Abstract
We tested the hypothesis that a reduced ability of the newborn (1–2 d old) to autoregulate cerebral blood flow (CBF) during acute hypertension is contributed by an increased synthesis of nitric oxide (NO) from endothelial (e) and neuronal NO synthase (nNOS). As previously reported, CBF (measured by radiolabeled microsphere technique) in newborn pigs remained constant only between 50 and 90 mm Hg of mean arterial blood pressure. Treatment of newborn pigs with Nω-monomethyl-L-arginine or specific nNOS inhibitors 7-nitroindazole monosodium, 3-bromo-7-nitroindazole, and 1-(2-trifluoromethylphenyl) imidazole extended the upper limit of CBF autoregulation as seen in saline-treated (control) juvenile (4–6-wk-old) animals. Cerebrovascular production of nitrite (stable NO oxidation product) in vivo was markedly increased during hypertension (mean arterial blood pressure >90 mm Hg) in newborn but not in the juvenile pigs. Inhibition of NOS with Nω-monomethyl-L-arginine, 7-nitroindazole monosodium, 3-bromo-7-nitroindazole, or 1-(2-trifluoromethylphenyl) imidazole prevented the hypertension-induced increase in nitrite levels. In addition, eNOS and nNOS protein expression and activity were 2- to 3-fold higher (p< 0.05) in the cerebral microvasculature of newborn than in the tissues of juvenile pigs. It is concluded that during acute hypertension, excess production of NO associated with increased activity of NOS curtails the upper limit of CBF autoregulation in the newborn subject; in addition, nNOS seems to serve a significant role in this important physiologic function.
Similar content being viewed by others
Main
CBF autoregulation is an important hemodynamic physiologic function. CBF response to acute changes in perfusion pressure is mainly governed by the microvasculature (<150-μm diameter) (1). The caliber of these resistance vessels adjusts to responses in fluctuations in perfusion pressure to maintain CBF constant; this intrinsic mechanism is referred to as autoregulation (2). CBF is autoregulated over a relatively narrower range of mean perfusion pressure (50–90 mm Hg) in the newborn than in the adult (50–150 mm Hg) (2–9). CBF can remain constant at high perfusion pressure provided the resistance vessels respond by adequate constriction to prevent an increase in blood flow.
PG have been found to play an important role in CBF autoregulation in the newborn (4, 10), partly because the constrictor PG are relatively ineffective in the newborn (11, 12) and mostly because the types of PG active in the newborn are mainly relaxants (11). Further, PG have been found to exert relaxation largely via NO in the newborn (13, 14) as well as to positively regulate NO production (15, 16). However, the role of NO on CBF autoregulation, particularly in the newborn, remains to be established.
It has been suggested that NO plays an important role on hypotension-induced vasorelaxation in adult rodents (17–19); this has not been confirmed in other species such as dogs and monkeys (20–22). Likewise, in the normoxemic perinate, this effect of NO is not apparent (23, 24). On the other hand, the involvement of NO on hypertension-induced vasomotor control is mostly unclear in the adult, largely because it has been studied within the normal range of CBF autoregulation (17, 20, 25), whereas in the newborn, it is unknown. Because NO is a potent vasodilator and can interfere with vasoconstrictor response of microvessels during increases in MABP and because NOS is developmentally regulated and generally found to be increased in the perinate (26–29), it is possible that NO contributes to the reduced upper perfusion pressure limit of CBF autoregulation.
NO synthesis is catalyzed by two classes of NOS identified as calcium-dependent constitutive NOS (cNOS) and calcium-independent inducible NOS (iNOS) (30–32). There are two isoforms of cNOS designated as endothelial (e) NOS and neuronal (n) NOS (31, 33). The cerebral vasculature contains both isoforms of cNOS; eNOS is present in endothelial cells (31), and nNOS in axon terminals of parenchymal neurons that are closely associated with microvessels (34–36), perivascular nerves (33, 35, 37, 38), and glial cells (39). A significant involvement of eNOS in basal cerebral microvascular tone has been suggested (40, 41). However, whether or not nNOS plays a role in autoregulatory cerebrovascular control is not clearly known (42). The present study was undertaken to test the hypothesis that a decrease in the vasodilator NO generated during acute hypertension might enhance CBF autoregulation in the newborn, and, in this process, the role of nNOS was also investigated. Our findings support the working hypothesis and disclose a significant role for nNOS in CBF autoregulation of the newborn.
METHODS
Animals.
Newborn (1–2-d-old) and juvenile (4–6-wk-old) pigs were used in the present study according to a protocol of the Ste-Justine Hospital Research Center Animal Care Committee. The animals were maintained at the Research Center at 25°C, 50–70% humidity, and a 12:12-h light-dark cycle (lights on 0700–1900 h), and fed ad libitum milk (newborn) or pig chow and tap water (juvenile pigs).
Surgical preparation for CBF studies.
Animals were anesthetized with 2% halothane and prepared for blood flow studies as previously described (10, 43). Briefly, tracheostomy was performed, and catheters were placed into the left subclavian artery for the withdrawal of blood samples, including reference samples, into the left ventricle through the right subclavian artery for the injection of radiolabeled microspheres, and into the femoral artery for continuous BP recording with a pressure transducer (Statham, Glen Burnie, MD) connected to a multichannel recorder (TA240 Gould, Valley View, OH). A silicone-coated balloon-tipped catheter was placed in the distal thoracic descending aorta via a femoral artery; inflation of this balloon produced hypertension in the aortic arch. A second balloon-tipped catheter was placed at the root of the aorta via the right common carotid artery, and its inflation produced hypotension in the aortic arch. A small polyethylene catheter (Intramedic PE-50, Becton Dickinson, Parsipany, NJ) was placed in the sagittal sinus via a small burr hole in the skull for blood sampling. Halothane was discontinued after surgery; animals were then maintained on α-chloralose (50 mg/kg bolus injection followed by infusion of 5 mg·kg−1·h−1) and paralyzed with pancuronium (0.1 mg/kg i.v.). The doses used for α-chloralose and pancuronium have been shown not to alter autoregulation of CBF in newborn pigs (44–46). Body temperature was maintained at 38°C with an overhead radiant lamp, and the animals were allowed to recover from the surgery for 2 h before the experiments were begun.
Measurements of CBF.
For CBF measurements, ∼106 microspheres (15-μm diameter) labeled with 141Ce, 95Nb, 46Sc, or 113Sn were injected in a random sequence into the left ventricle. Withdrawal of reference blood samples from the left subclavian artery catheter was started 10 s before the injection of each type of microspheres and was continued for 70 s at a rate of 2 mL/min using a Harvard infusion-withdrawal pump. Immediately after each injection of microspheres, blood samples were withdrawn from the left subclavian artery to determine blood gases, O2 content (ABL 300; Radiometer, Copenhagen, Denmark), and Hb concentration; these remained within normal limits. After the experiment, animals were killed with excess pentobarbital sodium, the location of catheters was verified, and the brains were removed. The brain was weighed, and the cortex, the periventricular area, and the brain stem were separated. Radioactivity in the cortex, periventricular region, brain stem, and reference blood samples was counted in a gamma scintillation counter (Cobra II; Canberra Packard, Meridien, CT). Regional CBF (mL·min−1·100 g−1) was calculated as (cpm/100 g tissue × reference blood withdrawal rate)/(cpm in the reference blood sample) using the computer system online with the counter (PCGERDA, Charlottesville, VA); cerebral vascular resistance was derived as MABP/CBF.
The range of CBF autoregulation in newborn pigs was studied using procedures we have described in detail (10, 47, 48). Basal CBF was measured 1 h after the injections of the drugs, and, 10 min later, one of the two balloon-tipped catheters was inflated to produce hypotension or hypertension. After a steady state MABP was achieved (within 30 to 40 s of balloon inflation), CBF was determined again as described above. The balloons were deflated after the blood flow measurements, and the animals were allowed to recover for 40 min. At the end of this recovery period, a second baseline CBF was measured, and, 10 min later, final measurement of CBF was made after inflating the other balloon-tipped catheter. Hence, each animal was subjected to one hypotensive and one hypertensive episode in a random order; for each treatment group of animals, MABP was scaled at intervals of 5 ± 1.5 mm Hg to cover a range of 13 to 157 mm Hg.
Further, to specifically study the upper limit of CBF autoregulation, CBF was measured in separate animals at preselected MABP values at and above the upper limit of the CBF autoregulation range of the newborn pig as previously reported (45, 49). For this purpose, CBF was measured in each animal after steady state MABP of 90, 105, 125 mm Hg was reached, and at time intervals (30 min) sufficient for recovery of CBF to baseline (10, 47).
Administration of NOS inhibitors.
Newborn pigs were randomly assigned to receive intravenous saline (1.5 mL;n= 13) or one of the following NOS inhibitors at a dose of 1 mg/kg followed by infusion of 50 μg·kg−1·min−1: nonselective NOS inhibitor L-NMMA (n= 13) (43) and relatively selective nNOS inhibitors 7-NINA (n= 3) (50, 51), 3-bromo-7-nitroindazole (n= 3) (52), and TRIM (n= 3) (53); dose used corresponded to NOS inhibitory activities (43, 50–54).
Measurements of plasma nitrite levels and cerebrovascular nitriteproduction in vivo.
Cerebrovascular production of NO was estimated by determination of nitrite (NO2−, stable oxidation product of NO) (55, 56) on simultaneously withdrawn arterial and sagittal sinus blood. In vivo cerebrovascular production of NO2− was calculated as the difference in NO2− concentrations of sagittal sinus and arterial blood × total CBF, expressed in ng·min−1·100 g−1 tissue, as we previously reported for other factors (47, 57).
Arterial and sagittal venous blood (1.5 mL) from newborn and juvenile pigs was collected in ice-cold polypropylene tubes containing 0.1 mM EDTA, 10 μM indomethacin, and 1 mM Nω-nitro-L-arginine (L-NNA). The blood was immediately centrifuged at 2450 ×g for 15 min at 4°C. The plasma was collected and stored at −70°C until NO2− measurement (56). Plasma samples were diluted 4-fold with distilled water containing nitrate reductase (200 U/L), flavin adenine dinucleotide (FAD) (5 μM), and NADPH (50 μM). Samples were subsequently incubated for 20 min at 37°C and then mixed with lactate dehydrogenase and sodium pyruvate to achieve a final concentration of 10 mM of both agents. Samples were further incubated for 5 min at 37°C to oxidize NADPH. Thereafter, samples were deproteinized with zinc sulfate (1 mM) spun at 10 000 ×g for 10 min at 20°C to remove proteins. The supernatant was recovered, and the Griess reagent containing 200 μL of 1% sulfanilamide in 5% phosphoric acid and 200 μL of 0.1%N-(1-naphthyl)ethylenediamine HCl was then added. After incubation of samples for 10 min at 20°C, the absorbance was recorded at 540 nm (Beckman DU-600 spectrophotometer). Standard curves were obtained with NaNO2 and had an interassay variability of <5%.
Preparation of microvessels.
Brain microvessels composed predominantly of small arterioles and capillaries were isolated as described (12, 49, 58). All procedures were performed at 4°C. Briefly, brain tissues from newborn and juvenile pigs (n= 4 for each) were gently homogenized with a Wheaton pestle in 5 mM Tris-HCl buffer (pH 7.4) containing 1.1 mM acetylsalicylic acid (ASA), 0.5 mM EGTA, 1 mM benzamidine, 0.1 mM phenylmethylsulfonyl fluoride (PMSF), and 5 μM soybean trypsin inhibitor. The homogenate was mixed with Ficoll 400 at a 1:1 vol/vol and centrifuged at 20 000 ×g for 20 min. The pellet, which contained the microvessels, was washed in the above buffer three times and subsequently filtered through a 150-μm filter. The filtrate fraction containing microvessels was retained, and the residue on the filter was discarded. The filtrate fraction was centrifuged at 1000 ×g for 15 min and stored at −80°C until assayed. The morphology and purity of microvessels were monitored by light microscopy and enrichment of γ-glutamyl transpeptidase (γ-GT) activity (59, 60). The activity of γ-GT was greater in the microvessels (5.6–5.9 mU/mg protein) than in brain parenchyma (0.30–0.35 mU/mg protein).
Western blotting.
Western blotting for eNOS and nNOS was performed using a method previously described (16, 57). Purified microvessels from newborn and juvenile brains were homogenized in ice-cold buffer (20 mM Tris-HCl, pH 8.0, 1 mM EDTA, 137 mM NaCl, 1% Nonidet P-40, 20 μM leupeptin, 15 μM pepstatin, 0.5 μM soybean trypsin inhibitor, 0.2 mM PMSF) with an Omni tissue grinder for 15–20 s; whole tissue lysates were obtained after centrifugation at 15 000 ×g for 10 min. Whole tissue lysates were used because nNOS is contained in both membrane and cytosolic fractions (61). Protein content was determined by the Bio-Rad dye-binding assay using BSA as the standard. After the addition of β-mercaptoethanol to aliquots of homogenates (100 μg protein) to a final concentration of 10%, the samples were denatured by boiling for 5 min and resolved by electrophoresis on an 8% SDS-polyacrylamide gel. Transfer of proteins to membranes and immunoblotting using antibodies (1:2000) against eNOS and nNOS were conducted exactly as previously described (16, 57). Immunoreactive bands were visualized by chemiluminescence (Amersham, Canada) as recommended by the supplier.
Brain microvessel NOS activity.
NOS activity was assayed by determining the conversion of L-arginine to L-citrulline (16, 62). In brief, microvessels were homogenized in 5 mL of ice-cold homogenization buffer (50 mM Tris-HCl, pH 7.5, 1 mM EDTA, 1 mM 1,4-DTT, 5 mM glucose, 1 mM PMSF, 3 μM aprotinin, 40 mM leupeptin, 1 mM soybean trypsin inhibitor). The homogenate was centrifuged at 12 000 ×g for 15 min, and the protein content of the supernatant was determined by the dye-binding method. An aliquot of the supernatant (100–200 μg protein) was incubated in the absence or the presence of the NOS inhibitor L-NNA (1 mM) or the selective nNOS inhibitor 7-nitroindazole (100 μM) in incubation buffer (in mM: HEPES, 50, pH 7.5; 1,4-DTT, 1; EDTA, 1; CaCl2, 1.25) with 0.1 mM L-arginine [containing 1 μCi L-[3H]arginine (91 Ci/mmol specific activity)], 1 mM NADPH, 15 μM (6R)-tetrahydrobiopterin, 1 μM FAD, and 1 μM calmodulin for 10 min at 37°C. The reaction was terminated by addition of 1 mL ice-cold 100 mM HEPES buffer (pH 5.5) containing 10 mM EGTA and 500 mg Dowex AG-50W-X8 cation exchange resin and immediately centrifuged at 10 000 ×g for 20 min. Radioactivity in the L-[3H]citrulline–containing supernatant was counted. Total NOS and nNOS activities were measured, respectively, from the L-NNA– and 7-nitroindazole–sensitive production of L-[3H]citrulline. iNOS activity was determined by adding EGTA (10 mM) to the incubation buffer. cNOS activity was obtained by subtracting iNOS activity from total L-NNA–sensitive NOS activity. 7-Nitroindazole–sensitive NOS activity was measured as total NOS activity minus that after addition of 7-nitroindazole (16).
Chemicals.
The following products were purchased: L-NMMA, L-NNA, soybean trypsin inhibitor (type II-S), PMSF, β-mercaptoethanol, 1,4-DTT, HEPES, EDTA, EGTA, L-arginine, nitrate reductase, NADPH, FAD, lactate dehydrogenase, sodium pyruvate, zinc sulfate, and (6R)-tetrahydrobiopterin (Sigma Chemical Co.-Aldrich, Oakville, Ontario); 7-NINA, 3-bromo-7-nitroindazole, and TRIM (Tocris Cookson, Ballwin, MO); radiolabeled microspheres (DuPont-NEN, Boston, MA); polyclonal anti-nNOS and anti-eNOS rabbit antibodies (Calbiochem, San Diego, CA); Dowex AG-50W-X8 resin, protein assay, and electrophoretic reagents (Bio-Rad, Mississauga, Ontario); enhanced chemiluminescence kit and L-[3H]arginine (Amersham, Mississauga, Ontario); pepstatin and leupeptin (Boehringer-Mannheim, Montreal, Quebec); Ficoll (Pharmacia, Baie D'urfé, Quebec); all other chemicals (Fisher, Montreal, Quebec).
Statistics.
CBF data were analyzed by regression analysis, as previously described in detail (43). The Pearson product moment coefficient (r) and the Kendall coefficient of rank correlation (τ) were calculated. The best fit line for the relationship between blood flow and perfusion pressure was determined by using the method of least squares of a polynomial regression analysis and by calculating the coefficient of determination (R2) (43). In addition, the relationship of blood flow to perfusion pressure was examined by the method of Lowess smoothing, and, based on these curves, separate linear regressions were performed using the random effects model for longitudinal data. Linear regressions were compared by regression equality test using the method of least squares. Other data were analyzed by ANOVA, factoring for treatment and age group, and by a comparison among means test (Tukey-Kramer method) and t test. Statistical significance was set at p< 0.05.
RESULTS
Stability of preparations.
Arterial pH, PO2, and PCO2 remained stable throughout the course of the experiments (Table 1 ]). CBF did not differ between the first and second baselines. L-NMMA caused an expected increase in resting MABP (41). 7-NINA, 3-bromo-7-nitroindazole, and TRIM did not affect resting MABP.
Effects of L-NMMA on CBF autoregulation.
CBF plotted as a function of MABP is shown for the cortex (Fig. 1A), periventricular area (Fig. 1B), and brain stem (Fig. 1C). In saline-treated animals, cortical, periventricular, and brain stem CBF autoregulation ranged from 50 to 90 mm Hg of MABP (r= 0.23 to 0.47, p> 0.1, based on polynomial and Lowess curves), beyond which CBF varied with MABP (τ = 0.41–0.57, p< 0.01;Fig. 1). Treatment with L-NMMA significantly broadened the range of CBF autoregulation [from 50 to 157 mm Hg (the maximum MABP studied)] by extending the upper limit; L-NMMA did not significantly affect CBF when MABP was reduced below 50 mm Hg (Fig. 1). L-NMMA slightly but significantly reduced resting cortical, periventricular, and brain stem CBF by 16 ± 5% compared with saline-treated animals (Table 1).
Effects of L-NMMA on blood flow to the cortex (A), periventricular region (B), and brain stem (C) as a function of MABP in newborn pigs. Animals were injected with saline (n= 8) or L-NMMA (1 mg/kg followed by 50 μg·kg−1·min−1;n= 8). Each animal was subjected to one hypotensive and one hypertensive episode, so animals were studied over MABP range of 13 to 157 mm Hg. In saline-treated animals, the best fit regression was a 3rd-order polynomial function for cortical, periventricular, and brain stem blood flow (R2 = 0.95–0.99, p< 0.001). In L-NMMA–treated pigs, 2nd-order polynomial regression fitted best the points for cortical blood flow (R2 = 0.89, p< 0.001) and 3rd-order polynomial regression for periventricular and brain stem blood flow (R2 = 0.85–0.90, p< 0.001).
In accordance with CBF data, cortical, periventricular, and brain stem vascular resistance correlated linearly with BP between 50 and 90 mm Hg in both saline- and L-NMMA–treated animals (r= 0.49–0.80, p< 0.05). Above an MABP of 90 mm Hg, cerebral vascular resistance was unrelated to MABP in saline-treated newborn animals (r= −0.24–0.02, p> 0.85), whereas it continued to increase linearly with MABP in L-NMMA–treated pigs (r= 0.83–0.98, p< 0.001).
Effects of L-NMMA, 7-NINA, 3-bromo-7-nitroindazole, andTRIM on the upper limit of CBF autoregulation.
Because nonselective NOS inhibition using L-NMMA affected mostly the upper limit of CBF autoregulation (Fig. 1), we focused on the latter. Likewise, since periventricular and brain stem blood flow changes paralleled those in the cortex, results are only presented for the cortex. In the saline-treated newborn pigs, CBF increased linearly with MABP >85 mm Hg (r= 0.59–0.88, p< 0.01) (Fig. 2). L-NMMA, 7-NINA, 3-bromo-7-nitroindazole, and TRIM prevented the change in CBF as a function of MABP (L-NMMA, r= 0.26–0.39, p≥ 0.1; 7-NINA, r= 0.11–0.2, p≥ 0.1; 3-bromo-7-nitroindazole, r= 0.10–0.18, p> 0.5; TRIM, r= 0.19–0.34, p> 0.5), as seen in juvenile pigs (r= 0.23–0.35, p> 0.5). Regressions for saline-treated newborn animals differed significantly from those treated with L-NMMA, 7-NINA, 3-bromo-7-nitroindazole, and TRIM and from juvenile (saline-treated) pigs (p< 0.05, by regression equality test); no difference in regression was noted among newborn animals treated with NOS inhibitors and juvenile (saline-treated) pigs (p> 0.2). Accordingly, the percent change in CBF secondary to increasing MABP from \F90 to 125 mm Hg was significantly greater in newborn saline-treated pigs (38–45%) than in those treated with L-NMMA, 7-NINA, 3-bromo-7-nitroindazole, or TRIM (1–9%) (p< 0.01). Consequently, the changes in cerebral vascular resistance were higher in newborns treated with L-NMMA, 7-NINA, 3-bromo-7-nitroindazole, and TRIM (15–31%) than in those treated with saline (1–5%) (p< 0.01).
Cortical CBF as a function of increased MABP in newborn (A–E) and juvenile pigs (F). Newborn animals were treated intravenously with 1 mg/kg bolus followed by 50 μg·kg−1·min−1 of one of the following agents: saline (n= 5), L-NMMA (n= 5), 7-NINA (n= 3), 3-bromo-7-nitroindazole (n= 3), and TRIM (n= 3); juvenile pigs received only saline (n= 3). Each animal was subjected to stepwise acute increases in MABP aiming at approximately 90, 105, and 125 mm Hg (set values for each animal differed by <6 mm Hg). The faint lines correspond to the regressions for individual animals, and the thick lines represent the mean regressions for all animals in the group. In saline-treated newborn animals, CBF increased linearly with MABP (r= 0.73–0.86, p< 0.01); symbols not seen are included within other symbols. In animals treated with L-NMMA, 7-NINA, 3-bromo-7-nitroindazole, or TRIM as well as in juvenile (saline-treated) pigs, CBF did not change as a function of MABP (r= 0.07–0.35, p≥ 0.2); regressions for saline-treated newborn pigs differed from all those treated (p< 0.05, by regression equality test).
Effects of NOS inhibitors on cerebrovascular production ofNO2−in vivo.
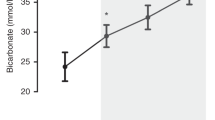
Basal cerebrovascular NO2− production was higher in newborn than in juvenile animals. During hypertension (MABP = 125 ± 6 mm Hg), NO2− production increased 4- to 5-fold in the newborn but changed only minimally in juvenile pigs (Fig. 3). The basal NO2− production was reduced by all NOS inhibitors to approach values in juvenile pigs, albeit the effects of the nonselective NOS inhibitor L-NMMA were greater than that of nNOS selective inhibitors. All NOS inhibitors blocked the increase in NO2− levels induced by hypertension (Fig. 3).
Cerebrovascular production of NO2−in vivo during normotension (70 ± 5 mm Hg) and hypertension (125 ± 6 mm Hg) in newborn and juvenile pigs. L-NMMA, 7-NINA, 3-bromo-7-nitroindazole, and TRIM were infused for 1 h at a dose of 1 mg/kg bolus followed by 50 μg·kg−1·min−1 before blood samples were collected. The production of NO2− was calculated as the product of total CBF × the difference in NO2− concentration in sagittal sinus and arterial blood, and expressed as ng·min−1·100 g−1 brain tissue. Values are mean ± SEM of three animals. *p< 0.05 compared with corresponding value during normotension. †p< 0.05 compared with corresponding values in saline-treated newborn pigs.
nNOS and eNOS protein expression and activities in cerebralmicrovessels.
cNOS accounted for >95% of all NOS activity in the cerebral microvasculature of both newborn and juvenile animals; of that, nNOS accounted for \F40% of the cNOS and the remainder was thus assumed by eNOS (Fig. 4). Both nNOS and eNOS activities and immunoreactive proteins were 2- to 3-fold greater in microvessels of newborn than of juvenile pigs.
nNOS and eNOS activities and immunoreactivity in newborn and juvenile pig cerebral microvessels. (A) Arrow points to the nNOS 155-kD protein, the only immunoreactive band detected in the range of interest, 100–165 kD. (B) Arrow points to the eNOS 140-kD protein, the only immunoreactive band detected in the range of interest, 100–165 kD;large bands at bottom of gel photograph are immunoglobulins of the immunoprecipitate. (A) and (B) are typical representations of four experiments, each using 100 μg protein loading. (C) cNOS and nNOS activities in cerebral microvessels of newborn and juvenile pig. Data are mean ± SEM of four separate experiments, each performed in duplicate in tissues from different animals; *p< 0.05 compared with corresponding values for juvenile pigs.
DISCUSSION
CBF is autoregulated over a much narrower upper range of MABP in the newborn than in adults (3–10). Because NO is a potent vasorelaxant and a role for NO in CBF autoregulation has been debated in adults (17–21, 25), we tested the hypothesis that increased NO production during the neonatal period may contribute to restrict the range of CBF autoregulation in the newborn when perfusion pressure is increased. Correspondingly, inhibition of NOS should increase the upper MABP range for CBF autoregulation in the newborn. Data of this study support the hypothesis. NOS activity was higher in the cerebral vasculature of the newborn than of the juvenile pig, and its reduction of NOS activity in newborns resulted in enhanced CBF autoregulation, as observed in older animals.
A significant role for NO in reducing the upper limit of CBF autoregulation of the newborn was indicated by numerous observations:1) increased hypertension-induced cerebrovascular formation of NO2− in the newborn (Fig. 3); 2) higher expression and activities of cNOS in the cerebral vasculature of the newborn than in that of older animals (Fig. 4), consistent with previous reports on this subject (26–29); and, most convincingly, 3) extension of the upper limit of CBF autoregulation by nonselective as well as selective nNOS inhibitors (Figs. 1 and 2), which reduce basal NO2− production to values that approach those of older animals (Fig. 3). Hence, increased relaxation induced by relatively excessive NO production in the newborn overcomes an otherwise apparently adequate hypertension-induced cerebral vasoconstriction, as reflected by changes in CBF and corresponding cerebral vascular resistance in the absence and presence of NOS inhibitors (Figs. 1 and 2). However, although the evidence presented in this study clearly points to a significant role for increased NO generation on the narrow range of CBF autoregulation in the newborn, one cannot exclude a contribution by ontogenic changes in mechanotransduction-NO coupling, as evidenced from a minimal hypertension-induced NO2− increase in juveniles compared with newborns (Fig. 3).
Shear stress–induced activation of cNOS is well described (63). A role for eNOS on basal CBF has also been suggested (63–68). On the other hand, a major feature of this study is the role of nNOS in CBF autoregulation. The use of various distinct nNOS inhibitors (50, 52, 53) reduced to an equivalent degree cerebrovascular NO2− production (Fig. 3) and enhanced similarly CBF autoregulation in the newborn (Fig. 2). A number of observations by others support our findings. Indeed, diaphorase-positive neural processes that can presumably release NO to affect vasomotor tone innervate cerebral arterioles (mostly larger ones) (35, 36). Stimulation of arterial baroreceptors may lead to activation of perivascular nerves as well as to central neural vasoactive nuclei that project axons directly or indirectly to vasculature and in turn can increase NO release onto adjacent blood vessels (69–71). Further, an intimate relationship of the cerebral microvasculature with NOS-containing neurons and glial cells has been shown (16, 33, 37).
The effects of selective nNOS inhibitors reproduced for the most part cerebral hemodynamic actions of nonselective inhibitors. One may be tempted to suggest a predominant role for nNOS on CBF autoregulation. However, despite available absence of selective inhibitors of eNOS, a distribution of this enzyme throughout the vasculature, a significant NO synthetic activity by eNOS (Fig. 4C), and regulation of this isozyme by shear stress (63), a contribution of eNOS in CBF autoregulation is also likely.
In contrast with its effects on the upper limit of CBF autoregulation, inhibition of NOS did not significantly alter the lower limit of CBF autoregulation in the newborn animal. In the adult rodent and ovine fetus, a role for NO in response to hypotension has been observed (17–19, 23, 24, 72). This discrepancy may be due to species differences (20–22). In addition, with regard to the fetus, because NOS is an O2-dependent enzyme, a lower O2 tension in the fetus may potentiate the effects of NOS blockers on the lower limit of autoregulation (23, 24). Alternatively, developmental differences in NOS activity may also be contributory. We have recently reported that NOS expression and activity in brain parenchyma are low in the fetus and increase in the neonate, after which it again decreases to values in the adult (16); similar differences in NOS expression and activity between newborn and adult are found in brain microvessels (Fig. 4). Hence, the newborn, with its higher NOS activity, may sustain better CBF after similar doses of NOS blockers.
The precise reason for increased NO production in neural tissue in the perinatal period is not known. Excess NO synthesis during the perinatal period increased the risk of brain damage after episodes of hypoxia-ischemia (73, 74). On the other hand, increased NO formation by the cerebral vasculature (and its neural connections) may be important to preserve adequate circulation at the end of parturition when arterial O2 tension is substantially reduced (75). NO may also serve a critical role in synaptogenesis in the developing subject (76).
Our previous observations implicated a significant role for PG in CBF autoregulation of the newborn (10, 45, 47). The present study points to a major involvement of NO. These two mechanisms are not mutually exclusive. In fact, PG and NO interact extensively at various levels. PG D2 and E2 actions have been found to be largely mediated by NO in newborn vasculature (13, 14), and the high perinatal levels of PG have also been found to control expression of cNOS (16). In addition, NO has also been found to stimulate formation of relaxant PG (77), which in turn can also mediate NO actions in the newborn (78). Therefore, there exist multiple epigenetic and genetic interactions between NO and PG. Thus, NO may interplay with PG in governing CBF autoregulation, as has been suggested (43).
In conclusion, our data reveal that excess formation of NO curtails the upper limit of CBF autoregulation during an acute rise in perfusion pressure in the newborn pigs and that nNOS plays an important role in this event. Nevertheless, this excessive NO production may overcome hypertension-induced constriction and thus provide additional explanation for the susceptible stressed immature neonate with insufficiently controlled cerebral circulation to develop intraventricular hemorrhage (79).
Abbreviations
- CBF:
-
cerebral blood flow
- NO:
-
nitric oxide
- NOS:
-
nitric oxide synthase
- PG:
-
prostaglandins
- MABP:
-
mean arterial blood pressure
- BP:
-
blood pressure
- L-NMMA:
-
Nω-monomethyl-L-arginine
- 7-NINA:
-
7-nitroindazole monosodium salt
- TRIM:
-
1-(2-trifluoromethylphenyl) imidazole
References
Baumbach GL, Heistad DD 1985 Regional, segmental, and temporal heterogeneity of cerebral vascular autoregulation. Ann Biomed Eng 13: 303–310.
Lassen NA 1964 Autoregulation of cerebral blood flow. Circ Res 14: 201–206.
Bill A, Linder J 1976 Sympathetic control of cerebral blood flow in acute arterial hypertension. Acta Physiol Scand 96: 114–121.
Leffler CW, Busija DW, Fletcher A, Beasley DG, Hessler JR, Green RS 1985 Effects of indomethacin upon cerebral hemodynamics of newborn pigs. Pediatr Res 19: 1160–1164.
Hernandez MJ, Brennan RW, Bowman GS 1980 Autoregulation of cerebral blood flow in the newborn dog. Brain Res 184: 199–202.
Papile LA, Rudolph AM, Heymann MA 1985 Autoregulation of cerebral blood flow in the preterm fetal lamb. Pediatr Res 19: 159–161.
Pasternak JF, Groothuis DR 1985 Autoregulation of cerebral blood flow in the newborn beagle puppy. Biol Neonate 48: 100–109.
Szymonowicz W, Walker AM, Cussen L, Cannata J, Yu VY 1988 Developmental changes in regional cerebral blood flow in fetal and newborn lambs. Am J Physiol 254: H52–H58
Tuor UI, Grewal D 1994 Autoregulation of cerebral blood flow: influence of local brain development and postnatal age. Am J Physiol 267: H2220–H2228
Chemtob S, Beharry K, Rex J, Varma DR, Aranda JV 1990 Prostanoids determine the range of cerebral blood flow autoregulation of newborn piglets. Stroke 21: 774–784.
Hayashi S, Park MK, Kuehl TJ 1985 Relaxant and contractile responses for prostaglandins in premature, newborn, and adult baboon cerebral arteries. J Pharmacol Exp Ther 233: 228–635.
Li DY, Abran D, Peri KG, Varma DR, Chemtob S 1996 Inhibition of prostaglandin synthesis in newborn pigs increases cerebral microvessel PGE2 and PGF2α receptors, their second messengers, and vasoconstrictor response to adult levels. J Pharmacol Exp Ther 278: 370–377.
Abran D, Varma DR, Chemtob S 1997 Regulation of prostanoid vasomotor effects and receptors in choroidal vessels of newborn pigs. Am J Physiol 272: R995–R1001
Abran D, Dumont I, Hardy P, Peri KG, Li DY, Molotchnikoff S, Varma DR, Chemtob S 1997 Characterization and regulation of prostaglandin E2 receptor and receptor-coupled functions in the choroidal vasculature of the pig during development. Circ Res 80: 463–472.
Gaillard T, Mulsch A, Klein H, Decker K 1992 Regulation by prostaglandin E2 of cytokine-elicited nitric oxide synthesis in rat liver macrophages. Biol Chem 373: 897–902.
Dumont I, Peri KG, Hardy P, Xin H, Martinez-Bermudez AK, Molotchnikoff S, Varma DR, Chemtob S 1998 PGE2, via EP3 receptors, regulates brain nitric oxide synthase in the perinatal period. Am J Physiol 275: R1812–R1821
Kajita Y, Takayasu M, Dietrich HH, Dacey RG Jr 1998 Possible role of nitric oxide in autoregulatory response in rat intracerebral arterioles. Neurosurgery 42: 834–842.
Jones SC, Radinsky CR, Furlan AJ, Chyatte D, Perez-Trepichio AD 1999 Cortical NOS inhibition raises the lower limit of cerebral blood flow-arterial pressure autoregulation. Am J Physiol 276: H1253–H1262
Tanaka K, Fukuuchi Y, Gomi S, Mihara B, Shirai T, Nogawa S, Nozaki H, Nagata E 1993 Inhibition of nitric oxide synthesis impairs autoregulation of local cerebral blood flow in the rat. Neuroreport 4: 267–270.
Thompson BG, Pluta RM, Girton ME, Oldfield EH 1996 Nitric oxide mediation of chemoregulation but not autoregulation of cerebral blood flow in primates. J Neurosurg 84: 71–78.
Saito S, Wilson DA, Hanley DF, Traystman RJ 1994 Nitric oxide synthase does not contribute to cerebral autoregulatory phenomenon in anesthetized dogs. J Auton Nerv Syst 49: S73–S76
Muhonen MG, Heistad DD, Faraci FM, Loftus CM 1994 Augmentation of blood flow through cerebral collaterals by inhibition of nitric oxide synthase. J Cereb Blood Flow Metab 14: 704–714.
van Bel F, Sola A, Roman C, Rudolph AM 1995 Role of nitric oxide in the regulation of the cerebral circulation in the lamb fetus during normoxemia and hypoxemia. Biol Neonate 68: 200–210.
McCrabb GJ, Harding R 1996 Role of nitric oxide in the regulation of cerebral blood flow in the ovine fœtus. Clin Exp Pharmacol Physiol 23: 855–860.
Talman WT, Dragon DN 1995 Mechanisms for preserved cerebrovascular autoregulation during hypertension in rats after sinoaortic denervation. Clin Exp Pharmacol Physiol 22: S77–S79
Lizasoain I, Weiner CP, Knowles R, Moncada S 1996 The ontogeny of cerebral and cerebellar nitric oxide synthase in the guinea pig and rat. Pediatr Res 39: 779–783.
Northington FJ, Tobin JR, Harris AP, Traystman RJ, Koehler RC 1997 Developmental and regional differences in nitric oxide synthase activity and blood flow in the sheep brain. J Cereb Blood Flow Metab 17: 109–115.
Tsukada M, Yamazaki Y, Koizumi A 1995 Changes in nitric oxide synthase activities in the cerebellum during development and aging of C57BL/6 mice. Tohoku J Exp Med 176: 69–74.
Riche D, Foutz AS, Denavit-Saubie M 1995 Developmental changes of NADPH-diaphorase neurons in the forebrain of neonatal and adult cat. Brain Res 89: 139–145.
Bredt DS, Snyder SH 1990 Isolation of nitric oxide synthetase, a calmodulin-requiring enzyme. Proc Natl Acad Sci USA 87: 682–685.
Lamas S, Marsden PA, Li GK, Tempst P, Michel T 1992 Endothelial nitric oxide synthase: molecular cloning and characterization of a distinct constitutive enzyme isoform. Proc Natl Acad Sci USA 89: 6348–6352.
Xie QW, Cho HJ, Calaycay J, Mumford RA, Swiderek KM, Lee TD, Ding A, Troso T, Nathan C 1992 Cloning and characterization of inducible nitric oxide synthase from mouse macrophages. Science 256: 225–228.
Bredt DS, Hwang PM, Snyder SH 1990 Localization of nitric oxide synthase indicating a neural role for nitric oxide. Nature 347: 768–770.
Garthwaite J 1991 Glutamate, nitric oxide, and cell-cell signaling in the nervous system. Neuroscience 14: 60–67.
Iadecola C, Beitz AJ, Renno W, Xu X, Mayer B, Zhang F 1993 Nitric oxide synthase-containing neural processes on large cerebral arteries and cerebral microvessels. Brain Res 606: 148–155.
Regidor J, Edvinsson L, Divac I 1993 NOS neurones lie near branchings of cortical arteriolae. Neuroreport 4: 112–114.
Estrada C, DeFelipe J 1998 Nitric oxide-producing neurons in the neocortex: morphological and functional relationship with intraparenchymal microvasculature. Cereb Cortex 8: 193–203.
Yoshida K, Okamura T, Kimura P, Bredt DS, Snyder SH, Toda N 1993 Nitric oxide synthase-immunoreactive nerve fibers in dog cerebral and peripheral arteries. Brain Res 629: 67–72.
Murphy S, Simmons ML, Agullo L, Garcia A, Feinstein DL, Galea E, Reis DJ, Minc-Golomb DJ, Schwartz JP 1993 Synthesis of nitric oxide in CNS glial cells. Trends Neurosci 16: 323–328.
Iadecola C, Pellegrino DA, Moskowitz M, Lassen NA 1994 Nitric oxide synthase inhibition and cerebrovascular regulation. J Cereb Blood Flow Metab 14: 175–192.
Huang PL, Huang Z, Mashimo H, Bloch KD, Moskowitz MA, Bevan JA, Fishman MC 1995 Hypertension in mice lacking the gene for endothelial nitric oxide synthase. Nature 377: 239–242.
Talman WT, Dragon DN 1995 Inhibition of nitric oxide synthesis extends cerebrovascular autoregulation during hypertension. Brain Res 672: 48–54.
Hardy P, Nuyt AM, Abran D, St-Louis J, Varma DR, Chemtob S 1996 Nitric oxide in retinal and choroidal blood flow autoregulation in newborn pigs: interaction with prostaglandins. Pediatr Res 39: 487–493.
Hayden JE, Leffler CW 1997 The effects of treatment with indomethacin on the cerebral vasculature of newborn piglets before and during hemorrhagic hypotension. Pediatr Res 41: 78–82.
Li DY, Hardy P, Abran D, Martinez-Bermudez AK, Guerguerian AM, Bhattacharya M, Almazan G, Menezes R, Peri KG, Varma DR, Chemtob S 1997 Key role for cyclooxygenase-2 in PGE2 and PGF2α receptor regulation and cerebral blood flow of the newborn. Am J Physiol 273: R1283–R1290
Chemtob S, Barna T, Beharry K, Aranda JV, Varma DR 1992 Enhanced cerebral blood flow autoregulation in the newborn piglet by d-tubocurarine and pancuronium but not by vecuronium. Anesthesiology 76: 236–244.
Chemtob S, Beharry K, Rex J, Varma DR, Aranda JV 1990 Changes in cerebrovascular prostaglandins and thromboxane as a function of systemic blood pressure. Circ Res 67: 674–682.
Hardy P, Abran D, Li DY, Fernandez H, Varma DR, Chemtob S 1994 Free radicals in retinal and choroidal blood flow autoregulation in the piglet: interaction with prostaglandins. Invest Ophthalmol Vis Sci 35: 580–591.
Hardy P, Bhattacharya M, Abran D, Peri KG, Asselin P, Varma DR, Chemtob S 1998 Increases in retinovascular prostaglandin receptor functions by cyclooxygenase-1 and −2 inhibition. Invest Ophthalmol Vis Sci 39: 1888–1898.
Babbedge RC, Bland-Ward PA, Hart S, Moore PK 1993 Inhibition of rat cerebellar nitric oxide synthase by 7-nitro indazole and related substituted indazoles. Br J Pharmacol 110: 225–228.
Mayer B, Klatt P, Werner E, Schmidt K 1994 Molecular mechanisms of inhibition of porcine brain nitric oxide synthase by the antinociceptive drug 7-nitro indazole. Neuropharmacology 33: 1253–1259.
Bland-Ward PA, Moore PK 1995 7-nitro indazole derivatives are potent inhibitors of brain, endothelium, and inducible isoforms of nitric oxide synthase. Life Sci 57: PL131–PL135
Handy RLC, Harb HL, Wallace P, Gaffen Z, Whitehead KJ, Moore PK 1996 Inhibition of nitric oxide synthase by 1-(2-trifluoromethylphenyl) imidazole (TRIM) in vitro: antinociceptive and cardiovascular effects. Br J Pharmacol 119: 423–431.
Rees DD, Palmer RMJ, Schulz R, Hodson HF, Moncada S 1990 Characterization of three inhibitors of endothelial nitric oxide synthase in vitro and in vivo. Br J Pharmacol 101: 746–752.
Verdon CP, Burton BA, Prior RL 1995 Sample pretreatment with nitrate reductase and glucose-6-phosphate dehydrogenase quantitatively reduces nitrate while avoiding interference by NADP+ when the Griess reaction is used to assay for nitrite. Anal Biochem 224: 502–508.
Moshage H, Kok B, Huizenga J, Jansen PLM 1995 Nitrite and nitrate determinations in plasma: a critical evaluation. Clin Chem 41: 892–896.
Peri KG, Hardy P, Li DY, Varma DR, Chemtob S 1995 Prostaglandin G/H synthase-2 is a major contributor of brain prostaglandins in the newborn. J Biol Chem 270: 24615–24620.
Li DY, Varma DR, Chemtob S 1994 Ontogenic increase in PGE2 and PGF2α receptor density in brain microvessels of pigs. Br J Pharmacol 112: 59–64.
Sasz G 1969 A kinetic photometric method for serum γ-glutamyl transpeptidase. Clin Chem 15: 124–136.
Goldstein GW, Wolinsky JS, Csejtey J, Diamond I 1975 Isolation of metabolically active capillaries from rat brain. J Neurochem 25: 715–717.
Hecker M, Mulsch A, Busse R 1994 Subcellular localization and characterization of neuronal nitric oxide synthase. J Neurochem 62: 1524–1529.
Hardy P, Peri KG, Lahaie I, Varma DR, Chemtob S 1996 Increased nitric oxide synthesis and action preclude choroidal vasoconstriction to hyperoxia in newborn pigs. Circ Res 79: 504–511.
Rubanyi GM, Romero JC, Vanhoutte PM 1986 Flow-induced release of endothelium-derived relaxing factor. Am J Physiol 250: H1145–H1149
Faraci FM 1991 Role of endothelium-derived relaxing factor in cerebral circulation: large arteries vs microcirculation. Am J Physiol 261: H1038–H1042
Prado R, Watson BD, Kuluz J, Dietrich WD 1992 Endothelium-derived nitric oxide synthase inhibition. Stroke 23: 1118–1124.
Rosenblum WI, Nishimura H, Nelson G 1990 Endothelium-dependent L-Argi- and L-NMMA-sensitive mechanisms regulate tone of brain microvessels. Am J Physiol 259: H1396–H1401
Gotoh F, Fukuuchi Y, Amano T, Tanaka K, Uematsu D, Suzuki N, Kawamura J, Yamawaki T, Itoh N, Obara K 1987 Role of endothelium in responses of pial vessels to change in blood pressure and to carbon dioxide in cats. J Cereb Blood Flow Metab 7: S275
Smiesko V, Kozik J, Dolezel S 1985 Role of endothelium in the control of arterial diameter by blood flow. Blood Vessels 22: 247–251.
Smeda JS, Daniel EE 1988 Elevations in arterial pressure induce the formation of spontaneous action potentials and alter neurotransmission in canine ileum arteries. Circ Res 62: 1104–1110.
Harada S, Tokunaga S, Momohara M, Masaki H, Togawa T, Imaizumi T, Takeshita A 1993 Inhibition of nitric oxide formation in the nucleus tractus solitarius increases renal sympathetic nerve activity in rabbits. Circ Res 72: 511–516.
Just A, Wittmann U, Wagner C, Ehmke H, Kirchheim HR, Persson PB 1994 The blood pressure buffering capacity of nitric oxide by comparison to the baroreceptor reflex. Am J Physiol 267: H521–H527
Kozniewska E, Oseka M, Stys T 1992 Endothelium-derived nitric oxide on cerebral circulation during normoxia and hypoxia in the rat. J Cereb Blood Flow Metab 12: 311–317.
Trifiletti RR 1992 Neuroprotective effect of NG-nitro- L -arginine in focal stroke in the 7-day-old rat. Eur J Pharmacol 218: 197–198.
Hamada Y, Hayakawa T, Hattori H, Mikawa H 1994 Inhibitor of nitric oxide synthesis reduces hypoxic-ischemic brain damage in the neonatal rat. Pediatr Res 35: 10–14.
Dildy GA, van den Berg PP, Katz M, Clark SL, Jongsma HW, Nijhuis JG, Loucks CA 1994 Intrapartum fetal pulse oximetry: fetal oxygen saturation trends during labor and relation to delivery outcome. Am J Obstet Gynecol 171: 679–684.
Lentile R, Malecka B, Picciurro V, Naso A, Pedale S, Macaione S 1996 Nitric oxide synthase in chick embryo retina during development. FEBS Lett 379: 82–84.
Salvemini D, Misko TP, Masferrer JL, Seibert K, Currie MG, Needleman P 1993 Nitric oxide activates cyclooxygenase enzymes. Proc Natl Acad Sci USA 90: 7240–7244.
Hardy P, Abran D, Hou X, Lahaie I, Peri KG, Asselin P, Varma DR, Chemtob S 1998 A major role for prostacyclin in nitric oxide-induced ocular vasorelaxation in the piglet. Circ Res 83: 721–729.
Perlman JM, McMenamin JB, Volpe JJ 1983 Fluctuating cerebral blood-flow velocity in respiratory-distress syndrome. N Engl J Med 309: 204–209.
Acknowledgements
The authors thank Hensy Fernandez for her technical assistance and F. Ménard Inc. (Ange-Gardien, Quebec) for their generous supply of newborn and juvenile pigs.
Author information
Authors and Affiliations
Additional information
Supported by grants from the Medical Research Council of Canada, the Heart and Stroke Foundation of Quebec, the Hospital for Sick Children's Foundation, and the March of Dimes Birth Defects Foundation. P. Hardy and A-M. Nuyt are recipients of fellowship awards from the Medical Research Council of Canada.
Rights and permissions
About this article
Cite this article
Hardy, P., Nuyt, AM., Dumont, I. et al. Developmentally Increased Cerebrovascular NO in Newborn Pigs Curtails Cerebral Blood Flow Autoregulation. Pediatr Res 46, 375 (1999). https://doi.org/10.1203/00006450-199910000-00004
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199910000-00004