Abstract
Glutaryl-CoA dehydrogenase deficiency (also known as glutaric aciduria type I) is an autosomal, recessively inherited neurometabolic disorder with a distinct neuropathology characterized by acute encephalopathy during a vulnerable period of brain development. Neuronal damage in this disease was demonstrated to involve N-methyl-d-aspartate (NMDA) receptor-mediated neurotoxicity of the endogenously accumulating metabolite 3-hydroxyglutarate (3-OH-GA). However, it remained unclear whether NMDA receptors are directly or indirectly activated and whether 3-OH-GA disturbs the intracellular Ca2+ homeostasis. Here we report that 3-OH-GA activated recombinant NMDA receptors (e.g. NR1/NR2A) but not recombinant α-amino-3-hydroxy-5-methyl-4-isoxazole propionate receptors (e.g. GluR-A/GluR-B) in HEK293 cells. Fluorescence microscopy using fura-2 as Ca2+ indicator revealed that 3-OH-GA increased intracellular Ca2+ concentrations in the presence of extracellular Ca2+ in cultured chick neurons. Similar to glutamate-induced cell damage, 3-OH-GA neurotoxicity was modulated by extracellular Na+. The large cation N-methyl-d-glucamine, which does not permeate NMDA receptor channels, enhanced 3-OH-GA-induced Ca2+ increase and cell damage. In contrast, 3-OH-GA-induced neurotoxicity was reduced after replacement of Na+ by Li+, which permeates NMDA channels but does not affect the Na+/Ca2+ exchanger in the plasma membrane. Spectrophotometric analysis of respiratory chain complexes I–V in submitochondrial particles from bovine heart revealed only a weak inhibition of 3-OH-GA on complex V at the highest concentration tested (10 mM). In conclusion, the present study revealed that NMDA receptor activation and subsequent disturbance of Ca2+ homeostasis contribute to 3-OH-GA-induced cell damage.
Similar content being viewed by others
Main
GDD [also known as glutaric aciduria type I; MIM #23170 (1)] is an autosomal, recessively inherited neurometabolic disorder (2). So far, more than 70 disease-causing mutations have been identified in the GCDH gene (3, 4), localized on chromosome 19p13.2 (5). The mitochondrial enzyme GCDH (EC 1.3.99.7) catalyzes the reaction of glutaryl-CoA to crotonyl-CoA in the catabolic pathways of l-tryptophan, l-lysine, and l-hydroxylysine (6).
Deficiency of GCDH results in an accumulation of upstream metabolites and their derivatives, mainly glutarate, 3-OH-GA, and glutaconate (7). Most of the affected children, if untreated, develop acute encephalopathic crises, usually around age 6–12 mo (8), typically precipitated by acute intercurrent illnesses (7). These episodes usually result in irreversible neurodestruction of vulnerable brain regions, i.e. striatum and cortex (9). The structural similarity of the accumulating organic acids to glutamate led to the suggestion that excitotoxic cell damage is involved in the neuropathogenesis of GDD (10, 11).
Excitotoxicity is a pathogenetic concept that has been considered as major mechanism in many neurologic diseases (12). Although the molecular basis of glutamate toxicity is still uncertain, a Ca2+-dependent component is undisputed (13). The NMDA subtype of glutamate receptors plays a key role in mediating excitotoxic damage, owing to its high Ca2+ permeability (14). Apart from this, primary inhibition of mitochondrial respiratory chain activity has been shown to indirectly induce NMDA receptor stimulation and excitotoxic damage, and therefore has been termed “secondary” excitotoxicity (15, 16).
Recently, it was shown that 3-OH-GA-induced neuronal damage involved the NMDA subtype of ionotropic glutamate receptors in vitro(10, 11) and in vivo(17), suggesting 3-OH-GA as the main neurotoxin in GDD. Increased formation of ROS (18) and a decreased energy-buffering capacity may also contribute to this process (10). However, although previous studies have strongly suggested an involvement of excitotoxic pathways in 3-OH-GA-induced neuronal damage, it remained open whether NMDA receptors are directly or indirectly activated. Therefore, the present study focuses on the initiation of excitotoxic neuronal damage by the organic acid 3-OH-GA, investigating the effects on recombinant ionotropic glutamate receptors, intracellular Ca2+ homeostasis, and mitochondrial respiratory chain function.
METHODS
Cell transfection and electrophysiology.
Transient NMDA receptor subunit expression and electrophysiology was performed in HEK293 cells as previously described (19). In brief, a vector carrying a cloned cDNA for the green fluorescent protein was co-transfected to visualize expressing cells 48 h after transfection by standard epifluoresence optics. Cells were continuously perfused with nominally Mg2+-free external solution containing 135 mM NaCl, 5.4 mM KCl, 1.8 mM CaCl2, 10 μM glycine, and 5 mM HEPES (pH 7.25, NaOH). The pipette solution contained 140 mM CsCl, 1 mM MgCl2, 10 mM EGTA, 10 mM HEPES, and 4 mM Mg2+-ATP (pH 7.25, CsOH). After the establishment of the whole-cell configuration of the patch-clamp technique, cells were lifted from the bottom of the dish to ensure rapid and complete solution exchange when applying agonists via a piezoelectric double-barreled pipette. The solution exchange time, measured with an open patch pipette, was 100–200 μs.
Cell cultures.
Primary neuronal cultures from chick embryo telencephalons, known to be susceptible to excitotoxic cell damage, were prepared as previously described (11). Briefly, neuronal cultures were maintained in Dulbecco's modified Eagle medium supplemented with 20% fetal bovine serum and penicillin/streptomycin (all obtained from Invitrogen, Eggenstein, Germany) until they were used for the experiments after 6 d in vitro. Animal care followed the official governmental guidelines and was approved by the government ethics committee.
Treatment protocol.
Neuronal cultures were exposed to 1 mM 3-OH-GA (the kind gift of W. Buckel, Department of Microbiology, University of Marburg, Germany) or with 1 mM glutamate (Sigma Chemical, St. Louis, MO, U.S.A.) for 1 h, diluted in standardized Mg2+- and Zn2+-free HBS (sHBS), containing 140 mM NaCl, 5.4 mM KCl, 1.8 mM CaCl2 × 2 H20, 10 mM d-glucose, 10 mM HEPES, and 10 μM glycine in deionized water (all adjusted to pH 7.4) as previously described (18). The effect of Ca2+ and Na+ on 3-OH-GA-induced cell damage was investigated by varying the contents of these cations in HBS. We used Ca2+-free (CaF-HBS) and regular sHBS to differentiate between exogenous and endogenous Ca2+ sources. Extracellular Na+ was present (sHBS) or was replaced by equimolar concentrations of NMG (NMG-HBS) or Li+ (Li-HBS). The large cation NMG+ is nearly unable to permeate NMDA receptor channels, whereas Na+ and Li+ permeate and depolarize the PM. However, only Na+ enhances Ca2+ entry via the NaCaX located in the PM (20–22). This experimental design was expected to discriminate the modulatory effect of Na+ on cytosolic Ca2+ concentrations after NMDA receptor activation, involving PM depolarization and NaCaX activation. The effect of 3-OH-GA on ionotropic glutamate receptors was investigated after pretreatment for 1 h with the competitive NMDA receptor antagonist D-AP5 (50 μM; #A8054, Sigma Chemical), the noncompetitive NMDA receptor antagonist MK-801 (#M107, Sigma Chemical), or the competitive non-NMDA receptor antagonist CNQX (50 μM; #C239, Sigma Chemical).
Measurement of [Ca2+]i.
Fura-2 acetoxymethylester (5 μM in HBS; Sigma Chemical) was bath-loaded into cultured neurons for 30 min in the presence of 0.1% Pluronic F-127 (Sigma Chemical), followed by washing and another 30 min incubation in HBS at 37°C (23). The intracellular Ca2+ concentration, [Ca2+]i, was measured using an inverted microscope (Axiovert 100; Carl Zeiss GmbH, Jena, Germany), equipped with a 40× fluorescence objective (Carl Zeiss GmbH), a charge-coupled device camera, an image processor and controller (all purchased from Hamamatsu, Herrsching, Germany) as described previously (24). Fura-2 fluorescence was recorded in single neurons (n = 60–90; excitation wavelengths: 340 nm and 380 nm; emission wavelength: 510 nm). The 340/380 nm ratios were converted to [Ca2+]i as previously described (23, 24). The application of the calcium ionophore ionomycin (10 μM; Sigma Chemical) at the end of measurement confirmed that cultured neurons revealed a similar responsiveness.
Cell viability assays.
Cell viability was determined by trypan blue (0.4% in PBS) exclusion method 24 h after 3-OH-GA or glutamate exposure as previously described (11). A total number of 600–800 neurons were counted in randomly chosen subfields (n = 8) without knowledge of treatment.
Measurement of single complex activities.
Protein was determined according to Lowry et al.(25). Submitochondrial particles (SMP) were prepared from bovine heart as described (26). After preparation, SMP were dissolved in 250 mM sucrose, 50 mM KCl, 5 mM MgCl2, and 20 mM Tris/HCl (adjusted to pH 7.4). Steady-state activities of single respiratory chain complexes I–V were recorded on a computer-tunable spectrophotometer (Versamax Microplate Reader, Molecular Devices, Sunnyvale, CA, U.S.A.) operating in the dual-wavelength mode. All activities were measured at pH 7.4 according to standard protocols (26–30). Standard activities (units per milligram total protein) were calculated and were expressed as percentage of control activity (normalized to 100%). Standard respiratory chain inhibitors [2-n-decyl-quinazolin-4-yl-amine (1 μM; the kind gift of U. Brandt, Department of Biochemistry I, Molecular Bioenergetics, University of Frankfurt, Germany), thenoyltrifluoroacetone (8 mM; #T9888, Sigma Chemical), antimycin A (1 μM; #A8674, Sigma Chemical), NaCN (2 mM; #S3296, Sigma Chemical), and oligomycin (80 μM; #O4876, Sigma Chemical)] were added as positive controls.
Data analysis.
All data are expressed as mean ± SEM. Figures show representative experimental data of one of at least three independent experiments. A p value of <0.05 was considered significant. A t test (two groups) or one-way ANOVA followed by Scheffé's test (three or more groups) was used to determine the statistical significance of any difference (SPSS Version 10.0, SPSS Inc., Chicago, IL, U.S.A.).
RESULTS
3-OH-GA activates recombinant NMDA but not AMPA receptors.
Previous studies demonstrated that 3-OH-GA-induced cell damage was mediated via NMDA but not via AMPA/kainate receptors in vitro and in vivo(10, 11, 17). To find out whether 3-OH-GA activates ionotropic glutamate receptors, we expressed NMDA receptor channels of the NR1/NR2A and NR1/NR2B subtype in HEK293 cells (19) and applied the potential agonist for 200 ms at −60 mV in the constant presence of the NMDA receptor co-agonist glycine (10 μM). Glutamate (1 mM) activated currents were 818 ± 228 pA (n = 6) in NR1/NR2A and 67 ± 32 pA (n = 4) in NR1/NR2B channels. Compared with glutamate, 3-OH-GA (1 mM) activated currents were 3.5 ± 1.0% (i.e. 24 ± 6 pA;n = 6) in NR1/NR2A (Fig. 1A) and not detected (n = 4) in NR1/NR2B channels, likely due to our signal-to-noise ratio (Fig. 1A, inset). As expected for NMDA receptor-activated currents, 3-OH-GA-activated currents were blocked in the presence of the NMDA receptor antagonist D-AP5 (50 μM; not shown). In contrast to NR1/NR2A, 3-OH-GA did not activate recombinant AMPA receptors, GluR-A (not shown), or GluR-A/GluR-B (n = 2;Fig. 1B).
3-OH-GA activates recombinant NMDA but not AMPA receptors. (A) Glutamate and 3-OH-GA (both 1 mM; 200 ms) were applied to HEK293 cells expressing NR1/NR2A channels at −60 mV. Compared with glutamate, 3-OH-GA-activated whole-cell currents were 3.5 ± 1.0% (n = 6) in NR1/NR2A. (B) In contrast, 3-OH-GA (1 mM, 200 ms, −60 mV) did not activate whole-cell currents in HEK 293 expressing the recombinant AMPA receptors GluR-A/GluR-B, which could be activated by glutamate. Insets: Enlargement of 3-OH-GA-mediated current traces.
3-OH-GA induces Ca2+ influx via NMDA receptors.
Next, we investigated the effect of 3-OH-GA on intracellular Ca2+ concentrations, [Ca2+]i, by fluorescence microscopy using fura-2 as Ca2+ indicator. 3-OH-GA (1 mM) raised [Ca2+]i moderately in chick neurons (Fig. 2A), which was only observed in the presence of extracellular Ca2+ (sHBS) but not in the absence of Ca2+ (CaF-HBS). Comparability of [Ca2+]i measurements in our model system was confirmed by final application of the Ca2+ ionophore ionomycin (Fig. 2A, right panel). 3-OH-GA-induced [Ca2+]i increase was prevented by the competitive NMDA receptor antagonist D-AP5 (50 μM), but not by the competitive AMPA/kainate receptor antagonist CNQX (50 μM;Fig. 2B). Combined determination of [Ca2+]i and cell viability in single neurons after exposure to 1 mM 3-OH-GA revealed a close relationship between [Ca2+]i increase and neuronal damage (Fig. 2C). NMDA receptor blockade by 10 μM MK-801 (95 ± 3% of control viability) or 50 μM D-AP5 (97 ± 5%) prevented 3-OH-GA (1 mM) induced neuronal cell damage, in line with previous studies (11, 17).
3-OH-GA induces Ca2+ influx via NMDA receptors in chick neuronal cultures. (A) 3-OH-GA (1 mM) induced a Ca2+ increase in chick neurons in the presence (sHBS, solid triangle) but not in the absence of extracellular Ca2+ (CaF-HBS, open triangle) or in the control (open circle). Glutamate (Glu; 1 mM, open square) induced a stronger Ca2+ increase than 3-OH-GA (1 mM). Administration of the Ca2+ ionophore ionomycin (10 μM) at the end of each measurement showed a homogenous increase in [Ca2+]i with or without previous 3-OH-GA or glutamate treatment (right panel). (B) NMDA receptor blockade by D-AP5 (50 μM, solid circle) but not AMPA receptor blockade by CNQX (50 μM, open square) prevented an increase in [Ca2+]i induced by 3-OH-GA (1 mM, diluted in sHBS). (C) Combined fura-2 measurement and trypan blue exclusion after exposure to glutamate (1 mM, 1 h, diluted in sHBS), 3-OH-GA (1 mM, 1 h, diluted in sHBS), or vehicle revealed a close relationship between [Ca2+]i increase and cell viability in viable (open bars) and damaged (solid bars) neurons. [Ca2+]i was determined 10 min after application of glutamate, 3-OH-GA, or vehicle; cell viability 24 h after the incubation with glutamate, 3-OH-GA, or vehicle. *vs viable (control), t(60) = 20.059, p < 0.001; #vs viable (Glu), t(56) = 13.090, p < 0.001; †vs viable (3-OH-GA), t(43) = 8.139, p < 0.001 (t test).
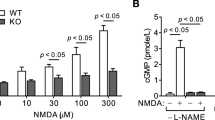
Modulation of 3-OH-GA-induced [Ca2+]i increase and cell damage by monovalent cations.
Besides being highly permeable to Ca2+(14), NMDA receptors are also permeable to Na+(31). Influx of Na+, Cl−, and water leads to neuronal death (32) but also modulates NMDA receptor-mediated Ca2+ influx in neurons by PM depolarization and by activating the reverse operation of NaCaX (21, 22). To differentiate the effects of Na+ on 3-OH-GA-mediated Ca2+ influx, we replaced Na+ (sHBS) with NMG+ (NMG-HBS) or Li+ (Li-HBS). Application of 3-OH-GA (1 mM) in NMG-HBS enhanced both [Ca2+]i increase (Fig. 3A) and neuronal damage (Fig. 3B). In contrast, incubation of 3-OH-GA in Li-HBS decreased Ca2+ influx (Fig. 3A) and neuronal damage (Fig. 3B) compared with sHBS. As expected, no Ca2+ increase or cell damage was observed in the absence of Ca2+ (Fig. 3, A and C). These results are in line with previous reports on the modulation of NMDA receptor-mediated cell damage by the monovalent ions Na+, NMG+, and Li+(20–22).
Modulation of 3-OH-GA-induced Ca2+ influx and cell damage by monovalent cations in chick neurons. (A) NMG+ enhanced 3-OH-GA (1 mM) induced [Ca2+]i in the presence (solid triangle) but not in the absence of extracellular Ca2+ (open triangle). In contrast, replacement of Na+ by Li+ (Li-HBS, solid circle) revealed a decrease in [Ca2+]i. Thus, 3-OH-GA-induced [Ca2+]i increases in the presence of Na+ were interposed between those induced in the presence of NMG+ or Li+ (see also Fig. 2A). Again, 3-OH-GA-induced Ca2+ influx was not observed in the absence of extracellular Ca2+ (open circle). (B) In parallel to the effects on [Ca2+]i, NMG+ enhanced, whereas Li+ reduced, the neurotoxic effect of 1 mM 3-OH-GA. After glutamate treatment (Glu; 1 mM, 1 h, diluted in sHBS), cell viability decreased stronger than after administration of 3-OH-GA. Statistical analysis was performed by one-way ANOVA (F6,49 = 93.713, p < 0.001) and a posteriori Scheffé's test: *3-OH-GA (Na+) vs control (Na+), p < 0.001; #3-OH-GA (NMG+) vs 3-OH-GA (Na+), p = 0.001; †3-OH-GA (Li+) vs 3-OH-GA (Na+), p = 0.021; ‡glutamate (Na+) vs 3-OH-GA (Na+), p < 0.001. (C) 3-OH-GA (1 mM) and glutamate (Glu; 1 mM) induced no significant cell damage in Ca2+-free media, confirming the importance of extracellular Ca2+ in this process. Statistical analysis was performed by one-way ANOVA (F4,35 = 4.097, p = 0.008) and a posteriori Scheffé's test: 3-OH-GA (Na+) vs control (Na+), p = 0.196; 3-OH-GA (Na+) vs 3-OH-GA (NMG+), p = 0.931; 3-OH-GA (Na+) vs glutamate (Na+), p = 0.883.
3-OH-GA does not affect respiratory chain complexes I–IV but weakly inhibits complex V.
Inhibition of the respiratory chain by mitochondrial toxins induces neuronal damage, involving indirect excitotoxic mechanisms (15, 16). However, 3-OH-GA weakly affected complex V activity only at a concentration of 10 mM in SMP (Fig. 4) but had no effect on complexes I–IV. The reliability of our system was confirmed by application of standard respiratory chain inhibitors, 2-n-decyl-quinazolin-4-yl-amine, thenoyltrifluoroacetone, antimycin A, NaCN, and oligomycin, which revealed an inhibition of 90–100%. However, an inhibitory effect of 3-OH-GA on the associated proteins of the mitochondrial respiratory chain cannot be completely excluded by this model (33).
Effect of 3-OH-GA on respiratory chain complexes I–V in submitochondrial particles from bovine heart. Steady-state activities (units per milligram protein) of single respiratory complexes I–V were recorded on a computer-tunable spectrophotometer operating in the dual-wavelength mode. Control activity was normalized to 100%. Activities of the electron-transferring complexes I (open circle), II (open square), III (open triangle, point down), or IV (open triangle, point up) were not affected by 3-OH-GA (1–10 mM), whereas a weak inhibition of complex V activity was revealed at a concentration of 10 mM (solid square). Statistical analysis was performed by one-way ANOVA (F3,32 = 13.784, p < 0.001) and a posteriori Scheffé's test: *3-OH-GA vs control;p < 0.001.
DISCUSSION
The major findings of the present study are the activation of recombinant NMDA receptors and the disturbance of the intracellular Ca2+ homeostasis by the endogenously accumulating organic acid 3-OH-GA as underlying neurotoxic mechanism in GDD.
Neurotoxicity of 3-OH-GA and a pathomechanistic involvement of NMDA receptors but not of AMPA receptors was previously demonstrated in different neuronal culture systems (10, 11) as well as after intrastriatal administration in rats (17). In this study, we demonstrated that 3-OH-GA activated NMDA but not AMPA receptors, confirming our previous hypothesis. Although a former study demonstrated a prevention of 3-OH-GA-induced neuronal damage by MK-801 in organotypic hippocampal and corticostriatal slice cultures from 6-d-old rats, these authors, however, failed to demonstrate an activation of NMDA receptors in Xenopus laevis oocytes that were injected with mRNA from neocortex of 21-d-old rats (10).
Based on cell viability data, we originally hypothesized that the NR1/NR2B receptor subtype might be of particular importance for 3-OH-GA-induced neuronal damage (11). However, here we excluded that this effect was mediated by a subtype-selective stimulation of NMDA receptors by 3-OH-GA. In fact, activation of the NR1/NR2A receptor subtype by 3-OH-GA was even more pronounced than that of NR1/NR2B. This was unexpected, inasmuch as the NR1/NR2B receptor subtype was the predominant receptor subtype in our neuronal culture system at the time point of 3-OH-GA exposure (11) as well as in immature brain (34), resulting in a high susceptibility to excitotoxic damage (35). Furthermore, because NR1/NR2B is highly expressed in neostriatal medium spiny neurons (36), which are particularly damaged during acute encephalopathy in GDD patients (37), this particular receptor subtype is still of pathophysiologic interest for GDD.
In the present study, 3-OH-GA induced an influx of Ca2+via NMDA receptors, which was dependent on the availability of extracellular Ca2+. Although Ca2+ increase after 3-OH-GA exposure was moderate, a neuronal Ca2+ load, which is one of the most important mechanisms in NMDA receptor-mediated neurotoxicity (38), seems likely to contribute to 3-OH-GA neurotoxicity. The excitotoxic mechanism could be facilitated by 3-OH-GA-induced inhibition of glutamate decarboxylase, the key enzyme in γ-aminobutyric acid formation (39). Reduced γ-aminobutyric acid levels in the CNS could indirectly enhance the excitatory influence of its physiologic counterplayer glutamate on susceptible neurons. In addition, inhibition of glutamate uptake—as demonstrated for the structurally related compound glutarate—may also contribute to 3-OH-GA-induced neuronal damage (40, 41). Although previous studies demonstrated a positive correlation between Ca2+ influx and cell death in NMDA receptor-mediated neuronal damage (38), the above-mentioned additional mechanisms may amplify the adverse effects of 3-OH-GA-induced NMDA receptor activation. On the other hand, even small NMDA receptor-mediated Ca2+ increases may be responsible for significant cell death, especially because 3-OH-GA is persistently present in affected patients. It has been demonstrated that NMDA receptor activation can initiate specific subcellular signaling under physiologic and pathophysiological conditions (42–44). Also, the precise relationships between NMDA receptor activation, cytosolic Ca2+ increase, and mitochondrial Ca2+ uptake are unknown. Therefore, cytosolic Ca2+ concentrations may not reflect the Ca2+ accumulation in mitochondria, to which Ca2+ after NMDA receptor activation shows a privileged access (45). These possibilities highlight the importance of Ca2+ influx via NMDA receptors for the induction of cell damage by 3-OH-GA.
NMDA receptors are permeable to Ca2+ but also to Na+, and increased intracellular Na+ concentrations enhance Ca2+ influx via reverse activation of the NaCaX in the PM (21). To investigate the relationship between extracellular Na+ and 3-OH-GA-induced damage, we replaced Na+ with NMG+ or Li+. Unlike Na+, neither NMG+ nor Li+ support Ca2+ transport via the NaCaX, whereas Na+ and Li+ but not NMG+ permeate NMDA receptor channels and depolarize the PM (22). In the present study, we found that replacement of Na+ by NMG+ enhanced Ca2+ increase and neuronal damage after 3-OH-GA exposure. In contrast, replacement of Na+ with Li+ reduced it. These results are in line with previous studies, revealing an enhancement of NMDA receptor-mediated Ca2+ influx and cell damage by NMG+ and a reduction by Li+(20, 22). These results underline the role of Na+ influx in excitotoxicity: 1) a limiting role, due to the depolarization-dependent decrease in the electrochemical driving force for Ca2+ (defined as the difference between the PM potential and the Ca2+ equilibrium potential); and 2) a promoting role, due to Ca2+ influx via reverse operation of NaCaX (22) and inhibition of Ca2+ extrusion by the NaCaX (20). Taken together, we suggest that Ca2+ influx is modulated by Na+ in 3-OH-GA-induced cell damage.
Inhibition of the respiratory chain can impair the ability of neurons to maintain normal resting membrane potential due to ATP depletion and can decrease the activity of Na+/K+-ATPases (46). In addition, ATPase activity can be reduced by a ROS-dependent mechanism as previously described for glutarate (47). Consequently, membrane depolarization, in general, and the removal of the voltage-dependent Mg2+ block of NMDA receptors, in particular, results in an unimpeded influx of Ca2+ and Na+ into neurons (15, 48). Furthermore, increased [Na+]i up-regulates NMDA receptor activity via an enhancement of Src kinase activity (49). However, because we found only a weak inhibition of complex V by 3-OH-GA at a high milli molar concentration (10 mM) and because 3-OH-GA did not affect intracellular ATP levels in a previous study (10), we suggest that a direct inhibition of the mitochondrial respiratory chain is only of minor importance for 3-OH-GA neurotoxicity. However, we cannot completely exclude that 3-OH-GA affects the associated proteins of the mitochondrial respiratory chain, the Krebs cycle, or the mitochondrial β-oxidation of fatty acids.
In conclusion, we confirmed that 3-OH-GA-induced cell damage is primarily mediated via NMDA receptors (11, 17, 18, 50), resulting in disturbed Ca2+ homeostasis. Because susceptibility to encephalopathic crises declines with age in GDD (7), ontogenetic factors may open a window of vulnerability for 3-OH-GA toxicity during infancy and early childhood. In particular, ontogenetic changes in the excitatory glutamatergic system should be considered (51–53). However, the neurotoxic properties of 3-OH-GA might not be sufficient to fully explain the onset of acute encephalopathy during a vulnerable period of brain development in GDD patients. Thus, the existence of additional potentiating factors has been suggested, such as catabolism and inflammatory cytokines. Catabolism, e.g. during intercurrent illness, is thought to enhance the accumulation of organic acids (37, 54) and to impair energy metabolism. Furthermore, inflammatory cytokines have been shown to potentiate 3-OH-GA neurotoxicity via induction of astrocytic iNOS (50) and are suggested to stimulate the intracerebral formation of the NMDA receptor agonist quinolinic acid, an alternative intermediate product of the tryptophan metabolism (55). Furthermore, data obtained in the present study clearly demonstrate that 3-OH-GA-induced cell damage might critically be modulated by Na+. Inasmuch as the final Ca2+ load, which determines whether neurons live or die, may be regulated by two opposite effects of Na+, i.e. PM depolarization and reverse activation of NaCaX (21, 22), and because electrolyte infusions with Na+ and Cl− are broadly implemented in current emergency treatment protocols with the intention to reduce cerebral edema (56), our results urge re-evaluation of the efficiency of this strategy in the light of neuroprotection.
Abbreviations
- 3-OH-GA:
-
3-hydroxyglutarate
- AMPA:
-
α-amino-3-hydroxy-5-methyl-4-isoxazole propionate
- CNQX:
-
6-cyano-7-nitroquinoxaline-2,3-dione disodium salt
- D-AP5:
-
(D)-(−)-2-amino-5-phosphonopentanoic acid
- GCDH:
-
glutaryl-CoA dehydrogenase
- GDD:
-
glutaryl-CoA dehydrogenase deficiency
- HBS:
-
HEPES-buffered saline
- MK-801:
-
(5R,10S)-(+)-5-methyl-10,11-dihydro-5H-dibenzo[a,d]cyclohepten-5,10-imine
- NaCaX:
-
Na+/Ca2+ exchanger of the plasma membrane
- NMDA:
-
N-methyl-d-aspartate
- NMG:
-
N-methyl-d-glucamine
- PM:
-
plasma membrane
- ROS:
-
reactive oxygen species
References
National Center for Biotechnology Information. OMIM™ Online Mendelian Inheritance in Man Web site. MIM #231670. Available at: http://www.ncbi.nlm.nih.gov/omim. Accessed May 8, 2002.
Goodman SI, Kohlhoff JG 1975 Glutaric aciduria: inherited deficiency of glutaryl CoA dehydrogenase activity. Biochem Med 13: 138–140
Goodman SI, Stein DE, Schlesinger S, Christensen E, Schwartz M, Greenberg CR, Elpeleg ON 1998 Glutaryl-CoA dehydrogenase mutations in glutaric acidemia (type I): review report of thirty novel mutations. Hum Mutat 12: 141–144
Zschocke J, Quak E, Guldberg P, Hoffmann GF 2000 Mutation analysis in glutaric aciduria type I. J Med Genet 37: 177–181
Greenberg C, Duncan AM, Gregory CA, Singal R, Goodman SI 1994 Assignment of human glutaryl-CoA dehydrogenase gene (GCDH) to the short arm of chromosome 19 (19p13.2) by in situ hybridization somatic cell hybrid analysis. Genomics 21: 289–290
Christensen E 1993 A fibroblast glutaryl-CoA dehydrogenase assay using detritiation of 3H-labelled glutaryl-CoA: application in the genotyping of the glutaryl-CoA dehydrogenase locus. Clin Chim Acta 220: 71–80
Hoffmann GF, Athanassopoulos S, Burlina AB, Duran M, deKlerck JBC, Lehnert W, Leonard JV, Monavari AA, Müller E, Muntau AC, Naughten ER, Plecko-Starting B, Superti-Furga A, Zschocke J, Christensen E 1996 Clinical course, early diagnosis, treatment, prevention of disease in glutaryl-CoA dehydrogenase deficiency. Neuropediatrics 27: 115–123
Bjugstad KB, Goodman SI, Freed CR 2000 Age at symptom onset predicts severity of motor impairment clinical outcome of glutaric acidemia type 1. J Pediatr 137: 681–686
Brismar J, Ozand PT 1995 CT MR of the brain in glutaric aciduria type I: a review of 59 published cases a report of 5 new patients. Am J Neuroradiol 16: 675–683
Ullrich K, Flott-Rahmel B, Schluff P, Musshoff U, Das A, Lücke T, Steinfeld R, Christensen E, Jakobs C, Ludolph A, Neu A, Roper R 1999 Glutaric aciduria type I: pathomechanisms of neurodegeneration. J Inherit Metab Dis 22: 392–403
Kölker S, Ahlemeyer B, Krieglstein J, Hoffmann GF 2000 Maturation-dependent neurotoxicity of 3-hydroxyglutaric glutaric acids in vitro: a new pathophysiologic approach to glutaryl-CoA dehydrogenase deficiency. Pediatr Res 47: 495–503
Lipton SA, Rosenberg PA 1994 Excitatory amino acids as final common pathway for neurologic disorders. N Engl J Med 330: 613–622
Sattler R, Tymianski M 2000 Molecular mechanisms of calcium-dependent excitotoxicity. J Mol Med 78: 3–13
MacDermott AB, Mayer ML, Westbrook GL, Smith SL, Barker JL 1986 NMDA-receptor activation increases cytoplasmic calcium concentration in cultured spinal cord neurons. Nature 321: 519–522
Albin RL, Greenamyre JT 1992 Alternative excitotoxic hypothesis. Neurology 42: 733–738
Beal MF 1992 Does impairment of energy metabolism result in excitotoxic neuronal death in neurodegenerative illnesses?. Ann Neurol 31: 119–130
De Mello CF, Kölker S, Ahlemeyer B, de Souza FR, Fighera MR, Mayatepek E, Krieglstein J, Hoffmann GF, Wajner M 2001 Intrastriatal administration of 3-hydroxyglutaric acid induces convulsions excitotoxic lesions in rats. Brain Res 916: 70–75
Kölker S, Ahlemeyer B, Krieglstein J, Hoffmann GF 2001 Contribution of reactive oxygen species to 3-hydroxyglutarate neurotoxicity in primary neuronal cultures from chick embryo telencephalons. Pediatr Res 50: 76–82
Köhr G, Eckardt S, Lüddens H, Monyer H, Seeburg PH 1994 NMDA receptor channels: subunit-specific potentiation by reducing agents. Neuron 12: 1031–1041
Mattson MP, Guthrie PB, Kater SB 1989 A role for Na+-dependent Ca2+extrusion in protection against neuronal excitotoxcitiy. FASEB J 3: 2519–2526
Hoyt KR, Arden SR, Aizenman E, Reynolds IJ 1998 Reverse Na+/Ca2+ exchange contributes to glutamate-induced intracellular Ca2+ concentration increases in cultured rat forebrain neurons. Mol Pharmacol 53: 742–749
Kiedrowski L 1999 N-methyl- d -aspartate excitotoxicity: relationship among plasma membrane potential, Na+/Ca2+ exchange, mitochondrial Ca2+ overload, and cytoplasmic concentrations of Ca2+, H+, and K+. Mol Pharmacol 56: 619–632
Grynkiewicz G, Poenie M, Tsien RY 1985 A new generation of Ca2+ indicators with greatly improved fluorescence properties. J Biol Chem 260: 3440–3450
Kölker S, Okun JG, Hörster F, Assmann B, Ahlemeyer B, Kohlmüller D, Exner-Camps S, Mayatepek E, Krieglstein J, Hoffmann GF 2001 3-Ureidopropionate contributes to the neuropathology of 3-ureidopropionase deficiency severe propionic aciduria: a hypothesis. J Neurosci Res 66: 666–673
Lowry OH, Roseborough NR, Farr AL, Randall RJ 1951 Protein measurement with the folin phenol reagent. J Biol Chem 193: 265–275
Okun JG, Lümmen P, Brandt U 1999 Three classes of inhibitors share a common binding domain in mitochondrial complex I (NADH:ubiquinone oxidoreductase). J Biol Chem 27: 2625–2630
Ziegler D, Rieske JS 1967 Preparation properties of succinate dehydrogenase coenzyme Q reductase (complex II). Methods Enzymol 10: 231–235
Percy JM, Pryde JG, Apps DK 1985 Isolation of ATPase I, the proton pump of chromatin-granule membranes. Biochem J 231: 557–564
Sinjorgo KMC, Durak I, Dekker HL, Edel CM, Hakvoort TBM, van Gelder BF, Muijsers AO 1987 Bovine cytochrome c oxidases, purified from heart, skeletal muscle, liver kidney, differ in the small subunits but show the same reaction kinetics with cytochrome c. Biochim Biophys Acta 893: 251–258
Brandt U, Okun JG 1997 Role of deprotonation events in ubihydroquinone: cytochrome c oxidoreductase from bovine heart yeast mitochondria. Biochemistry 36: 11234–11240
Mayer ML, Westbrook GL 1987 The physiology of excitatory amino acids in the vertebrate central nervous system. Prog Neurobiol 28: 197–276
Choi DW 1987 Ionic dependence of glutamate neurotoxicity. J Neurosci 7: 369–379
Trijbels FJ, Ruitenbeek W, Huizing M, Wendel U, Smeitinik JAM, Sengers RC 1997 Defects in the mitochondrial energy metabolism outside the respiratory chain the pyruvate dehydrogenase. Mol Cell Biochem 174: 243–247
Monyer H, Burnashev N, Laurie DJ, Sakmann B, Seeburg PH 1994 Developmental regional expression in the rat brain functional properties of four NMDA receptors. Neuron 12: 529–540
McDonald JW, Silverstein FS, Johnston MV 1988 Neurotoxicity of N-methyl-d-aspartate is markedly enhanced in developing rat central nervous system. Brain Res 459: 200–203
Landwehrmeyer GB, Standaert DG, Testa CM, Penney JB, Young AB 1995 NMDA receptor subunit mRNA expression by projection neurons interneurons in rat striatum. Neuroscience 15: 5297–5307
Goodman SI, Norenberg MD, Shikes RH, Breslich DJ, Moe PG 1977 Glutaric aciduria: biochemical morphological considerations. J Pediatr 90: 746–750
Hartley DM, Kurth MC, Bjerkness L, Weiss JH, Choi DW 1993 Glutamate receptor-induced Ca2+ accumulation in cortical cell culture correlates with subsequent neuronal degeneration. J Neurosci 13: 1993–2000
Stokke O, Goodman SI, Moe PG 1976 Inhibition of brain glutamate decarboxylase by glutarate, glutaconate, beta-hydroxyglutarate: explanation of the symptoms in glutaric aciduria type I?. Clin Chim Acta 66: 411–415
Bennett JP, Logan WJ, Snyder SH 1973 Amino acids as central nervous system transmitters: the influence of ions, amino acid analogues, ontogeny on transport systems forl-glutamicl-aspartic acids glycine into central nervous synaptosomes of the rat. J Neurochem 21: 1533–1550
Porciúncula LO, Dal-Pizzol A, Tavares RG, Coitinho AS, Emanuelli T, Souza DO, Wajner M 2000 Inhibition of synaptosomal [3H] glutamate uptake [3H] glutamate binding to plasma membranes from brain of young rats by glutaric acid in vitro. J Neurol Sci 173: 93–96
Tymianski M, Charlton MP, Carlen PL, Tator CH 1993 Source specificity of early calcium neurotoxicity in cultured embryonic spinal neurons. J Neurosci 13: 2085–2104
Sattler R, Charlton MP, Hafner M, Tymianski M 1998 Distinct influx pathways, not calcium load, determine neuronal vulnerability to calcium neurotoxicity. J Neurochem 71: 2349–2364
Hardingham GE, Arnold FJL, Bading H 2001 A calcium microdomain near NMDA receptors: on switch for ERK-dependent synapse-to-nucleus communication. Nat Neurosci 4: 565–566
Peng TI, Greenamyre T 1998 Privileged access to mitochondria of calcium influx through N-methyl-d-aspartate receptors. Mol Pharmacol 53: 974–980
Erecinska M, Dagani F 1990 Relationship between the neuronal sodium/potassium pump energy metabolism. Effects of K+, Na+, adenosine triphosphate in isolated brain synaptosomes. J Gen Physiol 95: 591–616
Kölker S, Okun JG, Ahlemeyer B, Wyse ATS, Hörster F, Wajner M, Kohlmüller D, Mayatepek E, Krieglstein J, Hoffmann GF 2002 Chronic treatment with glutaric acid induces partial tolerance to excitotoxicity in neuronal cultures from chick embryo telencephalons. J Neurosci Res 68: 424–431
Nowak L, Bregestovski P, Ascher P, Herbet A, Prochiantz A 1984 Magnesium gates glutamate-activated channels in mouse cerebral neurones. Nature 307: 462–465
Yu XM, Salter MW 1998 Gain control of NMDA-receptor currents by intracellular sodium. Nature 396: 469–474
Kölker S, Ahlemeyer B, Hühne R, Mayatepek E, Krieglstein J, Hoffmann GF 2001 Potentiation of 3-hydroxyglutarate neurotoxicity following induction of astrocytic iNOS in neonatal rat hippocampal cultures. Eur J Neurosci 13: 2115–2122
Wisden W, Seeburg PH, Monyer H 2000 AMPA, kainate and NMDA ionotropic glutamate receptor expression—an in situ hybridization atlas. In: Ottersen OP, Storm-Mathisen J (eds) Handbook of Chemical Neuroscience, Vol 18. Elsevier, New York, 99–143
Gegelashvili G, Schousboe A 1997 High affinity glutamate transporters: regulation of expression activity. Mol Pharmacol 52: 6–15
Christensen J, Sorensen JC, Ostergaard K, Zimmer J 2000 Early postnatal development of the rat corticostriatal pathway: an anterograde axonal tracing study using biocytin pellets. Anat Embryol (Berl) 200: 73–80
Land JM, Goulder P, Johnson A, Hockaday J 1992 Glutaric aciduria type I: an atypical presentation together with some observations upon treatment the possible cause of cerebral damage. Neuropediatrics 23: 322–326
Heyes MP 1987 Hypothesis: a role for quinolinic acid in the neuropathology of glutaric aciduria type I. Can J Neurol Sci 14: 441–443
Baric I, Zschocke J, Christensen E, Duran M, Goodman SI, Leonard JV, Müller E, Morton DH, Superti-Furga A, Hoffmann GF 1998 Diagnosis management of glutaric aciduria type I. J Inherit Metab Dis 21: 326–340
Acknowledgements
The authors thank P.H. Seeburg (Department of Molecular Neurobiology, Max Planck Institute for Medical Research, Heidelberg, Germany), H. Monyer (Department of Clinical Neurobiology, University of Heidelberg, Germany), and C.-M. Becker (Department of Biochemistry and Molecular Medicine, University of Erlangen, Germany) for fruitful discussions. We also thank S. Engel, S. Grünewald, and S. Exner-Camps for excellent technical support.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by a grant from the Deutsche Forschungsgemeinschaft to S.K. (KO 2010/1-1) and by a junior grant from the University of Heidelberg to F.H. (Nr. 12/2001).S.K. and G.K. contributed equally to the study.
Rights and permissions
About this article
Cite this article
Kölker, S., Köhr, G., Ahlemeyer, B. et al. Ca2+ and Na+ Dependence of 3-Hydroxyglutarate-Induced Excitotoxicity in Primary Neuronal Cultures from Chick Embryo Telencephalons. Pediatr Res 52, 199–206 (2002). https://doi.org/10.1203/00006450-200208000-00011
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200208000-00011
This article is cited by
-
The biochemical subtype is a predictor for cognitive function in glutaric aciduria type 1: a national prospective follow-up study
Scientific Reports (2021)
-
Toxic Synergism Between Quinolinic Acid and Glutaric Acid in Neuronal Cells Is Mediated by Oxidative Stress: Insights to a New Toxic Model
Molecular Neurobiology (2018)
-
Oxidative Stress, Disrupted Energy Metabolism, and Altered Signaling Pathways in Glutaryl-CoA Dehydrogenase Knockout Mice: Potential Implications of Quinolinic Acid Toxicity in the Neuropathology of Glutaric Acidemia Type I
Molecular Neurobiology (2016)
-
A cross-sectional controlled developmental study of neuropsychological functions in patients with glutaric aciduria type I
Orphanet Journal of Rare Diseases (2015)
-
The phenotypic spectrum of organic acidurias and urea cycle disorders. Part 1: the initial presentation
Journal of Inherited Metabolic Disease (2015)