Abstract
The aim of this study was to investigate whether reoxygenation with 21% O2 rather than 100% O2 results in reduced hydrogen peroxide (H2O2) concentrations in neutrophils (PMN). Piglets (2–4 d old) exposed to severe hypoxia (inspired fraction of oxygen, 0.08) were randomized to resuscitation with 21 (n = 13) or 100% O2 (n = 12). Five animals served as controls. H2O2 concentrations in PMN in terms of rhodamine 123 (Rho 123) fluorescence intensity from arterial and superior sagittal sinus blood were quantified by flow cytometry. Laser Doppler flowmetry (LDF) was used to assess cortical blood perfusion. During hypoxia, Rho 123 increased in arterial PMN in both study groups by 15 and 32%, respectively (p < 0.05). In cerebral venous PMN, the increase was less dominant (p = 0.06). Reoxygenation with 100 or 21% O2 had no different effect on Rho 123 in arterial PMN. In cerebral venous PMN, Rho 123 was approximately 40% higher after 60 min and 30% higher after 120 min compared with corresponding data in the 21% O2 group (p < 0.05), which were close to baseline levels. Further, O2 treatment in both groups induced PMN accumulation in arterial blood (p < 0.05). Laser Doppler flowmetry signals increased during transient hypoxia (p < 0.0001 compared with baseline) and were normalized after reoxygenation in both study groups. In conclusion, arterial and cerebral venous H2O2 concentration in PMN tended to increase during hypoxia. During reoxygenation, H2O2 concentration in PMN in the cerebral circulation was low with 21% O2 but remained high with 100% O2 ventilation. We speculate that oxygen should be reintroduced with more caution during neonatal resuscitation.
Similar content being viewed by others
Main
The primary release of products of the sequential reduction of oxygen, superoxide radical (O2−) and H2O2, and the secondary production of hydroxyl radical (HO−) constitute the molecular mechanism of oxygen toxicity. Any system producing O2− will, as a result of the dismutase reaction, also produce H2O2. Although stable, the damaging redox properties of H2O2 and its ability to form highly reactive free radicals in the presence of transition metal ions have caused the body to form defenses against it. The role of oxygen toxicity in the development of perinatal hypoxic-ischemic encephalopathy is still a matter of debate. The principal hypothesis put forward to explain this process is the oxygen free radical theory (1, 2).
Stimulation of PMN during hypoxia-reoxygenation may increase the concentration of reactive oxygen species (3) in these cells. To date, the production of H2O2 in PMN during hypoxia and resuscitation with pure or air-mixed O2 has not been studied in detail. Reoxygenation is necessary to prevent further injury to neuronal tissue, but the renewed availability of O2 to previously hypoxic brain tissue may also have detrimental effects both with respect to the microcirculation and to the parenchyma of the brain. The production of reactive oxygen metabolites may be proportional to Pao2, and the oxygen tension achieved during reactive hyperemia and reoxygenation with O2 concentrations higher than 21% may generate a correspondingly higher burst of these metabolites. However, we do not know with certainty whether the production of reactive oxygen species during resuscitation depends on the concentration of inspired O2(4–7).
The aim of the present study was to investigate the hypothesis that arterial and cerebral venous PMN activated by hypoxia produce higher H2O2 concentrations by reoxygenation with 100% compared with 21% O2. For this purpose, newborn piglets primarily exposed to hypoxia were randomized to resuscitation with 100 or 21% O2. The conversion of DHR 123 into Rho 123 was used as a fluorescent marker of H2O2 production in white blood cell suspensions. We studied the applicability of the oxidative dye DHR 123 as an available sensitive direct indicator of H2O2 content in PMN. Further, we characterized the temporal course of the cortical microvascular blood perfusion in the cortex and the CMRO2 during hypoxia and reoxygenation. Regional cerebral microcirculation was simultaneously monitored using the LDF technique.
METHODS
Animal preparation.
The experiments were performed on 2–4-d-old newborn piglets of both sexes, weighing from 1125 to 2065 g (1577 ± 50 g). Anesthesia was induced by mask inhalation of 3% halothane (Fluothane, Zeneca, Oslo, Norway) mixed with O2 until unconsciousness was achieved. Halothane inhalation was discontinued when a 3.5-uncuffed endotracheal tube (SIMS Portex, Hythe, UK) was inserted via tracheotomy and connected to a volume-controlled ventilator (900 B, Siemens Elema, Solna, Sweden). A humidifier (Humid-Vent Micro +3.5, Louis Gibeck, Upplands Väsby, Sweden) was connected to the endotracheal tube. Tidal volume was kept at 30 mL/kg and the respiratory frequency at 40 breaths/min to achieve a Paco2 at a range of 4–6 kPa. End-tidal CO2 was continuously measured with a CO2 monitor (Engström Eliza Plus, Datex-Ohmeda AB, Bromma, Sweden). Fio2 was set at 0.21. Inspired O2 concentration was monitored with an oximeter (Datex Instrumentation Corp., Helsinki, Finland), which was calibrated before the start of each experiment.
After cannulation of the intermediate or lateral auricular vein, bolus injections of 6–10 mg/kg of sodium pentobarbital, 20 μg/kg of fentanyl (Leptanal, Janssen-Cilag, Holmlia, Norway), and 0.1 mg/kg of pancuronium bromide (Pavulon, Organon Teknika, Cambridge, UK) were given. A continuous sodium pentobarbital infusion (6 mg·kg−1·h−1) was administered throughout the experiments except during the hypoxic period. Repeated doses of 2–4 μg/kg of fentanyl and 0.05 mg/kg of pancuronium bromide were given hourly. An i.v. infusion containing 0.75% NaCl and 1.25% glucose was given at a rate of 10 mL·kg−1·h−1. Polyethylene catheters (Portex PE 5, inside diameter 0.58 mm, SIMS Portex Ltd., Hythe, UK) were inserted into the left external jugular vein for maintenance of anesthesia and fluid replacement and into the right femoral artery for blood pressure monitoring. Body temperature was monitored by a rectal thermometer and kept at 36.5–38.5°C by a radiant heating lamp and warm blankets, minimizing temperature-induced variations on metabolism.
The animals were then laid in a prone position. After infiltration of 2–3 mL of 1.0% lidocaine (Astra Zeneca, Södertälje, Sweden), a longitudinal midline incision extending from the glabella to the C2 vertebra was made. A stereotaxic head holder (David Kopf Instruments, Tujunga, CA, U.S.A.) was used to clamp the head by ear bars and a mouthpiece bar at three points. Bone landmarks were used to define the planes. The axial horizontal plane was defined by a line passing through the bregma and lambda at right angles to the vertical planes. All coordinates were defined by the position of the bregma. Four holes, 3 mm in diameter, were drilled in the frontoparietal area of the skull. An 18-gauge cannula was inserted into the superior sagittal sinus for blood sampling. Two laser Doppler microprobes were placed in the exposed cortex with the dura removed by small incisions. The laser Doppler probes were initially held in position with methylmethacrylate (Histoacryl, Braun Melsungen AG, Melsungen, Germany) 16 mm anterior and 4.5 mm bilateral to the midline. To achieve permanent stability, the probes were inserted through cork cylinders, which fitted the hole in the skull. The fiber-tip position was set at 3 mm below the cortical surface in the frontal lobes at 0° from the vertical. The laser Doppler probes were connected to master probes with screw couplings (model PF 318, Perimed AB, Stockholm, Sweden). A nitric oxide-sensitive electrode was inserted in the left cortex. The arterial cannula was connected to a pressure transducer (Baxter Uniflow 43-212, Bentley Laboratories, Europe B.V., Uden, Netherlands) for continuous recording of arterial blood pressure and for collecting blood samples for the DHR 123 assay for analysis of blood gases and pH measurements. LDF measurements and arterial blood pressure recordings were transferred to a computer program by use of an analogue-to-digital converter (model M100 WS, Biopac Systems Inc., Santa Barbara, CA, U.S.A.) at a sample rate of 2/s.
Blood samples.
To measure blood gases and acid base status, 0.5 mL of arterial and sagittal sinus blood was taken before hypoxemia, 2, 5, and 30 min after start, at the end of hypoxemia, and at 5, 30, 60, and 120 min of reoxygenation. The withdrawn blood was replaced by 2.5-fold amounts of normal saline. Temperature-corrected arterial blood gases were analyzed with an AVL 945 automatic blood gas system (AVL Biomedical Instruments, Schaffhausen, Switzerland). Blood glucose was regularly analyzed using the hexokinase method in plasma (Gluco-quant Glucose, Boehringer Mannheim GmbH, Mannheim, Germany). Ten to 15 mL of glucose 5% solution was given i.v. when serum glucose concentration was <4 mmol/L. C-reactive protein was checked routinely to detect responses due to neutrophil activation for reasons other than changes in ventilatory O2 concentrations (e.g. infection) and was measured in EDTA plasma by an immunologic test (Tina-quant CRP, Boehringer Mannheim GmbH, Germany) at the same time points as for the H2O2 analysis. Leukocyte differential count was performed on a hematology cell counter (Cell Dyn 3500, Abbott Laboratories, Abbott Park, IL, U.S.A.) using arterial blood samples.
Reagents.
FACS lysing solution (10 × concentrate) was obtained from Becton Dickinson Immunocytometry Systems (Becton Dickinson, Lincoln Park, NJ, U.S.A.). DHR 123, MW 346.38, molecular formula C21H18N2O3 (Molecular Pobes, Eugene, OR, U.S.A.), sensitive to both light and air, was dissolved in dimethylsulfoxide (Sigma Chemical Co., St. Louis, MO, U.S.A.) at a concentration of 500 μM, and aliquots were stored in deoxygenated containers at −20°C in the dark.
Cell isolation.
Five hundred microliters of blood (Microtainer Brand, EDTA anticoagulated, Becton Dickinson, Vacutainer Systems, Franklin Lakes, NJ, U.S.A.) was drawn simultaneously from the femoral artery and from the superior sagittal sinus. For immediate isolation of the white blood cells (mainly neutrophils, monocytes, and lymphocytes), a mixture of 300 μL of blood and 3 mL of FACS lysing solution 1:10 was incubated in round-bottom polystyrene test tubes (Falcon 2058, Becton Dickinson Labware, Lincoln Park, NJ, U.S.A.). After lysis of red cells for 10 min, leukocytes were centrifuged at 160 ×g for 5 min, the pellet was resuspended in 3 mL of the lysing solution, and the cells were centrifuged again at 300 ×g and 1200 rpm for 5 min. Finally, they were washed once in 3 mL of Dulbecco's PBS + 2% FCS and centrifuged at 200 ×g and 1000 rpm for 5 min. The pellet was then incubated in 400 μL of PBS + 2% FCS + 5 mmol glucose, and the cells were kept at 4°C until subjected to flow cytometric analysis within 2 h.
Measurement of H2O2 concentration in neutrophils.
The pharmacologic probe DHR 123 was applied as a green fluorescence indicator in the flow cytometric analysis of H2O2 in neutrophils, as first described by Bass et al.(8). The principle behind the H2O2 assay is oxidation of the nonfluorescent compound DHR 123 into the highly fluorescent compound Rho 123 by primarily neutrophil-associated H2O2(9). The extracellular oxidation of DHR 123 to Rho 123 is extremely slow unless catalyzed by an enzyme with peroxidase activity. Myeloperoxidase from the azurophilic granules is the only peroxidase that has been described in neutrophils (10), and it has been shown to be essential for intracellular oxidation of DHR coupled with H2O2 activity (11, 12). Rho 123 cannot pass the plasma membrane and is retained within the cell. Neutrophil Rho 123 fluorescence intensity is proportional to the concentration of generated H2O2 and was detected by a 488-nm argon laser-equipped flow cytometer. The reaction is highly specific for respiratory burst activity, as it occurs in neutrophil subpopulations (13). Spontaneous oxidation of DHR 123 to Rho 123 over time was counteracted by keeping the dye solution refrigerated during the experiment and prewarmed to 37°C in the dark 30 min before use. DHR 123 was added at a final concentration of 30 μM, and the samples were incubated at room temperature for 5 min in the dark. After centrifugation at 500 ×g for 5 min, they were resuspended in 400 μL of PBS + 2% FCS + 5 mmol glucose. Dye uptake in granulocyte cells is fast and is considered to be temperature-insensitive, and a steady state was quickly achieved.
Flow cytometry analysis.
A standard flow cytometer (FACScan, Becton Dickinson, Immunocytometry Systems, San Jose, CA, U.S.A.) with excitation at 488 nm was used. Monocytes, lymphocytes, and dead cells were distinguished from intact granulocytes by measurement of the cellular forward angle and 90° side scatter. Fifteen × 103 events were acquired for data storage. For identifying neutrophils, an appropriate freeform polygonal software gate was carefully set around the granulocyte population, created as a two-parameter cytogram dot plot (Fig. 1). Each sample was run in this setup mode until the granulocyte acquisition gate was established. Gated cells were analyzed for their fluorescence properties. Rho 123 green fluorescence was collected in the FL-1 channel (530 nm, standard FITC filter set), and a fluorescence histogram was plotted (Fig. 2). The linear channels of the analog digital converter were reconverted to log values for this purpose (1–104). Data that met the gating criterion were collected in list mode and processed for statistical analysis. Because the flow cytometer acquisition gives relative semiquantitative and not absolute values of the Rho 123 fluorescence intensities, H2O2 concentration is measured in terms of Δ ln of baseline values and not in pmol concentrations in the detected cell clusters. DHR 123-free samples were run to test interfering background substances and were all found to be negative. Generation of H2O2 was measured in cell suspensions derived from the blood samples during the experiments. The values obtained are directly proportional to the average H2O2 generation within the reacting cells. The CELLQuest FACStation software (Becton Dickinson, Immunocytometry Systems, San Jose, CA, U.S.A.) for acquisition and analysis was run on a Macintosh computer.
Rho 123 fluorescence histograms. Relative changes in H2O2 concentration are proportional to the Rho 123 fluorescence intensity. Values at baseline, during hypoxia (Fio2 = 0.08) at 5 (H5) and 60 (H60) min, during reoxygenation with 21% O2 at 5 (R5), 60 (R60), and 120 (R120) min are shown. Each measurement is presented as one graph (overlay). Movement of the curves on the x axis (logarithmic scale) to the right is associated with an increase in Rho 123 fluorescence intensity, movement to the left with a decrease. FL-1, indicates FL-1 channel. (A) H2O2 concentration during hypoxia and during reoxygenation with 21% O2 in one animal. (B) H2O2 concentration during hypoxia and during reoxygenation with 100% O2 in one animal.
Measurement of cortical microvascular blood perfusion.
LDF has been established as a reliable method for the measurement of regional microvascular blood perfusion (14). The two-channel laser Doppler flowmeter (Periflux 4001 Master, Perimed AB, Stockholm, Sweden) emits a low-power 2-mW helium-neon laser light with a wavelength of 632.8 nm, which is directed to the tissue by the optical fibers (PF 319:0, 210 mm long and 0.5 mm in diameter). The magnitude and frequency of the Doppler shifted light are proportional to the number and velocity of blood cells moving through the illuminated area of the tissue. Photodetectors sample frequency information and convert back-scattered light into electrical signals that are measured in millivolts. Flowmeters provide relative, not absolute, values of blood flow, so that the measurement of mainly red blood cell flux by LDF is expressed in arbitrary PU. Directional blood flow is not measured. A good correlation between LDF and radionuclide-labeled microspheres for measuring cerebral blood flow in rabbits (coefficient of 0.92) (14) and in pigs (15) has been reported. The reference illuminated area for this type of probe is approximately 1.0–3.5 mm3 of tissue (16). The signals were considered inadequate if the LDF was nonpulsatile or the measurements were less than 20 PU at baseline. Postmortem values were considered to be zero blood flow and subtracted from actual values. Left- and right-side LDF measurements were monitored by two independent channels.
Experimental protocol.
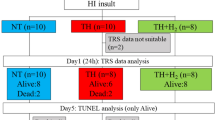
The animals were allowed to stabilize after completion of instrumentation for 1 h before the start of the experiment. After baseline recordings, hypoxia was produced by the inhalation of 8% O2 in 92% nitrogen. Hypoxia was terminated when MABP was <15 mm Hg or BE <−20 mmol/L or pH <7.0. Animals were randomized at the end of hypoxemia for reoxygenation with either 21% O2 (n = 13) or 100% O2 (n = 12) for 30 min, followed by 21% O2 for another 1.5 h. Control animals were exposed to 21% O2 throughout the observation time of 4 h (n = 5). Two laser Doppler flow signals, MABP, and nitric oxide (NO) electrode signals (data not shown) were continuously recorded throughout the experiment.
Calculated variables and statistical analysis.
CMRO2 was calculated by the following formula: (Cao2 − CssO2) × LDF, where Cao2 is the arterial oxygen content = (Hb) × (carrying capacity Hb) × (Sao2%) + (Pao2) × (solubility of oxygen in blood), and CssO2 is the cerebral venous oxygen content = (Hb) × (carrying capacity Hb) × (SssO2%) + (PssO2) × (solubility of oxygen in blood). CMRO2 values were displayed as relative numbers.
Variables recorded during a 15-s period were averaged to obtain one measuring point. Laser Doppler signals from two channels were averaged for each measuring point to use in statistical analysis. Because the laser Doppler provides relative values expressed in arbitrary PU rather than in blood flow in mL/100 g tissue/min, data of cortical microvascular blood perfusion were expressed as percentages in relation to baseline.
Changes from baseline DHR fluorescence intensity were expressed as percentages of baseline.
All values are presented as mean ± SEM. A mixed-model ANOVA for repeated measurements was used to investigate the effect of time, group, and group-by-time interactions. The effect of time within each group was studied by a 1-way analysis for repeated measurements. When a group-by-time effect was found, the t test was used to compare the baseline or the end-of-hypoxia values and the peak values at 5, 60, and 120 min of reoxygenation. This model was used to compare the treatment groups with regard to the following variables: MABP, pH, BE, Pco2, Po2, C-reactive protein, arterial oxygen saturation (SO2), DHR fluorescence, leukocytes, PMN, and CMRO2. A p value < 0.05 was considered statistically significant. Calculations were performed employing Stat View version 3.1 for Macintosh, Abacus Concepts, Inc., Berkley, CA, U.S.A.
Approval.
The present study was performed with the consent of the Institutional Animal Care and Use Committee of the University of Oslo. The experiments conformed to the guidelines for the care and handling of laboratory animals published by the European Convention for the Protection of Vertebrate Animals Used for Experimental and Other Scientific Purposes of March 18, 1986.
RESULTS
The total duration of hypoxia was 66 ± 2 min in the 100% O2 group and 71 ± 3 min in the 21% O2 group (NS). There were no significant differences between any of the three groups in any measured variable at baseline or between the two reoxygenated groups at the end of the hypoxemic period.
Physiologic variables.
Data for MABP are shown in Table 1. The acute responses (after 90 s) to hypoxemia led to a rapid but not significant increase in MABP of 4 mm Hg (both groups combined), which then decreased significantly toward the end of the hypoxemic period. During the first 5 min of reoxygenation, MABP increased by 44% in the 100% O2 group and by 18% in the 21% O2 group (compared with end of hypoxia). However, the group-by-group differences were not significant. At the end of the reoxygenation period, the MABP was 49 ± 5 mm Hg in the room air group and 55 ± 5 mm Hg in the 100% O2 group, which was significantly lower than baseline values (p < 0.05). Group-by-group effects during reoxygenation were not significant (p = 0.2).
CMRO2.
Calculations of CMRO2 during hypoxia and reoxygenation with 100 or 21% O2 are shown in Table 2. During hypoxia, CMRO2 decreased by 35 to 50% (p < 0.005 versus baseline) in the two hypoxemic groups. Reoxygenation with 100 and 21% O2 produced different responses at 60 min of reoxygenation. In the 100% group, CMRO2 rose from 2.8 ± 0.5 at the end of hypoxia to 4.5 ± 0.6 (p < 0.05). CMRO2 was higher in the 21% O2 group and rose from 3.7 ± 0.5 to 5.8 ± 0.5 at the end of hypoxemia (NS compared with the end of hypoxia). At 60 min of reoxygenation, the group-by-group comparison displayed a higher CMRO2 in the room air group than in the 100% O2 group (p < 0.05). However, at 120 min of reoxygenation, CMRO2 in all groups was restored, and no differences between the groups were found.
Blood gases.
pH, Pco2, Po2, BE, and SO2 values from arterial and venous sagittal sinus blood are shown in Tables 3 and 4. During hypoxemia, arterial pH and BE fell as expected dramatically in both study groups. During reoxygenation, pH and BE began to revert to normal and, after 120 min of reoxygenation, pH and BE values were almost restored in both groups. At the end of the hypoxia period, Pao2 fell to values lower than 3.5 kPa in both groups. During ventilation with 100% O2, Pao2 rose to 50.0 ± 5.0 kPa in the 100% O2 group and to 11.1 ± 0.4 kPa in the 21% O2 group. At the end of the experiments, O2 tension was normalized in both groups. During hypoxia, the changes in cerebral venous pH and BE were parallel to the values obtained from arterial blood. PssO2 fell 1–2 kPa during hypoxia, and cerebral venous O2 saturation (SssO2) decreased in mean 35% in the 100% O2 group and 24% in the 21% O2 group (p < 0.001 versus baseline values). During reoxygenation with 100% O2, PssO2 was 9.9 ± 1.9 kPa (100% O2) and 5.7 ± 0.7 kPa (21% O2). SssO2 rose by approximately 40% in the 100% O2 group and by 30% in the 21% O2 group compared with the end-of-hypoxia values. During reoxygenation, the values declined slowly until they reached subnormal values at the end of the experiment.
Paco2 was not significantly different between the two study groups at any time and was kept stable within the physiologic range (4.6–5.4 kPa) throughout the experiments in all animals.
C-reactive protein, oxyhemoglobin, and plasma glucose.
C-reactive protein from plasma derived from arterial and cerebral venous blood was negative (<10 mg/L) at baseline, during hypoxia, and during reoxygenation in all samples. Hb was stable throughout the study, and no differences were found between the groups. Plasma glucose concentrations were not different between the groups; however, a slight increase during the hypoxic period in both study groups was seen (data not shown).
White blood cells, granulocytes.
The total number of circulating leukocytes in arterial blood (Fig. 3) rose from baseline by 11% at the end of the hypoxemic period in both groups (NS). This increase continued during reoxygenation, and maximal values were obtained at 120 min of reoxygenation: 12.3 ± 1.5 cells × 109/L in the 100% O2 group versus 10.7 ± 1.1 at end of hypoxia (p < 0.05) and 13.2 ± 2.1 cells × 109/L in the 21% O2 group versus 8.8 ± 1.3 at end of hypoxia (p < 0.05); however, no intergroup differences were found. The relative number of circulating PMN in the 100% O2 group rose from 36.1 ± 5.3% at the end of hypoxia to 42.2 ± 4.7% (p < 0.05), in contrast with PMN in the 21% O2 group in which the number was unchanged.
Rho 123 fluorescence intensity in neutrophil cells.
Changes in Rho 123 fluorescence intensity during normoxia, hypoxia, and reoxygenation with 21 or 100% O2 are shown in Table 5 for arterial and cerebral venous samples. Arterial H2O2 concentration in PMN increased significantly at the end of hypoxia by 14.7 ± 4.7% and by 32.2 ± 14.5% in the 21 and 100% O2 groups, respectively (p < 0.05 versus baseline, both groups combined), with no significant difference between the two groups. During reoxygenation, baseline concentrations were obtained after 5 min both in the 100% O2 group and in the 21% O2 group and did not change from this level until the end of the experiment. The concentrations in the 21% O2 group tended to be lower than in the 100% group, but ANOVA for repeated measurements did not show a significant group-by-time difference between the two reoxygenated groups.
At the end of hypoxia in cerebral venous blood, H2O2 concentration tended to increase compared with baseline (121.1 ± 14.1% for the 100% group and 113.7 ± 8.6% for the 21% group, p = 0.06; both groups combined).
During reoxygenation in the 100% O2 group, levels of H2O2 remained elevated and were significantly higher both at 60 min (25.5% increase, p < 0.05 compared with baseline) and at 120 min of reventilation (13.5% increase, p < 0.05 compared with baseline), i.e. even 90 min after Fio2 had been reduced to 0.21. In contrast, at the same time points in the 21% O2 group, significantly lower H2O2 concentrations compared with the 100% O2 group were found (p < 0.05 versus 100% O2 group) and were approximately 10% lower compared with baseline.
Microvascular blood perfusion in the cortex.
Regional cortical microvascular perfusion increased significantly after 5 min of hypoxia by 26% for the 100% O2 group and by 49% for the 21% O2 group (p = 0.0006 versus baseline, both groups taken together). This increase seemed to reach a steady state during the period of hypoxia, and, at the end of hypoxia, it was approximately 39 and 49% higher for the respective groups than their baseline values (p < 0.0001, both groups taken together). During reoxygenation, LDF curves in both study groups returned to baseline levels and were similar to the corresponding control values of the normoxemic group. No differences were found between the two reoxygenation groups during the 2-h posthypoxic observation period (Fig. 4).
DISCUSSION
The present study showed an increased H2O2 concentration in PMN from arterial blood during hypoxia; by contrast, in cerebral venous blood, the H2O2 level in PMN tended to increase only. After reoxygenation, H2O2 was elevated in the 100% O2 group and lowered in the 21% O2 group compared with baseline. Hypoxia also resulted in an augmentation of regional cerebral blood flow in the cerebral cortex that remained until the end of hypoxemia. The cerebral microcirculation was restored as efficiently with room air as with 100% O2. After 60 min of reoxygenation, CMRO2 in the 21% O2 group tended to be higher than in the 100% O2 group.
Free radicals may stimulate the accumulation and activation of granulocytes. The exact role of PMN in triggering the oxidative-antioxidative balance during hypoxia-reoxygenation is unknown. The DHR flow cytometry assay in total leukocyte preparations used in the present study offers a direct detection system to measure intracellular H2O2 concentrations in PMN but not the generation of O2−(11). Adherent PMN that would have escaped measurement are not included. This means that only H2O2 concentration in circulating PMN was monitored. Others have shown that intracellular oxidation of DHR 123 is a sensitive and reliable method of quantifying H2O2 in PMN (13, 17, 18). However, flow cytometric experiments in cell suspension require cautious interpretation. Even normally stimulated PMN may respond heterogeneously, suggesting the existence of functional differences in the circulating cells (8). This heterogeneity in the oxidative response has to be taken into account.
Measurements of H2O2 concentrations were performed in circulating PMN in the cerebral and systemic circulation but not in the brain tissue. Neutrophils may act as inflammatory cells and are particularly important in the induction of oxidative stress in endothelial cells in the cerebral vascular bed (19, 20). Oxidative stress on endothelial cells invoked by neutrophils (and possibly monocytes, too) is at least partially responsible for the neutrophil rolling, adhesion, and finally migration through the endothelium into the tissue. Interaction of H2O2 with endothelial cells rapidly depletes ATP and causes extracellular appearance of xanthine and hypoxanthine. In vitro exposure of endothelial cells to H2O2 reduced intracellular ATP concentration by 72%(19). Neutrophil cells have the ability to initiate margination through the endothelium out of the circulating pool into the tissue and may stimulate microglia to produce cytokines as IL-1 and tumor necrosis factor-α (TNF-α). Expression of TNF-α, IL-1, and IL-6 was observed more frequently in brain lesions of neonatal brains with periventricular leukomalacia than in those without periventricular leukomalacia (21). A recent study in cultured bovine cerebral microvascular cells during hypoxia/reoxygenation demonstrated the influence of TNF-α and IL-1 on the adhesion of neutrophils and monocytes to the endothelium (22). Further, oligodendrocytes in culture exposed to H2O2 may facilitate apoptotic cell death (23, 24), indicating that H2O2 appears to participate in the cascade to oligodendroglial cell death. Thus, the appearance of reactive oxygen species including H2O2 in circulating cells in the brain may have importance for progressive intracerebral oxidative mechanisms in connection with hypoxia and reoxygenation. The release of reactive oxygen species from circulating leukocytes may go on in the brain and induce sequestration of the perivascular microenvironment. Increasing experimental evidence indicates that PMN adhesion should be further investigated.
Normally produced H2O2 is necessary for bactericidal mechanisms in the neutrophil cell. H2O2 can be produced either spontaneously or by Superoxide dismutase (SOD)-catalyzed dismutation of O2−. Our results suggest that the production of cerebral H2O2 is O2-dependent. This was also supported by a study in brains of rats exposed to room air where H2O2 was calculated to be 7.7 pM and a rise of approximately 60% was reported when O2 tension was increased to 100%(25). Armstead et al.(26) have demonstrated a significant production of O2− anion (8.7 ± 1.5 pmol/mm−2/20 min) in connection with global cerebral ischemia-reperfusion in the newborn pig, and, recently, an increased free radical production by fetal brain in postasphyxial lambs was demonstrated (27) despite oxygen tensions of only 3–3.5 kPa. As indicated in human studies (28), accumulation of H2O2 during hypoxia and hyperoxia may reflect a high production of O2−. The effect of 100% O2 on free radical formation was recently studied employing the electron spin resonance technique (4). The results of the latter study indicated that reoxygenation with 100% O2 was associated with significantly more free radical generation than reoxygenation with 21% O2. However, two studies have been performed in which hyperoxia after brain ischemia was not found to increase the concentration of reactive oxygen metabolites (5, 7).
Accumulation of leukocytes may contribute to an increase in cerebral H2O2 concentration during reoxygenation with 100% O2. H2O2 efflux (superior sagittal sinus) values were found to be significantly higher than the influx values (femoral artery) in the 100% O2 but not in the room air group. The antioxidant defense capacity may be overwhelmed by reoxygenation with 100% O2 due to an overload of reactive oxygen species. This could finally result in a higher cerebral H2O2 concentration, as demonstrated in this study. However, it is still unclear how effectively the newborn immature brain can mobilize a protective antioxidative response to the hyperoxic challenge.
It can be questioned whether the Fio2 was the only variable of interest associated with the changes of H2O2 concentrations. The influence of plasma glucose concentration on the brain in hypoxia-reoxygenation is still a matter of debate. As expected, in the present study, a slight increase of plasma glucose concentration during the hypoxic stress in both study groups was seen. Compared with the findings of Andersen et al. (4), it seems to us to be the most plausible explanation that oxygen is the most likely source of the H2O2 accumulation.
Another response to hypoxia and reoxygenation was an increase in PMN in the systemic circulation. Hallenbeck et al.(29) have shown in a canine model that cerebral hypoperfusion was associated with PMN accumulation in the injured brain hemisphere during the early postischemic period. Caceres et al.(30) showed in asphyxiated piglets that leukocyte accumulation occurred in cerebral arteries 4–6 h after the insult. Neutrophil accumulation in cerebral blood vessels may plug the microcirculation and cause damage from within the blood vessels during the first 24 h after asphyxia (31). This fits in with the observation that allopurinol-induced neutrophil depletion may be beneficial to the neonatal brain in rats exposed to hypoxia-ischemia (31). Neutrophils have a diameter of approximately 10 μm and have to be deformed before passing through the capillaries. Activated neutrophils will cause obstruction due to the loss of their viscoelastic properties. Moreover, the activated endothelium may express adhesion molecules, which attract circulating neutrophils and cause them to adhere (32).
We found that hypoxemia caused an initial increase in cortical microvascular perfusion of approximately 150% of baseline values, after which the flow returned to normal values at approximately 60 min of reoxygenation. Unexpectedly, there was no further increase in perfusion after the start of reoxygenation in either study group. As demonstrated in previous studies, when the microsphere technique (33) or the LDF technique (34) was used to assess regional cerebral blood flow in the cortex, the circulation was restored as efficiently with 21 as with 100% O2. However, the latter findings do not necessarily prove that there are no differences in deeper and more sensitive brain regions.
Hypoxia induced a decrease in forebrain oxygen uptake (CMRO2), which became restored during reoxygenation. After the start of reoxygenation, room air tended to induce a higher CMRO2 than 100% O2, which became significant after 60 min. It seemed that reoxygenation with 100% O2 reduced the O2 extraction and utilization in the predominantly cortical brain areas assessed in the present study. This depression in the O2 metabolism when oxygen is available in excess may reflect a protective mechanism possessed by the whole brain or a lower metabolic rate of oxygen in tissues drained by the superior sagittal sinus.
The fact that formation of H2O2 in cerebral venous PMN during reoxygenation with 21% O2 was lower, in contrast with the concentration found during reoxygenation with 100% O2, and that cortical vascular perfusion was restored in both groups indicates that care must be taken when higher O2 concentrations are used. Reducing the O2 to a more moderate level may be of therapeutic importance, a proposition that should be further examined.
In conclusion, H2O2 concentration in arterial PMN of newborn piglets increased during hypoxia and tended to increase in PMN from cerebral venous blood. During reoxygenation, neutrophil cells accumulated in the systemic arterial circulation. At the same time, H2O2 concentration in PMN in the cerebral circulation was low with room air but remained high with pure oxygen ventilation. Further, cortical microvascular perfusion increased during transient hypoxia and was almost normalized after reoxygenation in both study groups. We speculate that reoxygenation with increased oxygen concentrations may have side effects. This indicates that oxygen should be reintroduced with caution during neonatal resuscitation.
Abbreviations
- BE:
-
base excess
- CMRO2:
-
cerebral metabolic rate of oxygen
- DHR 123:
-
dihydrorhodamine 123
- Fio2:
-
inspired fraction of O2
- H2O2:
-
hydrogen peroxide
- LDF:
-
laser Doppler flowmetry
- MABP:
-
mean arterial blood pressure
- Pao2:
-
arterial O2 tension
- Pco2:
-
carbon dioxide tension
- PMN:
-
polymorphonuclear leukocytes
- PssO2:
-
cerebral venous oxygen tension
- PU:
-
perfusion units
- Rho 123:
-
rhodamine 123
References
Gerschman R, Gilbert DL, Nyl SW 1954 Oxygen poisoning and x-ray irradiation: a mechanism in common. Science 119: 624–626
Palmer C 1995 Hypoxic-ischemic encephalopathy. Therapeutic approaches against microvascular injury, and role of neutrophils, PAF, and free radicals. Clin Perinatol 22: 481–517
Fellman V, Raivio KO 1997 Reperfusion injury as the mechanism of brain damage after perinatal asphyxia. Pediatr Res 41: 599–606
Andersen CB, Hoffman DJ, Du C, McGowan JE, Ohnishi ST, Delivoria-Papadopoulos M 1997 Effect of reoxygenation with 21% or 100% oxygen on free radical formation following hypoxia in the cerebral cortex of newborn piglets. Pediatr Res 41: 30A(abstr)
Cino M, Del Maestro RF 1989 Generation of hydrogen peroxide by brain mitochondria: the effect of reoxygenation following postdecapitative ischemia. Arch Biochem Biophys 269: 623–638
Mickel HS, Vaishnav YN, Kempski O, von Lubitz D, Weiss JF, Feuerstein G 1987 Breathing 100% oxygen after global brain ischemia in Mongolian gerbils results in increased lipid peroxidation and increased mortality. Stroke 18: 426–430
Agardh CD, Zhang H, Smith ML, Siesjo BK 1991 Free radical production and ischemic brain damage: influence of postischemic oxygen tension. Int J Dev Neurosci 9: 127–138
Bass DA, Parce JW, Dechatelet LR, Szejda P, Seeds MC, Thomas M 1983 Flow cytometric studies of oxidative product formation by neutrophils: a graded response to membrane stimulation. J Immunol 130: 1910–1917
Emmendorffer A, Hecht M, Lohmann-Matthes ML, Roesler J 1990 A fast and easy method to determine the production of reactive oxygen intermediates by human and murine phagocytes using dihydrorhodamine 123. J Immunol Methods 131: 269–275
Lehrer RI, Ganz T 1990 Antimicrobial polypeptides of human neutrophils. Blood 76: 2169–2181
Henderson LM, Chappell JB 1993 Dihydrorhodamine 123: a fluorescent probe for superoxide generation?. Eur J Biochem 217: 973–980
van Pelt LJ, van Zwieten R, Weening RS, Roos D, Verhoeven AJ, Bolscher BG 1996 Limitations on the use of dihydrorhodamine 123 for flow cytometric analysis of the neutrophil respiratory burst. J Immunol Methods 191: 187–196
Rothe G, Oser A, Valet G 1988 Dihydrorhodamine 123: a new flow cytometric indicator for respiratory burst activity in neutrophil granulocytes. Naturwissenschaften 75: 354–355
Eyre JA, Essex TJ, Flecknell PA, Bartholomew PH, Sinclair JI 1988 A comparison of measurements of cerebral blood flow in the rabbit using laser Doppler spectroscopy and radionuclide labelled microspheres. Clin Phys Physiol Meas 9: 65–74
Kirkeby OJ, Rise IR, Nordsletten L, Skjeldal S, Hall C, Risoe C 1995 Cerebral blood flow measured with intracerebral laser-Doppler flow probes and radioactive microspheres. J Appl Physiol 79: 1479–1486
Johansson K, Jakobsson A, Lindahl K, Lindhagen J, Lundgren O, Nilsson GE 1991 Influence of fibre diameter and probe geometry on the measuring depth of laser Doppler flowmetry in the gastrointestinal application. Int J Microcirc Clin Exp 10: 219–229
Smith JA, Weidemann MJ 1993 Further characterization of the neutrophil oxidative burst by flow cytometry. J Immunol Methods 162: 261–268
Emmendorffer A, Nakamura M, Rothe G, Spiekermann K, Lohmann-Matthes ML, Roesler J 1994 Evaluation of flow cytometric methods for diagnosis of chronic granulomatous disease variants under routine laboratory conditions. Cytometry 18: 147–155
Ward PA 1991 Mechanisms of endothelial cell killing by H2O2 or products of activated neutrophils. Am J Med 91: 89S–94S
Fantone JC, Ward PA 1982 Role of oxygen-derived free radicals and metabolites in leukocyte-dependent inflammatory reactions. Am J Pathol 107: 395–418
Yoon BH, Romero R, Kim CJ, Koo JN, Choe G, Syn HC, Chi JG 1997 High expression of tumor necrosis factor-alpha and interleukin-6 in periventricular leukomalacia. Am J Obstet Gynecol 177: 406–411
Li TJ, Rui YC, Xu JP 1999 Effects of hypoxia/reoxygenation and cytokines on adhesion of leukocytes to cerebral microvascular endothelial cells. Zhongguo Yao Li Xue Bao 20: 137–140
Kameshwar-Rao AS, Gil S, Richter-Landsberg C, Givol D, Yavin E 1999 H2O2-induced apoptotic death in serum-deprived cultures of oligodendroglia origin is linked to cell differentiation. J Neurosci Res 56: 447–456
Richter-Landsberg C, Vollgraf U 1998 Mode of cell injury and death after hydrogen peroxide exposure in cultured oligodendroglia cells. Exp Cell Res 244: 218–229
Yusa T, Beckman JS, Crapo JD, Freeman BA 1987 Hyperoxia increases H2O2 production by brain in vivo. J Appl Physiol 63: 353–358
Armstead WM, Mirro R, Busija DW, Leffler CW 1988 Postischemic generation of superoxide anion by newborn pig brain. Am J Physiol 255: H401–H403
Bagenholm R, Nilsson UA, Gotborg CW, Kjellmer I 1998 Free radicals are formed in the brain of fetal sheep during reperfusion after cerebral ischemia. Pediatr Res 43: 271–275
Shigeoka AO, Charette RP, Wyman ML, Hill HR 1981 Defective oxidative metabolic responses of neutrophils from stressed neonates. J Pediatr 98: 392–398
Hallenbeck JM, Dutka AJ, Tanishima T, Kochanek PM, Kumaroo KK, Thompson CB, Obrenovitch TP, Contreras TJ 1986 Polymorphonuclear leukocyte accumulation in brain regions with low blood flow during the early postischemic period. Stroke 17: 246–253
Caceres MJ, Schleien CL, Kuluz JW, Gelman B, Dietrich WD 1995 Early endothelial damage and leukocyte accumulation in piglet brains following cardiac arrest. Acta Neuropathol Berl 90: 582–591
Hudome S, Palmer C, Roberts RL, Mauger D, Housman C, Towfighi J 1997 The role of neutrophils in the production of hypoxic-ischemic brain injury in the neonatal rat. Pediatr Res 41: 607–616
Hudetz AG, Wood JD, Kampine JP 1999 Nitric oxide synthase inhibitor augments post-ischemic leukocyte adhesion in the cerebral microcirculation in vivo. Neurol Res 21: 378–384
Rootwelt T, Loberg EM, Moen A, Oyasaeter S, Saugstad OD 1992 Hypoxemia and reoxygenation with 21% or 100% oxygen in newborn pigs: changes in blood pressure, base deficit, and hypoxanthine and brain morphology. Pediatr Res 32: 107–113
Kutzsche S, Kirkeby OJ, Rise IR, Saugstad OD 1999 Effects of hypoxia and reoxygenation with 21% and 100% oxygen on cerebral nitric oxide concentration and microcirculation in newborn piglets. Biol Neonate 76: 153–167
Acknowledgements
The authors thank Mette K. Olafsen for her advice on the use of the FACScan flow cytometer.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by grants from the Faculty of Medicine, University of Oslo, the AGA AB Medical Research Fund, and Rolf Geir Gjertsen Foundation.
Rights and permissions
About this article
Cite this article
Kutzsche, S., Ilves, P., Kirkeby, O. et al. Hydrogen Peroxide Production in Leukocytes during Cerebral Hypoxia and Reoxygenation with 100% or 21% Oxygen in Newborn Piglets. Pediatr Res 49, 834–842 (2001). https://doi.org/10.1203/00006450-200106000-00020
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200106000-00020
This article is cited by
-
Resuscitation with 100% oxygen increases injury and counteracts the neuroprotective effect of therapeutic hypothermia in the neonatal rat
Pediatric Research (2012)
-
Why are we still using oxygen to resuscitate term infants?
Journal of Perinatology (2010)
-
Postresuscitation N-acetylcysteine treatment reduces cerebral hydrogen peroxide in the hypoxic piglet brain
Intensive Care Medicine (2008)
-
Lebensrettende Maßnahmen bei Kindern (Paediatric Life Support, PLS)
Notfall + Rettungsmedizin (2006)
-
Oxygen for Newborns: How Much is Too Much?
Journal of Perinatology (2005)