Abstract
Group B streptococci (GBS) are the leading cause of pneumonia and sepsis in human newborns. Exudative pulmonary edema and alveolar hemorrhage seen in GBS pneumonia indicate vascular damage, and we reported that GBS injure lung microvascular endothelial cells (LMvEC) both in vivo and in vitro. The specific GBS factors causing LMvEC injury are uncertain, but GBS β-hemolysin activity is associated with lung epithelial cell injury. We hypothesized that GBS β-hemolysin contributes to LMvEC injury and exudative pulmonary edema. To test this hypothesis we used isogenic nonhemolytic and hyperhemolytic GBS mutants derived by transposon insertional mutagenesis from three different wild-type strains. Hemolytic titers for each strain were calculated using live GBS and Tween 80/starch-stabilized extracts of log-phase GBS. All nonhemolytic mutants lacked detectable hemolytic activity, whereas hyperhemolytic mutants produced 4-16 times the hemolytic activity of their parent strains. LMvEC injury was assayed by light microscopy, the release of lactate dehydrogenase, trypan blue nuclear staining, and Evans blue-albumin flux. Compared with the parent strains, all nonhemolytic mutants caused significantly reduced, and all hyperhemolytic mutants caused significantly greater, lactate dehydrogenase release from and trypan blue nuclear staining of LMvEC. Moreover, a nonhemolytic mutant caused reduced and a hyperhemolytic mutant caused increased Evansblue albumin flux across polar LMvEC monolayers. These findings were corroborated by light microscopic evidence of hemolysin-associated damage to the LMvEC monolayers. We conclude that GBS β-hemolysin promotes LMvEC injury and increases permeability in vitro, and speculate that GBS β-hemolysin contributes to the pathogenesis of alveolar edema and hemorrhage in early onset GBS pneumonia.
Similar content being viewed by others
Main
GBS are the most common pathogen in neonatal sepsis and pneumonia with an incidence of 1.8 to 3.2 cases/1000 live births(1,2). Early onset GBS disease is associated with significant morbidity and mortality, especially in premature infants(1–3). The primary portal of GBS entry into the neonate appears to be the lung after aspiration of infected amniotic or vaginal fluid(4–10). Multilobar pneumonia occurs in the majority of early onset cases with alveolar infiltrates and variable degrees of lung damage(7–10). GBS-induced lung endothelial cell injury is suggested by bacterial invasion into the lung capillaries, alveolar/interstitial hemorrhage, protein-rich pulmonary edema(4,7–10), and ultrastructural findings of lung capillary endothelial cell injury in some animal models of GBS sepsis(11).
We previously reported that GBS can invade and injure primary LMvEC in tissue culture and in a newborn primate model of early onset disease(12). The GBS virulence factors that promote LMvEC invasion and injury are uncertain, and the precise relationship between GBS invasion and LMvEC injury is not yet clear. As the extent of LMvEC injury is not proportional to the extent of GBS invasion(12), other virulence attributes of GBS are likely to play a major role in LMvEC injury.
Although 98-99% of GBS clinical isolates cause β-hemolysis when cultured on sheep blood agar(1,13), the role of β-hemolysin in GBS pathogenesis is only beginning to be defined. Attempts to isolate and characterize the GBS β-hemolysin have been thwarted by its instability and requirement for high molecular weight stabilizers(14–17). Hemolytic activity is not secreted into culture media in a stable form, but can be isolated from log-phase GBS culture supernatants in the presence of starch, albumin, or certain detergents(14–17). This stabilized, secreted form of GBS β-hemolysin is thermolabile, sensitive to the protease subtilisin, and inactivated by a variety of phospholipids(14–18).
There are limited data on the role of GBS β-hemolysin in lung injury. Recently, we reported that GBS β-hemolysin injures cultured A549 cells, a lung epithelial cell line(18). This β-hemolysin-induced injury is inhibited by the major phospholipid in lung surfactant, providing a rationale for increased incidence of GBS-induced lung injury in premature infants(16,18). In a neonatal rat model of pneumonia, chemical mutants devoid of β-hemolysin were less virulent and HH mutants were more virulent than the parent GBS strain(19,20). Hemolysin extracts were shown to cause increased release of β-glucuronidase into lavage fluid compared with control mice inoculated with buffer alone(19). These data suggested a potential role for β-hemolysin in GBS-induced lung injury.
We hypothesize that GBS β-hemolysin promotes LMvEC injury and loss of vascular integrity. In this study, we use transposon-derived, isogenic NH and HH mutants to test the role of β-hemolysin in GBS-induced injury to primary cultures of LMvEC. Our data show that the degree of β-hemolysin expression directly correlates with the extent of LMvEC injury and the amount of albumin flux across polar LMvEC monolayers.
METHODS
Bacterial strains. We used isogenic NH and HH mutants derived by transposon insertional mutagenesis from three GBS clinical isolates (Table 1). Prior Southern blot analysis showed that all mutants contained a single transposon insertion(18), except NH mutants COH31-C5 and COH31-C12, which possess two insertions(21). The latter two mutants share a common insertion that maps to the same genetic locus as the transposon insertion in NH mutant COH1-20(20). The laboratory Escherichia coli strain, DH5α, was used as a noninvasive control for the invasion assays(22). All bacteria were grown to mid-log phase in Todd-Hewitt broth (THB) to an OD of 0.4 at 600 nm (equal to ∼108 cfu/mL), pelleted, washed, and resuspended in RPMI media for immediate use in tissue culture assays.
Phenotypic characterization of GBS mutants. All wild-type and mutant strains were tested for group B antigen expression by latex agglutination (Streptex, Glaxo-Wellcome, London, U.K.), logarithmic growth in THB and RPMI + 1% FCS media by OD assay, production of CAMP factor on blood agar, and biochemical profile using the API 20 Strep identification kit (bioMerieux, St. Louis, MO)(18). Hyaluronidase production was tested by plating 2 µL of stationary cultures on brain, heart, infusion (BHI) agar containing 400 µg/mL hyaluronic acid (Sigma Chemical Co., St. Louis, MO) and measuring the diameter of the zone of clearing after overnight incubation at 37°C(23).
Lung microvascular endothelial cell culture. Primary piglet LMvEC (passage <3) were isolated and characterized as previously described (Cell Systems Corporation, Kirkland, WA)(12). Frozen aliquots of cells were grown to confluence on 24-well plates in serum-free defined CS-1 media with 50 µg/mL CS-GF-1 (∼105 cells/well) (Cell Systems Corporation, Kirkland, WA). Primary human lung microvascular endothelial cells (HMVEC-L, catalog #mL-2527) were obtained from Clonetics Corp. (San Diego, CA). These were grown to confluence in EGM-2 media (Clonetics) on 4-well glass chamber slides (Nunc, Inc., Naperville, IL) precoated with rat tail collagen. Twenty-four hours before inoculation with bacteria, the cell monolayers were washed and fresh RPMI + 1% FCS added to each well (2 mL for 24-well plates, 400 mL for 4-well chamber slides).
Lung endothelial cell invasion assays. A subset of NH and HH mutants were tested for LMvEC invasion as previously described(12). The assay is based on the lack of intracellular accumulation of gentamicin and penicillin in eukaryotic cells, such that extracellular bacteria are killed while intracellular bacteria survive and can be enumerated in cell lysates. Mid-log phase bacteria were inoculated onto confluent LMvEC monolayers at an MOI of 10 bacteria to 1 cell (106 cfu/105 cells), and then incubated at 37°C in 5% CO2 for 2 h (five wells per experimental condition). The monolayers were washed, and then incubated an additional 2 h in media with 5 µg/mL of penicillin and 100 µg/mL gentamicin. The percent invasion was calculated as previously described(12).
GBS hemolysin extracts. Hemolysin extracts of GBS were prepared as described by Marchlewicz and Duncan(14). GBS were grown to log-phase (OD600 = 0.4, ∼108 cfu/mL) in THB, and ∼1010 cfu of live GBS were centrifuged at 3000 × g at room temperature for 10 min, washed two times in PBS + 0.1% glucose, and then resuspended in 1 mL of PBS + 0.1% wt/vol glucose + 1% wt/vol starch and 3% vol/vol Tween 80 (hemolysin extract buffer)(14). The mixture was incubated at 37°C for 30 min, and the supernatant was removed after repeat centrifugation and stored on ice until assay of hemolytic activity within 1 h after preparation. The hemolysin extracts used in assays of LMvEC injury were obtained by the same method, except in the absence of Tween 80, which itself was shown to cause LDH release from endothelial cells.
Assay of β-hemolysin activity produced by live GBS strains and hemolysin extracts. β-hemolysin activity from all GBS strains was determined using a microtiter plate dilution assay that measures Hb release by absorbance at 420 nm(18). Data are presented as HT equal to the inverse of the greatest dilution causing 50% Hb release from sheep red blood cells. The assay was standardized to the least hemolytic parent strain, COH-1, which was assigned an HT = 1. The measurement of HT from fresh hemolysin extracts was performed in a similar fashion except dilutions were performed in hemolysin extract buffer. All GBS strains and extracts were tested in duplicate, and the experiment was performed three times.
Light microscopy of LMvEC exposed to GBS. Mid-log phase GBS were inoculated onto confluent LMvEC (HMVEC-L) monolayers on glass chamber slides at 106 or 107 cfu/105 cells (MOI = 10 or 100). The cultures were incubated at 37°C in 5% CO2 for 4 h, at which time the supernatant was removed by gentle aspiration. The monolayers were fixed by addition of 3% glutaraldehyde in 0.1 M sodium cacodylate buffer, stained by a standard hematoxylin-eosin technique, and photodocumentation performed at 100× magnification using a Nikon UFX-IIA system. Assays were performed in quadruplicate, along with E. coli DH5α and no bacteria controls.
Lactate dehydrogenase assay of LMvEC injury. LMvEC cell injury was assessed by the release of LDH activity into the culture media as previously described(12,24). Mid-log phase GBS were inoculated onto confluent LMvEC monolayers at 106 cfu/105 cells (MOI = 10), four wells per experimental condition). The cultures were incubated at 37°C with 5% CO2 for 16 h, and a 125-µL sample of supernatant was harvested from each well at 4 and 16 h for measurement of LDH (Sigma Chemical Co., diagnostic kit No. 500). All supernatants were stored at 4°C until LDH assay within 24 h. The LDH release for each condition was expressed as a ratio of released LDH (supernatant of experimental wells) to total available LDH (supernatants + cell lysates of sister wells) × 100. All GBS strains or extracts were tested in triplicate, and the experiments were performed three to five times with each strain.
For assays of LMvEC injury using fresh hemolysin extracts, a cytolytic titer was determined. Serial 2-fold dilutions of extracts (without Tween 80) were added to LMvEC and incubated for 4 h. The data are presented as cytolytic titer, which equals the greatest dilution producing 50% release of LDH compared with extract buffer control. The assay was standardized to the least hemolytic strain, COH-1, which was assigned a cytolytic titer = 1.
Trypan blue assay for LMvEC death. Confluent monolayers of LMvEC in 96-well microtiter plates (2 × 104 cells/well) were inoculated with 2 × 105 cfu of GBS (MOI = 10) in a final volume of 200 µL of fresh RPMI + 1% FCS. Cultures were incubated for 4 and 16 h at 37°C in 5%CO2. Media was then removed by gentle aspiration, and 200 µL of 0.04% trypan blue in RPMI + 1% FCS was added to each well and incubated for 5 min at 37°C in 5%CO2. The supernatant was removed, the monolayers gently washed two times with PBS, and the cells then fixed with 3% glutaraldehyde. The number of trypan blue-stained nuclei in three high-powered fields was counted. All strains were tested in triplicate, and the experiment was repeated twice.
Albumin flux across polar LMvEC monolayers. We used the method of Patterson et al.(25) to measure transendothelial albumin flux across polar monolayers of LMvEC. LMvEC were grown to confluence for 3 d on filter inserts (0.45-µm pore size, 24-well plate size; Costar, Acton, MA). On the day of experimentation, the filter inserts were transferred to 24-well plates with the abluminal wells (bottom) containing albumin-free CS-1 basal medium without phenol red. The luminal wells (top) were gently washed and fresh CS-1 basal medium + 4% BSA was added. Luminal wells were inoculated with saline, COH 31 r/s, COH31-C5, or COH31-C35 at an MOI = 10, and then incubated for 4 h. After 4 h of incubation, Evans blue albumin was added to the luminal wells at a final concentration of 67 mg/mL in 4% BSA. The filter units were then moved to new wells containing fresh albumin-free media in the abluminal chambers at 10 and 60 min after adding Evans blue albumin. Filters with no cells served as a control for maximal albumin flux (10 ± 2 µg/min between 0 and 10 min after addition of Evans blue albumin). Experimental filters that had albumin flux >5 µg/min between 0 and 10 min after adding Evans blue albumin were excluded from further data collection (a flux 10-fold greater than our intact filters). This was a rare event (∼5% of filters) and was caused by nonconfluent monolayers, or monolayers that were physically damaged during the experimental manipulations. Aliquots of media from the abluminal chamber were assayed for OD 620 nm to determine the concentration of Evans blue albumin that transited the monolayer(25). Albumin flux was calculated as the total micrograms of albumin that transited the monolayer, determined by albumin concentration × volume in bottom well, divided by the minutes of incubation. Each condition was tested in triplicate, and the experiment was performed three times.
Statistics. All data are expressed as mean ± SEM. Analysis of variance was used to compare intergroup mean values of the data, followed by Student-Neuman-Keuls correction for multiple comparisons (SPSS-PC+, v6.0, SPSS, Inc, Chicago, IL). To compare intragroup mean values over time, paired t tests were performed. A p value <0.05 was considered significant.
RESULTS
Phenotypic comparison of wild-type strains and transposon mutants. Three wild-type strains of GBS from the two most common capsular serotypes associated with neonatal infections (III and Ia) were used in our studies (Table 1). The transposon mutants were assayed for other phenotypic traits to test for potential pleiotropic effects that may influence lung endothelial cell injury. We have previously shown that 1) all wild-type strains and hemolysin mutants expressed the group B antigen as measured by latex agglutination, 2) all mutant strains had identical enzymatic and sugar fermentation patterns on the API 20 strep identification system as their respective parent strain, 3) logarithmic growth in THB and RPMI + 1% FCS was comparable for all parent and mutant strains, and 4) all HH mutants exhibited reduced CAMP factor activity compared with their parent strains (2+ versus 4+), whereas all NH mutants expressed similar CAMP factor activity compared with their parent strain(18). In addition, hyaluronidase expression was measured for the COH-1 and COH 31 r/s parent and mutant strains; all strains showed a similar 10- to 11-mm zone of hyaluronic acid degradation. Therefore, except for reduced CAMP factor expression by HH strains, the mutants do not differ in biochemical properties from their respective parent strains.
We previously proposed that GBS invasion into endothelial cells may promote injury(12,22). We therefore tested the COH-1 and COH 31 r/s mutants in β-hemolysin expression for potential pleiotropic effects on invasive properties. The subset of transposon mutants in β-hemolysin expression that was tested had similar levels of invasion compared with their respective parent strains (Table 2). Therefore, differences in the ability of such mutants to induce injury is not related to the their invasive potential.
Hemolytic activity of wild-type and mutant strains. The HT of live GBS and Tween/starch-stabilized extracts from all wild-type and mutant strains are shown in Table 1. The HT of wild-type strains COH 31 r/s and A909 organisms were 4 times greater than COH-1. NH mutants showed no detectable hemolytic activity. HH mutants produced 4-32 times the hemolytic activity of their respective parent strain. For all GBS strains, the HT of Tween/starch-stabilized extracts was comparable with that exhibited by the intact organism (Table 1).
Light microscopic evidence of GBS β-hemolysin-associated injury to LMvEC. Figure 1 shows representative light micrographs (100×) of LMvEC (HMVEC-L) monolayers stained with hematoxylin-eosin after a 4-h exposure to wild-type GBS strains COH1 and A909 and the corresponding isogenic HH and NH transposon mutants. The no bacteria control (Fig. 1A) demonstrates normal morphology of the LMvEC monolayer, composed of confluent polygonal cells with optically transparent cytoplasm. A negligible effect on monolayer integrity is seen after exposure to the control strain E. coli DH5α (Fig. 1B) at MOI = 10 bacteria/cell. At the same MOI = 10 bacteria/cell, small areas of monolayer damage (cytoplasmic retraction, alteration of nuclear structure) are noted with the weakly hemolytic wild-type strain GBS COH1 (Fig. 1C), and to a slightly greater extent with the moderately hemolytic wild-type GBS strain A909 (Fig. 1D). The HH transposon mutants derived from these strains, IN40 (Fig. 1E) and A909-HH4 (Fig. 1F), produced complete dissolution of the cytoplasmic contents and loss of nuclear structure throughout the entirely of the LMvEC monolayers at MOI = 10 bacteria/cell. In contrast, the NH mutants COH1-20 (Fig. 1G) and A909-NH2 (Fig. 1H), when introduced at an increased MOI = 100 bacteria/cell, produced only mild changes comparable with the parent strains at the lower MOI. Complete destruction of LMvEC monolayers was observed when the wild-type GBS strains COH1 and A909 or their HH derivatives were introduced at the higher MOI = 100 bacteria/cell (data not shown). From these light microscopic studies, we concluded that exposure to GBS produced morphologic evidence of injury to LMvEC monolayers, and that the degree of this injury was correlated with β-hemolysin production by the organism.
Light micrographs of LMvEC monolayers incubated with wild-type GBS strains COH-1 and A909, and respective NH and HH mutants (100 ×). Monolayers were stained with hematoxylin-eosin after a 4-h exposure to bacteria. A, No bacteria control; B, E. coli DH5α at MOI = 10; C, wild-type GBS COH-1 at MOI = 10; D, wild-type GBS A909 at MOI = 10; E, HH mutant of COH-1, IN40, at MOI = 10; F, HH mutant A909-HH4 at MOI = 10; G, NH mutant COH1-20 at MOI = 100; and H, NH mutant A909-NH2 at MOI = 100.
Hemolysin expression correlates with live GBS-induced LDH release from LMvEC. We measured the release of the eukaryotic cytoplasmic enzyme LDH as a biochemical marker of LMvEC injury. Supernatants from LMvEC monolayers infected with parent and isogenic mutant GBS strains for 4 or 16 h were assayed for percent release of total intracellular LDH activity (Fig. 2). All three parent GBS strains caused a significant amount of LDH release at 4 h, and a significantly greater increase in LDH release at 16 h compared with 4 h of infection. The NH mutants of COH-1, A909, and COH 31 r/s did not cause increased LDH release above media alone at 4 or 16 h. All HH mutants caused significantly greater LDH release at 4 h compared with their respective parent strain. All parent and HH GBS strains caused time-dependent LMvEC injury. We conclude that the hemolytic activity of the live GBS strains is directly correlated with biochemical evidence of LMvEC cytotoxicity.
Relationship between HT of isogenic GBS strains and percent total LDH release from LMvEC at 4 and 16 h of infection. Data are presented as mean ± SEM. Abbreviations for mutants are shown in Table 1. *p < 0.05. compared with media and the NH mutants, **p < 0.05 compared with media, NH mutant, and the parent strain.
Hemolysin extracts cause LDH release from LMvEC. We determined a cytolytic titer against LMvEC for the hemolysin extracts (without Tween 80) from the COH 31 r/s- and A909-derived strains (Fig. 3). All data are normalized to a cytolytic titer = 1 for COH-1. The extracts from NH mutants caused no significant LDH release from LMvEC above background levels (cytolytic titer <1). Hemolysin extracts from parent GBS strains caused significant LDH release from LMvEC compared with the NH mutants, with cytolytic titers between 4 and 8. The extracts from HH mutants caused significantly greater LDH release compared with the parent strains, with cytolytic titers of 16-32. As the cytotoxic activity of hemolysin extracts against LMvEC directly correlates with the HT for each strain, we conclude that the cytotoxic entity is the same extracellular factor that produces lysis of red blood cells.
Relationship between LMvEC cytolytic titer of hemolysin extracts and the HT of GBS strains. The GBS strain and HT are noted along the x axis vs the cytolytic titer of the hemolysin extracts against LMvEC. The cytolytic titer equals the inverse of the greatest dilution causing 50% release of LDH compared with buffer control. *p < 0.05 compared with extract buffer without Tween 80, and the NH mutants; **p < 0.05 compared with the extract buffer, NH mutants, and the parent strain (B = extract buffer).
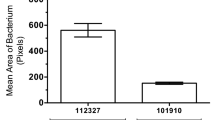
Hemolysin expression correlates with trypan blue nuclear staining of LMvEC. Trypan blue nuclear staining was used as an assay of GBS-induced LMvEC death at 4 and 16 h. The parent GBS strain COH 31 r/s caused a significant increase in LMvEC nuclear staining by trypan blue at 16 h, but not at 4 h (Fig. 4). No significant increase in trypan blue nuclear staining was observed at 4 h or 16 h after exposure to the NH mutants COH31-C5 and COH31-C12 compared with media alone controls. The HH mutant COH31-C35 caused increased trypan blue nuclear staining at 4 and 16 h compared with the parent strain. The parent and HH GBS strains caused a time-dependent increase in LMvEC death.
Relationship between HT of isogenic COH 31 r/s strains and trypan blue nuclear staining at 4 and 16 h of infection. The GBS strain abbreviations are noted in Table 1, and the HT for each strain are listed beneath the strain abbreviation at the 16-h time (the HT are the same at the 4-h time). *p < 0.05 compared with media alone and the NH mutant; **p < 0.05 compared with media, NH mutants, and the parent strain (M= media).
Hemolysin expression correlates with GBS-induced albumin flux across polar LMvEC. Transendothelial flux of Evans blue-labeled albumin has been used as a sensitive marker of injury to lung barrier cells(25,29,30). We used such an assay to test the role of hemolysin in GBS-induced permeability changes to polar LMvEC monolayers. To validate the assay with our reagents we showed that CS-1 basal media without phenol red has no significant absorption in the range of maximal Evans blue absorption, and thus caused no interference with our in vitro assays (data not shown). The absorbance of Evans blue albumin at 630 nm was linear in the range of 0-20 µg/mL (data not shown). Samples for assay of transendothelial cell albumin flux were diluted to this range.
Between 0 and 1 h after addition of Evans blue albumin into the luminal wells (4-5 h after inoculation), the polar LMvEC monolayers infected with an NH mutant (COH31-C5) on the apical side showed no increased albumin flux across to the basolateral well compared with uninfected control monolayers (Fig. 5). Transendothelial albumin flux for wells infected with a parent GBS (COH 31 r/s) strain was significantly higher than the flux for the NH mutant (COH31-C5) or the uninfected control. The HH mutant (COH31-C35) caused greater albumin flux compared with the parent GBS strain. Additional transendothelial albumin flux studies using A909, A909-NH2, and A909-HH4 showed a similar pattern (n = 2 experiments in duplicate; media, 85 ± 20 ng/min; A909, 220 ± 42 ng/min; A909-NH2, 98 ± 24 ng/min; A909-HH4, 446 ± 73 ng/min). These data suggest that GBS can alter endothelial cell permeability, and that β-hemolysin expression directly correlates with GBS-induced permeability changes to polar LMvEC monolayers.
DISCUSSION
The data presented show that GBS β-hemolysin is an important cytotoxin in GBS-induced LMvEC injury in a tissue culture model. GBS injury to primary LMvEC cultures was assessed by four methods: 1) release of the cytoplasmic enzyme, LDH, as a measure of cell plasma membrane injury, 2) trypan blue nuclear staining as an assay of endothelial cell death, and for the first time 3) light microscopy and 4) transendothelial Evans blue albumin flux as a measure of altered endothelial permeability. Isogenic NH mutants caused attenuated, whereas isogenic HH mutants caused increased, LMvEC injury, cell death, and transendothelial albumin flux compared with parent GBS strains representing the two capsular serotypes (III and Ia) most often associated with neonatal infection. Hemolytic and LMvEC cytotoxic activities of starch-stabilized cell-free extracts paralleled those of the intact organism. We did not identify phenotypic changes in the mutants other than altered β-hemolysin expression to explain the effects of transposon insertion on LMvEC injury. Our earlier studies have shown that the expression of GBS β-hemolysin is directly correlated with lung epithelial cell injury (A549 cells) in vitro(18). We have now provided data that GBS β-hemolysin acts as a pulmonary cytolysin to injure both major cellular barriers of the alveolus.
GBS also demonstrates intracellular invasion into both the lung epithelial and endothelial barriers(12,18). Our prior reports have shown that cellular invasion by GBS occurs in only ∼1-5% of the cells in tissue culture models(12,18) However, we show histologic and biochemical data that GBS β-hemolysin-producing strains can induce diffuse endothelial injury on the basis of light microscopy photomicrographs, trypan blue staining, and the extent of LDH release. Moreover, the NH GBS mutants invaded the LMvEC monolayers as well as wild-type strains, but did not produce significant monolayer injury. These findings raise interesting questions about the roles of cellular invasion and secreted products in the pathogenesis of GBS infections. Clearly, our results from this study show that β-hemolysin has cytotoxic effects beyond that observed by GBS invasion alone, and these cytotoxic properties appear to contribute more significantly to lung endothelial cell injury. Wild-type GBS strains do not produce high levels of β-hemolysin in vitro (Table 1,reference (18), and cause less severe cytotoxicity to monolayers compared with the HH isogenic strains (Fig. 1,reference (18). However, the higher density of GBS present in the lung of infected infants(8) compared with our in vitro studies with wild-type GBS may result in the accumulation of higher β-hemolysin concentrations and more severe cellular injury. In addition, conditions in the lung may up-regulate wild-type GBS β-hemolysin expression, resulting in more severe epithelial and endothelial cell injury compared with our in vitro models.
The use of isogenic mutants varying uniquely in hemolysin production indicates an important role of GBS hemolysin in the initiation of LMvEC injury compared with other GBS by-products. Theoretically, breakdown of hyaluronic acid in the extracellular matrix could facilitate lung injury by GBS(31), but the NH mutants were not injurious to the LMvEC monolayers despite producing hyaluronate lyase at wild-type levels. LTA purified from GBS is cytotoxic for a variety of human cell monolayers in tissue culture(32,33). However, the potential contribution of soluble LTA to LMvEC is uncertain because little LTA is released from the cytoplasmic membrane under normal growth conditions(34).
The GBS β-hemolysin has eluded isolation and purification to date. Some of the impediments to isolation include labile activity in the absence of high-molecular weight starch or protein stabilizers, inability to create neutralizing antibodies toward partially purified hemolysin activity, and the inability to detect a hemolytic protein band by native gel electrophoresis after partial purification(14–17,35). Previous studies have suggested the hemolytic activity is a small molecular weight protein on the basis of experiments using molecular sieve chromatography and protease sensitivity(15,35).
The histology of GBS pneumonia in human infants shows evidence of both lung epithelial and lung endothelial injury with hyaline membranes and hemorrhagic, proteinaceous pulmonary edema(4,7–11). GBS β-hemolysin has now been shown to cause injury to both the lung endothelium and epithelium in vitro(18), and thereby may contribute to the lung pathology and systemic spread of GBS after disruption of these alveolar barriers. Acute β-hemolysin-induced lung endothelial cell injury may also stimulate eicosanoid and cytokine release that contributes to GBS-induced lung inflammation and injury(12,36). Although in vivo injury to the alveolar barrier is presumably multifactorial, our in vitro studies in the absence of inflammatory cells suggest a direct role for GBS hemolysin in eukaryotic cellular injury. The GBS β-hemolysin-induced increase in lung endothelial cell permeability may in part explain the proteinaceous pulmonary edema in GBS pneumonia.
Prior studies in erythrocytes and lung epithelial cells suggest that GBS β-hemolysin is a pore-forming toxin(18,35). Poreforming bacterial cytotoxins contribute to lung injury and pneumonia in other models, including the Staphylococcus aureus α-toxin(37,38), E. coli hemolysin(39), Streptococcus pyogenes streptolysin O(40) and pneumolysin(41–43). Streptococcus pneumonia pneumolysin causes both epithelial and endothelial cell injury in vitro, and is important for virulence in a murine model of pneumonia(43). The pneumolysin molecule contains two characterized functional domains-a hemolysin and a complement-activating region. The hemolytic domain is important in acute lung injury and the development of proteinaceous pulmonary edema(43).
There are limited data on the role of β-hemolysin on virulence in animal models of GBS disease. Intravenous infusion of partially purified GBS hemolysin extracts into rabbits or rats caused shock and increased mortality compared with S. pneumonia streptolysin S(44). However, s.c. or i.v. injection of NH mutants into neonatal rats or piglets, respectively, showed the same LD50 and altered pathophysiology as the parent GBS strain(21,45). These models of systemic GBS infection bypass the alveolar barrier, and do not test the role of hemolysin in lung alveolar injury during the acute events of GBS infection, i.e. aspiration of infected amniotic fluid. In contrast, intranasal inoculation of mice with chemical-induced hemolysin mutants of GBS showed that the degree of hemolysin production was inversely correlated with LD50 and time to death(19). In addition, lung lavage levels of β-glucuronidase, a marker of cellular injury, were increased from mice inoculated intranasally with hemolysin extracts compared with buffer alone. Our preliminary data in a neonatal rate model shows that after intrathoracic injection, the nonhemolytic isogenic A909-NH2 mutant has a 1000-fold increased LD50 compared with the parent strain A909 (5 × 106 cfu versus 5 × 103 cfu)(20).
We conclude that GBS β-hemolysin expression directly correlates with the extent of lung endothelial cell injury in vitro. GBS β-hemolysin-mediated endothelial cell injury may contribute to the pathophysiology of neonatal pneumonia and proteinaceous pulmonary edema. Loss of vascular integrity may allow access of the organism to the bloodstream where-upon bacteremic spread and sepsis syndrome can ensue. Premature neonates deficient in pulmonary surfactant phospholipids, a known inhibitor of GBS hemolytic and cytolytic activity(18), are at greater risk of early onset GBS pneumonia and sepsis. Future studies will seek to isolate and clone the GBS β-hemolysin to more closely study its role in neonatal pneumonia and the possibility of therapeutic interventions to block its cytotoxic properties.
Abbreviations
- GBS :
-
group B streptococcus
- HT :
-
hemolytic titer
- HH :
-
hyperhemolytic
- LDH :
-
lactate dehydrogenase
- LMvEC :
-
lung microvascular endothelial cells
- MOI :
-
multiplicity of infection
- NH :
-
nonhemolytic
- OD :
-
optical density
- LTA :
-
lipotechoic acid
- LD 50 :
-
median lethal dose
References
Baker CJ, Edwards MS 1995 Group B streptococcal infections. In: Remington J, Klein JO (eds) Infectious Diseases of the Fetus and Newborn Infant, 4th Ed. W.B. Saunders, Philadelphia, 980–1054.
Zangwill KM, Schuchat A, Wenger JD 1992 Group B streptococcal disease in the United States, 1990: report from a multistate active surveillance system. MMWR CDC Surveill Summ 41(SS-6), N. ov 20: 25–32.
Weisman LE, Stoll BJ, Cruess DF, Hall RT, Merenstein GB, Hemming VG, Fischer GW 1992 Early-onset group B streptococcal sepsis: a current assessment. J Pediatr 121: 428–433.
Vollman HJ, Smith WL, Ballard ET, Light IJ 1976 Early onset group B streptococcal disease: clinical and roentgenographic and pathologic features. J Pediatr 89: 199–203.
Baker CJ 1976 Early onset group B streptococcal disease. J Pediatr 93: 124–125.
Eickhoff TC, Klein JO, Daly AL, Ingall D, Finland M 1964 Neonatal sepsis and other infections due to group B α-hemolytic streptococci. N Engl J Med 271: 1221–1228.
Becroft DMO, Farmer K, Mason GH, Stewart JH 1976 Perinatal infections by group B beta-hemolytic streptococcal infections in infants. Br J Obstet Gynecol 83: 960–965.
Rubens CE, Raff HV, Jackson JC, Chi EY, Bielitzki JT, Hillier SL 1991 Pathophysiology and histopathology of group B streptococcal sepsis in Macaca nemestrina primates induced after intraamniotic inoculation: evidence for bacterial cellular invasion. J Infect Dis 164: 320–330.
Katzenstein A, Davis C, Braude A 1976 Pulmonary changes in neonatal sepsis due to group B beta-hemolytic streptococcus: relation to hyaline membrane disease. J Infect Dis 133: 430–435.
Hemming VG, McCloskey DW, Hill HR 1976 Pneumonia in the neonate associated with group B streptococcal septicemia. Am J Dis Child 130: 1231–1233.
Rojas J, Larsson LE, Hellerqvist CG, Brigham KL, Gray ME, Stahlman MT 1983 Pulmonary hemodynamic and ultrastructural changes associated with group B streptococcal toxemia in adult sheep and newborn lambs. Pediatr Res 17: 1002–1008.
Gibson RL, Soderland C, Henderson WR, Chi EY, Rubens CE 1995 Group B streptococci injure lung endothelium in vitro: increased invasion and eicosanoid production with microvascular compared to pulmonary artery cells. Infect Immun 63: 271–279.
Facklam RR, Padula JF, Thacker LG, Wortham EC, Sconyers BJ 1974 Presumptive identification of groups A, B, and D streptococci. Appl Microbiol 27: 107–113.
Marchlewicz BA, Duncan JL 1980 Properties of a hemolysin produced by group B streptococci. Infect Immun 30: 805–813.
Tsaihong JC, Wennerstrom DE 1983 Effect of carrier molecules on production and properties of extracellular hemolysin produced by Streptococcus agalactiae. Curr Microbiol 9: 333–338.
Tapsall JW, Philips EA 1991 The hemolytic and cytolytic activity of group B streptococcal hemolysin and its possible role in early onset group B streptococcal disease. Pathology 23: 139–144.
Dal MC, Montiel H 1983 Hemolysin produced by group B streptococcus agalactiae. FEMS Microbiol Lett 16: 89–94.
Nizet V, Gibson RL, Chi EY, Framson PE, Hulse M, Rubens CE 1996 Group B streptococcal β-hemolysin expression is associated with injury to lung epithelial cells. Infect Immun 64: 3818–3826.
Wennerstrom DE, Tsaihong JC, Crawford JT 1985 Evaluation of the role of hemolysin and pigment in the pathogenesis of early onset group B streptococcal disease. In: Kimura Y, Kotami S, Shiokawa Y (eds) Recent Advances in Streptococci and Streptococcal Diseases. Bracknell, U.K., Reedbooks, 155–156.
Nizet V, Gibson RL, Rubens CE 1997 The role of group B streptococci beta-hemolysin expression in newborn lung injury. Adv Exp Med Biol 418: 627–630.
Weiser JN, Rubens CE 1987 Transposon mutagenesis of group B streptococcus beta-hemolysin biosynthesis. Infect Immun 55: 2314–2316.
Gibson RL, Lee MK, Soderland C, Chi EY, Rubens CE 1993 Group B streptococci invade endothelial cells: type III capsular polysaccharide attenuates invasion. Infect Immun 61: 478–485.
Smith RF, Willet NP 1968 Rapid plate method for screening hyaluronidase and chondroitin sulfatase-producing microorganisms. Appl Microbiol 16: 1434–1436.
Meyrick B, Hoover R, Jones MR, Berry LC Jr, Brigham KL 1989 In vitro effects of endotoxin on bovine and sheep lung microvascular endothelial cells. J Cell Physiol 138: 165–174.
Patterson CE, Rhoades RA, Garcia JGN 1992 Evans blue dye as a marker of albumin clearance in cultured endothelial monolayer and isolated lung. J Appl Physiol 72: 865–873.
Rubens CE, Kuypers JM, Heggen LM, Kasper DL, Wessels MR 1991 Molecular analysis of the group B streptococcal capsule genes. In: Dunny GM, Cleary PP, McKay LL (eds) Genetics and Molecular Biology of Streptococci, Lactococci, and Enterococci. American Society for Microbiology, Washington, DC, 179–183.
Rubens CE, Wessels MR, Heggen LM, Kasper DL 1987 Transposon mutagenesis of type III group B streptococcus: correlation of capsule expression with virulence. Proc Natl Acad Sci U S A 84: 7208–7212.
Framson PE, Nittayajarn A, Merry J, Youngman P, Rubens CE 1997 New genetic techniques for group B streptococci: high-efficiency transformation, maintenance of temperature-sensitive pWV01 plasmids, and mutagenesis with Tn917. Appl Environ Microbiol 63: 3539–3547.
Chang SW, Ohara N 1993 Increased pulmonary vascular permeability in rats with biliary cirrhosis: role of thromboxane A2. Am J Physiol 264:L245–L252.
Senaldi G, Vesin C, Chang R, Grau GE, Piquet PF 1994 Role of polymorphonuclear neutrophil leukocytes and their integrin CD11a (LFA-1) in the pathogenesis of severe murine malaria. Infect Immun 62: 1144–1149.
Pritchard DG, Lin B, Willingham TR, Baker JR 1994 Characterization of the group B streptococcal hyaluronate lyase. Arch Biochem Biophys 315: 431–437.
Miyazaki S, Leon O, Ponos C 1988 Adherence of Streptococcus agalactiae to synchronously growing human cell monolayers without lipotechoic acid involvement. Infect Immun 56: 505–512.
Goldschmidt JC, Ponos C 1984 Techoic acids of Streptococcus agalactiae: chemistry, cytotoxicity, and effect on bacterial adherence to human cells in tissue culture. Infect Immun 43: 670–677.
Mattingly SJ, Johnston BP 1987 Comparative analysis of the localization of lipotechoic acid in Streptococcus agalactiae and Streptococcus pyogenes. Infect Immun 55: 2383–2386.
Marchlewicz BA, Duncan JL 1981 Lysis of erythrocytes by a hemolysin produced by a group B streptococcus sp. Infect Immun 34: 787–794.
Brown Z, Gerritsen ME, Carley WW, Strieter RM, Kunkel SL, Westwick J 1994 Chemokine gene expression and secretion by cytokine-activated human microvascular endothelial cells: differential regulation of monocyte chemoattractant protein-1 and interleukin-8 in response to interferon-gamma. Am J Pathol 145: 913–921.
Seeger WR, Birkemeyer RG, Ermert L, Suttorp N, Bhakdi S, Duncker HR 1990 Staphylococcal alpha-toxin-induced vascular leakage in isolated perfused rabbit lungs. Lab Invest 63: 341–349.
Bhakdi S, Tranum-Jensen J 1991 Alpha-toxin of Staphylococcus aureus. Microbiol Rev 55: 733–751.
Ermert L, Rousseau S, Schutte H, Birkemeyer RG, Grimminger F, Bhakdi S, Duncker HR, Seeger W 1992 Induction of severe vascular leakage by low doses of Escherichia coli hemolysin in perfused rabbit lungs. Lab Invest 66: 362–368.
Bhakdi S, Tranum-Jensen J, Sziegoleit A 1985 Mechanisms of membrane damage by streptolysin-O. Infect Immun 47: 52–60.
Rubins JB, Duane PG, Charboneau D, Janoff EN 1992 Toxicity of pneumolysin to pulmonary endothelial cells in vitro. Infect Immun 60: 1740–1746.
Rubins JB, Duane PG, Clawson D, Charboneau D, Young J, Niewoehner DE 1993 Toxicity of pneumolysin to pulmonary alveolar epithelial cells. Infect Immun 61: 1352–1358.
Rubins JB, Charboneau D, Fasching C, Berry AM, Paton JC, Alexander JE, Andrew PW, Mitchell TJ, Janoff E 1996 Distinct roles for pneumolysin's cytotoxic and complement activities in the pathogenesis of pneumococcal pneumonia. Am J Respir Crit Care Med 153: 1339–1346.
Griffiths BB, Rhee H 1992 Effects of haemolysins of group A and group B streptococci on cardiovascular system. Microbios 69: 17–27.
Gibson RL, Redding GJ, Truog WE, Henderson WR, Rubens CE 1989 Isogenic group B streptococci devoid of capsular polysaccharide or -hemolysin: pulmonary hemodynamic and gas exchange effects during bacteremia in piglets. Pediatr Res 26: 241–245.
Acknowledgements
The authors thank Paul Framson for developing a Tn917 mutagenesis protocol for GBS and Moni Guha for her expert technical assistance.
Author information
Authors and Affiliations
Additional information
Supported by NIH grants AI 01451 (V.N.), and AI 30068 and AI 25152 (C.E.R.), an American Lung Association Edward Livingston Trudeau Award (R.L.G.), and an American Lung Association Research Grant RG-020-N (V.N.).
Rights and permissions
About this article
Cite this article
Gibson, R., Nizet, V. & Rubens, C. Group B Streptococcal β-Hemolysin Promotes Injury of Lung Microvascular Endothelial Cells. Pediatr Res 45 (Suppl 5), 626–634 (1999). https://doi.org/10.1203/00006450-199905010-00003
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199905010-00003
This article is cited by
-
Population genomics of Group B Streptococcus reveals the genetics of neonatal disease onset and meningeal invasion
Nature Communications (2022)
-
Phenotypic changes in group B streptococci grown in the presence of the polyols, erythritol, sorbitol and mannitol
BMC Microbiology (2021)
-
Effect of Alcohol on Bacterial Hemolysis
Current Microbiology (2008)
-
The pathogenesis of streptococcal infections: from Tooth decay to meningitis
Nature Reviews Microbiology (2003)