Abstract
From 1985 through 1995, 348 infants aged 3 wk–3 mo were referred to the Stanford Sleep Clinic for “apparent life-threatening events” (ALTE). A small group of 48 infants with no history of sleep-disordered breathing (SDB) was also recruited and used as controls (they comprised group C). We conducted a systematic investigation of relatives (parents, siblings, and grandparents) of the infants, including a clinical evaluation, craniofacial investigation, and the completion of an extensive (189-question) validated sleep/wake questionnaire. All data were calculated before the subdivision of ALTE infants into two groups. The subdivision was based on a blind scoring of the infants' polygraphic recordings; 42.5% of the infants were negative for SDB (Group A), whereas 57.5% of the infants were positive for SDB (Group B). Groups A and C were not significantly different from each other. Forty-three percent of the relatives of Group B infants had been treated for SDB (with nasal CPAP, surgical or dental appliance treatments) compared with 7.1% of Group A relatives. Clinical investigation indicated a significantly higher presence of small upper airways in the families of infants with SDB. About twice as many relatives reported the presence of asthma in Group B compared with Group A. Naso-oro-maxillomandibular anatomic traits that may lead to small upper airways in parents may be risk factors for abnormal breathing during sleep in their infants.
Similar content being viewed by others
Main
Between 1974 and 1980, researchers at the Stanford University Sleep Disorders Center and other clinics performed research on infants who experienced near-miss SIDS. In later years, the name of this phenomenon was changed to ALTE because many of these infants were found to have a medical diagnosis that explained the “event” that had brought them to clinical attention. Using nocturnal polygraphic investigation, various studies have demonstrated that some ALTE infants experience abnormal breathing during sleep (1–4).
In 1979, Strohl et al.(5) reported on a SIDS victim who came from a family in which several members experienced obstructive sleep apneas. Between 1980 and 1985, we examined the upper airway anatomy of some ALTE children and parents in families in which a SIDS victim had been identified, (6) and who had demonstrated a familial tendency to have small upper airways. We therefore added a family study component to the clinical protocol performed on infants referred to the clinic for ALTE. The data obtained on the ALTE infants are presented in a separate article (7); the results of that data only will be summarized here as the findings obtained on these infants are the basis for the subdivision into two groups. In this report, we present the results of our examination of family members of the ALTE infants. In addition, we have included the family information of the infants who were recruited to serve as “normal controls” for various research protocols that investigated the development of sleep/wake patterns, circadian rhythms, and breathing patterns during sleep. These data on normal controls are included for informational purposes only. These infants were recruited with the specific caveat that there be no history of ALTE or sleep-related breathing disorders in their families; thus they are termed “hypernormal.” However, they can be a useful contrast to the findings presented and are designated as the “normal population.”
We questioned whether there was a higher frequency of SDB in families of ALTE infants identified as having abnormal breathing during sleep. We also questioned whether there were more anatomical problems with an impact on upper airway size in the family members of ALTE infants with SDB compared with the parents of the other infants.
METHODS
Patient Population: Short Review of the Index Cases (Infants)
Recruitment of infant population.
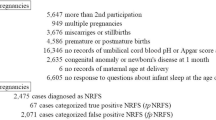
An administrative review (7) indicated that 411 infants younger than 10 mo of age were referred to the center because of an ALTE. These infants were initially seen by a community pediatrician who referred them to an emergency room or a pediatric department. The infants were subsequently referred to our clinic. There was no known cause for the ALTE in the infants referred to us; thus, these are cases of idiopathic ALTE (Table 1).
Our core clinical protocol, which was approved by the institutional review board and formed part of the general clinical workup after a 1-y trial, was not completed in 39 of these 411 infants. Further information was incomplete or data were unavailable for an additional 24 infants. Data were thus available for 348 referred infants (85% of the total referred population). These 348 referred infants (162 females), from whom we obtained complete information, are considered the index population (100%).
During the same time period, 68 normal controls were recruited from the same community as the infants who were referred. Criteria for inclusion as a control were the following:1) a full-term pregnancy with normal delivery;2) normal neurobehavioral and pediatric development;3) absence of family history of SDB, ALTE, or SIDS; and 4) signature on an informed consent form. Normal controls underwent the same evaluation, polygraphic recordings, and family investigation as the ALTE children. Of the 68 infants recruited as controls, 48 infants (25 females) had appropriate data (70.6% of the potential population). They represent the “control” population.
Data collected on infants.
In addition to a pediatric and neurologic workup, the infants had a structured sleep medicine evaluation. This sleep evaluation included the following elements:1) clinical interviews with caregivers concerning child behavior while awake and sleep/wake activity over time;2) reconstruction of the sleep/wake behavior during the previous 3 d; and 3) completion of a questionnaire investigating breathing and movements during sleep, as well as behavior while awake. Our questionnaire included many segments of the Brouillette et al. questionnaire (8).
The questionnaire included questions concerning noisy breathing during sleep, snoring, sweating during sleep, quiet or restless sleep, movements during sleep, growth and development, development of sleep/wake patterns, daytime naps, nighttime duration and fragmentation of sleep, upper-airway and ear infections, and signs of allergies. Parents were asked to indicate whether the problems were present daily, at least once every 15 d, at least once a month, or of an unknown frequency. The questions concerning sleep/wake patterns were associated with reconstruction of a “sleep log” of the three days just before referral.
The physical examination included a mandatory evaluation of the face and the oropharynx. Although this assessment was based on subjective scales, the same individual always performed it and the evaluation was always performed before the results of the sleep recording were known. The evaluation was always performed before polygraphic recordings were begun and included the following:
-
1. Face shape, with three classifications: long, round, or intermediate.
-
2. Chin: small, triangular and narrow, wide, or intermediate.
-
3. Position of the chin when the infant is supine: clearly visible retroposition of chin, mild retroposition, or no retroposition.
-
4. Hard palate: high and narrow, intermediate, or low placement.
-
5. Tonsils on a four-point scale: 1 = very small tonsils and 4 = “kissing” tonsils.
-
6. Uvula: long uvula located behind the base of the tongue, short uvula located high, and intermediate position of uvula tip located above the base of the tongue.
-
7. The presence or absence of temporomandibular joint laxity and nasal flaring at inspiration were determined at the end of the examination, with the infant supine. The mouth was closed and the chin was held gently while mild backward pressure was applied.
-
8. Size of the oropharynx: small, medium, or wide open.
Polygraphic recording.
All children had at least 12 h of nocturnal polygraphic recording and were simultaneously videotaped. Recordings included EEG (C3/A2, C4/A1, and O1/A1), right and left electrooculogram, chin EMG, oronasal airflow, thoracic and abdominal efforts, intercostal (diaphragmatic) EMG with laterally placed electrodes between scapular and maxillary lines, measurement of oxygen saturation, breathing sounds monitored with a microphone placed on the front of the neck, measurement of respiratory efforts with an esophageal catheter connected to a pressure transducer, and an ECG (modified V2 lead). CO2 monitoring was the only test in which variability of measurements occurred due to equipment changes. End-tidal CO2 and transcutaneous CO2 were monitored in 352 infants (they were not monitored in all children). This was due to:1) technical problems related to the end-tidal CO2 cannula (because of the prior demonstration of better abnormal breathing-pattern identification with Pes recording (9)), 2) the absence of any suspicion of hypoventilation from clinical history, and SaO2 monitoring in the hospital one or two nights before the recording. Follow-up studies were performed at regular intervals during the first 10 mo of life with reinvestigation of clinical symptoms, clinical signs, craniofacial clinical scales, and PSG.
Records and clinical information, collected systematically, were not analyzed until an appropriate computer program could be established. Then a coinvestigator, who had never been involved in the data collection, entered the clinical information and the results of the clinical scales into the database. Another coinvestigator, who also had never been involved in patient care or data collection, rescored all polygraphic recordings.
The concept of “abnormal upper airway resistance” is recent, and the abnormal respiratory efforts indicated by Pes monitoring were not initially scored by the technical staff. It was also believed that, in view of interscorer variability, the use of only one scorer for all polygraphic recordings would maintain consistency for all polygraphic recordings. The classification of an infant as a subject “with obstructive breathing during sleep” or “without sleep breathing abnormalities” was determined by this individual, blind to clinical information and prior sleep scoring.
All records were hand scored for sleep and wakefulness using the international atlases (10, 11). The criteria for “abnormal breathing” were based on breathing patterns, oxygen saturation, and arousal responses during sleep (9, 12, 13). Apnea was defined as the absence of airflow as determined by thermistor for more than two respiratory cycles (14). Hypopnea was defined as a reduction of airflow, again as defined by thermistors, by at least 50% compared with normal segments, and was associated with an arousal at the end of the event. This association was based on the analysis of respiratory efforts (with thoracic and abdominal bands, and Pes patterns) and airflow (with thermistors). Apneas and hypopneas were subdivided into central, mixed, and obstructive. The published criteria were used to score the presence of the pathology (3, 13).
The term “obstructive breathing” was applied to infants when the above criteria for apnea or hypopnea were not reached. Infants defined as having obstructive breathing all had at least one obstructive apnea in their recording and also had further indications of abnormal breathing efforts during sleep, as assessed from the analysis of the Pes curve. “Increased respiratory effort” was considered when peak-end inspiratory Pes was more than an estimated 2 SD from prior breathing for at least three successive breaths (9). It was considered abnormal if it was associated with an arousal and if an abrupt change in Pes pattern, called “Pes reversal,” was seen after the arousal. Pes reversal (9, 12) was defined as an abrupt decrease of inspiratory effort indicated by the Pes curve when the arousal occurred. A final pattern, called “crescendos,” was also defined (Fig. 1). This pattern was scored when a greater inspiratory effort with each successive breath was indicated by a more negative peak-end inspiratory Pes (9, 12). It was considered abnormal if it led to an arousal (usually associated with a Pes reversal). An “arousal” was defined according to the age of the infant.
The presence of a crescendo pattern during polygraphic recording. Pes is monitored on channel 10 from the top. Note the progressively more negative peak-end inspiratory pressure with each breath and the arousal response at the end of the breathing pattern. The arousal is associated with a brief movement indicated by movement artifact in the EEG-EMG channels. There is no indication of breathing changes in the airflow channel (naso-buccal thermocouples, i.e. three probes on one channel).
There must also have been a burst of EMG associated with the increase in heart rate, lasting at least 2 s in infants younger than 3 mo of age. In older infants the presence of a recognizable burst of fast theta or alpha, an increase in heart rate, or a burst of EMG activity seen with the change in breathing was scored as an arousal. Recordings were considered to be pathologic if there was one or more obstructive event per hour of sleep, including the above-defined obstructive breathing events (9, 13) associated with the change in breathing pattern.
In summary, the polygraphic classification of the ALTE infants was obtained in a blinded fashion; the new scorer was unaware of clinical history, clinical data, and family history.
Analyses.
The analysis performed on infants involved variables obtained from polygraphic recordings and those derived from clinical evaluations. All data from the questionnaire were analyzed on a five-point scale and the results of the craniofacial anatomy examination, in which a three-point scale was usually used, were placed in a database. The presence or absence of specific medical history was also entered, as was drug intake history.
Demographic, clinical, and polygraphic findings obtained on index cases.
The index group included 348 infants (162 females). Seven infants were born before 40 wk of gestational age (36–38 wk). The mean birth weight was 3101 ± 208 g. The mean postnatal age at the time of referral was 4.1 ± 1.7 wk. The initial polygraphic recording was performed a mean of 3.2 ± 1.1 d after the initial referral to the university hospital. The demographic profile of the subgroups is presented in Table 1.
The analysis of ECG data (modified V2 lead) indicated that there were no important heart rate changes that were not associated with an abnormal respiratory event. Based on nocturnal polygraphic recordings, the infants were subdivided into two subgroups. Group A was judged to have normal breathing during sleep, whereas Group B was judged to have an abnormal breathing pattern. Group A was called the “normal breathing group.” Group B was called the “obstructive breathing group.” The control subjects comprised Group C (“controls”).
Results of PSG by group are presented in Table 2. Group B (abnormal breathing) consisted of 103 infants with sleep apnea and hypopnea and an additional 97 infants who were classified with SDB based on the evaluation of Pes, crescendos, and arousals. No significant differences were found between these two subgroups when clinical symptoms or scores on anatomical scales were considered. For the purposes of our study, they were therefore treated as a single group (group B).
Results of the subjective scores given at facial evaluation are presented in Table 3.
Patient Population: Families of Index Cases.
The familial investigation was limited to parents, grandparents, and siblings.
Family members were asked to sign consent forms. They were also told that we hoped to learn more about what was behind the ALTE by performing family studies.
The following components were included in the core investigation of family members:1) responses to a validated questionnaire (the Sleep Disorders Questionnaire) (15);2) clinical evaluation including a general physical and examination of past medical history, general medical condition, and medication intake history; and 3) craniofacial evaluation including a description of the face, measurement of neck circumference and overjet, and evaluation of the hard and soft palate, mandible, tonsils, turbinate, and nasal septum. The same classifications as those outlined for infants were used. (The evaluation of “craniofacial features” in adults led to measurements calculated with calipers (16). Calipers were not used during the first years of the study.) The technique used to perform the evaluation of maxilla, mandible, and height of hard palate in adults has been reported and normal cutoff points indicated in a previous report (16).
Questionnaires and clinical evaluations were usually obtained from parents and siblings during the recording, or very shortly thereafter, but always before the results of the infant recording had been tabulated. Evaluations that were performed later (mostly on grandparents) were conducted by a person who did not know the results of the tests. The presence of associated medical problems was assessed by responses to the SDQ, clinical evaluation, and review of medication intake. The presence of asthma, for example, was determined by the report of a diagnosis made previously by the personal physician, and the review of symptoms and drug intake.
We asked questions about some of the symptoms and signs based on prior studies performed on children and adults with SDB. For example, the history of extraction of several or all four wisdom teeth, particularly if performed during the teenage or early adult years, is an indication of small jaws wherein wisdom teeth cannot grow normally, become impacted, and have to be removed.
Repeated earaches and upper-airway infections during early childhood are commonly seen with abnormal nasal resistance in early childhood. Repeated allergies and upper airway infections during early childhood leads to abnormal nasal resistance that affects the growth of the maxillomandibular complex. Night terrors and sleepwalking may be related to the sleep fragmentation associated with SDB; removal of the anatomic causes of the breathing disorder during sleep, such as enlarged tonsils and/or adenoids, may stop the nocturnal symptoms.
All family members were asked to undergo the full protocol. If clinical evaluation was impossible, they were asked to at least provide questionnaire data (15). The latter type of response was due, primarily, to the issue of geographic distance from the sleep center. Data were obtained during the first 12 mo of follow-up. The number of individuals participating in the study was dependent on distance and ease of contact.
Statistical Analysis
Descriptive statistics were used. Investigation of the presence or absence of normal distribution mandated the usage of parametric/nonparametric statistics. Discontinuous variables were treated with χ2 statistics. Analysis of variance was also used for comparisons of the groups, and odds ratios were calculated. Group A included the relatives of infants who had no SDB; Group B included those who had SDB.
RESULTS
Relatives of Referred and Control Infants: Potential Population
The 348 infants who were referred to the clinic had a total of 691 parents, 1188 grandparents, and 228 siblings who were alive and could be identified. This information was gathered from administrative forms and parent reports. Five fathers were listed as “unknown.”
The 48 control infants had 96 parents, 179 grandparents, and 58 siblings who were alive and could be identified (100%). The total potential population was 2107 individuals (100%) for referred infants, and 333 individuals for the control infants.
Relatives of Referred and Control Infants: Population Studied.
The population actually studied (and not the full number of potential participants) will be considered as representing 100% of the population.
Families of referred infants.
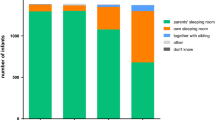
In the case of the infants referred to the clinic, 668 parents (96.7%), 843 grandparents (71%), and 221 siblings (97.8%) were clinically evaluated. An additional 167 grandparents mailed back questionnaires (for a total of 1010 questionnaire responses or 85% of the potential grandparent population). All siblings of the referred infants were examined, as were all the mothers.
A total of 28 fathers were “unexamined.” Five fathers were not examined because they were unknown. In addition to the unknown fathers, 23 other fathers were not examined and had no corresponding questionnaires, including one black, 21 white, and one Hispanic father. Thirteen of these fathers were from group A (4.6% of the “potential” parents of Group A subjects), and 10 were from group B (2.6% of the “potential” parents of Group B subjects).
Black families participated less in the family evaluation. All black mothers and siblings participated, but there were large numbers of grandparents who did not complete questionnaires. Of the 139 living black grandparents, 69.8% were examined and 77.7% responded to the questionnaire. By comparison, in group B whites (all black children were in group B) 80% of grandparents were examined and 95.4% sent back completed questionnaires. Overall, as stated above, 85% of living grandparents responded to the questionnaire.
Families of “control” infants.
For normal controls, 96 parents (100%), 50 siblings (96%), and 118 grandparents (66%) were examined and responded to questionnaires. An extra 48 questionnaires were mailed back for a total of 166 questionnaire responses (93%) from grandparents. The ethnic composition of the control parent group was 91 whites, one black, and four Far-East Asians.
Relatives of Referred and Control Infants: Variables Studied
Symptoms associated with SDB.
Table 4 presents the symptoms reported in the questionnaires. If the subject underwent clinical evaluation, these symptoms were confirmed. If a treatment had been prescribed for SDB, it was also extracted from the questionnaires and confirmed at subject evaluation. As the table demonstrates, the differences between data obtained from control relatives and Group A relatives are minor. Controls usually had a lower percentage of subjects with symptoms (which again is not surprising given the inclusion criteria for controls); however, most of the differences were not significant.
Even after taking into consideration the differences in the total number of subjects in each of the three subpopulations, Group B appears to be very different from the other two groups. For example, approximately 65% of Group B relatives snore, compared with 20.8% of Group A relatives. In fact, all symptoms associated with SDB are highly represented in the Group B relative population (see Table 4).
Signs associated with SDB.
Table 5 is based only on the subjects' physical evaluations. The clinical craniofacial evaluation confirms that the anatomical findings known to be associated with SDB are much more prevalent in Group B relatives than in group A relatives.
Reported treatment with SDB.
Finally, Table 6 shows that Group B relatives have been treated for SDB with nasal CPAP, UPPP, dental appliances, or other maxillomandibular surgeries, whereas very few Group A relatives were similarly treated. Interestingly, the Group B relatives also report double the frequency of asthma and nasal allergies than those in Group A or in the control group.
Families of normal controls.
Of the parents, eight men and one woman (9.4%) were reported to be intermittent snorers. Although 26 grandparents (a number that includes questionnaire-only respondents) (15.7%) were reported to snore “regularly,” only two were reported to snore “loudly.” None of the parents or grandparents studied were found to currently be undergoing or to have undergone treatment for OSAS; this fact is not surprising in view of the inclusion criteria. Five siblings (1%) were expected to undergo or were undergoing orthodontic treatment for class II malocclusions. One child (0.02%) had tonsils scored at “+3”. None were reported to have asthma.
In conclusion, Tables 4–6 indicate that major differences exist between family members of Group A infants (normal breathing group) and those of Group B (obstructive breathing group) insofar as the percentage of relatives presenting symptoms or signs associated with SDB is concerned. Family members of Group C infants were closely related to those of Group A infants.
DISCUSSION
The results show that infants identified by polygraphic recording with SDB in early infancy are more likely to have a positive family history of SDB in close relatives. During the first weeks of life, a child's “dolichocephaly”(17) is often masked and is easier to see in parents and siblings. The presence of signs or symptoms of SDB in the relatives of an infant can provide an important diagnostic clue. It is thus necessary to ask questions concerning symptoms and signs of SDB in first-degree relatives when an infant is referred for an ALTE, noisy breathing during sleep, or abnormal nocturnal behavior.
Our study had its limitations. As in many studies of this type, it was difficult to obtain the participation of all family members. The lowest response rate occurred among the black families. This is unfortunate insofar as all black infants were classified in Group B (evidence of SDB). Their percentage in our population is higher than the overall percentage of blacks in the immediate vicinity of Stanford University, where, based on data from the last census, whites and Asians represent the bulk of the population. Lack of financial support and inability to reimburse travel expenses may have been a handicap in reaching this community.
Another discrepancy in the study is the low number of referrals of Far-East Asian children. This is not related to low representation in the vicinity. The last census placed this group at approximately 7% of the Palo Alto area population (18). In addition, a substantial number of adult Asians are referred to our clinic for suspicion of SDB. The only two Asian infants referred were in group A and were the children of married students living away from their families. ALTE is less reported in the Asian community. Our study offers no explanation for this phenomenon.
The control group was selected in a way that avoided cases of SDB and, as such, was hypernormal. Analysis of the control group was conducted to indicate that Group A children and families presented closely related findings. This is the only value of this group in the study presented here, particularly given the near complete absence of blacks.
Our center has long been interested in SDB; it is therefore possible that a bias in recruitment exists. Infants referred to us for possible ALTE may have had a presentation that was suspicious to the referring pediatrician, and we may have an overrepresentation of children with SDB. Even if an overrepresentation exists, the issue is the frequency of breathing problems during sleep in close relatives of index cases.
The subjective nature of the study's anatomical scales should also be noted. Most of the scoring was done by one individual and this gave a certain uniformity to the data. These scales have been previously reported in the investigation of adults with SDB (19). Based on this first investigation, we developed a less-subjective technique with measurements in millimeters that has been reported in adults (16). Our study began before we implemented this new clinical approach. However, when adult normal and pathologic labeling were compared (in a population in which craniofacial measurements were obtained using the technique developed by Kushida et al.(16) and the technique presented here), there were no significant discrepancies between the two methods of measurement.
The fact that SDB occurs in familial aggregates has been previously reported (5, 6, 19–22), usually in studies examining adult index cases. In 1986, we reported several cases in which we documented a SIDS victim and both abnormal breathing during sleep and small upper airways in first-degree relatives of the victim (6). In the ten years since our 1986 report, we have had very few SIDS victims in the families we studied (this is not surprising in view of the frequency of SIDS). However, we have found infants who present a certain upper-airway anatomy and who are more prone to present SDB events (6, 23).
Our study shows that if, as a starting point, we select ALTE infants and base our subdivision of these infants on findings obtained during nocturnal polysomnography, we can delineate at least two groups. We find that one of the infant groups has many more abnormal breathing events of an obstructive type during sleep than the other group (group A). Group A infants have breathing patterns during sleep no different from those noted in a group of infants selected for study due to the absence of any clinical suspicion of SDB. The infants included in group B present with a higher frequency of mild facial dysmorphia. When the relatives of infants placed in each of the two groups are investigated, those with an obstructive SDB have a significantly higher chance of including members with overt SDB and with mild anatomic abnormalities involving the craniofacial complex and associated with the presence of a small upper airway. The small upper airway appears to be related to the anatomic buildup of the upper airway.
There is an unresolved debate concerning whether the small craniofacial anomalies that underlie SDB syndrome are related to genetics, environmental factors, or both. The existence of genetic factors in craniofacial-maxillomandibular development has been well known since the 1960s (24, 25). The many studies performed by Harvold and his group over a 15-y period on the rhesus monkey (26–29) have also demonstrated the role of environmental factors. That research has particularly emphasized the role of nasal resistance on nasal disuse, mouth breathing, and functional changes in craniofacial muscle contractions that may lead to craniofacial anatomical changes early in life. The anatomical features noted in our population may be risk factors for the development of SDB.
It is interesting to note that allergies and asthma are twice as prevalent in Group B subjects as they are in Group A and control subjects. This may be significant. Anatomical abnormalities present early in life may play a role in favoring nocturnal asthma in subjects who are susceptible to this illness later on in childhood (30).
Redline et al.(31), who studied risk factors for SDB in 2- to 18-y-old children, have also found that wheezing was an independent risk factor for SDB. These findings suggest that other familial risk factors may be present. The association of several risk factors in the same family may favor the appearance in early life of SDB, a possibility that is not considered in our study. A clinical point to note is that some ALTE incidents may be the first indication of an SDB syndrome; consequently, investigation of a family history of SDB is warranted when confronted with an ALTE in an infant.
Finally, the investigation of the families of subjects with SDB from early infancy to adulthood not only brings back the notion of familial aggregates but also the hypothesis that maxillomandibular complex grows in a different way. This growth is a phenomenon that takes place early in life, as 60% of the adult face is completely developed by the age of 4 y. The collection of data on families (with the inclusion of as many family members as can be reached) with index cases of SDB may allow for the calculation of potential genetic participation in the occurrence of the mild dysmorphia observed in a group of subjects with SDB.
Abbreviations
- ALTE:
-
apparent life-threatening event
- SIDS:
-
sudden infant death syndrome
- Pes:
-
esophageal pressure
- ECG:
-
electrocardiogram
- SDB:
-
sleep-disordered breathing
- UPPP:
-
uvulopalatopharyngoplasty
- PSG:
-
polysomnography
- OSAS:
-
obstructive sleep apnea syndrome
- CPAP:
-
continuous positive airway pressure
References
Guilleminault C, Peraita R, Souquet M, Dement WC 1975 Apneas during sleep in infants: possible relationship with sudden infant death syndrome. Science 190: 677–679
Guilleminault C, Ariagno RL 1978 Why should we study the “infant near miss for Sudden Infant Death”?. Early Hum Dev 2: 207–218
Guilleminault C, Ariagno R, Korobkin R, Nagel L, Baldwin R, Coons S, Owen M 1979 Mixed and obstructive sleep apnea and near miss for sudden infant death syndrome: comparison of near miss and normal control infants by age. Pediatrics 64: 882–891
Hoppenbrouwers T, Harper RM, Hodgman JE, Sterman MB, McGinty DJ 1978 Polygraphic studies of normal infants during the first months of life: II. Respiratory rate and variability as a function of state. Pediatr Res 12: 120–125
Strohl KP, Saunders NA, Feldman NT, Hallett M 1978 Obstructive sleep apnea in family members. N Engl J Med 299: 969–973
Guilleminault C, Heldt G, Powell N, Riley R 1986 Small upper airway in near-miss sudden infant death syndrome infants and their families. Lancet 1: 402–407
Guilleminault C, Pelayo R, Leger D, Philip P 2000 Apparent life-threatening events, facial dysmorphia and sleep-disordered breathing. Eur J Pediatr 159: 444–449
Brouillette R, Hanson D, David R, Klemka L, Szatkowski A, Fernbach S, Hunt S 1984 A diagnostic approach to suspected obstructive sleep apnea in children. J Pediatr 105: 10–14
Guilleminault C, Stoohs R, Skrobal A, Labanowski M, Simmons J 1993 Upper airway resistance in infants at risk for Sudden Infant Death Syndrome. J Pediatr 122: 881–886
Anders T, Emde R, Parmalee A 1971 A manual of standardized terminology, techniques and criteria for scoring states of sleep and wakefulness in newborn infants. UCLA Brain Information Service, Brain Research Institute, Los Angeles, CA, 1–68.
Guilleminault C, Souquet M 1979 Sleep states and related pathology. In: Korobkin R, Guilleminault C (eds) Advances in Perinatal Neurology. Spectrum Publications, New York, 225–247.
Guilleminault C, Kim YD, Stoohs R 1995 Upper airway resistance syndrome. Oral Maxillo Facial Clin North Am 7: 243–256
Marcus CL, Omlin KJ, Basinski DJ, Bailey SL, Rachel AB, Keens TG, Ward SLD 1992 Normal polysomnographic values for children and adolescents. Am Rev Resp Dis 146: 1235–1239
Coup A, Coup D, Wealthall S, Withy S 1983 The development and abnormality of breathing pattern. In: Tildon JT, Roeder LM, Steinschnider A (eds) Sudden Infant Death. Academic Press, New York, 423–441.
Miles L 1982 The sleep questionnaire and assessment of wakefulness (SQAW). In: Guilleminault C (ed) Sleep/Wake Disorders: Indications and Techniques. Addison Wesley, Menlo Park, CA, 384–4130.
Kushida CA, Efron B, Guilleminault C 1997 A predictive morphometric model for the obstructive sleep apnea syndrome. Ann Intern Med 127: 581–587
Stricker M, Raphael B 1993 Croissance crania-faciale normale et pathologique. Editions Morfos, Reims, France, 1–431.
1990 Census of Population and Housing Summary Tape, File 3A [computer file], Washington, DC
Guilleminault C, Partinen M, Hollman K, Powell N, Stoohs R 1995 Familial aggregates in obstructive sleep apnea syndrome. Chest 107: 1545–1551
Wittig RM, Zorick FJ, Roehrs TA, Sicklesteel JM, Roth T 1988 Familial childhood sleep apnea. Henry Ford Hosp Med J 36: 13–15
el Bayadi S, Millman RP, Tishler PV, Rosenberg C, Saliski W, Boucher MA, Redline S 1990 A family study of sleep apnea. Anatomic and physiologic interactions. Chest 98: 554–559
Redline S, Tosteson T, Tishler PV, Carskadon MA, Millman RP 1992 Studies in the genetics of obstructive sleep apnea. Familial aggregation of symptoms associated with sleep-related breathing disturbances. Am Rev Respir Dis 145: 440–444
Guilleminault C, Souquet M, Ariagno RL, Korobkin R, Simmons FB 1984 Five cases of near-miss sudden infant death syndrome and development of obstructive sleep apneas syndrome. Pediatrics 73: 71–78
Kraus BS, Wise WJ, Frei RH 1959 Heredity and the cranio-facial complex. Am J Orthod 45: 172–217
Holland PW 1988 Homeobox genes and the vertebrate head. Development 103: 17–24
Harvold EP 1968 The role of function in the etiology and treatment of malocclusion. Am J Orthod 54: 883–898
Tomer BS, Harvold EP 1982 Primate experiments on mandibular growth direction. Am J Orthod 82: 114–119
Miller A, Vargervik K, Chierici G 1984 Experimentally induced neuromuscular changes during and after nasal airway obstruction. Am J Orthod 85: 385–392
Vargervik K, Harvold EP 1987 Experiments on the interaction between oro-facial function and morphology. Ear Nose Throat J 66: 201–208
Guilleminault C, Quera-Salva MA, Powell N, Riley R, Romaker A, Partinen M, Baldwin R, Nino-Murcia G 1988 Nocturnal asthma: snoring, small pharynx and nasal CPAP. Eur Respir J 1: 902–907
Redline S, Tishler PV, Schluchter M, Aylor J, Clark K, Graham G 1999 Risk factors for sleep disordered breathing in children: associations with obesity, race and respiratory problems. Am J Resp Crit Care Med 159: 1527–1532
Acknowledgements
Dr. Guilleminault is the recipient of an Academic Award from the Center for Sleep Research of the National Heart, Lung, and Blood Institute.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guilleminault, C., Pelayo, R., Leger, D. et al. Sleep-Disordered Breathing and Upper-Airway Anomalies in First-Degree Relatives of ALTE Children. Pediatr Res 50, 14–22 (2001). https://doi.org/10.1203/00006450-200107000-00006
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200107000-00006
This article is cited by
-
Apparent Life-Threatening Events (ALTE): Italian guidelines
Italian Journal of Pediatrics (2017)
-
Scheinbar lebensbedrohliche Ereignisse im Säuglingsalter
Monatsschrift Kinderheilkunde (2003)