Abstract
To evaluate changes in autonomic nervous system controls in response to obstructive events in future victims of sudden infant death syndrome (SIDS), we studied the polysomnographic sleep recordings of 18 future SIDS infants and those of 36 matched control infants. A heart rate autoregressive power spectral analysis was performed preceding and after the obstructive apneas. The low-frequency to high-frequency power ratio was computed to evaluate sympathovagal balance. Future SIDS victims had significantly more obstructive apneas (p = 0.001) and mixed apneas (p = 0.005) than control infants. Obstructive events occurred mainly during rapid eye movement sleep in the two populations (84.5% in future SIDS victims and 95.8% in control infants; p = NS). Comparing heart rate power spectral analysis before and after obstructive apneas in rapid eye movement sleep, high-frequency power values were significantly lower and low-frequency to high-frequency power ratios higher in future SIDS victims than in control infants. Compared with preapnea values, low-frequency to high-frequency power ratios significantly decreased after obstructive apneas in control infants (p < 0.001) but not in the future SIDS victims. When the obstructive apneas were divided according to duration, the findings were seen mainly for long apneas. In conclusion, future SIDS victims were characterized by different autonomic status and responses to obstructive apneas during sleep. These findings could be relevant to mechanisms implicated in some cases of SIDS.
Similar content being viewed by others
Main
SIDS is considered a heterogeneous clinical entity(1). Compared with control subjects, some future SIDS infants were characterized by repeated upper airway obstructions during sleep(2–4) and by symptoms attributed to ANS dysfunctions, such as tachycardia(5), bradycardia(6), higher overall HR and smaller HR variability(7–9), prolonged Q-Tc index(10,11), or excessive sweating(1,2,12). It was suggested that infants who subsequently died of SIDS suffered from both impaired vagal tone and increased sympathetic activity(5,7–9,13,14). Some authors have pointed out the importance of an intact ANS to elicit HR changes after obstructive events(15–17). The purpose of the present study was to evaluate autonomic cardiac responses to obstructive apneas in future SIDS victims and in control infants by means of autoregressive spectral analysis of the infants' HR.
METHODS
Patients. Between May 1992 and May 1995, a polygraphic sleep study was performed on 18 infants who later became victims of SIDS. These recordings were collected from 13 sleep laboratories. The sleep studies were conducted as part of different sleep research programs or to alleviate parental anxiety about sleep apnea. The present study was approved by the Institutional Review Board, and parents gave their informed consent. Of the 18 SIDS, 13 infants were males and six were preterm infants. Two preterm infants had inappropriate weight for gestational age. One infant was a sibling of a SIDS victim. No infant was being monitored at the time of death. The 18 deaths were unexpected and remained unexplained despite postmortem studies. The recording of two control infants was selected for each SIDS recording. Control and SIDS infants were matched for sex, gestational age, postnatal age, weight at birth, and sleeping position. All control infants were asymptomatic, had no family history of SIDS, and survived the first year of life uneventfully. At the time of recording, no infant had signs of infection and none were receiving medication. Data on the children's history and usual behavior were collected using a standard questionnaire before sleep monitoring was undertaken. The questionnaires were coded and analyzed with the sleep recordings.
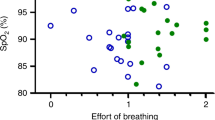
Polygraphic recordings. The infants were admitted for a night monitoring session (8-9 h). The data were collected on a computerized polygraph recording system (Morpheus system, Medatec, Belgium). The following variables were recorded simultaneously: two EEG, two electrooculograms, digastric electromyography, ECG (DII), thoracic and abdominal respiratory movements by inductive plethysmography, and airflow by means of thermistors taped under each nostril and on the side of the mouth. Oxygen saturation was recorded continuously using a transcutaneous sensor (Ohmeda Box, USA).
Data analysis. Each record was allocated a random code number. The code was disclosed after completion of the analysis. Two independent scorers analyzed the sleep recordings to ensure reliability. The two scorers had not taken part in the collection of the data and analyzed the coded recordings without knowledge of the patient's identity. Disagreements were discussed and subsequently agreed upon codes were used in data analysis. Thirty-second periods of the recordings were analyzed and categorized as NREM sleep, REM sleep, indeterminate sleep, or wakefulness according to criteria recommended in the literature(18,19). NREM refers to NREM II and III stages. Behavioral arousal was defined as opening the eyes. Gross body movements were measured by actigrams and confirmed visually. Sleep efficiency was defined as the ratio of the total sleep time divided by the total recording time, expressed as a percentage. Mean values for oxygen saturation, HR, and respiratory rate were calculated on 1-min stable sleep periods, at least 15 min after any change in body position, movement, sigh, or arousal artifact. Baseline HR and saturation in oxygen were calculated during 1-min periods preceding respiratory events. Transient arousals after obstructive events were defined through the presence of EEG changes associated with irregular respiratory and body movement(20). Sleep apneas were scored only if they lasted 3 s or more. A central apnea was scored when flat tracings were obtained simultaneously from strain gauges and thermistors. Periodic breathing was defined by the succession of at least three central apneas separated from each other by <20 s of breathing. An obstructive apnea was scored when continuous deflections were obtained from strain gauges while a flat tracing was recorded from thermistors. To avoid artificial scoring due to thermistor displacement, obstructive apneas preceded by body movements, crying, or sighs were rejected. Mixed apneas were defined as central apneas followed directly by obstructive episodes and were scored with obstructive apneas.
Selection of obstructive apneas. Two obstructive events were selected in the recordings of each infant. Obstructive apneas were selected with similar characteristics in the two populations: time of night, sleep stage, duration, prior apnea oxygen saturation, postapnea desaturation, and postapnea HR deceleration.
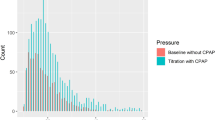
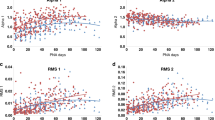
HRSA. Digitized ECG signals were sampled at 300 Hz. Periods of 256 successive RR intervals were selected preceding the event and after the end of the obstructive apnea (Figs. 1–3). Premature ventricular contractions or artifactual RR intervals due to gross body movements or arousals were eliminated by visual analysis of the HR data before HRSA was performed. A HRSA of the trendgram was calculated for each period, and center frequency and power of each spectral component were obtained(21,22) (Figs. 2 and 3). Two major peaks were recognizable: a LF component defined by center frequency of 0.1 Hz Eq (0.04-0.15 Hz Eq) and a HF component defined by a center frequency of 0.4 Hz Eq (>0.15-2 Hz Eq)(21). Respiratory frequency during the selected period was measured manually after being printed on paper. For each 256-RR interval period, the major component in the LF band of the HR spectrum was related to the major component in the HF band corresponding to the mean respiratory frequency as determined by analysis of breathing rate. The ratio of LF/HF powers for each episode was calculated as an index of sympathovagal interaction(23). Because of the possibility of variation of the breathing rate within the selected segment, we compared the normalized powers obtained by this method (major component of the band) with the results obtained when the totality of the band was studied: LF band, 0.04-0.15 Hz Eq; HF band, >0.15-2 Hz Eq. Spectral components were represented as RR intervals (in ms), power (in ms2), bandwidth (in Hz Eq), and normalized power values obtained by dividing the power of the period by the total power component (in percent) after subtraction of the direct current component(21,22). The optimal autoregressive model order was determined by minimizing the value of the final predictor error(24). Stationary was confirmed by a pole diagram analysis(21,22).
Polysomnographic recording of a mixed apnea. From surface ECG, time series of RR intervals were calculated as a function of beats before (2) and after the end (3) of the mixed apnea. EMG, electromyogram; EOG1, 2, electrooculogram 1, 2; F3-C3 and F4-C4, bipolar EEG; VTH and VAB, thoracic and abdominal volumes; NAF, nasal thermistor; SAO2, oxygen saturation.
Statistical evaluation. The Friedman test was applied to compare the future SIDS victim and the two control subjects. When the test was significant, Wilcoxon matched-pairs signed rank test was used to compare the SIDS case with each of the matched control subjects and to compare the two control subjects with each other. The test was considered positive when significant differences were observed between the SIDS case and the two control subjects, but not between the two control subjects(25). Because of the fewer number of obstructive events in the control infants, Wilcoxon nonpaired matched test was applied to compare the spectral analysis values between the future SIDS victims and the control group. The medians presented in the tables are those obtained by pooling the two control subjects. The χ2 test was used with 2 × 2 tables.
RESULTS
General characteristics of the population. Due to the study design, no differences existed between the future SIDS and the control subjects for the following variables: sex, gestational age, postnatal age, weight at birth, and sleeping position. Mothers of future SIDS victims were younger [median 24 y for SIDS infants and 29 y in control subjects; range 20-43 y (p = 0.038)] and more frequently smoked during pregnancy [4/18 for SIDS infants and 3/36 for control infants (p = 0.003)] (Table 1).
Sleep characteristics. After sleep recordings, no significant differences were seen between the two groups of infants for the following variables: total recording time (median duration 480 min; range 330 to 510 min), total sleep time (median 347 min for SIDS infants, 370 min for control infants; range 201 to 478 min), sleep efficiency (median 80.2% for SIDS infants, 77.25% for control infants; range 47.5-100%), NREM sleep (median 29.95% for SIDS infants, 32% for control infants; range 16.6-45.5%), REM sleep (median 46.05% for SIDS infants, 42% for control infants; range 22.7-69.8%), sleep stage changes (median 15.5 for SIDS infants, 17 for control infants; range 11-23), movements (median 4.65% for SIDS infants, 3.75% for control infants; range 0-17.4%), arousals (median 15.4% for SIDS infants, 17.8% for control infants; range 0-49.9), frequency of central apneas per infant (median 27 for SIDS infants, 32.5 for control infants; range 3-106), maximum duration of central apneas (median 8 s for SIDS infants, 7 s for control infants; range 4.1-18.9 s), basal HR in NREM sleep [median 133 beats per minute (bpm) for SIDS infants, 127.3 bpm for control infants; range 110-155 bpm], basal HR in REM sleep (median 136 bpm for SIDS infants, 129 bpm for control infants; range 111-156 bpm), basal breathing rate in NREM sleep (median 39 breaths per minute for SIDS infants, 31 breaths per minute for control infants; range 22-62 breaths per minute), basal breathing rate in REM sleep (median 43 breaths per minute for SIDS infants, 36 breaths per minute for control infants; range 25-62 breaths per minute), and oxygen saturation values (median 93.7% for SIDS infants, 95.2% for control infants; range 86.5-98.6%). After apneas, no differences were seen for the percentage of HR deceleration associated with central or obstructive events or for the percentage of oxygen desaturation associated with both types of apneas.
Characteristics of obstructive events. As shown in Table 2, more future SIDS than control infants had obstructive or mixed apneas. Each future SIDS victim had more obstructive and mixed episodes than their matched control subjects. No significant differences were found between the two groups for the duration of the obstructive or mixed apneas. Obstructive events occurred mainly during REM sleep in the two populations (84.5% in future SIDS victims and 95.8% in control infants; p = NS). All obstructive events were thus selected during REM sleep.
Two obstructive events were selected in each SIDS infant with obstructive events (34 events) and, according to the number of obstructive events, zero to two obstructive events were selected in each control subject (37 events). There were 16 control infants and one future SIDS infant without obstructive event (p = 0.009), three control infants and no future SIDS infant with one obstructive event (p = NS), and 17 control infants and 17 future SIDS infants with at least two obstructive events (p = 0.002). No difference was seen between the two groups for the duration of obstructive events (median 5.2 s in future SIDS victims and 5.1 s in control infants; range 3.2-12.1 s) or oxygen saturation values before obstructive events (median 98%; range 93-100%). After the obstructive apneas, no differences were seen for oxygen saturation values (median 94.5% in future SIDS victims and 96% in control infants; range 82-99%), the percentage of oxygen desaturation (median 2.5% in future SIDS victims and 3% in control infants; range 3-15%), the HR values (median 120 bpm for future SIDS victims and 112 bpm for control group; range 60-153 bpm), or the percentage of HR decelerations (median 23.5% for SIDS infants and 30.5% for control infants; range 9-81%). No differences were noted in the frequency of transient arousals after obstructive events (26/34 in future SIDS victims and 29/37 in the control group). There was no difference in the ratio of obstructive to mixed apneas in the two populations (20/14 for future SIDS infants and 19/16 for control infants). There was no difference in the nycterohemeral selection of obstructive events (median 0511 h for SIDS infants and 0555 h for control infants; range 0003-2357 h). The obstructive events in REM sleep were divided according to duration (3 to <5 s, 5 to <10 s, and >10 s). There were 15 apneas of <5 s in SIDS infants and 18 in control infants, 19 apneas of 5 to 10 s in SIDS infants and 17 in control infants, no apnea of >10 s in SIDS infants and two in control infants (NS).
Comparison of HRSA between SIDS and control infants. When both populations were compared before and after the obstructive apneas by means of HRSA (Table 3), HF powers and HF normalized powers were significantly lower, and the LF/HF power ratios higher in future SIDS victims than in control subjects. After the obstructive apneas, these differences between the two populations were greater than in the preapnea situation. HF bandwidth was larger in the future SIDS victims than in the control infants before obstructive apneas. Comparing the HRSA, no difference was seen between the two groups for total spectrum power, RR intervals, normalized or nonnormalized LF powers, and LF bandwidth between the two populations, either before or after the obstructive sleep events. The results were similar when the major components within the band or the totality of the spectral band were studied.
Comparison of HRSA before and after obstructive events. Comparing HR power values for apnea-associated changes, significantly lower LF/HF power ratios were measured after obstructive apneas in control infants, whereas no difference was seen in future SIDS victims (Table 3). Of the 37 obstructive episodes studied in control infants, 29 were associated with a decrease in LF/HF energy and eight with an increase. Of the 34 obstructive episodes studied in the future SIDS group, 18 were followed by a decrease and 16 by an increase in LF/HF power (p = 0.044). After the apneas, there was a significant decrease in LF normalized power in the two populations. Total spectrum power increased significantly as well as HF power in control subjects after obstructive apneas. These differences were not found in future SIDS victims. When the obstructive events were partitioned according to duration (Table 4), these differences were found mainly in the long apneas. No differences were seen when the changes in HRSA associated with obstructive events were studied in relation to sleep position, sex, prematurity, or maternal smoking habit.
DISCUSSION
The obstructive apneas seen during REM sleep were followed by significantly more frequent decreases in LF/HF ratio in the control than in the future SIDS infants. The difference in autonomic reactions cannot be attributed to experimental conditions such as age, body position during sleep(26), time of night, feeding times, characteristics of obstructive events (duration, time, saturation, or HR changes), or sleep fragmentation(27).
We must admit several limitations to the present study. First, we hypothesized that before and after obstructive apneas, the HR varies in a sinusoidal fashion, a prerequisite for the application of Fourier analysis. For this reason, an autoregressive spectral analysis method was used because it was well suited for the analysis of short time series(28). Second, no spectral analysis was performed on respiratory movements, and cross-spectral analysis of respiration and HR changes were not evaluated(28). We studied the major component in the HF band corresponding to the mean respiratory frequency and the HF band to consider the breathing variations within the selected segment. When comparing future SIDS victims with control infants, HF energy was seen to decrease during REM sleep. These results are similar to those reported by Kluge(14) with the use of cross-spectral analysis of respiration and HR changes. Third, the interpretation of the LF/HF ratio is complex. Within the LF range, the HR fluctuations depend on both symphathetic and parasympathetic controls. The band under 0.09 Hz represents fluctuations of vasomotor or thermal origin(29); the mild-frequency band (between 0.1 and 15 Hz) has been related to baroreceptor control(30). The power in these two frequency bands usually merges into one wide peak. The respiratory peak has been shown to be mainly vagally mediated(31). The vagal efferent fibers could not originate in a common brainstem structure. The HF peak that corresponds to the respiratory sinus arrhythmia would reflect only the part of the vagal efferent system from the nucleus ambiguus(32). Spectral HR techniques do not permit evaluation of the influence of the other branch of the parasympathetic system from the dorsal motor nucleus(32), although it was suggested that competition between the two branches of the parasympathetic system could be responsible for autonomic dysfunction(32,33).
With these restrictions in mind, the present study highlights that after OSA, future SIDS victims do not exhibit the decrease in LF/HF ratio seen in control infants.
In OSA adult patients, sleep apneas are associated with marked hemodynamic oscillations consisting of bradycardia during apneas, followed by a transient increase in HR and arterial pressure with resumption of breathing(34–37). In OSA adults, muscle sympathetic nerve activity recorded from peroneal nerve revealed that apneas were accompanied by an increase in sympathetic activity that resolved on resumption of breathing(34,36). This postapnea decrease in sympathetic activity was attributed to lung inflation and to changes in arterial baroreflex activity(38).
The cardiac responses observed in the control infants could thus result from various changes in autonomic controls, such as decreases in orthosympathetic tone, or increases in parasympathetic activity or a combination of both. The lack of decrease in LF/HF ratio measured in the future SIDS victims could result from an impairment of ANS control, as postulated in these infants(5,7–9,13,39). The future SIDS victims had lower values of normalized and nonnormalized HF powers and higher values for the LF/HF power ratios than the control subjects. Similar findings were reported previously(14,40,41). Such potential HR dysautonomia could reduce the electrical stability of the heart(7,39) and precipitate ventricular fibrillation and sudden cardiac death(42,43). An intact adrenal function is necessary for gasping and surviving from anoxia in newborn rats(44). Such response is blunted in growth-retarded newborn rats with high basal sympathoadrenal activity(45). An attenuated vagal or an increased sympathetic activity could reduce behavioral adaptation to environmental stresses(33,46). An autonomic dysautonomia could explain the inhibition of some homeostatic reflexes, as reported in some future SIDS infants, including a deficiency in ventilatory and arousal responsiveness to hypercarbia or hypoxia(47,48), a decrease in consistent sustained HR changes(9), or an increased frequency of obstructive events(3,4).
CONCLUSION
Compared with control infants, future SIDS victims were characterized by different autonomic status and autonomic responses to obstructive apneas during sleep. It could be hypothesized that these characteristics may be associated with a higher vulnerability to external or endogenous stress factors.
Abbreviations
- ANS:
-
autonomic nervous system
- HF:
-
high frequency
- HR:
-
heart rate
- HRSA:
-
heart rate power spectral analysis
- LF:
-
low frequency
- LF/HF:
-
low-frequency to high-frequency
- NREM:
-
non-rapid eye movement
- REM:
-
rapid eye movement
- OSA:
-
obstructive sleep apnea
- SIDS:
-
sudden infant death syndrome
References
Valdes-Dapena MA 1980 Sudden infant death syndrome: a review of the medical literature 1974-79. Pediatrics 66: 597–614
Tonkin S 1975 Sudden infant death syndrome: hypothesis of causation. Pediatrics 55: 650–660
Roberts JL, Mathew OP, Thach BT 1981 Upper airway obstruction and the sudden infant death syndrome. Pediatr Res 15: 729
Kahn A, Groswasser J, Rebuffat E, Sottiaux M, Blum D, Foerster M, Franco P, Alexander M, Bachy A, Richard P, Verghote M, Le Polain D, Wayenberg JL 1992 Sleep and cardiorespiratory characteristics of infant victims of sudden death: a prospective case-control study. Sleep 15: 287–292
Southall DP, Stevens V, Franks CI, Newcombe RG, Shinebourne Ea, Wilson AJ 1988 Sinus tachycardia in infants subsequently suffering from the sudden infant death syndrome. Eur J Pediatr 147: 74–78
Kelly DH, Golub H, Carley D, Shannon DC 1986 Pneumograms in infants who subsequently died of the sudden infant death syndrome. J Pediatr 109: 249–254
Matthews TG 1984 Is autonomic control a factor in some cases of sudden infant death syndrome?. Lancet 1: 744
Schechtman VL, Harper RM, Kluge KA, Wilson AJ, Hoffman HJ, Southall DP 1988 Cardiac and respiratory patterns in normal infants and victims of the sudden infant death syndrome. Sleep 11: 413–424
Schechtman VL, Raetz SL, Harper RK, Garfinkel A, Wilson AJ, Southall DP, Harper RM 1992 Dynamic analysis of cardiac RR intervals in normal infants and in infants who subsequently succumed to the sudden infant death syndrome. Pediatr Res 31: 606–612
Schwartz PJ, Segantini A 1988 Cardiac innervation, neonatal electrocardiography, and SIDS: a key for a novel preventive strategy?. Ann NY Acad Sci 533: 210–220
Multicentre Study Group. 1983 Identification of infants destined to die unexpectedly during infancy: evaluation of predictive importance of prolonged apnea and disorders of cardiac rhythm or conduction. BMJ 286: 1091–1096
Kahn A, Van de Merckt C, Dramaix M, Magrez P, Blum D, Rebuffat E, Montauk L 1987 Transepidermal water loss during sleep in infants at risk for sudden death. Pediatrics 80: 245–250
Leistner HL, Haddad GG, Epstein RA, Lai TL, Epstein MA, Mellins RB 1980 Heart rate and heart rate variability during sleep in aborted sudden infant death syndrome. J Pediatr 97: 51–55
Kluge AK, Harper RM, Schechtman VL, Wilson AJ, Hoffman HJ, Southall DP 1988 Spectral analysis assessment of respiratory sinus arrhythmia in normal infants and infants who subsequently died of sudden infant death syndrome. Pediatr Res 24: 677–682
Briskin JG, Lehrman KL, Guilleminault C 1978 Shy-Drager syndrome and sleep apnea. In: Guilleminault C, Dement WC (eds) Sleep Apnea Syndromes. Alan R. Liss, New York, pp 317–322
Guilleminault C, Briskin JG, Greenfield MSQ, Silvestri R 1981 The impact of autonomic nervous system dysfunction on breathing during sleep. Sleep 4: 263–278
Coccagna G, Martinelli P, Zucconi M, Cirignotta F, Ambrosetto G 1985 Sleep-related respiratory and hemodynamic changes in Shy-Drager syndrome: a case report. J Neurol 232: 310–313
Anders T, Emde R, Parmelee A 1971 A Manual of Standardized Terminology, Technology and Criteria for Scoring of States of Sleep and Wakefulness in Newborn Infants. UCLA Brain Information Service/BRI Publication Office, Los Angeles, pp 8–11
Guilleminault C, Souquet M 1979 Sleep states and related pathology. In: Korobkin R, Guilleminault C (eds) Advances in Perinatal Neurology, Vol I. Spectrum Publications, New York, pp 225–247
Carskadon MA 1994 Monitoring and staging human sleep. In: Kryger MH, Roth T, Dement WC (eds) Principles and Practice of Sleep Medicine. WB Saunders, Philadelphia, pp 934–960
Baselli G, Cerutti S, Civardi S, Liberati D, Lombardi F, Malliani A, Pagani M 1986 Spectral and cross-spectral analysis of heart rate and arterial blood pressure variability signals. Comp Biomed Res 19: 520–534
Pagani M, Lombardi F, Guzzetti S, Rimoldi O, Furlan R, Pizzenelli P, Sandrone G, Malfatto G, Dell'Orto S, Piccaluge E, Turciel M, Basselli G, Cerutti S, Malliani A 1986 Power spectral analysis of heart rate and arterial pressure variabilities as a marker of sympathovagal interaction in man and conscious dog. Circ Res 59: 178–193
Malliani A, Pagani M, Lombardi F, Cerutti S 1991 Cardiovascular neural regulation explored in the frequency domain. Circulation 84: 482–492
Akaike H 1970 Statistical predictor identification. Ann Inst Stat Math 22: 203–217
Siegel S, Castellan NJ 1988 Nonparametric Statistics for the Behavioral Sciences. McGraw-Hill, New York, pp 87–95
Franco P, Groswasser J, Sottiaux M, Broadfield E, Kahn A 1996 Decreased cardiac responses to auditory stimulation during prone sleep. Pediatrics 97: 174–178
Berry RB, Kouchi KG, Der DE, Dickel MJ, Light RW 1996 Sleep apnea impairs the arousal response to airway occlusion. Chest 109: 1490–1496
Akselrod S 1992 Spectral analysis of fluctuations in heart rate and other cardiovascular parameters as a tool for the assessment of autonomic control. In: Elghozi JL, Coumel PH, Jacque O (eds) Hemodynamic and electrocardiographic exploration of the autonomic nervous system. INSERM Conference Le Vesinet, December 10-11, pp 34–70
Burton AC 1939 The range and variability of the blood flow in the human fingers and the vasomotor regulation of body temperature. Am J Physiol 127: 437–453
Schweitzer A 1945 Rhythmical fluctuations of the arterial blood pressure. J Physiol 104: 25P
Akselrod S, Gordon D, Madwed JB, Snidman NC, Shannon DC, Cohen RJ 1985 Hemodynamic regulation: investigated by spectral analysis. Am J Physiol 249:H867–H875
Porges SW 1994 Orienting in a defensive world: mammalian modifications of our evolutionary heritage. A polyvagal theory. Psychophysiology 32: 301–318
Porges SW 1992 Vagal tone: a physiologic marker of stress vulnerability. Pediatrics 90: 498–504
Shimizu T, Takahashi Y, Kogawa S, Takahashi K, Kanbayashi T, Saito Y, Hishikawa Y 1994 Muscle sympathetic nerve activity during apneic episodes in patients with obstructive sleep apnea syndrome. Electroenceph Clin Neurophysiol 93: 345–352
Bonsignore MR, Marrone O, Insalaco G, Bonsignore G 1994 The cardiovascular effects of obstructive sleep apneas: analysis of pathogenic mechanisms. Eur Respir J 7: 786–805
Leuenberger URS, Jacobs E, Sweer L, Waravdekar N, Zwillich C, Sinoway L 1995 Surges of muscle sympathetic nerve activity during obstructive apnea are linked to hypoxemia. J Appl Physiol 79: 581–588
Vanninen E, Tuunainen A, Kansanen M, Uusitupa M, Lansimies E 1996 Cardiac sympathovagal balance during sleep apnea episodes. Clin Physiol 16: 209–216
Somers VK, Mark AL, Abboud FM 1991 Interaction of baroreceptor and chemoreceptor reflex control of sympathetic nerve activity in normal humans. J Clin Invest 87: 1953–1957
Schwartz PJ, Stramba-Badiale M, Segantini A, Austoni P, Bosi G, Giorgetti R, Grancini F, Marni ED, Perticone F, Rosti D, Salice P 1998 Prolongation of the QT interval and the sudden infant death syndrome. N Engl J Med 338: 1709–1714
Schechtman VL, Harper RM, Kluge KA, Wilson AJ, Hoffman HJ, Southall DP 1989 Heart rate variation in normal infants and victims of the sudden infant death syndrome. Early Hum Dev 19: 167–181
Kitney RI 1984 New findings in the analysis of heart rate variability in infants. Automedica 5: 289–310
Schwartz PJ 1976 Cardiac sympathetic innervation and the sudden infant death syndrome: a possible pathogenetic link. Am J Med 60: 167–172
Schwartz PJ, Stone HL 1982 The role of the autonomic nervous system in sudden coronary death. Ann NY Acad Sci 382: 162–180
Yuan SZ, Runold M, Lagercrantz H 1997 Adrenalectomy reduces the ability of newborn rats to gasp and survive anoxia. Acta Physiol Scand 159: 285–292
Shaul PW, Cha CM, Oh W 1989 Neonatal sympathadrenal responses to acute hypoxia: impairment after experimental intrauterine growth retardation. Pediatr Res 25: 466–472
Skinner JE, Molnar M, Harper RM 1994 Higher cerebral regulation of cardiovascular and respiratory functions. In: Kryger MH, Roth T, Dement WC (eds) Principles and Practice of Sleep Medicine. WB Saunders, Philadelphia, pp 231–251
Shannon DC, Kelly DH, O'Connell K 1977 Abnormal regulation of ventilation in infants at risk for sudden infant death syndrome. N Engl J Med 197: 747–750
Hunt CE, McCulloch K, Brouillette RT 1981 Diminished hypoxic ventilatory responses in near-miss sudden infant death syndrome. J Appl Physiol 10: 1313–1317
Acknowledgements
The authors gratefully acknowledge the physicians of the 12 other sleep units for their collaboration: F. Alu (St. Elizabeth), F. Ravet (Citadelle), F. Lemmens (St. Jans Ziekenhuis), M. Foulon (Hôpital Civil), Y. Vandeplas (AZ VUB), F. van Horebeke (Onze Lieve Vrouw), R. Vinckx (Imelda Ziekenhuis), J. Barillari (Kiniek Maria Midelares), R. Marien (HZ St. Augustinus), F. Deneyer (Vilvoorde Ziekenhuis), J. Van Egemont (UZ Ghent), F. Michel (Clinique St. Pierre).
Author information
Authors and Affiliations
Additional information
Supported by the Fondation Scientifique Universitaire Erasme.
Rights and permissions
About this article
Cite this article
Franco, P., Szliwowski, H., Dramaix, M. et al. Decreased Autonomic Responses to Obstructive Sleep Events in Future Victims of Sudden Infant Death Syndrome. Pediatr Res 46, 33–39 (1999). https://doi.org/10.1203/00006450-199907000-00006
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199907000-00006
This article is cited by
-
Schlafbezogene Atmungsstörungen im Kindes- und Jugendalter
Monatsschrift Kinderheilkunde (2016)