Abstract
The association of GB virus type C (GBV-C) virus and clinical disease is uncertain. The role of GBV-C and (Envelope) E2 antibody in children with liver transplants has not been determined. This study's aim is to examine the prevalence of GBV-C in children with liver transplants, to assess the relationship of GBV-C to posttransplant hepatitis, and to determine the role of E2 antibodies. Sera from 34 children, preliver and postliver transplant, between 1989-1996 were tested for GBV-C (Ribonucleic acid) RNA by the automated Abbott LCx PCR assay. Anti-E2 antibodies were detected by an Abbott immunoassay. Recent posttransplant liver biopsies were examined for hepatitis. The results of the study determined that pretransplant, four children (12%) were GBV-C RNA positive. Posttransplant, 14 (42%) children were GBV-C RNA positive. The GBV-C RNA positive conversion rate was 33% (CI 17.2-55.7%). Patients received blood products from a mean of 68 ± 34 donors, which correlated with GBV-C acquisition. There was no difference in the incidence (32% versus 36%; p = 0.726) or severity (grade 2.00 versus 0.68; p = 0.126) of posttransplant hepatitis in the liver biopsies of GBV-C RNA negative and/or positive children, respectively. Pretransplant, nine of 32 children were anti-E2 positive. Posttransplant, eight of 32 children were anti-E2 positive, including five children who were anti-E2 positive pretransplant. Of nine children who were anti-E2 positive and GBV-C RNA negative pretransplant, three became GBV-C RNA positive posttransplant. The results of this study conclude that the prevalence of GBV-C infection in children postliver transplantation is high and that blood product transfusions correlate with GBV-C acquisition. Also, no correlation was found between GBV-C RNA and the incidence or severity of posttransplant hepatitis. Finally, E2 antibody presence before transplantation failed to provide complete protection from GBV-C acquisition.
Similar content being viewed by others
Main
Hepatitis viruses A through E have traditionally been associated with acute and chronic liver disease. Several lines of evidence point to the existence of additional infectious hepatitis agents(1). A small percentage (0.4%) of posttransfusion hepatitis and 18 to 20% of community-acquired hepatitis are unexplained and remain classified as non-A, non-B, non-C (NANBNC) hepatitis(2–4).
Two new viruses belonging to the Flaviviridae family, hepatitis G virus (HGV) and GB virus C (GBV-C), were discovered recently(5–7). Phylogenetic analysis indicated that HGV and GBV-C are variants of the same viral species and distantly related to hepatitis C virus(5–9).
Earlier reports raised the possibility that this new virus might play an etiologic role in NANBNC hepatitis(5–7,10,11–15). However, despite ample evidence demonstrating persistent GBV-C infection, this virus has not been linked to disease in humans or other primates, and neither seems to influence long-term morbidity and mortality nor cause postliver transplant disease in adults(16–22). It may, however, be associated with increased serum gamma glutamyl transferase (GGT) levels(23).
Most previous studies of GBV-C have been performed in adults. Studies to date in children are limited but important because viral infections such as GBV-C may produce identifiable clinical signs and symptoms not observed in adults. Immunocompromised children are known to be susceptible to GBV-C infection(24). GBV-C and hepatitis C co-infections were not causative agents for postliver transplant hepatitis in children in the United Kingdom(25).
The present study was designed to determine the prevalence of HGV/GBV-C infection in immunocompromised children with liver transplants, assess the relationship between GBV-C viremia and postliver transplant hepatitis, and examine the effect of GBV-C anti-E2 antibodies, which are believed to provide protection against acquisition of GBV-C viral infection(26–29). To our knowledge the role of E2 antibodies has not been studied previously in children.
PATIENTS AND METHODS
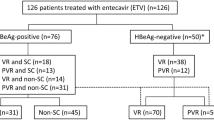
The study population consisted of children who underwent liver transplantation at the University of California, San Francisco (UCSF) or California Pacific Medical Center (CPMC) in San Francisco. Sera were collected before and after liver transplantation between April 1996 and February 1998 from 34 out of a total of 268 children (175 at CPMC and 93 at UCSF). Only 41 patients had paired sera available before and after transplant. Seven children who had evidence of hepatitis secondary to other known infectious etiologies (i.e. hepatitis C or hepatitis B) were excluded from the study. The remaining 34 patients formed the study cohort. Patient charts were reviewed for clinical data, including age, gender, ethnicity, and year of liver transplantation, indications for transplantation, and risk factors for parenteral acquisition of viral disease, such as number of blood transfusions, i.v. drug abuse, tattoos, and dialysis. Ethnicity was classified as African-American, Asian, Caucasian, Hispanic, and Other. All patients and/or their parents gave written informed consent before liver transplantation. The Committee on Human Research approved this study.
The study population included 25 girls (73%) and 9 (27%) boys. Median age at the time of transplantation was 1.25 y (range 4 months to 14.5 y). Thirteen children (38%) were Caucasian, four (12%) were Hispanic, four (12%) were Asian, two (6%) were African-American, and 11 (32%) were classified as Other, a group that included those from a multiethnic background. Indications for liver transplant included: biliary atresia(20), intrahepatic bile duct paucity(3), autoimmune hepatitis(3), cryptogenic cirrhosis(3), metabolic liver disease(3), hepatic tumor(1), and fulminant hepatic failure(1).
Pretransplant sera averaged 39.6 d before liver transplant (SD 66.4 d, range 1-300 d), and postliver transplant sera averaged 504.3 d after transplantation (SD 271.2, range 151-1 110 d). All sera were stored at -70°C. GBV-C RNA was amplified by reverse-transcription, polymerase chain reaction (60°C 30 min for 1 cycle, 94°C 40 sec, 63°C 1 min for 35 cycles, 97°C 5 min, 12°C 5 min for 1 cycle). The final step, which denatured the products and cooled them rapidly to 12°C, allowed the GBV-C probe to hybridize to the amplicon. This amplicon/probe complex was detected on the Abbott Laboratories LCx® analyzer (Abbott Park, IL) via a microparticle enzyme immunoassay (MEIA as previously reported(27,30)).
The immunoassay for detection of human antibodies elicited against GBV-C was performed at Abbott Laboratories, using a glycosylated form of GBV-C E2 protein that was purified and used as an antigenic target for detection of human anti-GBV-C(26). Serum samples were assayed by an indirect immunoassay, which used the E2 protein on a solid phase to capture antibodies from human plasma, followed by the addition of an enzyme-conjugated, antihuman antibody for color development(31).
For the purposes of this study, the definition of hepatitis was based on histologic assessment. At UCSF, protocol liver biopsies were performed weekly in the early posttransplantation period and annually thereafter. Additional liver biopsies were performed as clinically indicated (i.e. abnormal liver function tests). At CPMC, biopsies were obtained by clinical indication and stained with hematoxylin and eosin. All biopsies were reviewed, by two experienced hepatopathologists (LDF, RGK), using the same histologic scoring index for hepatitis on liver biopsy, which included portal/periportal activity, lobular activity, fibrosis, and cytopathic swelling. Each category was given a score of zero to four (0 absent, 1 minimal, 2 mild, 3 moderate, 4 severe)(32). The maximum histologic score was 16.
For statistical analyses, appropriate values were expressed as mean, median, range, and percentage. To analyze the data, the predictor variable was GBV-C RNA status and the outcome variable was hepatitis (yes/no). For the relationship between the presence or absence of GBV-C RNA and the presence or absence of hepatitis, we used the Fisher's Exact test. For the relationship between GBV-C RNA and histologic score, we used the Wilcoxon test. To evaluate the risk factors for acquiring the virus, we used a conversion rate.
RESULTS
Four of 34 children (12%) were GBV-C RNA positive pretransplant (3 had biliary atresia; 1, fulminant hepatic failure). After transplantation, 14 of 34 (42%) children were GBV-C RNA positive, including the three GBV-C RNA positive pretransplants and 11 newly acquired infections (7 biliary atresia, 1 hepatic tumor, 1 autoimmune hepatitis, 1 cryptogenic cirrhosis, and 1 fulminant hepatic failure). The GBV-C conversion rate was 33% (10 of 30), (CI 17.2-55.7%). There was no correlation between the child's sex, race, or indication for liver transplantation and GBV-C RNA conversion. The only parenteral risk factor for acquiring GBV-C was receipt of blood products. Three patients had a history of blood transfusion before liver transplantation. During and postliver transplant, patients who seroconverted received blood products from a mean of 68 donors (range 4 to 93, SD 34), compared with 43 donors (range 4 to 48, SD 29) for those patients who did not seroconvert. Donor sera were not tested for GBV-C RNA or E2 antibodies. None of the patients had tattoos, none of the patient's parents admitted to a history of drug abuse, and none of the patients required dialysis. Since the history of vertical transmission, breast-feeding, or other nonparenteral factors were not available in most of the patients' charts, these could not be analyzed.
Review of the liver biopsies indicated 23 children (67%) had evidence of hepatitis in the transplanted liver (Table 1). When comparing the grade of hepatitis(32), the average score for children with GBV-C viremia was 2.40 out of a maximum score of 16, while the average score for children without GBV-C infection was 0.63 out of 16. There was no statistical difference in the incidence or severity of hepatitis between the children who were GBV-C RNA positive compared with the GBV-C RNA negative group. (Table 1)
Overall, 26% (9 of 34) of the children were E2 antibody positive before transplant, and 23.5% (8 of 34) were E2 antibody positive after transplant.
Pretransplant E2 antibody status had no effect on the rate of viral (GBV-C RNA) acquisition. In the pretransplant patient population characterized as E2 antibody positive and GBV-C RNA negative, 33% (3 of 9) acquired GBV-C RNA positivity posttransplant. These data are not substantially different from the pretransplant patient population characterized as E2 antibody negative and GBV-C RNA negative, in which 33% (7 of 21) of the patients acquired GBV-C RNA positivity posttransplant (Table 2). The posttransplant E2 antibody positive and GBV-C RNA positive patients were of particular interest. Two of these patients were antibody positive, RNA negative pretransplant, and two were antibody and RNA negative pretransplant.
DISCUSSION
The liver transplant model provides a means of assessing the relationship of GBV-C to liver injury. Immunocompromised children with liver transplants would be more prone to virus acquisition and may be more likely to exhibit clinical manifestations of infection. Because many of the liver transplant recipients underwent protocol liver biopsies, we had the opportunity to examine these transplanted organs for evidence of hepatic injury. In our study, the prevalence of GBV-C infection in children recovering from liver transplantation was 42%, similar to that reported in other postliver transplantation populations (24-67%)(16–18,25,33). The high frequency of de novo infection may most aptly be explained by transmission of the virus through blood product transfusions given to the patients (mean of 68 donors per recipient). Based on the estimated GBV-C RNA prevalence in American blood donors (1.4-1.7%)(4,5,13,34) and the mean number of donor exposures per transplant recipient, the expected prevalence of GBV-C viremia posttransplant would be 1-(0.983)68 = 0.68 for patients who acquired GBV-C, and 0.52 for patients who did not convert. In both groups, the risk is high (more than 50%) and associated with the risk of receiving blood products. None of the patients had other parenteral risk factors for acquisition of viral disease such as i.v. drug abuse, tattoos, or dialysis. A lower prevalence rate has been reported in children who received fewer transfusions and were not immunocompromised(35,36).
Four of the children (12%) in our study were GBV-C RNA positive before transplantation and three of the four received blood product transfusions (1-3 donors each) before transplantation. A 12% pretransplant GBV-C RNA positivity rate is consistent with the rather broad pretransplant percentage (8-39%) reported for adults with liver disease(5,11,12). One of the children who was GBV-C RNA positive pretransplant had fulminant hepatic failure of unknown etiology. It has been suggested that GBV-C virus may be related to hepatic failure. Alternatively, the GBV-C RNA may have been an "innocent bystander," secondary to blood transfusion as previously suggested(2–4,11,37–40). No etiology for acquisition of GBV-C RNA positivity was identified in the fourth child, an infant, although we were unable to evaluate the possibility of vertical transmission that had been previously reported(41).
GBV-C infection in immunocompromised children apparently did not contribute significantly to the incidence or severity of postliver transplant hepatitis. Posttransplant biopsies documented that hepatitis was present in similar numbers in GBV-C RNA positive and negative children, which is similar to the results of studies in postliver transplanted adults(16–18,33) and GBV-C and hepatitis C co-infected children(25). Although patients with GBV-C viremia had slightly higher histologic scores on biopsy after transplantation, the difference was not statistically significant. However, immunosuppression may contribute to prolonged GBV-C viremia. Long-term follow up of the children in our study demonstrated that GBV-C RNA could be detected as long as 37 months after transplant, which is longer than the GBV-C viremia described in postliver transplanted adults(16,33), but shorter than that reported for children after neonatal transfusion(42) or infant cardiac surgery(36,43).
Previous studies in postliver transplanted adults indicated that the appearance of E2 antibody correlated with resolution of GBV-C viremia and possible protection against further GBV-C infection(26–28). We noted that none of our patients were E2 Ab positive or GBV-C RNA positive before transplant, which is consistent with previous observations. However, the presence or absence of pretransplant E2 antibody had no effect on the percent of patients who acquired GBV-C RNA positivity posttransplant. Exactly 33% of patients who were E2 Ab negative pretransplant or E2 Ab positive pretransplant acquired GBV-C RNA posttransplant. These results contrast with previous reports in which the presence of E2 antibody affected the rate of GBV-C RNA acquisition(26–28). Furthermore, four children lost their E2 antibodies posttransplantation and one of them acquired GBV-C infection. The ages of the patients with E2 antibodies pretransplant ranged from 4.5 mos to 14.5 y, suggesting that the E2 antibodies present in these children were not transient or due to transplacental transfer of maternal antibodies. Since posttransplant sera were obtained at the average of 504.3 d after transplant, it is highly unlikely that these patients acquired E2 Ab by means of passive transfusion via blood products.
The loss of the E2 antibodies, and the acquisition of GBV-C in the presence of E2 Ab, suggests that the immunity E2 Ab provides in immunocompromised children is neither complete or long standing after liver transplantation. We were unable to examine the differences in immunosuppression regimens to determine whether this influenced the loss of the E2 antibodies. This information may prove useful in the future development of a GBV-C virus vaccine.
In summary, the prevalence of GBV-C RNA positivity after liver transplantation in children was high. We found no correlation between GBV-C viremia and the incidence or severity of postliver transplant hepatitis. In immunocompromised children with liver transplants, E2 antibodies did not appear to afford complete protection against GBV-C, and were not present in some children after transplantation. However, the possibility of transient viremia cannot be ruled out. Further studies of this newly identified virus need to be performed in other groups of children to fully understand its clinical significance.
Abbreviations
- GBV-C:
-
GB virus type C
- HGV:
-
hepatitis G virus
- E2 Ab:
-
envelope antibody
- NANBNC:
-
non-A, non-B, non-C
References
Alter M 1989 Non-A, non-B hepatitis: sorting through a diagnosis of exclusion. Ann Intern Med 110: 583–585.
Koretz R, Abbey H, Coleman E, Gitnick G 1993 Non-A non-B post transfusion hepatitis. Looking back in the second decade. Ann Intern Med 119: 110–115.
Gonzalez A, Esteban J, Madoz P. Viladomiu L, Genesca J, Muniz E, Enriquez J, Torras X, Hemandez JM, Quer J, Vidal X, Alter HJ, Shih JW, Esteban R, Guardia J 1995 Efficacy of screening donors for antibodies to the hepatitis C virus to prevent transfusion-associated hepatitis: final report of a prospective trial. Hepatology 12: 439–445.
Alter MJ, Gallagherr M, Morris TT, Moyer LA, Meeks EL, Krawczynski K, Kim JP, Margolis HS 1997 Acute non A-E hepatitis in the US and the role of HGV. N Engl J Med 346: 741–746.
Linnen J, Wages J, Zhang-Keck ZY, Fry KE, Krawczynski KZ, Alter H, Koonin E, Gallagher M, Alter M, Hadziyannis S, Karayiannis P, Fung K, Nakatsuji Y, Shih JW, Young L, Piatak M, Hoover C, Fernandez J, Chen S, Zou JC, Morris J, Hyams KC, Ismay S, Lifson JD, Hess G, Foung SKH, Thomas H, Margolis H, Kim JP 1996 Molecular cloning and disease association of hepatitis G virus: a transfusion-transmissible agent. Science 271: 505–508.
Simons JN, Leary TP, Dawson GJ, Pilot-Matias TJ, Muerhoff AS, Schlauder GG, Desai SM, Mushahwar IK 1990 Isolation of novel virus like sequences associated with human hepatitis. Nat Med 1: 564–569.
Simons JN, Pilot-Matias TJ, Leary TP, Dawson GJ, Desai SM, Schlauder GG 1995 Identification of two flavivirus-like genomes in the GB hepatitis agent. Proc Natl Acad Sci USA 92: 3401–3405.
Balistreri WF 1997 "G" another form of viral hepatitis?. J Pediatr 131: 503–506.
Ohba K, Mizokami M, Lau JYN 1996 Evolutionary relationship of hepatitis C, pesti-, flavi- plantviruses, and newly discovered GB hepatitis agents. FEBS Lett 378: 232–234.
Leary TP, Muerhoff AS, Simons JN, Pilot-Matias TJ, Erker JC, Chalmers ML, Schlauder GG 1996 Sequence and genomic organization of GBV-C: a novel member of the Flaviviridae associated with human non A-E hepatitis. J Med Virol 48: 600–67.
Fiordalisi G, Zanella I, Mantero G, Bettinardi A, Stellini A, Paraninfo G, Cadedo G 1996 High prevalence of GBV-C infection in a group of Italian patients with hepatitis of unknown etiology. J Infect Dis 174: 181–183.
Moriyama M, Miyauchi I, Naki K, Shimizu T, Matsumura H, Segawa T, Tanaka N, Okubo H, Arakawa Y, Abe K 1996 HGV infection in Japanese patients with various forms of liver disease. Hepatology 24: 550
Fukushima S, Hyashi S, Abe K, Masaki N, Shimizu K, Isu N, Isuu N, Ohhara H, Yamasshina S, Akiyama J, Sekigawa K, Matsukawa M, Yamato S, Muraoko A, Shoda R, Matsueda K, Shimijo E, Umeda N 1996 Clinical features of acute hepatitis G. Hepatology 24: 1148
Saiz M, Sans Olmedo, Lopez-Labrador FX, Resterop JC, Rimola A, Ohara H, Yamasshina S, Akiyama J, Sekigawa K, Matsukawa M, Yamato S, Muraoko A, Shoda R, Matsueda K, Shimijo E, Umeda N 1996 Hepatitis G virus infection in fulminant hepatitis. Hepatology 24: 663
Monuz S, Alter H, Liang TJ, Nakatzuji Y, Shin J, Jeffers Reid, Marrone K, Rothstein TJ, Manzarbieta C 1996 Hepatitis G virus is present in serum of patients with fulminant hepatitis of unknown ethiology. Hepatology 24: 665
Pessoa MG, Terrault NA, Detmer J, Kolberg J, Wright TL 1997 Hepatitis G virus in patients with cryptogenic liver disease undergoing liver transplantation. Hepatology 25: 1266–1270.
Hoofnagle JH, Lombardoo M, Wei Y, Everhart J, Weisner R, Zetterman R, Yun AJ, Yang L, Kim JP 1997 Hepatitis G virus infection before and after liver transplantation. Liver Transpl Surg 3: 578–585.
Hagsma Eb, Cuypres HT, Ouw AS, Sjerps MC, Huizenga JR, Slooff MJ, Yun AJ, Yang L, Kim JP 1997 High prevalence of hepatitis G virus after liver transplantation without apparent influence on long-term graft function. J Hepatol 2: 921–925.
Kallinowski B, Buhrmann C, Seipp S, Arnold JC, Goeser T, Stremmel W, Otto G, Theilman L 1996 Infection with Hepatitis GBV-C virus after orthotopic liver transplantation. Hepatology 24: 289
Belli LS, Silini E, Ideo G 1995 HGV and post transplantation hepatitis. N Engl J Med 335: 1394–1395.
Belli LS, Silini E, Alberti AB, Asti A, Asti L, Bellati G, Rondinaara L, De Carlis, Forti D, Ideo G 1997 HGV infection and liver transplantation: virological, serological and clinical course. Hepatology 26: 1408
Fischer L, Sternecck M, Schuhmacher C, Feucht H, Malago M, Laufs R, Broelch CE 1997 HGV infection after liver transplantation has no impact on graft survival. Hepatology 26: 1513
Colombatto P, Randonr A, Civitico G, Monti G, Dolci L, Medaina N, Calleri G, Oliveri F, Baldi M, Tappero G, David E, Brunetto MR 1997 A new hepatitis G virus-like flavivirus in patients with cryptogenic liver disease associated with elevated GGT and alkaline phosphatase serum levels. J Viral Hepat 1: 55–60.
Kutdo T, Morishima T, Tsuzuki K, Orito E, Mizokami M 1996 HGV in immunosuppressed pediatric allograft recipients. [letter] Lancet 348: 751
Davidson SM, Skidmore SJ, Collingham KE, Irving WL, Hubscher SS, Kelly DA 1998 Chronic hepatitis in children after liver transplant: role of hepatitis C virus and hepatitis G virus infections. J Hepatol 28: 764–770.
Dille BJ, Surowy TK, Gutierrez RA, Coleman PF, Knigge MF, Carrich RJ, Aach RD, Hollinger F, Stevens C, Barbosa L, Memo Mosley, Dawson G, Mushahwar I 1997 An ELISA for detection of antibodies to the E2 protein of GBV-C. J Infect Dis 175: 458–461.
Hassoba HM, Terrault NA, El-Gohary AM, Scheffel C, Joe C, Brackett J, Hunt J, Lou SC, Wright TL 1997 Antibody to GBV-C second envelope glycoprotein (anti-GBV-C E2): is it a marker for immunity?. J Med Virol 53: 354–360.
Hassoba MH, Passoa MG, Terrault NA, Wright TL 1997 Anti-envelope antibodies are protective against further GBV-C infection: evidence from the transplant model. Hepatology 26: 776
Tacke M, Schmolke S, Schelueter V, Sauleda S, Tanaka E, Engel AM 1997 Humoral immune response to the E2 protein of hepatitis G virus is associated with long term recovery from infection and reveals a high frequency of hepatitis G virus exposure among healthy blood donors. Hepatology 26: 1626–1633.
Marshall RL, Cockerill J, Friedman P, Hayden M, Hodges S, Holas C, Jennings C, Jou CK, Kratochvil J, Laffler T, Lewis N, Scheffel C, Traylor D, Wang L, Solomon N 1998 Detection of GB Virus C by the RT-PCR LCx® System. J Virol Methods 73: 99–107.
Lou S, Qiu X, Tegtmeier G, Leitza S, Brackeett J, Cousineau K, Varma A, Seballos H, Kundu S, Hunt JC 1997 Immunoassay to study prevalence of antibody against GBV-C in blood donors. J Virol Methods 68: 45–55.
Scheuer P 1991 Classification of chronic viral hepatitis: a need for reassessment. J Hepatol 13: 372–374.
Dickson RC, Qian KP, Lau JY 1997 High prevalence of GBV-C infection in liver transplant recipients. Transplantation 63: 1695–1697.
Alter HJ, Nakatsuji Y, Melpolder J, Wages J, Wesley R, Shin JW-K, Shin JW, Kim JP 1997 The incidence of transfusion associated HGV infection and its relation to liver disease. N Engl J Med 336: 747–754.
Shimizu M, Osada K, Okamoto H 1996 Transfusion transmitted hepatitis G virus following open-heart surgery. [letter] Transfusion 366: 937
Huey LC, Mei-Hwei C, Yen-Hsuan N, Hong-Yuan HSU, JIA-Horng K, Pei-Jeer C 1997 HGV infection in normal and prospectively followed post-transfusion children. Pediatr Res 42: 784–787.
Ishikawa K, Hasegawa S, Hayashi N 1996 HGV is rare but possible causative agent of non A-C fulminant Hepatitis. Hepatology 24: 527
Matsui A, Momoya T, Ishikawa T, Sasaki N, Okamato 1996 GBV-C genome in two children with fulminant hepatic failure and chronic active hepatitis. Hepatology 24: 545
Tatsuoo K, Osamu Y, Toshiki Yasushi, Fumio I, Hiromitsu S 1997 Detection of GBV-C RNA in patients with non-A-E fulminant hepatitis by PCR. Hepatology 25: 1261–1265.
Yoshiba M, Okamoto H, Mishiri S 1995 Detection of GBV-C hepatitis virus genome in serum from patients with fulminant hepatitis of unknown etiology. Lancet 346: 1131–1132.
Feucht HH, Zollner B, Polywka S, Laufs R 1996 Vertical transmission of hepatitis G virus. Lancet 347: 615–616.
Berg T, Woelfle J, Schrier J, Hopf U, Lentze MJ 1997 HGV can persist in children after neonatal blood transfusion for more then 15 years without evidence of hepatitis. Hepatology 26: 785
Chen HL, Ni YH, Kao H, Wang JT, Chen DS 1997 Failure of hepatitis G virus anti-E2 response in infants: more persistent infection after mother to infant transmission?. Hepatology 26: 774
Acknowledgements
Materials and equipment for performing reverse-transcription polymerase chain reaction for GBV-C were provided by Abbott Laboratories (Abbott Park, IL). The immunoassay for detection of human antibodies elicited against GBV-C was performed at Abbott Laboratories.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Elkayam, O., Hassoba, H., Ferrell, L. et al. GB Virus C (GBV-C/HGV) and E2 Antibodies in Children Preliver and Postliver Transplant. Pediatr Res 45, 795–798 (1999). https://doi.org/10.1203/00006450-199906000-00002
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199906000-00002