Abstract
Carboxyterminal propeptide of type I procollagen (PICP), a marker of bone formation, has not yet been studied in preterm infants. In this study, PICP concentrations were measured longitudinally for 12 wk after birth using the ELISA technique in 43 preterm infants with a gestational age (GA) ranging from 24–29 wk and in 35 preterm infants with a GA ranging from 30–34 wk. PICP values in these preterm infants were higher than in children and adults. In cord plasma of preterm infants there was a significant gender difference, with higher PICP concentrations in male infants. A characteristic longitudinal pattern with an initial decrease during the first 3 postnatal days followed by a rapid increase from d 7 to d 28 was seen in both groups. Regarding the individual gestational ages, all preterm infants attained maximum PICP concentrations around 36 wk postmenstrual age. Multiple regression analysis revealed cord plasma PICP concentrations were significantly associated with GA, birth weight, sex, and IGF-I. A significant correlation between PICP concentrations and GA was seen at wk 1–4 and between PICP concentrations and protein intake at wk 1. Body weight and energy intake were shown to exert a significant effect on the PICP concentrations at 2 wk. The collected data in preterm infants may serve further studies evaluating PICP as a marker for bone formation and growth in very low birth weight premature infants.
Similar content being viewed by others
Main
Pediatricians rely on gain in body weight and length as standard parameters to assess thriving and growth of preterm infants. However, in preterm infants body weight may be influenced by the state of hydration, and common anthropometric measurements tend to be difficult and faulty. A predictive marker of bone formation would be very helpful in identifying preterm infants with reduced bone formation at an early stage. Carboxyterminal propeptide of type I procollagen (PICP) can be used to assess short-term therapeutic effects, for example, of growth hormone (1). PICP has been shown to be a useful marker for the rate of collagen type I production and seems to be a promising parameter for use in clinical practice (2). Collagen is the major structural protein of the extracellular matrix in the body. Type I collagen is the main body collagen and the major product of osteoblasts, accounting for more than 90% of the organic substance of bone; it is a constituent of soft connective tissues together with other collagens (2–4). After the secretion of the procollagen, the amino- and the carboxyterminal peptide are cleaved and collagen is formed. The carboxyterminal propeptides can subsequently be identified in serum in a stoichiometric relationship to the quantity of collagen molecules formed (5). The propeptides significantly correlate with histomorphometric measurements of bone formation (2, 6), indicating that PICP serum levels are a physiologic marker of bone formation. As PICP is not filtered by the kidneys, its serum levels are not dependent on renal function (7).
Previous studies have demonstrated the utility of this marker in infants. PICP levels in children are closely related to growth velocity (8–10). So far there is no information on PICP concentrations in preterm infants.
Our prospective study was performed to collect data on PICP in conjunction with growth and nutrition in premature infants.
METHODS
Patients.
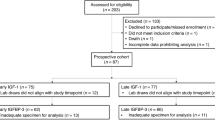
This study included all preterm infants (gestational age [GA] 24–34 wk) that were born in the Children's Hospital of the University of Tübingen and treated at the Department of Neonatology, starting from February 1995 until September 1996, if informed written consent was obtained from the parents. The parents of six preterm infants refused to participate.
The study population consisted of 78 preterm neonates (42 females, 36 males) with a GA between 24 and 34 wk. None of the infants had major congenital malformations or apparent diseases of bone, liver, kidney, or renal system. Twenty-seven of 67 (40%) of the mothers of the preterm infants had antenatal steroid therapy for lung maturation. Twenty-two of 78 (28%) of the preterm infants had postnatal early or late dexamethason therapy for chronic lung disease. Osteopenia of prematurity was not observed in the routine radiographic chest analysis.
Small for gestational age was defined as a birth weight below the 10th percentile. The local standard growth curves were used for infants from 24 to 27 weeks (11) and the Swiss growth chart was used for infants from 28–34 weeks (12). That was because the Swiss growth chart starts with a GA of 28 weeks. Infants having a birth weight between the 10th and 90th percentiles were categorized as appropriate for GA. According to their GA (determined from the last menstrual period of the mother and by antenatal ultrasonic measurements), the population was further divided into two groups—24–29 wk GA and 30–34 wk GA. Table 1 shows the clinical details of our study population.
PICP concentrations in cord serum of 80 appropriate for GA term newborns (40 male, 40 female, mean birth weight 3610 g [2950–4100 g]) served as controls.
The protocol of the study was approved by the ethical committee of the University of Tübingen in December 1994.
Study protocol.
EDTA blood samples were collected in conjunction with routine blood sampling, which was performed between 5 and 7 a.m. Plasma was separated by centrifugation, frozen, and stored at –20°C until assayed for PICP. Body weight (g) was recorded daily and at the time of serum sampling. Individual nutritional intake was evaluated for energy (kcal), protein (g), and calcium (mg).
Biochemical analyses: assay for plasma PICP.
PICP concentrations in plasma were measured on d 1, 2, and 3 and wk 1, 2, 3, 4, 8, and 12 after birth using ELISA (Metra/Biosystems, USA) (13). Before analysis the samples were diluted with a standardized serum pool 1:11. The sensitivity of the assay (minimum detectable limit) was 0.2 ng/mL. The intra-assay coefficients of variation were 6.8, 5.5, and 6.6 at concentrations of 80.8, 98.1, and 296.7 ng/mL, respectively; interassay coefficients of variation at these levels were 7.0, 7.2, and 5.0. IGF-I was measured with a specific RIA (RIA; Mediagnost, Tübingen, Germany). In this assay an excess of IGF-II eliminates interference by insulin-like growth-factor-binding proteins (14).
Data analysis.
Median values were calculated and the cumulative frequency distribution for PICP was separately given for each time point. Pairwise comparisons were done by the Wilcoxon test. A stepwise multiple regression analysis was performed to model the main effects of the potential explanatory variables (age [gestational age + postnatal age], sex, body weight, IGF-I, intake of protein, calcium, and energy] on the PICP values separately in cord plasma and on d 7, 14, 21, and 28. A linear model was fitted to calculate the p value and R2 of the whole model as well as the p values of the test statistics for each parameter. The level of statistical significance was set at α = 0.05.
RESULTS
PICP concentrations.
The number of samples analyzed at the different times is shown in Table 2 and Table 3. As a result of the longer hospital stay for the extremely low birth weight infants, these are overrepresented at the end of the observation period.
The PICP reference levels (medians) at various postnatal ages according to the gestational age of the preterm infants and the reference levels for term newborns are illustrated in Figures 1 and 2 as well as in Table 2.
Cord plasma PICP concentrations of preterm infants showed a significant sex difference, with lower concentrations in girls. Controls born at term had lower PICP concentrations in cord plasma and there was no difference according to gender (Table 2).
During the investigation period PICP levels showed a characteristic course (Figs. 1 and 2). A rapid decrease in PICP concentrations during the initial postnatal days in both groups (GA 24–29 wk, p < 0.0008; GA 30–34 wk, p < 0.07) was followed by a significant increase from d 7 to d 28 (GA 24–29 wk, p < 0.02; GA 30–34 wk, p < 0.0001). In infants with a GA ranging from 24–29 wk median PICP concentrations were lower from d 3 to d 28 than in infants with a GA ranging from 30–34 wk. Independent of GA, all preterm infants reached their peak plasma PICP concentration around 36 wk postmenstrual age;i.e. the group with lower GA at birth (24–29 wk GA) showed the peak aproximately 4 wk later.
Multiple regression analysis.
In cord plasma the GA, birth weight, sex, and IGF-I are significantly correlated with the PICP levels. The GA was proven to exert a significant effect on the PICP concentrations at 1, 2, 3, and 4 wk postnatal age. PICP levels were significantly associated with protein intake in the first week of life, and with energy intake and body weight in the second week of life. The calculated regression models explained 39–47% of the variations of the outcome variable.
Table 4 shows the results of the multiple regression analysis, which was confirmed for both groups of the study population.
DISCUSSION
Our study showed that PICP concentrations were higher in preterm infants than in children and adults. This could be an indicator for greater osteoblast activity and type I collagen synthesis in preterm infants.
Cord plasma levels of PICP in preterm infants with a GA from 24–29 wk are higher compared with those with a gestational age from 30–34 wk. The functional significance of this age-dependent decrease is yet unclear, however, it parallels the curve of intrauterine longitudinal growth velocity, which rapidly decreases after the age of 30 wk (15).
A significant gender difference, with higher levels in male infants, was measured in cord plasma of preterm infants but not in that of term newborns. This difference could simply reflect the higher body mass in boys (weight, 1240 ± 383 g in boys versus 1059 ± 378 g in girls; length, 38 ± 4.5 cm in boys versus 36.4 ± 3.5 cm in girls). However, this is contradicted by the fact that there was no difference in the PICP concentrations of term infants despite significantly different anthropometric values.
During the period of sexual differentiation and throughout the second trimester of pregnancy, the serum concentrations of testosterone in male fetuses are higher than in female fetuses (16). At term, this difference is no longer observable. The higher testosterone concentrations in male fetuses (16, 17) might be responsible for the elevated PICP values in cord plasma of male preterms; as during puberty, testosterone concentrations and PICP are positively correlated (18).
Postnatally, PICP concentrations in premature infants exhibit a characteristic age-dependent pattern with a rapid decrease during the first 3 postnatal days and a slow increase thereafter (Figs. 1 and 2). This increase is delayed in the group of preterm infants born before 30 wk compared with the more mature ones. The early decrease in PICP concentrations is most likely caused by the catabolic metabolic condition during this period, which is even more pronounced in the younger preterm infants. PICP concentrations start to rise with increasing nutrition in our study population. The longitudinal course parallels postnatal growth velocity curves of both investigated groups (data not shown). The slower increase of PICP levels in preterm infants with lower GA (Fig. 1) may be caused by their higher morbidity (e.g. chronic lung disease or more frequent intolerance to enteral nutrition).
Regression analysis (Table 4) revealed that, aside from GA, birth weight, and sex, PICP concentrations in cord plasma are significantly correlated with IGF-I concentrations. IGF-I is an endocrine and paracrine growth factor in pre- and postnatal life and stimulates osteoblastic cell proliferation and function such as type I collagen synthesis in different model systems (19). Puistola et al. (20) suggested that IGF-I stimulates type I collagen synthesis during pregnancy. Our results indicate that IGF-I possibly stimulates fetal type I collagen synthesis. Postnatal PICP plasma concentrations were not significantly correlated with the plasma levels of IGF-I in our study group. However, this does not rule out its possible function as a link between the metabolic situation and osteoblast activity. IGF-I may well affect bone turnover at the tissue level through local autocrine or paracrine action .
One of our hypotheses was that nutritional factors might regulate circulating PICP concentrations. Regression analysis (Table 4) revealed effects of protein intake (d 7), total energy intake (d 14), and calcium intake (d 21 and 28); thereafter, no significant influence of nutrition could be demonstrated.
Enteral nutrition in premature infants consisted of protein-fortified and calcium- and potassium-enriched breast milk (approximately two-thirds of the infants) or formula for preterm infants (21, 22). After the fourth week of life, nearly all preterm infants in our study population got the recommended nutrient intake (i.e. energy, protein, and calcium), so influence of these nutritional factors could not be demonstrated after this time.
The GA was strongly correlated with the PICP concentrations in preterm infants during the first 4 wk, suggesting a higher osteoblast activity rate in preterm infants with higher GA. As shown by Lieuw et al. (23), in children PICP reflected previous growth velocity. We hypothesized that PICP concentrations in preterm infants are correlated with former catch-up growth.
CONCLUSION
For the first time, circulating PICP concentrations—as an important marker for osteoblast activity—were monitored in preterm infants, revealing a characteristic longitudinal pattern that is strongly influenced by GA. Founded on these normative data, PICP concentrations in preterm neonates might be used as a diagnostic tool to measure the effect of different nutritional regimes, a specific treatment, or bone disease. Its possible role as a predictor of catch-up growth and long-term development of children is under investigation.
Abbreviations
- PICP:
-
carboxyterminal propeptide of type I procollagen
- GA:
-
gestational age
References
Trivedi P, Ristelli J, Ristelli L, Hindmarsh CP, Brook CGD, Mowat AP 1991 Serum concentrations of the type I and III procollagen propeptides as biochemical markers of growth velocity in healthy infants and children and in children with growth disorders. Pediatr Res 30: 276–280
Parfitt AM, Simon LS, Villanueva AR, Krane SM 1987 Procollagen type I carboxy-terminal extension peptide in serum as a marker of collagen biosynthesis in bone. J Bone Miner Res 2: 427–436
Risteli J, Risteli L 1989 Growth and collagen. Curr Med Lit Growth Growth Factors 4: 159–164
Prockop DJ, Kivirikko KJI, Tuderman L, Guzman NA 1979 The biosynthesis of collagen and its disorder. N Engl J Med 301: 13–23
Graham MF 1989 The use of serum levels of procollagen propeptides to predict growth velocity. J Pediatr Gastroenterol Nutr 2: 143–145
Eriksen EF, Charles P, Melsen F, Mosekilde L, Ristelli L, Ristelli J 1993 Serum markers of type I collagen formation and degradation in metabolic bone disease: correlation with bone histomorphometry. J Bone Miner Res 8: 127–132
Calvo MS, Eyre DR, Gundberg CM 1996 Molecular basis and clinical application of biological markers of bone turnover. Endocr Rev 17: 333–368
Hyams JS, Carey DE, Leichtner AM, Goldberg BD 1989 Type I procollagen as a biochemical marker of growth in children with inflammatory bowel disease. J Pediatr 109: 619–634
Saggese G, Baroncelli GI, Bertelloni S, Cinquanta L, Di Nero G 1994 Twenty-four-hour osteocalcin, carboxyterminal propeptide of type I procollagen, and aminoterminal propeptide of type III procollagen rhythms in normal and growth-retarded children. Pediatr Res 35: 409–415
Saggese G, Bertelloni S, Baroncelli GI, Di Nero G 1992 Serum levels of carboxyterminal propeptide of type I procollagen in healthy children from 1st year of life to adulthood and in metabolic bone diseases. Eur J Pediatr 151: 764–768
Roemer VM, Buehler K, Kieback DG 1990 Gestationszeit und Geburtsgewicht. Z Geburtsh u Perinat 194: 241–253
Largo RH, Waelli R, Duc G, Fanconi A, Prader A 1980 Evaluation of perinatal growth. Helv Paediatr Acta 35: 419–436
Winterbottom N, Vernon S, Freeman K, Daniloff P, Garnero P, Seyedin S 1992 An immunoassay for the C-terminal propeptide of type I collagen. J Bone Min Res 7: 254
Blum WF, Breier BH 1994 Radioimmunoassay for IGFs and IGFBPs. Growth Regul 4: 11–19
Tanner JM 1989 Foetus into Man: Physical Growth from Conception to Maturity. Castle Mead Publications, Ware, U.K., pp 39
Hercz P, Kazy Z, Siklos P, Ungar L 1989 Quantitative comparison of serum steroid and peptide hormone concentrations in male and female fetuses in the maternal-fetoplacental system durng the 28th-40th weeks of pregnancy. Obstet Gynecol 30: 201–204
Abramovich DR, Rowe P 1973 Foetal plasma testosterone levels at mid-pregnancy and at term: relation to foetal sex. J Endocrinol 56: 621–622
Falorni A, Bini V, Cabiati G, Papi F, Arzano S, Celi F, Massimo S 1997 Serum levels of type I procollagen C-terminal propeptide, insulin-like-growth factor, and IGF binding protein-3 in obese children and adolescents: relationship to gender, pubertal development, growth, insulin and nutritional status. Metabolism 46: 862–871
Linkart TA, Mohan S, Baylink DJ 1996 Growth factors for bone growth and repair: IGF, TGFβ and BMP. Bone 19: 1S–12S
Puistola U, Risteli L, Kauppila A, Knip M, Risteli J 1993 Markers of type I and type III collagen synthesis in serum as indicators of tissue growth during pregnancy. J Clin Endocrinol Metab 77: 178–182
American Academy of Pediatrics, Committee on Nutrition. 1985 Nutritional needs of low-birth-weight infants. Pediatrics 75: 976–986
ESPGAN Committee on Nutrition of the Preterm Infant. 1987 Nutrition and feeding of preterm infants. Acta Paediatr Scand Suppl 336: 1–14
Lieuw-a-fa M, Sierra RI, Specker BL 1995 Carboxy-terminal propeptide of human type I collagen and pyridinium cross-links as markers of bone growth in infants 1 to18 months of age. J Bone Miner Res 6: 849–853
Acknowledgements
The authors thank Professor Gasser of the University of Zurich, Switzerland, for statistical advice.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Seibold-Weiger, K., Wollmann, H., Ranke, M. et al. Plasma Concentrations of the Carboxyterminal Propeptide of Type I Procollagen (PICP) in Preterm Neonates from Birth to Term. Pediatr Res 48, 104–108 (2000). https://doi.org/10.1203/00006450-200007000-00018
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200007000-00018
This article is cited by
-
Leptin and bone turnover in monochorionic twins complicated by twin–twin transfusion syndrome
Osteoporosis International (2007)
-
Physical Activity Combined with Massage Improves Bone Mineralization in Premature Infants: A Randomized Trial
Journal of Perinatology (2004)