Abstract
We studied the development of visual processing in 58 children, ranging from 1 d to 12 y of age (median age 29 mo), using functional magnetic resonance imaging. All but nine children had either been sedated using chloral hydrate (n = 12) or pentobarbital (n = 28). Nine children were studied under a full halothane/N2O:O2 anesthesia. In the first postnatal month, 30% of the neonates showed a positive blood oxygenation level-dependent (BOLD) contrast signal, whereas, for infants between the ages of 1 mo and 1 y, 27% did so. Thirty-one percent of children between 1 and 6 y of age and 71% of children aged 6 y and above showed a positive BOLD contrast signal change to our visual stimulation paradigm.
Besides the usual positive BOLD contrast signal change, we also noted that a large portion of the children measured displayed a negative BOLD contrast signal change. This negative BOLD contrast signal change was observed in 30% of children up to 1 mo of age, in 27% between 1 mo and 1 y of age, in 47% between 1 and 6 y of age, and in 14% of children 6 y and older. In the children in which we observed a negative correlating BOLD contrast signal change, the locus was more anterior and more lateral than the positive BOLD contrast signal, placing it in the secondary visual cortical area. The results indicate that when using functional magnetic resonance imaging on children, the primary visual cortical area does not respond functionally in the same manner as that of the adult until 1.5 y of age. This supports earlier clinical and electrophysiologic findings that different cortical mechanisms seem to contribute to visual perception at different times postnatally.
Similar content being viewed by others
Main
The development of fMRI has enabled us to map brain function in a noninvasive manner(1–3). fMRI studies in human adults have localized regions of brain activation in response to passive sensory stimulation(4–7) or active neurocognitive tasks(8–11). However, studies that have focused on imaging maturational changes of brain function during early human life are still scarce(12–15). One of the most interesting areas in this regard is the development of vision. The cortical visual system in man is believed to differentiate entirely postnatally(16). Whereas for the neonate, vision probably plays a subordinate role, by the age of 6 mo it gradually becomes the dominant sense, with which the infant explores its environment and makes social contact. Vision, then, forms the basis not only for perceptual, but also for future cognitive, intellectual, and social development(17).
Our understanding of the functional development of the visual system in man has always depended on technical advances. Most of our current knowledge and understanding is the result of behavioral testing and studies using visually evoked potentials to trace the emergence of activity in the visual system. In the past, various authors have noted that neonates and infants display a variety of vision related behavior, from tracking a salient object to mimicking facial expressions(17–19). The development of stereopsis and visual topography during infancy is accompanied by changes in visual-evoked potentials and coincides with the time when visual acuity measurements have noted a rapid improvement(20,21). These observations are also supported by the most salient phases in the anatomical development of the human visual system(22,23). The presence of visually guided behavior immediately after birth, however, would indicate that neonates are either able to analyze their visual environment by structures other than the visual cortex, or that the visual cortex is not a tabula rasa at birth but contains hard-wired mechanisms. With the recent advances of fMRI, a noninvasive method for monitoring functional development of the CNS in children has become available.
We investigated developmental aspects of the human visual system that take place during early life by studying its cortical activity in response to visual stimulation in children between the ages of 1 d and 12 y using fMRI. This enabled us to elucidate the role of the primary visual cortex and prestriate areas in the processing of visual information at different stages of brain development.
METHODS
Subjects. Seventy five children ranging in age between 1 d and 12 y (median age 29 mo; first quartile 4 mo; third quartile 62 mo) were examined with fMRI after a diagnostic imaging examination on a 2 Tesla magnetic resonance system (Tomicon S-200A, Bruker-Medical). Children displaying signs or symptoms that might have interfered with normal cerebral development or function, particularly of the visual cortical areas, were excluded from our study. Data from 58 children free of motion artifacts were available for final analysis.
In all but nine children, it was deemed necessary to administer a sedative agent to ensure the acquisition of well-defined diagnostic images. Of the 49 children who had been administered a sedative, nine were examined under general anesthesia (0.5% halothane in a gas mixture of N2O:O2), 12 were sedated with chloral hydrate orally via a naso-gastric tube (75 to 100 mg/kg), and 28 children received pentobarbital i.v. (3 to 5 mg/kg [maximum 120 mg]). The sedative agent was administered 10-30 min before the onset of the diagnostic imaging session, which usually lasted 1 h or longer. The fMRI study always followed the clinical diagnostic procedure.
The child was placed face-up and entered the magnetic resonance tomograph headfirst. The head was positioned using a laser-based positioning system. To stabilize the head position, we padded the space between the head and the headrest with foam rubber padding material. Then the flicker-goggles were placed over the eyes. The eyes were kept open by taping the eyelids open. In children examined under a general anesthesia, the eyes were kept open using eyelid retractors. In both cases, all appropriate eye protection measures were taken. The child's heart rate, respiratory rate, and blood oxygen saturation were continuously monitored.
Data Acquisition. A BOLD contrast-sensitive(24), multi-slice fast gradient echo sequence with interleaved excitation cycles (MUSIC) was used for data acquisition(25). The repetition time was 100 ms and the echo time 40 ms, the pulse flip angle was 20O, and the field of view between 22 and 25 cm2. A package of six axial oblique slices, with a thickness of 4 mm and a slice separation of 1 mm, was placed through the visual cortex, parallel to the calcarine sulcus. This enabled us to obtain activity measurements from the upper and lower bank of the calcarine sulcus, thus covering a large part of the primary visual area and extra striate visual cortical areas. We included the thalamic nuclei and tectum of the midbrain in the packet when studying neonates and infants. The acquisition matrix was 128 × 64, reconstructed into a 128 × 128 matrix, after zero filling. Subjects were shown eight stimulus cycles, with each cycle consisting of a 30-s period (four images) without stimulation followed by a 30-s period (four images) with stimulation. In total 64 images per slice were acquired. Visual stimulation occurred with a set of red light, light-emitting diode goggles (Grass Co., Quincy, MA) flickering at a frequency of 8 Hz. The entire experiment was under the control of a microcomputer, which triggered the stimulation. In the children tested under general anesthesia, titanium eyelid retractors were inserted using all appropriate protective measures. In sedated children adhesive tape was used to retract the eyelids. The study was conducted with the approval of the ethics committee of University Children's Hospital Zurich.
Functional Analysis. BOLD contrast activity was measured with a cross-correlation analysis between the stimulus presentation and the time series signals for each slice, using AVS (Advanced Visual Systems Inc., Waltham, MA) software. Voxels with a correlation coefficient of r > 0.4 for positive BOLD contrast-related signals and r > -0.35 for negative BOLD contrast-related signals were accepted as representing correlated responses to our stimulus paradigm.
RESULTS
Out of the total of 75 children examined, 17 had to be excluded from the final analysis due to motion artifacts, leaving 68 measurements in 58 children. Data from eight neonates aged 1 to 30 d, from 14 infants aged 1 mo to 1 y, and from 29 children aged 1 to 6 y and seven aged 6 to 12 y were obtained.
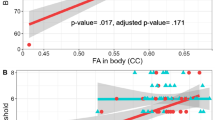
The stimulus paradigm produced two different types of responses in the visual cortex. In 25 instances, we observed a positively correlating BOLD contrast signal change (Fig. 1A) and in 23 instances a negatively correlating BOLD contrast signal change (Fig. 1B). In 10 children both positive and negative BOLD signals could be observed but in physically different locations of the brain, so they were treated as separate signals. No stimulus-related signals could be detected in the remaining 20 children. In the instances where we observed a negatively correlated signal, the locus of the activity was located more anterior in the calcarine sulcus compared with the locus of the positive BOLD contrast signal. This locus of negative BOLD contrast signal was judged from the anatomical slices to correspond to V2.
(A) A positive BOLD contrast signal change during visual stimulation in an 8-y-old, female child during general anesthesia (halothane/N2O:O2). The entire posterior portion of the calcarine sulcus representing the visual cortex shows up as being activated. (B) A negative BOLD contrast signal change during visual stimulation in a 26-mo-old, female child sedated with pentobarbital. No visual activity is observed in the calcarine sulcus with the locus of activity having shifted to a more anterior and more superior location (presumably V2).
Data Analysis. The use of the BOLD contrast signal as a means of probing the development of the CNS will yield a picture of the CNS that is dominated by oxygen consumption during the course of its development. With this in mind, we opted to divide the children into age groups that corresponded to the development of synaptic density, as described by Huttenlocher et al.(22), which is indirectly linked to oxygen consumption. Table 1 shows the number of children in the different age groups that showed either a positive or a negative BOLD contrast signal in V1 when being stimulated.
A positive BOLD signal change in the visual cortex was observed in six out of 18 infants between the ages of 1 d and 4 mo, in four out of 25 small children between 4 mo and 3.5 y, and in 13 out of 25 children 4 y and older. A negative BOLD signal was observed in five out of 18 of the youngest group, 12 out of 25 children of the middle age group, and eight out of 25 of the older children. We used a χ2 test to examine whether the frequency distribution of the BOLD contrast differed between the groups. The distribution of the positive BOLD contrast signal differed significantly between the different age groups (χ2 = 6.59, df = 2, p < 0.05) as did the distribution of the negative BOLD contrast signal (χ2 = 7.36, df = 2, p < 0.05).
Table 2 shows the number of children that displayed either a positive or a negative BOLD signal in the visual cortex upon visual stimulation in relation to the anesthetic agent administered.
Due to the small number of children examined without a sedative agent, we combined this group with the group that had been given a general anesthesia using halothane in a gas mixture N2O:O2. We found this legitimate because, in a comparative study by Lindauer et al.(26), halothane altered CBF the least among the anesthetic agents used. Moreover, Tsubokawa et al. showed that halothane even raises CBF slightly(27), whereas both chloral hydrate and pentobarbital lower CBF. Statistical analysis of the frequency of positive or negative BOLD contrast signals in the group tested without anesthetic and the group tested under a general anesthetic (halothane/N2O:O2) revealed no difference in the frequency of either BOLD contrast signal change (Fisher's exact probability test; positive p = 0.15; negative p = 0.12). We therefore grouped the sedative agents, depending on their suppressive effect on CBF, into three groups: 1 = None/Mild, 2 = Moderate, and 3 = Strong(26).
Group 1 contained 18 children, of which half had been given no sedative agent and half had been tested under general anesthesia using halothane in N2O:O2 gas. Group 2 consisted of 12 children sedated with chloral hydrate and group 3 contained 28 children sedated with pentobarbital. A χ2 analysis revealed no significant differences in the frequency distribution of the positive BOLD contrast signal (χ2 = 3.71, df = 2, NS) with the type of sedative agent used. A significant difference in the distribution of the negative BOLD contrast signal, however, with respect to the type of anesthetic agent (χ2 = 7.54, df = 2, p < 0.05) was found. Thus, we examined the possible effect that the anesthetic agent may have had on the type of signal change observed, positive or negative(28).
DISCUSSION
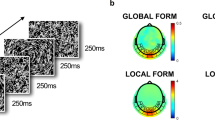
Our results indicate that, with increasing age, the incidence of a negative BOLD signal response exhibits a bi-phasic pattern peaking around 1 to 2 y of age and decreasing thereafter, whereas that of a positive BOLD response increases with age. The presence of brain activity in neonates and infants clearly indicates that a part of the visual cortex is responsive to visual stimulation from birth and can be detected using fMRI. Careful analysis of the negatively correlating BOLD contrast signal revealed that its origin is not due to a simple phase shift between the stimulus cycle and the response function. The polarity of the BOLD signal depends on the ratio Hboxy/Hbdeoxy. In human adults, local CBV has been found to be increased during brain activation compared with the resting state(1,29,30), leading to an increase in the ratio Hboxy/Hbdeoxy and consequently a positively correlated BOLD signal change(31). Although in adults the quantitative dynamic interrelationship of local cerebral metabolic rate of oxygen, CBV, and local cerebral blood flow (lCBF) is a matter of research, regional changes of CBF dominate, leading to a net increase in the venous oxy-hemoglobin concentration as a consequence of neuronal activation. The presence of a positive BOLD contrast signal could, therefore, be taken as an indication of a fully mature vascular system, able to increase lCBF in response to neuronal activation and increased metabolic demand. Figure 2 depicts the relationship between changes in local cerebral metabolic rate of oxygen and changes in vascular response (lCBF) schematically, after a change in neuronal activity.
This diagram shows the relationship between change in metabolic rate of oxygen consumption and the change in cerebral blood flow and the nature of the BOLD contrast signal. If, during neuronal activity, the increase in blood flow overcompensates for the oxygen metabolized, the BOLD contrast signal is positive (red region). If increase in the cerebral blood flow cannot compensate for the oxygen metabolized, the BOLD contrast signal is negative (blue region).
On the basis of these mechanisms, our findings of negative BOLD contrast-related signals in neonates, where we found visual activity, and in the majority of our infants and small children can be interpreted in several ways. First, the vascular system of the infant may be unable to redress the increased oxygen demand by increasing the lCBF, as in the adult, leading to a decrease in the ratio Hboxy/Hbdeoxy. (See Fig. 2). A role for the immature vascular response is supported by our observation of negative activity-related BOLD contrast signal changes in nine unsedated infants. Meek et al. have observed a wide range of variation in the magnitude of CBV changes in the occipital region of neonates and infants upon visual stimulation, as measured by near-infrared spectroscopy(32). Their observation is in concordance with our own observation. If the development of CBF were lagging behind visual responsiveness in V1, we would expect to see many more instances of a negative BOLD contrast signal in this area. This was not the case in V1 but was the case in V2. There are no known differences between V1 and V2 in the rate of development or reactivity of the vascular system. Such a difference could explain the presence of a negative BOLD contrast signal in V2 and its absence in V1. Secondly, the brains of infants and young children exhibit larger numbers and higher densities of neurons and synapses than adult brains. Neurons in the visual cortex show the highest number of growth cones, dendritic and somatic spines between the ages of 4 to 8 mo, followed by a pruning of superfluous connections to adult levels by the age of 11 y(22,23,33,34). As a consequence the increased neuronal and synaptic density leads to a higher metabolic demand during the early phases of brain development(12). This pattern of development results in an increased cerebral metabolic rate of oxygen and, in response to neuronal activation, in an increased oxygen demand. Consequently, the ratio Hboxy/Hbdeoxy falls below resting level and a negatively correlated BOLD contrast signal ensues (See Fig. 2). This conclusion is supported by the fMRI study by Yamada et al.(35), and a near-infrared spectroscopy study by Meek et al.(32). The latter study showed that in contrast to adults, neonates and infants exhibit an increase in cerebral oxygen use during visual stimulation to such an extent that it outstripped the increase in CBF observed in the visual cortex. The fMRI study by Yamada et al.(35) reports a positive BOLD contrast signal during the first month of life, which subsequently changes into a negative BOLD contrast signal. This finding stands in contradiction to our own findings as well as those of Meek et al.(32). However, there is one important difference between the study of Yamada et al. and the studies both Meek et al. and we performed that has to be taken into account. All children in the Yamada et al. study were tested under pentobarbital sedation. Every study using this sedative agent has reported that it has the most, not the least, profound effect on the vascular response.(26–28). In this light there must be some concern that the positive BOLD contrast signal observed in neonates younger than 1 mo may somehow be a confounding effect between an immature vascular system and the presence of the sedative agent.
At this point we would like to address the possible effect of the sedative agent in our own study. Chloral hydrate and pentobarbital are known to impede CBF response(26). A companion study on adult volunteers showed that 15 min after i.v. administration of pentobarbital, the normal positive BOLD contrast signal was significantly reduced, occasionally even turned into a negative BOLD contrast signal(28). However, we found no significant difference in the visual response functions when comparing presedative test results with those conducted 45 min after the application of the drug. Because the children were always studied at least 1 h after administration of the sedative agent, it is likely that its influence on our data would have been greatly diminished. This is born out by our statistical analysis. We conclude that the presence of a negative BOLD contrast signal would indicate that there is neuronal activity but that the vascular response is immature. The presence of a positive BOLD contrast signal on the other hand indicates neuronal activation and a mature vascular response.
In the instances where we observed negatively correlated brain activity, the site of the activity was always located more anterior in the calcarine sulcus and more dorsal in the superior parietal lobule, i.e. area V2, when compared with areas of positive BOLD signals (Fig. 1B). The presence of these regions with negatively correlated BOLD contrast signals clearly indicates that visual cortical areas outside of V1 are being activated in response to visual stimulation from birth and can be detected using fMRI. Although the positively correlated fMRI signal seen in older children and adolescents was always located in V1, only rarely did we observe visual activity in this area before the end of the first year of life. Our observation that no significantly correlated BOLD signals, positive or negative, were found in the primary visual cortex of neonates and young infants is a further indication that V1 is not functioning in the same manner during early life as it does in older children and adults. This is not to say that V1 is not active during visual stimulation before the end of the first year of life. What our findings indicate is that, when using fMRI techniques, great caution has to be exercised if visual activity is to be detected using a BOLD contrast signal. Activity in V1 does not resemble that of the adult until late infancy. We, therefore, conclude that the absence of any BOLD contrast signal, positive or negative, in V1 must be due to a combination of immature vascular response and low responsiveness of the primary visual area in this age group.
Of major interest was the observation that three neonates also exhibited significant stimulus-related activity in subcortical areas, e.g. in the region of the pulvinar thalami and next to the quadrigeminal plate. This may indicate that a second, subcortical, visual pathway acts as an alternative route, bypassing the primary visual area, activating visual cortical areas beyond striate cortex. For a long time it was assumed that the cortical visual system was functional from birth, inefficient at first but maturing rapidly(36,37). Research on animals led to the conclusion that two visual systems coexist(38). Diamond and Hall(39) and later Bronson(16) proposed that the secondary, phylogenetically older, extrageniculate visual system, which consists of a number of subcortical structures such as the superior colliculi and thalamic nuclei, may play an important role in neonatal and infantile visual behavior. This correlates with our finding of positively correlated BOLD signals in dorsal thalamic nuclei and mesencephalic tectum. This secondary system processes stimuli falling outside the central area of the retina and has direct connections to various extra-striate visual cortical areas. The involvement of this older subcortical system in visual perception of neonates has been voiced by Dubowitz et al.(18) and Snyder et al.(40), who pointed out that early visual function is predominantly subcortically controlled. A second line of evidence favoring the view that the subcortical system is involved in visual perception comes from the study of "blindsight." Patients who are reportedly blind display visual abilities, such as object avoidance, direction of motion discrimination, and light source identification,(41,42) without being conscious of the visual stimulus. In these patients the information is believed to be routed via subcortical structures to the extra-striate visual areas. Our observation that visual activity can first be located in the extra-striate cortex of neonates and infants and only later in the striate cortex agrees well with these neurologic, electrophysiologic, and imaging findings.
Abbreviations
- BOLD:
-
blood oxygenation level-dependent
- fMRI:
-
functional magnetic resonance imaging
- V1, V2:
-
primary and secondary visual cortical area
- CBF:
-
cerebral blood flow
- CBV:
-
cerebral blood volume
- ICBF:
-
local cerebral blood flow
References
Belliveau JW, Kennedy DN Jr, McKinstry RC, Buchbinder BR, Weisskoff RM, Cohen MS, Vevea JM, Brady TJ, Rosen BR 1991 Functional mapping of the human visual cortex by magnetic resonance imaging. Science 254: 716–719
Frahm J, Bruhn H, Merboldt KD, Hanicke W 1992 Dynamic MR imaging of human brain oxygenation during rest and photic stimulation. J Magn Reson Imaging 2: 501–505
Kwong KK, Belliveau JW, Chesler DA, Goldberg IE, Weisskoff RM, Poncelet BP, Kennedy DN, Hoppel BE, Cohen MS, Turner R, Cheng HM, Brady TJ, Rosen BR 1992 Dynamic magnetic resonance imaging of human brain activity during primary sensory stimulation. Proc Natl Acad Sci USA 89: 5675–5679
Turner R 1992 Magnetic resonance imaging of brain function. Am J Physiol Imaging 7: 136–145
Binder JR, Rao SM, Hammeke TA, Yetkin FZ, Jesmanowicz A, Bandettini PA, Wong EC, Estkowski LD, Goldstein MD, Haughton VM, Hyde JS 1994 Functional magnetic resonance imaging of human auditory cortex. Ann Neurol 35: 662–672
Sereno MI, Dale AM, Reppas JB, Kwong KK, Belliveau JW, Brady TJ, Rosen RR, Tootell RBH 1995 Borders of multiple visual areas in human revealed by functional magnetic resonance imaging. Science 268: 889–893
Tootell RBH, Hadjikhani NK, Vanduffel W, Liu AK, Mendola JD, Sereno MI, Dale AM 1998 Functional analysis of primary visual cortex (V1) in humans. Proc Natl Acad Sci USA 95: 811–817
Le Bihan D, Turner R, Zeffiro TA, Cuenod CA, Jezzard P, Bonnerot V 1993 Activation of human primary visual cortex during visual recall: a magnetic resonance imaging study. Proc Natl Acad Sci USA 90: 11802–11805
Indefrey P, Kleinschmidt A, Merboldt KD, Kruger G, Brown C, Hagoort P, Frahm J 1997 Equivalent responses to lexical and nonlexical visual stimuli in occipital cortex: a functional magnetic resonance imaging study. Neuroimage 5: 78–81
Binder JR, Frost JA, Hammeke TA, Cox RW, Rao SM, Prieto T 1997 Human brain language areas identified by functional magnetic resonance imaging. J Neurosci 17: 353–362
Posner MI, Pavese A 1998 Anatomy of word and sentence meaning. Proc Natl Acad Sci USA 95: 899–905
Chugani HT, Phelps ME 1986 Maturational changes in cerebral function in infants determined by 18-FDG positron emission tomography. Science 231: 840–843
Chugani HT, Phelps ME, Mazziotta JC 1987 Positron emission tomography study of human brain functional development. Ann Neurol 22: 487–497
Joeri P, Huisman TA, Ekatodramis D, Loenneker TH, Rumpel H, Martin E 1996 Functional magnetic resonance imaging (fMRI) of the visual cortex in children. Pediatr Res 40: 535
Born P, Rostrup E, Leth H, Peitersen B, Lou H 1996 Change of visually induced cortical activatin patterns during development. Lancet 347: 543
Bronson G 1974 The postnatal growth of visual capacity. Child Dev 45: 873–890
Atkinson J 1984 Human visual development over the first 6 months of life: a review and a hypothesis. Hum Neurobiol 3: 61–74
Dubowitz LM, Mushin J, De Vries L, Arden GB 1986 Visual function in the newborn infant: is it cortically mediated?. Lancet 1: 1139–1141
Atkinson J 1992 Early visual development: differential functioning of parvocellular and magnocellular pathways. Eye 129: 135
Tabuchi A 1985 Dynamic topography of visual evoked potential in children: a study of the development of the visual system. Jpn J Ophthalmol 29: 153–160
Roy MS, Barsoumhomsy M, Orquin J, Benoit J 1995 Maturation of binocular pattern visual evoked potentials in normal full-term and preterm infants from 1 to 6 months of age. Pediatr Res 37: 140–144
Huttenlocher PR, De Courten C, Garey LJ, Van der Loos H 1982 Synoptogenesis in human visual cortex: evidence for synapse elimination during normal development. Neurosci Lett 33: 247–252
Garey LJ 1984 Structural development of the visual system of man. Hum Neurobiol 3: 75–80
Ogawa S, Lee TM, Kay AR, Tank DW 1990 Brain magnetic resonance imaging with contrast dependent on blood oxygenation. Proc Natl Acad Sci USA 87: 9868–9872
Loenneker T, Hennel F, Hennig J 1996 Multislice interleaved excitation cycles (MUSIC): an efficient gradient-echo technique for functional MRI. Magn Reson Med 35: 870–874
Lindauer U, Villringer A, Dirnagl U 1993 Characterization of CBF response to somatosensory stimulation: model and influence of anesthetics. Am J Physiol 264: 1223–1228
Tsubokawa T, Katayama Y, Kondo T, Ueno Y, Hayashi N, Moriyasu N 1980 Changes in local cerebral blood flow and neuronal activity during sensory stimulation in normal and sympathectomized cats. Brain Res 190: 51–64
Joeri P, Huisman TA, Loenneker T, Ekatodramis D, Rumpel H, Martin E 1996 Reproducibility of fMRI and effects of pentobarbital sedation on cortical activation during visual stimulation. Neuroimage 3: 280
Fox PT, Raichle ME 1984 Stimulus rate dependence of regional cerebral blood flow in human striate cortex demonstrated by positron emission tomography. J Neurophysiol 51: 1109–1120
Fox PT, Raichle ME 1986 Focal physiological uncoupling of cerebral blood flow and oxidative metabolism during somatosensory stimulation in human subjects. Proc Natl Acad Sci USA 83: 1140–1144
Ogawa S, Menon RS, Tank DW, Kim SG, Merkle H, Ellermann JM, Ugurbil K 1993 Functional brain mapping by blood oxygenation level-dependent contrast magnetic resonance imaging: a comparison of signal characteristics with a biophysical model. Biophys J 64: 803–812
Meek JH, Firbank M, Elwell CE, Atkinson J, Braddick O, Wyatt JS 1998 Regional hemodynamic responses to visual stimulation in awake infants. Pediatr Res 43: 840–843
de Courten C, Garey L J 1983 Morphological development of the primary visual pathway in the child. J Fr Ophthalmol 6: 187–202
Blakemore C 1991 Sensitive and vulnerable periods in the development of the visual system. Ciba Found Symp 156: 129–147
Yamada H, Sadato N, Konishi Y, Kimura K, Tanaka M, Yonekura Y, Ishii Y 1997 A rapid brain metabolic change in infants detected by fMRI. Neuroreport 8: 3775–3778
Hershenson M 1967 Development of the perception of form. Psychol Bull 67: 326–336
Bond EK 1972 Perception of form by the human infant. Psychol Bull 77: 225–245
Schneider GE 1969 Two visual systems. Science 163: 895–902
Diamond IT, Hall WC 1969 Evolution of neocortex. Science 164: 251–262
Snyder RD, Hata SK, Brann BS, Mills RM 1990 Subcortical visual function in the newborn. Pediatr Neurol 6: 333–336
Weiskrantz L 1996 Blindsight revisited. Curr Opin Neurobiol 6: 215–220
Stoerig P, Cowey A 1997 Blindsight in man and monkey. Brain 120: 535–559
Acknowledgements
The authors thank Dr. Guido Gerig and Dr. Gabor Szekely from the Swiss Federal Technical University Zurich, Switzerland, for their cooperation in postprocessing.
Author information
Authors and Affiliations
Additional information
Supported by the Swiss National Science Foundation, Grant Nr. 31-39706.93.The authors dolorously inform the readers that P. Joeri died unexpectedly on September 10, 1996
Rights and permissions
About this article
Cite this article
Martin, E., Joeri, P., Loenneker, T. et al. Visual Processing in Infants and Children Studied Using Functional MRI. Pediatr Res 46, 135–140 (1999). https://doi.org/10.1203/00006450-199908000-00001
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199908000-00001
This article is cited by
-
Functional and structural connectivity of the visual system in infants with perinatal brain injury
Pediatric Research (2016)
-
Pediatric applications of functional magnetic resonance imaging
Pediatric Radiology (2015)
-
Challenges of Functional Imaging Research of Pain in Children
Molecular Pain (2009)
-
Advanced imaging in paediatric neuroradiology
Pediatric Radiology (2009)