Abstract
Erythropoietin receptors (Epo-R) are expressed on cells in the small bowel of human fetuses, but their function has not been defined. We hypothesized that intestinal Epo-R are present postnatally, and that recombinant erythropoietin (rEpo) would increase enterocyte migration and decrease cytokine-induced apoptosis. We used reverse transcriptase-polymerase chain reaction and immunohistochemistry to evaluate the presence of Epo-R mRNA and protein in rat intestinal epithelial cells (IEC-6), and in postnatal human and rat bowel. The effect of rEpo on rates of cell migration and proliferation were established in IEC-6 cells by using cell counting and incorporation of bromodeoxyuridine. To determine whether rEpo affects response to injury, cells were pretreated with rEpo, then were damaged with 25 or 50 ng/mL tumor necrosis factor-α plus 2.5 µg/mL cycloheximide. Cell death was determined by colorimetric bioassay. We found that Epo-R mRNA and protein were expressed by IEC-6 cells and by enterocytes of postnatal rat and human small bowel. Cells that had been exposed to 0.05 or 5.00 U/mL rEpo migrated faster than did the controls (p < 0.05), but no difference was noted in cell proliferation. Treatment of IEC-6 cells with rEpo before or at the time of injury resulted in a lower percentage of cell death, and this effect was neutralized by anti-Epo antibody. We conclude that Epo-R is expressed in enterocytes postnatally in rats and humans. Recombinant Epo increases the rate of migration of IEC-6 cells and decreases cytokine-induced apoptosis. These studies suggest that Epo within human milk has actions on neonate's intestinal function.
Similar content being viewed by others
Main
rEpo is commonly used to treat anemias, including the anemia associated with renal failure and the anemia of prematurity. Initially, Epo was thought to act only on cells of erythropoietic lineage, but it is now clear that the Epo-R is expressed by a variety of cell types, including endothelial cells(1,2), neurons(3–5), splenic cells(6,7), and cardiomyocytes(8). We have previously shown that Epo-R staining is prominent in proximal bowel of the 8- and 16-wk human fetus(6). However, it is not known whether these receptors persist on enteric cells postnatally, or whether the receptors are functional and, if so, what their function might be.
One role for enteral Epo-R might be to absorb Epo. It is intriguing that human milk contains significant Epo concentrations(9). Furthermore, rats nursing from dams rendered anemic have an erythropoietic response, suggesting that an elevated Epo concentration in the mother could be transmitted through milk to the pups(10–12). Alternatively, Epo might not be absorbed enterally but might have specific local effects on cells of the intestinal mucosa. This possibility is supported by work from Okada et al. showing that rEpo stimulated the growth of gastric mucosa cells(13).
To determine the relevance of these issues to human neonates, we first asked whether Epo-R persist postnatally in human intestine. We next asked whether rat small bowel and, specifically, IEC-6 cells, undifferentiated rat enterocytes, also expressed Epo-R. We then focused on possible nonabsorptive functions of the enterocyte Epo-R. Repair from mucosal injury requires a combination of cellular migration to reestablish mucosal continuity and cellular proliferation to replace injured or dying cells. In other cell systems, Epo increases cell migration(8) and exerts protective effects when cells are exposed to injury(4,14). We therefore hypothesized that rEpo would increase the rate of IEC-6 cell migration, and attenuate cell injury.
MATERIALS AND METHODS
Immunohistochemistry. Polyclonal rabbit anti-rat Epo-R and anti-human Epo-R antibodies were purchased from Santa Cruz Biotechnology, Inc (Santa Cruz, CA). Fetal liver or postnatal kidney were used as positive controls for both antibodies. The negative control for routine experiments was to incubate slides with nonimmune rabbit IgG (Ventana Medical Systems, Tucson, AZ). In addition, selected slides were incubated with primary antibody that had been preincubated with a 10-fold excess of the corresponding immunizing peptide (Santa Cruz). Both treatments abolished immunostaining in positive controls and in experimental sections.
Human postnatal tissues were obtained from surgical or autopsy specimens (n = 5). The age of the individuals ranged from 35 wk gestation, 2 d old; to term gestation, 3 mo old. Use of these tissues was permitted by the University of Florida Institutional Review Board. Rat tissues were obtained from 3- and 7-d-old rats, euthanized for unrelated experiments, which were approved by the University of Florida Institutional Animal Care Committee. For the immunolocalization of Epo-R in tissue sections, tissues were fixed in 10% formalin solution, then paraffin-embedded. Seven-micron sections were deparaffinized in two xylene washes, then were rehydrated through a graded series of alcohols, finishing with water. To stain the cultured cells, they were first fixed for 20 min in 10% formalin and then allowed to air dry. Before staining, cells were rehydrated in Ventana APK wash solution (Tris buffer, pH 7.6) for 20 min. For staining, we used the Ventana slide-staining system-a computer-based system for automated immunohistochemistry (Ventana Medical Systems)-with diaminobenzidine as the chromogen. Primary antibody reactions were done at 1:100 dilutions for 32 min. PBS containing 0.1% triton X-100 was used as the diluent for all antibody reactions. Sections were counterstained for 2 min with both hematoxylin and bluing (Ventana).
IEC-6 cells. Cells were maintained in T-75 flasks as a monolayer in DMEM supplemented with 5% fetal bovine serum (Sigma Chemical Co., St. Louis, MO), 2 mM L-glutamine, and 100 U penicillin, 100 µg streptomycin, and 0.25 µg Fungizone, pH 7.2 (GIBCO, BRL, Grand Island, NY) at 37°C in an atmosphere of humidified air and 5% CO2. Cells were trypsinized and plated into 60-mm, 100-mm, or 96-well dishes (Fisher) for the cell migration and cell injury experiments, and into double-chambered Lab-Tek chamber slides (Nunc, Inc, Naperville, IL) for immunostaining.
Preparation of total RNA. Total RNA was extracted from the cultured cells or homogenized tissue with the RNeasy elution kit, a method of RNA extraction based on the selective binding of RNA to a silica membrane (Qiagen, Chatsworth, CA)(4,15). Manufacturer directions were followed. Total RNA was extracted from IEC-6 cells, rat jejunum, liver, and bone marrow, as well as from human fetal jejunum, liver, and bone marrow. Purity and concentration of extracted RNA was determined by measuring UV absorbance at 260 and 280 nm. Total RNA was treated with RNase-free DNase I (GIBCO) before further experimentation.
Reverse transcription of RNA and amplification of cDNA. Reverse transcription of RNA and amplification of cDNA were performed with a DNA thermal cycler (Perkin-Elmer Cetus). Total RNA (2.0 µg) was combined with 2.0 µM oligo (dT) primers (GIBCO), heated to 70°C for 10 min, then placed on ice. The mixture was then combined with 250 µM dNTP (GIBCO), 0.01 M DTT, 50 mM Tris, pH 8.3, 75 mM KCl, and 3 mM MgCl2. After a 42°C incubation for 2 min, 2 µL of Superscript II reverse transcriptase (GIBCO) were added, and the mixture was incubated for 50 min further. The reaction was terminated by heating to 70°C for 15 min. Amplification cycles for human Epo-R and β-actin were performed under the following conditions: 10 mM Tris (pH 8.3), 50 mM KCl, 1.5 mM MgCl2, 2.0 mM dNTP, 0.2 µM upstream and downstream primers, 5% reverse transcriptase mix, 0.1 U/µL Ampli Taq 94°C for 1 min, 56°C for 1 min, 72°C for 2 min for 30 cycles, followed by 10 min elongation at 72°C. Temperatures and times used to amplify the rat Epo-R were: 94°C for 1 min, 65°C for 2 min, 72°C for 3 min for 38 cycles, followed by 10-min elongation at 72°C. The primer pair used to amplify rat Epo-R was: 5′-CTA-TGG-CTG-TTG-CAA-CGC-GA with 5′-CCG-AGG-GCA-CAG-GAG-CTT-AG, resulting in a 402 bp fragment(3,14). β-Actin primers were: 5′-TGA-CGG-GGT-CAC-CCA-CAC-TGT -GCC-CAT-CTA and 5′-CTA-GAA-GCA-TTT-GCG-GTG-GAC -GAT-GGA-GGG, resulting in a 661-bp fragment. All RNA samples were tested for DNA contamination by running a PCR sample using RNA that had not been reverse transcribed. All negative controls were negative. Liver and bone marrow were used as positive controls.
Specific Epo-R identification. Specificity of the RT-PCR products was confirmed by direct sequencing of an amplified PCR product, using the Taq DyeDeoxy Terminator protocol developed by Applied Biosystems (Perkin-Elmer Corp, Foster City, CA). The labeled extension products were analyzed on an Applied Biosystems Model 373 DNA sequencer.
Cell migration studies. IEC-6 cells were plated into 60-mm dishes. When cells were 80-90% confluent, medium was changed from 5% to 1% fetal bovine serum. rEpo (Amgen) was added to quadruplicate cultures at 5.00 or 0.05 U/mL (high dose versus low dose). Additional cultures were exposed to 0.05 U/mL rEpo plus 0.5 µg/mL neutralizing AEA (R & D systems, Inc.), 0.5 µg/mL AEA alone, or PBS. Cells were incubated under these conditions overnight. Confluent cultures were wounded with a sterile, 3-cm straight razor blade(16). Triplicate wounds, 4 mm wide, were made per plate. Immediately after wounding, cells were washed with PBS, and the medium was replaced. Cell migration was evaluated at 8 and 24 h after wounding. Cells were fixed in 10% formaldehyde for 20 min, then were lightly stained with hematoxylin. The number of nuclei that had migrated past the razor line were counted in four high-power fields on each of three lines at each time point. Thus there were 12 data points per culture dish. To determine whether pretreatment was necessary, we repeated these experiments, adding the experimental conditions (5.00 or 0.05 U/mL rEpo, 0.05 U/mL rEpo plus 0.5 µg/mL AEA, 0.5 µg/ml AEA alone, or PBS) at the time of cell wounding.
A dose-response relationship experiment was performed next. rEpo concentrations of 0.005, 0.05, 0.50, or 5.00 U/mL were used to pretreat cells 16 h before cell wounding. Cell migration was evaluated 8 and 24 h after wounding.
Cell proliferation experiments. In situ BrdU labeling (Calbiochem) was used to determine whether Epo affected the rate of proliferation of the IEC-6 cells. Briefly, cells were labeled with BrdU labeling solution for 60 min at 37°C. After being washed in PBS, the cells were fixed with 4% paraformaldehyde. Cells were then incubated with anti-5-bromo-2′-deoxyuridine/nuclease for 60 min, and washed with PBS. A diaminobenzidine-based detection system was then used. Labeled cells in five fields were counted at 200× in the region of confluence, as well as in the wounded region.
Cell injury experiments. Cells were plated into 96-well plates at a density of 2 × 104 cells/well. After the cells had been allowed to attach for 24 h, media were changed to phenol red-free media containing either 0.006, 0.06, 0.60, or 6.00 U/mL rEpo, 0.06 U/mL rEpo plus 0.6 mg/mL neutralizing AEA, or PBS. Twenty-four hours later, 50 or 25 ng/mL TNF-α plus 2.5 µg/mL CHI were added. Eight to 12 replicates of each condition were completed, including wells with no cytotoxic agents, which were used as controls. Also performed were experiments in which rEpo was administered at the same time the cells were exposed to TNF-α, rather than 24 h beforehand. The concentrations of TNF-α were chosen, based on pilot data, to create an experimental paradigm in which 60-80% of cells were killed in the absence of protective agents. Cell viability was evaluated with an In Vitro Toxicology Assay Kit XTT (Sigma Chemical Co.). This assay is based on the fact that mitochondrial dehydrogenases of viable cells cleave the tetrazolium ring of 2,3-bis[2-methyl-4-nitro-5-sulfophenyl]-2H-tetrazolium-5-carboxyanilide (XTT), yielding an orange product which is released into the media. Briefly, cells were incubated with 20% XTT for 2-4 h. At the end of this time, the individual wells were read spectrophotometrically at 450 nm. Two wells containing only media were used per plate, and the optical density (OD) from these cells was considered zero. Control wells that were not exposed to any cytotoxic agents were considered 100%.
Statistical analysis. Results are presented as means ± SEM. For statistical analysis, a t test was used (Primer of Biostatistics software, Windows version 4.02, copyright 1996 by McGraw-Hill, New York). Significance was defined as p < 0.05.
RESULTS
Epo-R was expressed on proximal and distal small bowel from all five postnatal infants (ages 2 days to 3 months). All samples showed specific immunoreactivity in cells of the brush border. Fig. 1A shows a representative section from the distal small bowel of a 3-month-old child. All tested samples of rat small bowel were also immunoreactive with anti-rat Epo-R. Fig. 1B shows a section of proximal bowel from a 3-d-old rat. The distribution of immunostaining differed slightly in the rat, with less immunoreactivity in their crypt cells, compared with humans.
Erythropoietin receptor immunoreactivity in infant human and infant rat small bowel. Panel A shows a section of infant human distal small bowel stained with anti human Epo-R Antibody (200×). Note the immunoreactivity of both the brush border and crypt cells (brown). Panel C shows the negative control for the human antibody, preincubated with blocking peptide. Panel B shows a section of infant rat proximal small bowel stained with anti rat Epo-R antibody (200×). Panel D shows the negative control for anti-rat Epo-R, incubated with preimmune serum.
To perform RT-PCR on total RNA extracted from human fetal bone marrow, small bowel, and liver, we used primers specific to human Epo-R. Similarly, we used primers specific for rats to amplify Epo-R mRNA from IEC-6 cells, rat bone marrow, small bowel, and liver. Fig. 2A shows that all tissues and cells tested expressed mRNA for Epo-R. Panel B shows the β-actin controls for each tissue. The presence of Epo-R on IEC-6 cells was confirmed in confluent cultured cells that demonstrated moderate immunoreactivity (data not shown).
RT-PCR of fetal human and infant rat tissues using primers specific for Epo-R. Panel A shows a representative ethidium bromide-stained 2% wt/vol agarose gel showing RT-PCR cDNA fragments for Epo-R from fetal human tissues and from infant rat tissues, as well as from IEC-6 cells. Lane 1 shows a 100-bp ladder as a molecular weight marker. Lanes 2-4 show human bone marrow, intestines and liver, whereas lanes 5-8 IEC-6 cells, bone marrow, intestines and liver, respectively. Lane 9 shows a negative control (RNA that was not reverse transcribed before PCR reaction). Panel B shows β-actin controls for the tissues shown in panel A.
To determine whether rEpo stimulated migration, we cut across confluent IEC-6 cells in culture and counted cells that migrated across the razor border after 8 and 24 h. Both high and low-dose rEpo significantly increased cell migration (Fig. 3). To determine an optimal dosing range of rEpo, we pretreated cells for 24 h with rEpo ranging from 0.005 to 50.00 U/mL. Cells that migrated across the razor mark were counted 24 h after the cut. Results are shown in Table 1. Cells showed significantly increased migration at rEpo concentrations of 0.05 U/mL or higher. To determine the effect of rEpo pretreatment on cell migration, we repeated the experiments, adding Epo at the time the razor cut was made. No differences in cell migration at 24 h were found at any rEpo concentration tested in the absence of pretreatment (data not shown). The incorporation of BrdU into DNA in cells exposed to rEpo was similar to that in cells not exposed; thus the difference in the number of cells migrating across the razor line was not explained by a difference in cell proliferation.
IEC-6 migration after wounding. The Y axis of panel A shows the number of cells that had migrated across the razor cut border in 8 h. The X axis shows cells treated with high-dose rEpo (5 U/mL), low-dose rEpo (0.05 U/mL), low-dose Epo plus neutralizing anti-Epo antibody, and control cells treated with PBS only. Panel B shows cell migration 24 h after wounding. Each column represents the mean value of 12 counts ± SEM. * = p < 0.0001, ** = p < 0.001 when experimental condition was compared with PBS control.
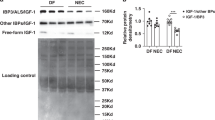
To determine whether rEpo has protective effects on cultured enterocytes, we exposed IEC-6 cells to either 25 or 50 ng/mL TNF-α plus 2.5 µg/mL CHI. We used cells that had been pretreated with rEpo for 24 h (Fig. 4A), as well as cells that were not pretreated (Fig. 4B). A dose-response curve was generated by using rEpo concentrations from 0.06 U/mL to 60.00 U/mL. rEpo concentrations in the range from 0.06 to 6 U/mL decreased cell death in cytokine-exposed cells. This effect was reversed by the addition of neutralizing anti-Epo antibody. No protective response was noted at the highest dose used (60 U/mL).
rEpo effects on IEC-6 survival subsequent to cytokine damage. Panel A shows cell survival when IEC-6 cells were pretreated with varying doses of rEpo for 24 h. The dose of rEpo is shown on the X axis. Hatched columns show mean values ± SEM of cells treated with 50 ng/mL TNF-α plus 2.5 µg/mL CHI, solid columns show results of injury with 25 ng/mL TNF-α plus 2.5 µg/mL CHI, and stipled columns show control values for each rEpo condition. Panel B shows rEpo effects on cell survival in the absence of pretreatment. * = p < 0.005, ** = p < 0.05 when an experimental condition was compared with PBS control.
DISCUSSION
These studies focus on functions of Epo-R within the intestine. There are many benefits to breast feeding, including decreased susceptibility to infections such as sepsis, meningitis, enteritis, and even necrotizing enterocolitis(17–21). Many factors that might contribute to this protective effect are contained in human milk(22). One of these factors might be Epo. Epo concentrations in human milk vary somewhat with postpartum day, with mean concentrations of 34 ± 6 mU/mL measured after 2 months of breast feeding(9). Calculations of enteral Epo intake based on average milk intake suggest that a breast-feeding infant might receive between 4 and 40 U/kg/wk(9). Receptors for Epo have been identified in human fetal small bowel(6), but it is not known whether these receptors persist postnatally or whether they are functional. Different types of function might include an absorptive function [although rEpo was given enterally to premature neonates in one pilot study, with no notable increase in circulating Epo concentrations or reticulocyte counts(23)] or a local effect in the intestine.
We found that Epo-R persist in the small bowel of the postnatal human infant and that they are also present in the postnatal rat bowel. This suggests that the rat might be a model for the study of enteric Epo function. We also identified Epo-R on IEC-6 cells, a line of intestinal cells derived from rats.
We hypothesized that Epo would be functional in enteric cells and that its function in these cells might be similar to its nonhematopoietic effects in other types of cells. Wald et al.(8) showed that rEpo stimulates migration of cardiomyocytes, an effect mediated by Na+-K+ ATPase. We and others reported that rEpo can protect neurons from death after a stimulus that ordinarily induces programmed cell death(4,14,24). We therefore sought to determine whether rEpo would increase cell migration in IEC-6 cells and whether it would decrease cell death after a cytokine exposure that would induce apoptosis. Indeed, Epo did increase migration of IEC-6 cells, and survival rate after a cytokine insult in cells exposed to rEpo was approximately double that of cells that were not treated. These effects were seen over a range of rEpo concentrations: 0.05-50.0 U/mL increased cell migration, whereas 0.06-6.00 U/mL decreased cell death due to TNF-α + CHI. At the lowest dose of rEpo tested (0.005 U/mL), we did not see any effects on migration or cell death. At 0.05 U/mL, comparable to the higher end of Epo concentrations found in breast milk (mean 0.034 ± 0.006 U/mL)(9), we did find such effects. To minimize the possible effects of growth factors contained in the serum on cell migration, the concentration of fetal bovine serum was decreased from 5% to 1% 24 h before the experiment. All cultures were maintained under identical conditions, with the exception of the added rEpo, PBS, or neutralizing antibody. Thus, any effects of growth factors contained in the 1% fetal bovine serum were the same across experimental conditions and should not have been responsible for the experimental differences. The addition of neutralizing anti-Epo antibody alone did not affect cell migration, suggesting that there was not a significant amount of Epo in the added FBS, and, similarly, that Epo probably was not produced by the cultured cells as a response to the razor cut.
We speculate that one of the factors contributing to the protective effects of human milk is Epo. Studies are underway in our laboratory to determine whether the protective effect of rEpo that we observed on cells in culture also occurs in vivo.
Abbreviations
- AEA:
-
anti-Epo antibody
- BrdU:
-
bromodeoxyuridine
- CHI:
-
cycloheximide
- DMEM:
-
Dulbecco's modified Eagle medium
- Epo:
-
erythropoietin
- Epo-R:
-
erythropoietin receptors
- rEpo:
-
recombinant erythropoietin
- IEC-6:
-
rat intestinal epithelial cell line
- PBS:
-
phosphate-buffered saline
References
Anagnostou A, Liu Z, Steiner M, Chin K, Lee ES, Kessimian N, Noguchi CT 1994 Erythropoietin receptor mRNA expression in human endothelial cells. Proc Natl Acad Sci USA 91: 3974–3978.
Yamaji R, Okada T, Moriya M, Naito M, Tsuruo T, Miyatake K, Nakano Y 1996 Brain capillary endothelial cells express two forms of erythropoietin receptor mRNA. Eur J Biochem 239: 494–500.
Masuda S, Nagao M, Takahata K, Konishi Y, Gallyas F Jr, Tabira T, Sasaki R 1993 Functional erythropoietin receptor of the cells with neural characteristics: comparison with receptor properties of erythroid cells. J Biol Chem 268: 11208–11216.
Juul SE, Anderson DK, Li Y, Christensen RD 1998 Erythropoietin and erythropoietin receptor in the developing human central nervous system. Pediatr Res 43: 40–49.
Juul SE, Yachnis AT, Rojiani AM, Christensen RD 1999 Immunohistochemical localization of erythropoietin and its receptor in the developing human brain. Pediatr Dev Pathol 2: 148–158.
Juul SE, Yachnis AT, Christensen RD 1998 Tissue distribution of erythropoietin and erythropoietin receptor in the developing human fetus. Early Hum Dev 52: 235–249.
Dame C, Fahnenstich H, Freitag P, Hofmann D, Abdul-Nour T, Bartmann P, Fandrey J 1998 Erythropoietin mRNA expression in human fetal and neonatal tissue. Blood 92: 3218–3225.
Wald MR, Borda ES, Sterin-Borda L 1996 Mitogenic effect of erythropoietin on neonatal rat cardiomyocytes: signal transduction pathways. J Cell Physiol 167: 461–468.
Kling PJ, Sullivan TM, Roberts RA, Philipps AF, Koldovsky O 1998 Human milk as a potential enteral source of erythropoietin. Pediatr Res 43: 216–221.
Carmichael RD, Gordon AS, Lobue J 1986 Effects of the hormone erythropoietin in milk on erythropoiesis in neonatal rats. Endocrinol Exp 20: 167–188.
Carmichael RD, LoBue J, Gordon AS 1992 Neonatal erythropoiesis. I. Peripheral blood erythropoietic parameters: data suggest erythropoietin transfer via maternal milk. Endocr Regul 26: 83–88.
Carmichael RD, LoBue J, Gordon AS 1992 Neonatal erythropoiesis. II. Bone marrow and splenic erythropoietic activity: data suggest erythropoietin transfer via maternal milk. Endocr Regul 26: 143–149.
Okada A, Kinoshita Y, Maekawa T, Hassan MS, Kawanami C, Asahara M, Matsushima Y, Kishi K, Nakata H, Naribayashi Y, Chiba T 1996 Erythropoietin stimulates proliferation of rat-cultured gastric mucosal cells. Digestion 57: 328–332.
Morishita E, Masuda S, Nagao M, Yasuda Y, Sasaki R 1997 Erythropoietin receptor is expressed in rat hippocampal and cerebral cortical neurons, and erythropoietin prevents in vitro glutamate-induced neuronal death. Neuroscience 76: 105–116.
Martin VV, Nock S, Meyer-Gauen G, Hager K-P, Jensen U, Cerff R 1993 A method for isolation of cDNA-quality mRNA from immature seeds of a gymnosperm rich in polyphenolics. Plant Mol Biol 22: 555–556.
Ciacci C, Lind SE, Podolsky DK 1993 Transforming growth factor beta regulation of migration in wounded rat intestinal epithelial monolayers. Gastroenterology 105: 93–101.
Lucas A, Cole TJ 1990 Breast milk and neonatal necrotising enterocolitis. Lancet 336: 1519–1523.
Ashraf RN, Jalil F, Zaman S, Karlberg J, Khan SR, Lindblad BS, Hanson LA 1991 Breast feeding and protection against neonatal sepsis in a high risk population. Arch Dis Child 66: 488–490.
Golding J, Emmett PM, Rogers IS 1997 Does breast feeding have any impact on non-infectious, non-allergic disorders?. Early Hum Dev 49( suppl): S131–142.
Haffejee IE 1991 Neonatal rotavirus infections. Rev Infect Dis 13: 957–962.
Hylander MA, Strobino DM, Dhanireddy R 1998 Human milk feedings and infection among very low birth weight infants. Pediatrics 102: E38.
Garofalo RP, Goldman AS 1998 Cytokines, chemokines, and colony-stimulating factors in human milk: the 1997 update. Biol Neonate 74: 134–142.
Britton JR, Christensen RD 1995 Enteral administration of recombinant erythropoietin to preterm infants. J Perinatol 15: 281–283.
Sakanaka M, Wen TC, Matsuda S, Masuda S, Morishita E, Nagao M, Sasaki R 1998 In vivo evidence that erythropoietin protects neurons from ischemic damage. Proc Natl Acad Sci USA 95: 4635–4640.
Author information
Authors and Affiliations
Additional information
Supported by grant RR-00083 from the National Institutes of Health, and by grants from the Howard Hughes Medical Institute Research Resources Program of the University of Florida College of Medicine, and Children's Miracle Network.
Rights and permissions
About this article
Cite this article
Juul, S., Joyce, A., Zhao, Y. et al. Why Is Erythropoietin Present in Human Milk? Studies of Erythropoietin Receptors on Enterocytes of Human and Rat Neonates. Pediatr Res 46, 263–268 (1999). https://doi.org/10.1203/00006450-199909000-00003
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199909000-00003
This article is cited by
-
The impact of indole-3-lactic acid on immature intestinal innate immunity and development: a transcriptomic analysis
Scientific Reports (2021)
-
Erythropoietin prevents necrotizing enterocolitis in very preterm infants: a randomized controlled trial
Journal of Translational Medicine (2020)
-
Robust increases in erythropoietin production by the hypoxic fetus is a response to protect the brain and other vital organs
Pediatric Research (2018)
-
Retinopathy of prematurity: inflammation, choroidal degeneration, and novel promising therapeutic strategies
Journal of Neuroinflammation (2017)
-
Erythropoietin regulates intestinal iron absorption in a rat model of chronic renal failure
Kidney International (2010)