B) decreased MPAP and reduced PVR more than any concentration of NO studied (Table 2), this dose is unacceptable in clinical practice because of the systemic hypotension it induces. Additionally, the combination of decreased coronary perfusion pressures and increased heart rate can be deleterious for right and left ventricular function as well as myocardial oxygen balance. Despite a possible residual effect of the low-dose dipyridamole, the abrupt decrease in MPAP, MAP, PVR, and SVR on initiation of 100 μg/kg/min i.v. suggests this high dose to be responsible for the potentially dangerous effects on systemic hemodynamics.
Interestingly, low-dose dipyridamole combined with 2.5 ppm NO reduces PVR more than 20 ppm NO alone, with a clinically acceptable decrease in MAP (Table 1). In clinical practice, this might allow the use of much lower doses of inhaled NO, thereby reducing the potential toxicity related to NO inhalation, such as methemoglobinemia (24), oxidation of NO to NO2(25), and NO2-related bronchospasm in humans (20). Furthermore, very little is known about the oxidant stress from the production of peroxynitrite (21) in patients with lung inflammation and in immature babies likely to have decreased antioxidant defenses (10). Although the toxicity issue of NO inhalation is not yet resolved, in the absence of in vivo studies addressing safe duration and dosage of NO inhalation, the combination of dipyridamole with low inhaled NO concentrations can be considered to reduce potential NO and NO2-related toxicity.
Our results are similar to those obtained by Ziegler et al. (26) in pediatric patients with severe PHT. The authors report a decrease in PVR and SVR with dipyridamole alone, and a further reduction by 20% in PVR in half of the patients when NO and dipyridamole are combined. In contrast to these and our data, Fullerton et al. (27) report i.v. dipyridamole in combination with inhaled NO to cause selective pulmonary vasodilation in patients immediately after mitral or aortic valve surgery. The authors also reported an increase in CO (+50%) similar to what we have found when dipyridamole and NO are combined. The longstanding left atrial and pulmonary venous hypertension and the relatively low dose of dipyridamole administered in their study may account for the selective nature of the pulmonary vasodilation.
Rebound PHT on withdrawal of inhaled NO after congenital heart surgery (12, 28, 29) and in severe respiratory failure (13) has been described previously. The dangers of rebound PHT are not only related to an abundant increase in pulmonary artery pressure, jeopardizing right ventricular function, but also to a sudden “rebound” decrease in arterial oxygen saturation (13). Because there is evidence that NO itself inhibits NO synthase activity in various tissues via a feedback mechanism (30), a possible explanation for the phenomenon of rebound PHT is inhibition of endogenous NO production in the pulmonary vascular endothelium during NO inhalation, combined with a reduced NO production after sudden withdrawal of inhaled NO (31). When endogenous pulmonary NO production cannot be restored instantly after discontinuation of NO inhalation, we speculate that drugs that prolong the half-life of NO's second messenger, cGMP, may be useful to prevent rebound PHT.
Although there is increasing evidence that dipyridamole augments the effects of inhaled NO (22, 27, 32) and may be useful in patients who cannot be weaned easily from NO inhalation (33), there is only one report that addresses the potential of dipyridamole to attenuate rebound PHT after withdrawal of inhaled NO (29). The obvious hypothesis for this phenomenon is that dipyridamole reduces the breakdown of increased cGMP levels resulting from NO inhalation in pulmonary vascular smooth muscle cells. Although increased plasma cGMP levels during zaprinast infusion and cGMP release from the lungs during combined treatment with i.v. zaprinast and inhaled NO have been described (23), to the best of our knowledge the present study is the first to address the role of increased cGMP levels during dipyridamole infusion in the setting of rebound PHT. Our data show that i.v. dipyridamole increases plasma cGMP concentrations. The long half-life of i.v. dipyridamole (between 12 and 15 h) (34) may well explain why, even 20 min after both dipyridamole and NO were discontinued, cGMP levels were significantly elevated (Fig. 4) and pulmonary artery pressures were similar to those during dipyridamole infusion (Table 2). We hypothesize that the increased plasma cGMP levels measured in our study reflect, to some extent, intrapulmonary vascular smooth muscle cGMP concentrations and, therefore, may protect against rebound PHT after sudden withdrawal of inhaled NO. Although slowly weaning the NO is usually sufficient to avoid rebound PHT in most instances, this technique may be cumbersome and low-dose dipyridamole may be a valuable alternative when weaning from NO is difficult.
Study Limitations
The increased plasma cGMP levels in our study cannot solely be attributed to the release of cGMP from pulmonary blood vessels, but other tissues such as systemic blood vessels may be involved. Another putative mechanism of vasodilation by dipyridamole includes inhibition of adenosine re-uptake (35). However, the evidence that pulmonary vasodilation by dipyridamole is not altered by adenosine receptor blockers such as theophylline but is exerted through an effect on cGMP metabolism (15, 32), and the fact that i.v. dipyridamole can prevent rebound PHT, suggest that cGMP concentrations in pulmonary vascular smooth muscle cells are increased by dipyridamole.
From our results, it is difficult to conclude whether dipyridamole induces true pulmonary vasodilation. Although it decreases MPAP, the reduction in PVR is mainly the result of an increase in CO and may indicate recruitment of pulmonary arterioles. However, the setting of a decrease in pulmonary artery pressure in combination with an important increase in pulmonary blood flow suggests at least a component of direct pulmonary vasodilation. Comparison of these data with those obtained with an inotropic agent, the use of lower doses of dipyridamole, or a more selective PDE 5 inhibitor like sildenafil (36), with probably less effect on the systemic circulation, might resolve this problem. Furthermore, our study design cannot elucidate whether the increase in CO with dipyridamole should be attributed solely to a reduction in right and left ventricular afterload, or also results from a direct inotropic and chronotropic effect on the myocardium. The fact that the increase in heart rate occurs mainly during the NO withdrawal period (both with and without dipyridamole) further complicates interpretation of these data.
CONCLUSION
Intravenous dipyridamole enhances the effects of inhaled NO on PHT. It allows lower doses of inhaled NO to be used in this setting, and may thus reduce potential toxicity related to NO inhalation. The combination of both drugs, when properly titrated, may result in adequate reductions of pulmonary artery pressure and right ventricular afterload with clinically acceptable effects on systemic hemodynamics. In clinical practice, i.v. dipyridamole is a promising drug in the setting of neonatal and pediatric cardiac surgery to prevent rebound PHT on withdrawal of inhaled NO, and may be useful in patients who cannot be weaned easily from NO inhalation.
Abbreviations
- CO:
-
cardiac output
- MAP:
-
mean arterial pressure
- MPAP:
-
mean pulmonary artery pressure
- NO:
-
nitric oxide
- NO2:
-
nitrogen dioxide
- PDE 5:
-
phosphodiesterase type 5
- PHT:
-
pulmonary hypertension
- ppm:
-
parts per million
- PVR:
-
pulmonary vascular resistance
- SVR:
-
systemic vascular resistance
References
Furchgott RF, Zawadski JV 1980 The obligatory role of endothelial cells in the relaxation of arterial smooth muscle by acetylcholine. Nature 288: 373–376
Moncada S, Higgs EA, Hodson HF, Knowles RG, Lopez-Jaramillo P, McCall T, Palmer RMJ, Radomski MW, Rees DD, Schultz R 1991 Thel-arginine: nitric oxide pathway. J Cardiovasc Pharmacol 17( suppl 3): 1–9
Arnold WP, Mittal CK, Katsuki S, Murad F 1977 Nitric oxide activates guanylate cyclase increases guanosine 3′ 5′ –cyclic monophosphate levels in various tissue preparations. Proc Natl Acad Sci U S A 74: 3203–3207
Thomas MK, Sharron HF, Corbin JD 1990 Characterization of a purified bovine lung cGMP-binding cGMP phosphodiesterase. J Biol Chem 265: 14964–14970
Pepke-Zaba J, Higenbottam TW, Dinh-Xuan AT, Stone D, Wallwork J 1991 Inhaled nitric oxide as a cause of selective pulmonary vasodilatation in pulmonary hypertension. Lancet 338: 1173–1174
Frostell C, Fratacci MD, Wain JC, Jones R, Zapol WM 1991 Inhaled nitric oxide. A selective pulmonary vasodilator reversing hypoxic pulmonary vasoconstriction. Circulation 83: 2038–2047
Rossaint R, Falke KJ, Lopez F, Slama K, Pison U, Zapol WM 1993 Inhaled nitric oxide for the adult respiratory distress syndrome. N Engl J Med 328: 399–405
Kinsella JP, Neish SR, Ivy DD, Shaffer E, Abman SH 1993 Clinical responses to prolonged treatment of persistent pulmonary hypertension of the newborn with low doses of inhaled nitric oxide. J Pediatr 123: 103–108
Wessel DL, Adatia I, Giglia TM, Thompson JE, Kulik TJ 1993 Use of inhaled nitric oxide acetylcholine in the evaluation of pulmonary hypertension endothelial function after cardiopulmonary bypass. Circulation 88: 2128–2138
Roberts JD, Lang P, Bigatello LM, Vlahakes GJ, Zapol WM 1993 Inhaled nitric oxide in congenital heart disease. Circulation 87: 447–453
1988 NIOSH recommendations for occupational safety health standards 1988. MMWR Morb Mortal Wkly Rep 37( suppl 7): 1–29
Atz AM, Adatia I, Wessel DL 1996 Rebound pulmonary hypertension after inhalation of nitric oxide. Ann Thorac Surg 62: 1759–1764
Lavoie A, Hall JB, Olson DM, Wylam ME 1996 Life-threatening effects of discontinuing inhaled nitric oxide in severe respiratory failure. Am J Respir Crit Care Med 153: 1985–1987
Braner DAV, Fineman JR, Chang R, Soifer SJ 1993 MB 22948, a cGMP phosphodiesterase inhibitor, is a pulmonary vasodilator in lambs. Am J Physiol 264: H252–H258
Ziegler JW, Ivy DD, Fox JJ, Kinsella JP, Clarke WR, Abman SH 1995 Dipyridamole, a cGMP phosphodiesterase inhibitor, causes pulmonary vasodilation in the ovine fetus. Am J Physiol 269: H473–H479
Cohen AH, Hanson K, Morris K, Fouty B, Mc Murty IF, Clarke W, Rodman DM 1996 Inhibition of cyclic 3′ - 5′ - guanosine monophosphate-specific phosphodiesterase selectively vasodilates the pulmonary circulation in chronically hypoxic rats. J Clin Invest 97: 172–179
Stamler JS, Loh E, Roddy MA, Currie KE, Creager MA 1994 Nitric oxide regulates basal systemic pulmonary vascular resistance in healthy humans. Circulation 89: 2035–2040
Celermajer DS, Dollery C, Burch M, Deanfield JE 1994 Role of endothelium in the maintenance of low pulmonary vascular tone in normal children. Circulation 89: 2041–2044
Giaid A, Saleh D 1995 Reduced expression of endothelial nitric oxide synthase in the lungs of patients with pulmonary hypertension. N Engl J Med 333: 214–221
Bauer MA, Utell MJ, Morrow PE, Speers DM, Gibb FR 1986 Inhalation of 0.30 ppm nitrogen dioxide potentiates exercise-induced bronchospasm in asthmatics. Am Rev Respir Dis 134: 1203–1208
Beckmann JS, Beckmann TW, Chen J, Marshall PA, Freeman BA 1990 Apparent hydroxyl radical production by peroxynitrite: implications for endothelial injury from nitric oxide superoxide. Proc Natl Acad Sci U S A 87: 1620–1624
Thusu KG, Morin FC, Russell JA, Steinhorn RH 1995 The cGMP phosphodiesterase inhibitor zaprinast enhances the effect of nitric oxide. Am J Respir Crit Care Med 152: 1605–1610
Ichinose F, Adrie C, Hurford WE, Zapol WM 1995 Prolonged pulmonary vasodilator action of inhaled nitric oxide by zaprinast in awake lambs. J Appl Physiol 78: 1288–1295
Wessel DL, Adatia I, Thompson JE, Hickey PR 1994 Delivery monitoring of inhaled nitric oxide in patients with pulmonary hypertension. Crit Care Med 22: 930–938
Foubert L, Fleming B, Latimer RD, Jonas M, Oduro A, Borland C, Higenbottam TW 1992 Safety guidelines for use of nitric oxide. Lancet 339: 1615–1616
Ziegler JW, Ivy DD, Wiggins JW, Kinsella JP, Clarke WR, Abman SH 1998 Effects of dipyridamole inhaled nitric oxide in pediatric patients with pulmonary hypertension. Am J Respir Crit Care Med 158: 1388–1395
Fullerton DA, Jaggers J, Piedalue F, Grover FL, McIntyre RC 1997 Effective control of refractory pulmonary hypertension after cardiac operations. J Thorac Cardiovasc Surg 113: 363–370
Miller OI, Tang SF, Keech A, Celermajer DS 1995 Rebound pulmonary hypertension on withdrawal from inhaled nitric oxide. Lancet 346: 51–52
Ivy DD, Kinsella JP, Ziegler JW, Abman SH 1998 Dipyridamole attenuates rebound pulmonary hypertension after inhaled nitric oxide withdrawal in postoperative congenital heart disease. J Thorac Cardiovasc Surg 115: 875–882
Buga GM, Giscavage JM, Rogers NE, Ignarro LJ 1993 Negative feedback regulation of endothelial cell function by nitric oxide. Circ Res 73: 808–812
Oka M, Ohnishi M, Takahashi H, Soma S, Hasunuma K, Sato K, Kira S 1996 Altered vasoreactivity in lungs isolated from rats exposed to nitric oxide gas. Am J Physiol 271: L419–L424
Ziegler JW, Ivy DD, Fox JJ, Kinsella JP, Clarke WR, Abman SH 1998 Dipyridamole potentiates pulmonary vasodilation induced by acetylcholine nitric oxide in the ovine fetus. Am J Respir Crit Care Med 157: 1104–1110
Al-Alaiyan S, Al-Omran A, Dyer D 1996 The use of phosphodiesterase inhibitor (dipyridamole) to wean from inhaled nitric oxide. Intensive Care Med 22: 1093–1095
Mosby's Complete Drug Reference 1997, 7th Ed. Mosby-Year Book, St. Louis, p II–207
Collis MG, Palmer DB, Saville VL 1985 Comparison of the potency of 8-phenyltheophylline as an antagonist at A1 and A2 adenosine receptors in atria aorta from the guinea pig. J Pharm Pharmacol 37: 278–280
Atz AM, Wessel DL 1999 Sildenafil ameliorates effects of inhaled nitric oxide withdrawal. Anesthesiology 91: 307–310
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Foubert, L., De Wolf, D., Mareels, K. et al. Intravenous Dipyridamole Enhances the Effects of Inhaled Nitric Oxide and Prevents Rebound Pulmonary Hypertension in Piglets. Pediatr Res 52, 730–736 (2002). https://doi.org/10.1203/00006450-200211000-00020
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200211000-00020