Abstract
The hypoplastic lung in congenital diaphragmatic hernia (CDH) has both a quantitative and qualitative reduction in surfactant. Tumor necrosis factor-α (TNF-α) drastically decreases surfactant phospholipids synthesis by isolated human type II pneumocytes. Recently, it was shown that TNF-α mRNA expression is increased in human hypoplastic CDH lung. Antenatal glucocorticoid therapy demonstrates improved surfactant biochemical immaturity in an animal CDH model. The aim of this study was to investigate the effect of antenatal dexamethasone (Dex) on TNF-α protein and gene expression in nitrofen-induced CDH hypoplastic lung in rats. A CDH model was induced in pregnant rats after the administration of nitrofen on d 9.5 of gestation. Dex was given intraperitoneally on d 18.5 and 19.5. Cesarean section was performed on d 21. In situ hybridization was performed with a rat TNF-α-specific and digoxigenin-labeled oligonucleotide probe. TNF-α level was measured in solubilized lung tissue extracts by ELISA. In control lung, TNF-α mRNA expression was weak or absent. In contrast, strong TNF-α mRNA expression was demonstrated in type II pneumocytes and bronchiolar epithelium in CDH lung. In Dex-treated CDH lung, TNF-α mRNA expression was weak in both type II pneumocytes and the bronchiolar epithelium. The level of TNF-α was elevated significantly in CDH lung compared with levels in control lung extracts (p< 0.01). In Dex-treated CDH lung, TNF-α protein was significantly decreased compared with CDH lung (p< 0.05). Our findings suggest that the reduction in the local production of TNF-α may be one contributing mechanism by which antenatal glucocorticoid therapy improves pulmonary parenchymal immaturity, including surfactant.
Similar content being viewed by others
Main
Despite significant advances in neonatal resuscitation and intensive care, newborn infants with CDH still have a high mortality rate (1). In CDH, this high rate has been attributed to pulmonary hypoplasia and PPH (1). CDH lung is developmentally arrested in the canalicular or saccular stage of development (2). Structural and functional parenchymal immaturities have been demonstrated as the characteristics of hypoplastic CDH lung in many clinical reports and animal experiments (3, 4). They include the lack of adequate surfactant, poor compliance, thickened alveolar septa, and the association with hyaline membrane formation despite term gestation (3, 4).
TNF-α is a polypeptide that is a potent inhibitor of the biosynthesis of surfactant phospholipids. TNF-α is a principal mediator of cardiopulmonary shock and ARDS associated with invasive bacterial infection and reperfusion injury (5). TNF-α was increased in BAL and serum of patients with ARDS or sepsis syndrome (6, 7). Surfactant component composition and function were also disrupted in animal models and patients with ARDS. High doses of TNF-α supplementation on embryonic mouse lung promida diminished branching morphogenesis (8). Thus, elevated TNF-α is associated with disease complicated by surfactant dysfunction. A recent study from our laboratory for the first time reported that mRNA expression of TNF-α is markedly increased in human newborn and stillborn CDH hypoplastic lung, suggesting the important role of elevated pulmonary TNF-α in the development of CDH hypoplastic lung (9).
In vitro studies have demonstrated that the expression of TNF-α is suppressed by glucocorticoids at both protein and mRNA levels (10, 11). In experimental CDH models, antenatal glucocorticoid therapy improves structural and functional abnormalities in hypoplastic CDH lung, promoting parenchymal maturation (12, 13). The exact mechanism by which antenatal glucocorticoids treatment promotes parenchymal maturation in CDH hypoplastic lung is not fully understood. The aim of this study was to investigate the effect of antenatal glucocorticoid administration on TNF-α protein and mRNA expression in nitrofen-induced CDH hypoplastic lung in rats.
MATERIAL AND METHODS
Creation of CDH and protein extraction.
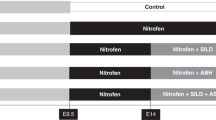
Adult Sprague-Dawley rats were bred after overnight controlled matings. Observation of positive smears was considered a proof of pregnancy; the day of observation was determined d 0. Water and food were supplied ad libitum. At d 9.5 of pregnancy (term = 22 d), a single dose consisting of 100 mg nitrofen (WAKO Chemical, Osaka, Japan) dissolved in olive oil was given via a stomach tube, under short anesthesia. Antenatal Dex therapy was administered 72 and 48 h before delivery' the lowest dose of dexamethasone (0.25 mg/kg intraperitoneally) was used on d 18.5 and 19.5 of gestation. Pregnancy was continued, and cesarean section was performed on d 21 of gestation. The animals were killed by intracardiac pentobarbital injection. To determine which litters had CDH, we opened the chest and abdomen of fetuses under the dissecting microscope. The fetuses were divided into three groups: group I, control (n= 12); group II, nitrofen-induced left CDH (n= 12); group III, nitrofen-induced left CDH with antenatal Dex treatment (n= 12). In control animals, the same dose of olive oil was given without nitrofen. The research project had been approved by the Department of Health, Ministry of Health, Ireland.
Tissues.
The fetuses were killed by cesarean section at term, and lungs were dissected out from the thoracic cavity under a dissecting microscope and fixed by intratracheal instillation of 4% paraformaldehyde at a water pressure of 20 cm. The dissected lung tissue was fixed in 4% paraformaldehyde solution for 24 h and cryopreserved; 8-μm cryosections were mounted on poly-L-lysine-coated glass slides for in situ hybridization. Protein content was extracted from each lung with commercially available TRIZOL reagent (Life Technologies, Paisley, United Kingdom), according to the recommended protocol. Briefly, each sample was homogenized by TRIZOL reagent and incubated in chloroform. After removal of supernatant, protein fraction was collected in ethanol. Precipitated protein in isopropyl alcohol was washed in a solution containing 0.3 M guanidine hydrochloride in 95% ethanol. Finally, the protein pellet was redissolved in 1% SDS.
In situ hybridization.
To perform in situ hybridization, we used rat TNF-α-specific oligonucleotide probe (Biogenostic, Gottingen, Germany), a method we have described previously (14). The probe was labeled by DIG, with a DIG oligonucleotide tailing kit (Boehringer Mannheim, Mannheim, Germany). The slides were placed in freshly mixed 0.25% acetic anhydride in 0.1 M triethanolamine HCl, pH 8.0, for 10 min at room temperature, and were treated with graded ethanol and chloroform. After tissue preparation, the sections were prehybridized with hybridization buffer. Then the slides were incubated with hybridization buffer in which rat TNF-α probe was diluted to 100 ng/mL. Sections were processed for immunologic detection using alkaline phosphatase-conjugated anti-DIG serum. Nitroblue tetrazolium salt and 5-bromo-4-chloro-3-indolyl phosphate toluidinium salt were used as substrate. At least 10 random fields of alveolar region were examined. The number of TNF-α mRNA-positive cells were graded independently by two of us (H.S. and T.O.), without knowledge of the animal group, as (−), no TNF-α mRNA-positive cells; (±). occasional; (+), moderate; and (++), many. If the grades were not identical, sections were regraded and a consensus reached.
ELISA.
Rat TNF-α expression was measured in protein content from solubilized lung tissue extracts by ELISA analysis. ELISA procedure was done according to the protocol of the rat TNF-α ELISA kit (Genzyme Diagnostic, Cambridge, MA). This kit is a solid-phase ELISA that uses the multiple antibody sandwich principle. Briefly, a capturing anti-TNF-α antibody was coated onto microwell strips, and samples were incubated in each well. Then HRP-conjugated anti-TNF-α was added to each well and the plate was incubated. Each sample was incubated in the substrate regent, which was added in each well. After incubation, the substrate reaction was stopped by the addition of 1 M sulfuric acid.
Absorbance of colored reaction product was read with an ELISA microplate reader at 450 nm. Concentrations of pulmonary TNF-α in samples were determined by relating absorbance value to values from a standard curve generated with recombinant rat TNF-α. Samples were assayed in duplicate by two operators to assess interassay precision. Soluble protein concentrations of each tissue extract were measured by BCA protein assay kit (Pierce, Rockford, IL). Values of TNF-α for soluble protein were expressed as μg TNF/g soluble protein.
For statistical evaluation, we used the nonparametric Mann-Whitney U test. Differences were considered significant when p< 0.05.
RESULTS
The results are summarized in Table 1.
In situ hybridization.
In control lung (group I), TNF-α mRNA expression was weak or absent in type II pneumocytes in mature lung parenchyma (Fig. 1a). In nitrofen-induced CDH lung (group II), abundant and strong TNF-α mRNA expression was demonstrated in type II pneumocytes and bronchiolar epithelium in immature lung parenchyma (Fig. 1b). In contrast, in nitrofen-induced CDH lung with antenatal Dex treatment (group III), TNF-α mRNA expression was markedly reduced in both type II pneumocytes and bronchiolar epithelium with an increase in air saccule size and thinning of septal walls (Fig. 1c). (C) Nitrofen-induced CDH lung with antenatal Dex treatment (group II). Weak and occasional TNF-α mRNA expression in type II pneumocytes with an increase in air saccule size and thinning of septal walls (×200). \.
ELISA.
TNF-α levels (TNF-α/soluble protein) were significantly elevated in group II (mean ± SD, 0.42 ± 0.11) compared with control lung extract (0.23 ± 0.08); (p< 0.01) (Fig. 2). In group III, TNF-α protein (0.28 ± 0.17) were significantly decreased compared with nitrofen-induced CDH lung extract (p< 0.05) (Fig. 2).
DISCUSSION
TNF-α, well-recognized as a proinflammatory cytokine, generated mainly by macrophages, is implicated in the pathogenesis of a variety of lung diseases, such as adult respiratory distress syndrome, neonatal RDS, and pulmonary fibrosis (15–18). It has been demonstrated that TNF-α is synthesized locally in lung and functions in an autocrine/paracrine mode (16, 18). This potent cytokine is reported to generate chemotactic factors, inflammatory mediators, and induce various changes in pulmonary tissue, vascular endothelium, and the surfactant system (19). It has recently been shown that TNF-α interferes with the synthesis of surfactant. A previous study from our laboratory demonstrated markedly increased TNF-α mRNA expression in human newborns and stillborns CDH hypoplastic lungs (9). It was suggested that the up-regulated pulmonary TNF-α gene expression may contribute to development of the surfactant deficiency, the decreased pulmonary compliance, and the persistent pulmonary hypertension observed in CDH hypoplastic lung. The present study confirmed our previous observations that hypoplastic lungs in nitrofen-induced CDH in rats demonstrated markedly increased TNF-α mRNA expression and TNF-α protein levels similar to those seen in human CDH hypoplastic lung.
CDH lung shows structural and functional parenchymal immaturity, as though it was developmentally arrested in the canalicular or saccular stage of development (2). Lung morphogenesis requires epithelial-mesenchymal interactions with precise regulatory controls (20). Specific hormones and growth factors have been implicated in this regulation (21–23). A recent study reported that TNF-α has a marked dose-dependent stimulatory effect on branching morphogenesis in the development of fetal lung (8). In contrast, with the higher concentration of TNF-α, TNF-α has a markedly inhibitory effect on branching morphogenesis in the developing lung (8). It has been shown that TNF-α is a potent inhibitor of the biosynthesis of surfactant phospholipids and proteins by isolated human type II pneumocytes (24). Over-production of pulmonary TNF-α in hypoplastic CDH lung may cause structural and functional parenchymal immaturity.
The present study demonstrated that antenatal dexamethasone treatment dramatically down-regulated TNF-α mRNA and protein levels in nitrofen-induced CDH hypoplastic lung in rat. Glucocorticoids are widely used in infants with RDS and result in improving pulmonary compliance, reduce alveolar proteinase activity, and frequently decrease the duration of ventilation and improve outcome (25). Over-expression of TNF-α has been implicated in the pathogenesis of ARDS, inducing the alterations in surfactant synthesis, composition, and function (7). Dexamethasone treatment has been shown to reduce the concentration of TNF-α in the bronchoalveolar secretions of patients with ARDS. Glucocorticoids influence numerous physiologic and pathologic processes. Glucocorticoids have been reported to have a wide range of effects on lung morphogenesis, promoting pulmonary maturation, type II pneumocyte histodifferentiation, and surfactant protein A expression (26, 27). Glucocorticoids enter the target cell primary by diffusion, interact with intracellular receptors, and then mediate their effects by regulation of specific genes or their products (28). There is a large body of evidence that glucocorticoids suppress TNF-α production (29). In vitro studies have demonstrated that dexamethasone will suppress the production of TNF-α in human and murine macrophages (30). It has been shown that glucocorticoids inhibit TNF-α at both the transcriptional and translational level by blocking gene transcription and mRNA mobilization (30). The therapeutic effects of glucocorticoid treatment in ARDS may be mediated by reduced production of pulmonary TNF-α (7). Histologic, morphologic, and quantitative biochemical similarities have been shown between the fetus/newborn with CDH and the surfactant-deficient newborn with RDS (3, 4). Recent studies demonstrated that antenatal glucocorticoid treatment in experimentally induced CDH hypoplastic lung results in an increase in air saccule size, thinning of septal walls, maturation of pulmonary parenchymal interstitium, acceleration of surfactant expression in type II cells, and increase in lung compliance, distensibility and functional residual capacity (12, 13, 31).
The precise mechanism by which antenatal glucocorticoids treatment promotes parenchymal maturation in CDH hypoplastic lung is not known. Steroidal growth of lung morphogenesis is mediated by regulating the effects of growth factors, cytokines, and their receptors (32). Our findings of barely detectable TNF-α mRNA expression and markedly reduced TNF-α protein levels in the dexamethasone-treated CDH lung suggest that the reduction of local TNF-α, which is up-regulated in CDH hypoplastic lung, may be one contributing mechanism by which antenatal glucocorticoid therapy improves lung parenchymal immaturity, including surfactant.
Abbreviations
- ARDS:
-
adult respiratory distress syndrome
- BAL:
-
bronchoalveolar lavage
- CDH:
-
congenital diaphragmatic hernia
- Dex:
-
dexamethasone
- DIG:
-
digoxigenin
- PPH:
-
persistent pulmonary hypertension
- RDS:
-
respiratory distress syndrome
- TNF-α:
-
tumor necrosis factor-α
References
Puri P 1994 Congenital diaphragmatic hernia. Curr Prob Surg 31: 785–859
George DK, Cooney TP, Chiu BK, Thurlbeck WM 1987 Hypoplasia and immaturity of the terminal lung unit (acinus) in congenital diaphragmatic hernia. Am Rev Respir Dis 136: 947–950
Wilcox DT, Irish MS, Holm BA, Glick PL 1996 Pulmonary parenchymal abnormalities in congenital diaphragmatic hernia. Clin Perinatol 23: 771–779
Buckburn WR, Logsdon P, Alexander JA 1977 Congenital diaphragmatic hernia: studies of lung composition and structure. Am Rev Respir Dis 115: 275
Alegre M, Depierreux M, Florquin S, Najdovski T, Vandenabeele P, Abramowicz D, Leo O, Deschodt-Lancman M, Goldman M 1990 Acute toxicity of anti CD3 monoclonal antibody in mice: a model for OKT3 first dose reactions. Transpl Proc 22: 1920–1921
Hyers TM, Tricomi SM, Dettenmeier PA, Fower AA 1991 Tumour necrosis factor levels in serum and bronchoalveolar lavage fluid of patients with the adult respiratory distress syndrome. Am Rev Respir Dis 144: 268–271
Suter PM, Suter S, Girardin E, Roux LP, Grau GE, Dayer JM 1992 High bronchoalveolar levels of tumour necrosis factor and its inhibitors, interleukin-1, interferon, and elastase, in patients with adult respiratory distress syndrome after trauma, shock, or sepsis. Am Rev Respir Dis 145: 1016–1022
Jaskoll T, Boyer PD, Melnick M 1994 Tumor necrosis factor-α and embryonic mouse lung morphogenesis. Dev Dynam 201: 137–150
Ohshiro K, Miyazaki E, Taira Y, Puri P 1998 Upregulated TNF-α gene expression in hypoplastic lung in patients with congenital diaphragmatic hernia. Pediatr Surg Int 14: 21–24
Waage A 1987 Production and clearance of tumor necrosis factor in rats exposed to endotoxin and dexamethasone. Clin Immunol Immunopathol 45: 348–355
Ledda-Columbano GM, Columbano A, Cannas A, Simbula G, Okita K, Kayano K, Kubo Y, Katyal SL, Sinozuka H 1994 Dexamethasone inhibits induction of liver tumor necrosis factor-α mRNA and liver growth induced by lead nitrate and ethylene dibromide. Am J Pathol 145: 951–958
Suen HC, Bloch KD, Donahoe P 1994 Antenatal glucocorticoid corrects pulmonary immaturity in experimentally induced congenital diaphragmatic hernia in rats. Pediatr Res 35: 523–529
Suen HC, Losty PD, Donahoe PK, Schnitzer JI 1994 Combined antenatal thyrotropin-releasing hormone and low-dose glucocorticoid therapy improves the pulmonary biochemical immaturity in congenital diaphragmatic hernia. J Pediatr Surg 29: 359–362
Ohshiro K, Puri P 1998 Increased insulin-like growth factor-I mRNA expression in pyloric muscle in infantile hypertrophic pyloric stenosis. Pediatr Surg Int 13: 253–255
Old LJ 1985 Tumor necrosis factor (TNF). Science 230: 630–632
Millar AB, Foley NM, Singer M, Johnson NM, Mearger A, Rook GA 1989 Tumor necrosis factor in bronchopulmonary secretions of patients with adult respiratory distress syndrome. Lancet 2: 712–714
Murch SH, McDonald TT, Wood CB, Costeloe KL 1992 Tumor necrosis factor in the bronchoalveolar secretions of infants with the respiratory distress syndrome and the effect of dexamethasone treatment. Thorax 47: 44–47
Piguet PF, Ribaux C, Karpuz V, Grau GE, Kapanci Y 1993 Expression and localization of tumor necrosis factor-α and its mRNA in idiopathic pulmonary fibrosis. Am J Pathol 143: 651–655
Baur FM, Brenner B, Goetze-Speer B, Neu S, Speer CP 1998 Natural porcine surfactant (curosurf) down-regulated mRNA of tumor necrosis factor-α (TNF-α) and TNF-α type II receptor in lipopolysaccharide-stimulated monocytes. Pediatr Res 44: 32–36
Canigga I, Tesu I, Han RN, Smith BT, Tanswell K, Post M 1991 Spatial and temporal differences in fibroblast behavior in fetal rat lung. Am J Physiol 261:L424–433
Deterding RR, Shannon JM 1995 Proliferation and differentiation of fatal rat pulmonary epithelium in the absence of mesenchyme. J Clin Invest 95: 2963–2972
Nogawa H, Ito T 1995 Branching morphogenesis of embryonic mouse lung epithelium in mesenchyme-free culture. Development 121: 1015–1022
Whisett JA, Zhou L 1996 Use of transgenic mice to study autocrine-paracrine signal in lung morphogenesis and differentiation. Clin Perinatol 23: 753–768
Balibrea-Cantero JL, Arias-Diaz J, Garcia C, Torres-Melero J, Simon C, Rodriguez JM, Vara E 1994 Effect of pentoxifylline on the inhibition of surfactant synthesis induced by TNF-α in human type II pneumocytes. Am J Respir Crit Care Med 149: 699–706
Gladstone IM, Ehrenkranz RA, Jacobs HC 1989 Pulmonary function tests and fluid balance in neonates with chronic lung disease during dexamethasone treatment. Pediatrics 84: 1072–6
Jaskoll T, Choy HA, Melnick M 1996 The glucocorticoid-glucocorticoid receptor signal transduction pathway, transforming growth factor-α, and embryonic mouse lung development in vivo. Pediatr Res 39: 749–759
Ballard PL 1989 Hormonal regulation of pulmonary surfactant. Endocr Rev 10: 165–181
Gustafsson JA, Carlatedt-Duke J, Poelinger L, Okret S, Wikstrom AC, Bronnegard M, Gillner M, Dong Y, Fuxe K, Cintra A 1987 Biochemistry, molecular biology, and physiology of the glucocorticoid receptor. Endocr Rev 8: 185–234
Beutler B, Krochin N, Milsark IW, Leudke C, Cerami A 1986 Control of cachectin (tumor necrosis factor) synthesis: mechanisms of endotoxin resistance. Science 232: 977–980
Beutler B, Cerami A 1986 Cachectin and tumor necrosis factor as two sides of the same biological coin. Nature 320: 584–588
Losty PD, Suen HC, Manganaro TF, Donahoe PK, Schnitzer JJ 1995 Prenatal hormonal therapy improves pulmonary compliance in the nitrofen-induced CDH rat model. J Pediatr Surg 30: 420–426
Melnick M, Choy HA, Jaskoll T 1996 Glucocorticoids, tumor necrosis factor-α, and epidermal growth factor regulation of pulmonary morphogenesis: a multivariate in vitro analysis of their related actions. Dev Dynam 205: 365–378
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Shima, H., Ohshiro, K., Taira, Y. et al. Antenatal Dexamethasone Suppresses Tumor Necrosis Factor-α Expression in Hypoplastic Lung in Nitrofen-Induced Diaphragmatic Hernia in Rats. Pediatr Res 46, 633 (1999). https://doi.org/10.1203/00006450-199911000-00023
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199911000-00023
This article is cited by
-
Anti-inflammatory effects of antenatal administration of stem cell derived extracellular vesicles in the brain of rat fetuses with congenital diaphragmatic hernia
Pediatric Surgery International (2023)
-
Emerging antenatal therapies for congenital diaphragmatic hernia-induced pulmonary hypertension in preclinical models
Pediatric Research (2021)
-
Pulmonary hypertension secondary to congenital diaphragmatic hernia: factors and pathways involved in pulmonary vascular remodeling
Pediatric Research (2019)
-
Assessment of the nitrofen model of congenital diaphragmatic hernia and of the dysregulated factors involved in pulmonary hypoplasia
Pediatric Surgery International (2019)
-
Congenital diaphragmatic hernia: a systematic review and summary of best-evidence practice strategies
Journal of Perinatology (2007)