Abstract
During pregnancy, 17β-estradiol (E2) and progesterone (P) plasma concentrations increase up to 100-fold. The fetus is exposed to these increasing amounts of E2 and P. Within 1 d after delivery, E2 and P concentrations fall to nonpregnancy concentrations in the mother and the infant. Extremely premature infants are cut off from the placental supply of E2 and P at a very early developmental stage, and therefore they suffer from this deprivation for a longer period than infants born at term. Nothing is known about the consequences of this deprivation. The purpose of this study was to investigate how intrauterine concentrations of E2 and P could be maintained after birth. In 13 infants with a median gestational age of 26.4 wk (24.1-28.7), a phospholipid-stabilized soybean oil emulsion available for parenteral nutrition that contains different amounts of E2 and P was continuously administered, starting within the first postnatal hours. The supplementation was continued as long as venous access was indicated but not longer than 6 wk (median 20 d, 12-44). To maintain intrauterine plasma concentrations of 2000-6000 pg/mL E2 and 300-600 ng/mL P, 2.30 mg·kg-1·d-1 E2 (1.13-3.42 mg·kg-1·d-1) and 21.20 mg·kg-1·d-1 P (11.23-27.36 mg·kg-1·d-1) were needed. We conclude that supplementation of E2 and P to maintain intrauterine concentrations in extremely premature infants is possible intravenously. The infants in this study are enrolled in a randomized, controlled pilot study to evaluate the potential benefits of E2 and P supplementation.
Similar content being viewed by others
Main
During pregnancy, concentrations of E2 and P increase up to 100-fold compared with the nonpregnant status(1). Determinations of umbilical cord plasma concentrations at different gestational ages have shown that the fetus is exposed to the same increasing concentrations of sex steroids. Reported mean values of E2 plasma concentrations at gestational ages of 28 to 40 wk range between 2 000 and 17 000 pg/mL in the umbilical vein and between 2 000 and 7 000 pg/mL in the umbilical artery(2–5). Plasma concentrations of P have been found between 200 and 1 700 ng/mL in the umbilical vein and between 100 and 1 200 ng/mL in the umbilical artery(6–8). The highest concentrations were observed at gestational ages between 33 and 36 wk with a decline toward the end of pregnancy. These sex steroids are produced by the placenta from precursors originating from the maternal and fetal circulation, known as the feto-placento-maternal unit(9). The placental supply of sex steroids is terminated at delivery, and the concentrations in the mother and the newborn infant decrease to nonpregnancy concentrations within 24 h. This is a physiologic condition for an infant delivered at term. An extremely premature infant is deprived of the supply of these steroids at an earlier developmental stage. Nothing is known about the consequences of the deprivation of E2 and P.
As shown in postmenopausal women, a deficiency of sex steroids can lead to bone demineralization(10). This is also seen in ELBW infants, even if mineral supplementation has been individually adjusted(11). In vitro studies on cultured neurons of rats support the view that E2 has an effect on neuronal growth and dendritic development(12,13). Would extremely premature infants benefit from supplementation with these hormones?
The aim of this study was to establish how the intrauterine concentrations of E2 and P could be maintained after birth. Because of frequent feeding problems in this group of patients and the known side effects of an oral application of sex steroids(14,15), a form of parenteral application was needed. Commercially available solutions containing E2 and P are developed only for intramuscular administration, in which a dosage adjustment is difficult because of depot effects. The aim of this study was to identify a preparation that would maintain the high intrauterine concentrations of E2 and P when continuously infused intravenously.
METHODS
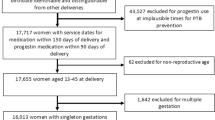
Subjects. Thirteen female infants with a median gestational age of 26.4 wk (24.1-28.7) and a median birth weight of 690 g (450-980) were investigated. Eleven of the 13 infants were delivered by cesarean section because of untreatable labor and/or pathologic cardiotocogram, and two had vaginal delivery. The infants are encountered in a randomized controlled pilot study evaluating the effect of E2 and P supplementation on clinical outcome data. The parents gave written informed consent. The study was approved by the local ethics committee.
Supplementation. Crystalloid E2 [estra-1,3,5(10)-triene-3,17β-diol; Fa. Synopharm, Hamburg, Germany] and P (pregn-4-ene-3,20-dione; Fa. Synopharm, Hamburg, Germany) were diluted in 98% ethanol in concentrations between 0.53 ng/mL and 17.8 mg/mL E2 and between 32 ng/mL and 100 mg/mL P. A phospholipid-stabilized soybean oil emulsion used for parenteral nutrition containing 0.2 g/mL fat (Intralipid® 20%; Pharmacia & Upjohn, Erlangen, Germany) was diluted with water to a content of 0.05 g/mL fat. To obtain mixtures containing 6.6 pg/mL to 0.17 mg/mL E2 and 0.4 ng/mL to 1.25 mg/mL P, 1.25 mL of the alcoholic E2 and P stock solution was added to 100 mL of the diluted fat solution. The E2 and P content of the different E2-P-lipid-5% mixtures ranged from 2.2 ng/mL to 0.22 mg/mL for E2 and from 0.4 µg/mL to 1.25 mg/mL for P. The E2-P-lipid-5% mixtures were compared by microscope for the size of lipid particles and for the separation of the lipid emulsion with the native Intralipid® 20% after a period of 24 h. Neither alteration in the size of the lipid particles nor a significant creaming was found in the E2-P-lipid-5% mixtures. The E2-P-lipid-5% mixtures were produced daily under aseptic conditions. The preparations were administered within 24 h.
Two estimations were made for the amounts of E2 and P required to maintain intrauterine concentrations. The first evaluated the postnatal decline of E2 and P in newborn infants(7,16,17). Assuming a decline of E2 plasma concentrations within 24 h from approximately 2 000 pg/mL to less than 100 pg/mL and P plasma concentrations from approximately 200 ng/mL to less than 10 ng/mL, at least 2 000 pg E2 and 200 ng P per mL of plasma disappear. In a newborn infant weighing 1 000 g with an assumed plasma volume of 40 mL/1 000 g, 2 000 pg × 40 = 80 000 pg = 80 ng E2 and 200 ng × 40 = 8 000 ng = 8 µg P per 24 h can be calculated. This calculation would be true for a constant metabolic rate for E2 and P, not taking into account a third compartment of E2 and P or de novo synthesis.
The second estimation was based on studies of the umbilical cord blood flow and the umbilical arteriovenous difference of P plasma concentrations(18). Using an umbilical blood flow rate of 75 mL/min and an umbilical arteriovenous difference of 212 ng/mL, we calculated that 23 mg of progesterone per day was delivered to the fetal circulation at term. This corresponds to 6.6 mg·kg-1·d-1 P in an infant with a birth weight of 3500 g. Assuming an umbilical arteriovenous difference for E2 of at least 2000-3000 pg(2–4), the amount of E2 delivered to the fetal circulation would be approximately 0.06-0.09 mg·kg-1·d-1 E2 at term.
As soon as central or peripheral venous access was available, the continuous infusion of 15 mL·kg-1·d-1 E2-P-lipid-5% mixture was started corresponding to 0.75 g·kg-1·d-1 parenteral fat. In the first infant given supplemental E2 and P, the E2-P-lipid-5% mixture provided approximately 0.1% of the amounts of E2 and P calculated by the first method. This dosage was expected to be too low but was used because of the lack of clinical experience with E2 and P supplementation in this group of infants. E2 and P plasma concentrations were measured in the umbilical cord blood and in sequential blood samples drawn at 24 h and 72 h on the 5th and 7th day and thereafter once a week. Additional samples were obtained from residues if diagnostic blood sampling was drawn from the infants for other reasons. The E2 and P plasma concentrations were received from the clinical laboratory within 4 h. Thereafter the E2 and P supplementation was adjusted via the infusion rate (median 19.2 mL·kg-1·d-1, 10.9-32) or an altered mixture of the E2-P-lipid-5% to maintain plasma concentrations of 2000-6000 pg/mL E2 and 300-600 ng/mL P. Supplementation was continued as long as venous access was indicated but not longer than 6 wk postnatally. After the supplementation had been stopped, the E2 and P plasma concentrations were measured again as soon as standard care indicated the need for blood sampling.
E2 and P measurement. Total unconjugated E2 and P were measured by commercially available EIA (Enzymun-Test® Estradiol and Enzymun-Test® Progesterone; Boehringer-Mannheim Biochemica, Mannheim, Germany). Measurements were performed on an ES300 analyzer (Boehringer Mannheim Biochemica, Mannheim, Germany). A maximum amount of 100 µL of plasma was needed. Samples with E2 and P concentrations exceeding the standard curve range were diluted with human plasma containing low endogenous E2 and P concentrations to retain the sample matrix for the test system. Diluted samples were corrected for endogenous E2 and P concentrations of the plasma. Intra- and interassay coefficients of variation were below 6%.
To test the accuracy of the E2-EIA, E2 was determined in the umbilical cord blood of 37 newborn infants (mean gestational age 38.9 wk, 35.9-42.0) both by the EIA as well as by ID/GC-MS. Regarding ID/GC-MS, plasma was equilibrated with [2,4-2H2] E2 (Sigma Chemical Co., Deisenhofen, Germany) as internal standard. After solvent extraction and purification, heptafluorobutyrate derivatives were prepared. GC was carried out on a Hewlett Packard 5890 GC housing an OV-1 fused silica capillary (25 m × 0.2 mm, film 0.1 µm; Macherey & Nagel, Düren, Germany). The GC was directly interfaced to a Hewlett Packard 5972 mass selective detector operated in the selected ion monitoring mode. For quantification ions m/z 664 (analyte) and m/z 666 (internal standard) were recorded.
RESULTS
The E2 and P supplementation with the corresponding E2 and P plasma concentrations for the first supplemented infant over the period of 33 d is shown in Figure 1. Starting with 100 pg·kg-1·d-1 E2 and 5.8 ng·kg-1·d-1 P, a plasma concentration of P greater than 300 ng/mL was reached on the 12th postnatal day with 11.86 mg·kg-1·d-1 P. E2 plasma concentrations of more than 2000 pg/mL was reached 5 d later with 6.23 mg·kg-1·d-1 E2.
Plasma concentrations of E2 and P were within the limits of 2000-6000 pg/mL E2 and 300-600 ng/mL P with a median daily supplementation of 2.30 mg·kg-1·d-1 E2 (1.13-3.42 mg·kg-1·d-1) and 21.20 mg·kg-1·d-1 P (11.23-27.36 mg·kg-1·d-1). These plasma concentrations could be achieved with individually adjusted supplementation in all of the 13 infants with the exception of one showing either plasma concentrations of P less than 300 ng/mL or greater than 600 ng/mL. Median duration of the E2 and P supplementation was 20 d (12-44). Figures 2 and 3 correlate the supplemented amounts of E2 and P with the corresponding E2 and P plasma concentrations for all 13 infants. The relation between them is best fitted by logarithmic functions. The intercept (E2: - 2.18; P: - 7.55) and slope (E2: 1.25; P: 11.08) of these functions represent the medians derived from the individual logarithmic functions (intercept, E2: -6.73 to 1.91; P: -39.67 to 13.84; slope, E2: 0.09 to 2.76; P: 2.32 to 24.85; n = 13). This calculation was done to compensate for the individual different number of samples resulting from varying durations of supplementation.
The median E2 and P plasma concentrations after discontinuation of the supplementation were 16 pg/mL (5-35) and 2.8 ng/mL (0.84-8.43), respectively. The median time from stopping the supplementation until blood sampling was 7 d(6–20).
No clinically obvious negative side effects that would have been related to the E2 and P supplementation have been observed.
When comparing the concentrations of E2 present in umbilical cord plasma of the 37 newborn infants 7 961 pg/mL (median, 2 146 - 24 527) were found by EIA and 7 340 pg/mL (2 490 to 19 350) by ID/GC-MS. Although ID/GC-MS yielded slightly lower and less scattering concentrations of E2, the overall correlation with EIA values was good (r = 0.89; Pearson, p < 0.05) and showed an exceptional reliability for a direct immunoassay.
DISCUSSION
To our knowledge this is the first study of E2 and P supplementation in ELBW infants to maintain the intrauterine plasma concentrations of E2 and P after birth. Clinical research that is related to this approach involved the prenatal exposure of human fetuses to synthetic estrogens and progestins. Beginning in the early 1940s and throughout the following 30 y, more than 2 million pregnant women were treated with synthetic estrogens such as DES. The initial concept was that DES would stimulate placental progesterone secretion because progesterone deficiency was related to abortion and premature delivery(19). Therapy was started in "risk pregnancies", e.g. previous abortions or early bleedings, as early as the 6th wk of gestation. The therapy was shown to reduce prematurity and to improve survival(19,20). Several studies were performed retrospectively to evaluate the effects of intrauterine estrogen and progestin therapy on educational attainment. A higher intelligence level was found in infants of progesterone treated mothers(21,22). Effects on personality and psychosexual identity in infants born to mothers treated with synthetic progestins and estrogens were described(23). Higher prevalence of tomboyishness and personality factors such as independence, sensitivity, heightened individuality, and self-assuredness were observed in individuals who had been exposed to prenatal hormone. After the possibility of developing vaginal adenocarcinomas had been discussed in young women associated with their intrauterine exposure to DES, treatment of "risk pregnancies" with this drug was abandoned(24).
There are two important differences between estrogen supplementation in pregnancies and supplementation in ELBW infants. First, DES treatment was started as early as the 6th wk of gestation. Therefore, in a very early stage of organogenesis the genital tract was exposed to a synthetic drug known to have a biologic activity 5-fold higher than the natural 17β-estradiol. Second, it was a treatment for the mother without an evaluation of the plasma concentrations reached in the fetus.
Several studies in rodents deal with the neonatal administration of estrogens and progestins and considered effects (e.g. cancerogenicity) on the genital tract, breast tissue, and adrenal gland(25–27), or influence on sex specific behavior(28). However, the effects observed were the result of a nonphysiologic high exposure to certain hormones. Supplementation of E2 and P in ELBW infants is an attempt to adapt the hormonal environment to the intrauterine physiologic condition.
Reported umbilical cord plasma concentrations of E2 and P vary between 2 000 and 17 000 pg/mL and between 100 and 1 700 ng/mL, respectively(2–8). Our measurements in seven infants born at a gestational age of 24 to 30 wk (median 27) with a median birth weight of 840 g (720-960) resulted in median concentrations of 3 900 pg/mL (1 295-8 054) for E2 and 480 ng/mL (228-1 185) for P. These results, together with the concentrations referred to in other studies, led us to aim supplementation at plasma concentrations of 2 000-6 000 pg/mL E2 and 300-600 ng/mL P.
The determination of steroids in the neonatal period by immunoassays can lead to extremely false-positively elevated concentrations with widely disparate reference ranges. This phenomenon has been attributed to potential interferences, e.g. steroid sulfates, originating from the fetal adrenal zone(29). ID/GC-MS currently presents the most specific technique in steroid analysis, because this physicochemical technique is independent of phenomena such as matrix effects or cross-reactivity. Comparison of the used E2-EIA, a direct immunoassay with the reference method ID/GC-MS showed that E2 concentrations were significantly overestimated. But we think that the small difference is without clinical relevance with regard to the physiologic intrauterine reference.
A median daily supplementation of 2.30 mg·kg-1·d-1 E2 and 21.20 mg·kg-1·d-1 P was needed to reach the desired plasma concentrations. These results show E2 requirements to be approximately 30 times higher than E2 requirements calculated from the arteriovenous difference of E2 plasma concentrations and the blood flow in the umbilical cord. The supplemented P was approximately 3 times higher than that calculated by the same method. The included arteriovenous differences of E2 and P umbilical cord plasma concentrations were 2 000 pg/mL and 212 ng/mL, respectively. However, arteriovenous differences up to 10 000 pg/mL for E2 and 500 ng/mL for P have been reported, bringing the calculated and supplemented amounts of E2 and P nearer to each other. In addition, the ability of sex steroids to adsorb to synthetic surfaces, as found with i.v. lines and syringes, has to be taken into consideration. In an experimental setting with an E2-P-lipid-5% mixture containing tritium-labeled E2 (3H-E2) and P (3H-P) administered over 24 h through an i.v. line system used in the infants, approximately 80% of the radioactivity for 3H-E2 and 60% for 3H-P was detectable after passage through the line system (unpublished data). Therefore, supplemented E2 and P had been adsorbed in part to the i.v. line.
Umbilical cord blood concentrations of E2 and P show no sex-specific differences in the cited literature. Nevertheless, we studied only female infants because uterine growth and vaginal cytology can serve as parameters to monitor biologic effects of the E2 and P supplementation.
We conclude that maintenance of intrauterine plasma concentrations of E2 and P in ELBW infants is possible via i.v. supplementation. We observe no side effects; however, our experience is limited. The 13 infants represented here are part of a current randomized, controlled pilot study, evaluating the effect of E2 and P supplementation on bone mineralization and clinical outcome in ELBW infants. Mid- and long-term follow-up with these infants is needed before supplementation of E2 and P can be regarded as a valid new approach to the care of ELBW infants.
Abbreviations
- E2:
-
17β-estradiol, pg/mL × 3.671 = pmol/L
- P:
-
progesterone, ng/mL × 3.18 = nmol/L
- ELBW:
-
extremely low birth weight
- DES:
-
diethylstilbestrol
- EIA:
-
enzyme immunoassay
- ID/GC-MS:
-
isotope dilution/gas chromatography-mass spectrometry
References
Tulchinsky D, Hobel CJ, Yeager E, Marshall JR 1972 Plasma estrone, estradiol, estriol, progesterone, and 17 - hydroxyprogesterone in human pregnancy: I-normal pregnancy. Am J Obstet Gynecol 112: 1095–1100.
Kenny FM, Angsusingha K, Stinson D, Hotchkiss J 1973 Unconjugated estrogens in the perinatal period. Pediatr Res 7: 826–831.
Hercz P, Ungar L, Siklos P, Farquharson RG 1988 Unconjugated 17 beta-oestradiol and oestriol in maternal serum and in cord vein and artery blood at term and preterm delivery. Eur J Obstet Gynecol Reprod Biol 27: 7–12.
Tayama C, Ichimaru S, Ito M, Nakayama M, Maeyama M, Miyakawa I 1983 Unconjugated estradiol, estriol and total estriol in maternal peripheral vein, cord vein, and cord artery serum at delivery in pregnancies with intrauterine growth retardation. Endocrinol Jpn 30: 155–162.
Herruzo AJ, Mozas J, Alarcon JL, Lopez JM, Molina R, Molto L, Martos J 1993 Sex differences in serum hormone levels in umbilical vein blood. Int J Gynaecol Obstet 41: 37–41.
Scommegna A, Burd L, Bieniarz J 1972 Progesterone and pregnenolone sulfate in pregnancy plasma. Am J Obstet Gynecol 113: 60–65.
Sippell WG, Becker H, Versmold HT, Bidlingmaier F, Knorr D 1978 Longitudinal studies of plasma aldosterone, corticosterone, deoxycorticosterone, progesterone, 17-hydroxyprogesterone, cortisol, and cortisone determined simultaneously in mother and child at birth and during the early neonatal period: I-spontaneous delivery. J Clin Endocrinol Metab 46: 971–985.
Hercz P 1985 Quantitative changes in steroid and peptide hormones in the maternal-fetoplacental system between the 28th-40th weeks of pregnancy. Acta Med Hung 42: 29–39.
Siler-Khodr TM 1992 Endocrine and paracrine function of the human placenta. In: Polin RA, Fox WW (eds) Fetal and Neonatal Physiology. WB Saunders, Philadelphia, 74–85.
Lindsay R 1988 Sex steroids in the pathogenesis and prevention of osteoporosis. In: Riggs BL, Melton III J (eds) Osteoporosis: Etiology, Diagnosis and Management. Raven Press, New York, 333–358.
Pohlandt F 1994 Prevention of postnatal bone demineralization in very low-birthweight infants by individually monitored supplementation with calcium and phosphorus. Pediatr Res 35: 125–129.
Uchibori M, Kawashima S 1985 Effects of sex steroids on the growth of neuronal processes in neonatal rat hypothalamus-preoptic area and cerebral cortex in primary culture. Int J Dev Neurosci 3: 169–176.
Arimatsu Y, Hatanaka H 1986 Estrogen treatment enhances survival of cultured fetal rat amygdala neurons in a defined medium. Brain Res 391: 151–159.
Geola F, Frumar A, Tataryn I, Lu K, Hershman J, Eggena P, Sambhi M, Judd H 1980 Biological effects of various doses of conjugated equine estrogens in postmenopausal women. J Clin Endocrinol Metab 51: 620–625.
Judd H 1987 Efficacy of transdermal estradiol. Am J Obstet Gynecol 156: 1326–1331.
Radfar N, Ansusingha K, Kenny FM 1976 Circulating bound and free estradiol and estrone during normal growth and development and in premature thelarche and isosexual precocity. J Pediatr 89: 719–723.
Dvoracsek E, Kassai Z, Torok I, Balogh A 1990 Sexual steroid levels and their clinical significance in the early neonatal age. Acta Physiol Hung 76: 151–158.
Tulchinsky D, Okada DM 1975 Hormones in human pregnancy: IV-plasma progesterone. Am J Obstet Gynecol 121: 293–299.
Smith OW 1948 Diethylstilbestrol in the prevention and treatment of complications of pregnancy. Am J Obstet Gynecol 56: 821–834.
Dalton K 1962 Controlled trials in the prophylactic value of progesterone in the treatment of preeclamptic toxaemia. J Obstet Gynaecol 69: 463–468.
Dalton K 1968 Ante-natal progesterone and intelligence. Br J Psychiatry 114: 1377–1382.
Dalton K 1976 Prenatal progesterone and educational attainments. Br J Psychiatry 129: 438–442.
Reinisch JM 1977 Prenatal exposure of human foetuses to synthetic progestin and oestrogen affects personality. Nature 266: 561–562.
Herbst A, Ulfelder H, Poskanzer D 1971 Adenocarcinoma of the vagina: Association of maternal stilbestrol therapy with tumor appearance in young women. N Engl J Med 284: 878–881.
Jones L, Bern H 1977 Long-term effects of neonatal treatment with progesterone, alone and in combination with estrogen, on the mammary gland and reproductive tract of female BALB/cfC3H mice. Cancer Res 37: 67–75.
Tapanainen J, Penttinen J, Huhtaniemi I 1979 Effect of progesterone treatment on the development and function of neonatal rat adrenals and testes. Biol Neonate 36: 290–297.
Warner M, Yau L, Rosen J 1980 Long term effects of perinatal injection of estrogen and progesterone on the morphological and biochemical development of the mammary gland. Endocrinology 106: 823–832.
Levine S, Mullins R 1964 Estrogen administered neonatally affects sexual behavior in male and female rats. Science 144: 185–187.
Wudy SA, Wachter UA, Homoki J, Teller WM 1995 17 alpha-hydroxyprogesterone, 4-androstenedione, and testosterone profiled by routine stable isotope dilution/gas chromatography-mass spectrometry in plasma of children. Pediatr Res 38: 76–80.
Acknowledgements
The authors thank M. Schulz (Endocrinological Laboratory, Department of Obstetrics and Gynecology, University of Ulm) and M. Hartman (Steroid Laboratory, Department of Pediatrics, University of Ulm) for excellent technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Trotter, A., Maier, L., Grill, HJ. et al. 17β-Estradiol and Progesterone Supplementation in Extremely Low-Birth-Weight Infants. Pediatr Res 45, 489–493 (1999). https://doi.org/10.1203/00006450-199904010-00006
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199904010-00006
This article is cited by
-
Viable bacterial colonization is highly limited in the human intestine in utero
Nature Medicine (2020)