Abstract
Persistent diarrhea, vomiting, and dehydration are symptoms often seen in patients suffering from food allergy after chronic antigen exposure; however, the precise mechanisms involved have not been well defined. In an effort to clarify the mechanisms of the chronic intestinal changes attributable to genuine IgE-mediated anaphylactic reactions induced by orally administered antigen, a mouse model was established by s.c. implantation of a murine hybridoma capable of producing monoclonal antitrinitrophenyl IgE antibody, and the morphologic and immunologic changes occurring in the intestine upon chronic antigen exposure were investigated. In the early stage after ingestion of the antigen, diarrhea and noticeable infiltration of mast cells as well as eosinophils into the lamina propria were observed. A substantial increase in serum histamine levels as well as an increase in leukotriene C4 synthesis in the jejunal mucosa were observed 1 h after antigen challenge. Also, the synthesis of leukotriene B4 was significantly elevated for up to 9 h after antigen challenge. The expression of both intercellular adhesion molecule-1 (ICAM-1) on mucosal vascular endothelial cells and IAd on epithelial cells was markedly enhanced, and noticeable infiltration of eosinophils and lymphocytes was also confirmed in the mouse model after chronic antigen exposure. These findings suggest that oral antigen exposure induces anaphylactic reactions in the intestine mediated by mast cells and eosinophils in response to the IgE-antigen complex in the early phase, and also induces lymphocyte migration after chronic antigen exposure.
Similar content being viewed by others
Main
Diarrhea and vomiting are often seen in infants and young children as the symptoms of food allergy caused by ingested foods. It is evident that both antigen-specific IgE-mediated reactions and cell-mediated reactions are involved in the pathogenesis of food allergy. IgE-mediated reactions are involved in the early phase of the symptoms, and intestinal biopsy specimens show mucosal edema and mast cells degranulation (1–4). On the other hand, cell-mediated reactions are involved in the late phase of the symptoms and often show prolonged symptoms, such as persistent diarrhea, dehydration, and failure to thrive, and cause mucosal damage, evident as villous atrophy and crypt hyperplasia, and lymphocyte migration (3–8). However, IgE-mediated reactions could also be involved in prolonged symptoms by chronic antigen exposure, because allergic patients often suffer from frequent and prolonged allergic responses as a result of repeated antigen exposure. There is relatively little information available about the effects of chronic antigen exposure in relation to IgE-mediated reactions, even though this may be highly relevant to the clinical situation.
Several animal models of immediate-type allergy have been established to investigate allergic responses (9–11). Most of these models were established by active immunization of mice with certain antigen-adjuvant complexes, and as a result, there is a limitation of IgE production. These limited IgE could be trapped by mast cells and exhausted by chronic antigen exposure (12). We also have to be aware that the active immunization could also produce substantial amounts of IgA and IgG in these mice (11). These Igs could interfere with genuine IgE-mediated reactions, because IgA could protect further antigen invasion into mucosa and IgG could directly react with lymphocytes. Therefore, these models are considered to be not appropriate for the analysis of the chronic phase of genuine IgE-dominant anaphylactic reactions, especially when concerned with lymphocyte involvement.
In an effort to clarify the mechanisms of the chronic intestinal changes induced by genuine IgE-mediated reactions, a mouse model was established by s.c. implantation of a murine hybridoma capable of producing monoclonal anti-TNP IgE antibody, which maintains high levels of expression of antigen-specific IgE (13). Using this model of IgE-mediated allergic responses, we investigated the morphologic and immunologic changes that occur in the intestinal mucosa upon chronic oral antigen exposure, and found that continuous antigen challenge actually elicits lymphocyte migration, and possibly cell-mediated immunologic reactions, in the intestine.
METHODS
Mice. Female BALB/c mice aged 8-10 wk were purchased from Clea Japan, Inc. (Tokyo). Three sets of two groups, consisting of 10 mice each, of hybridoma-nonbearing control mice and hybridoma-bearing mice were prepared. The first set was prepared to examine the changes at 1 h after antigen challenge, the second set was prepared to examine the changes at 9 h after antigen challenge, and the third set was prepared to examine the changes upon antigen challenge continuously for 10 d, to see the early phase, late phase, and chronic phase IgE-mediated reactions. In the case of the first two sets, 50 µg of TNPO37-HSA dissolved in 1 mL of PBS (the volume required to fill the stomach) was administered into the stomach of each mouse by means of a feeding tube, and in the case of the last set, TNP37-HSA was administered as a constituent of the drinking water, in which the antigen was dissolved (10 µg/mL), and the morphologic and immunologic changes in the intestine were examined in each group.
Establishment of the mouse model. Murine hybridoma, IGEL a2 cells (ATCC, TIB 142) secreting anti-TNP IgE (14) were maintained in Dulbecco's minimum essential medium (Nissui Seiyaku Co. Ltd., Tokyo) supplemented with 10% fetal bovine serum, 10 mM HEPES, 2 mM glutamine, 50 U/mL penicillin, and 50 µg/mL streptomycin. After washing with Hank's solution (Nissui Seiyaku Co. Ltd., Tokyo), IGEL a2 cells at a dose of 1 × 107 cells/mouse were s.c. injected at a site on the back of the syngenic BALB/c mice. Blood samples were obtained before and after antigen challenge, and the concentration of serum anti-TNP IgE was quantitatively determined by ELISA as described previously (13). Serum anti-TNP IgE increased to a level higher than 600 ng/mL around 10 d after inoculation of the mice with these cells, and the anti-TNP IgE level stayed above 600 ng/mL after chronic antigen exposure for 10 d, whereas anti-TNP IgG and IgA were not detectable during this period.
Histologic evaluation of the intestinal mucosa. More than five jejunal samples (each about 1 cm long), taken from a location 10 cm toward the anal side from the pylorus, were obtained from each mouse and washed gently with PBS. For evaluation of morphologic changes and the migration of IEL, each jejunal sample was fixed with 10% formalin, and stained with a hematoxylin and eosin solution. To confirm mast cell infiltration, other jejunal samples were fixed with Carnoy's solution and stained with Alcian blue and safranin dye (15). Modified Hansel's staining was also performed to determine eosinophil infiltration (16). More than 10 villi were examined in each section, and the numbers of mast cells and eosinophils per 1 mm2 were determined. The number of IEL per 100 epithelial cells was also counted for each specimen, and the average number of IEL per 100 epithelial cells was determined as previously described (17).
Determination of the plasma histamine level. Blood samples were collected in plastic tubes containing EDTA and immediately placed on ice. Then, the samples were centrifuged at 4°C for 10 min at 2500 × g, and the plasma was carefully pipetted into polypropylene tubes. Plasma histamine concentration was measured by a radioenzymatic assay following the method of Verburg et al. (18) with the kit supplied by Du Pont de Nemours & Co. (NEN Products, Boston, MA). All samples were assayed in duplicate.
LTB4 and LTC4 production in A23187 stimulated intestinal mucosa. The production of LTB4 and LTC4 in A23187-stimulated intestinal mucosa was measured as described previously (19). Jejunal mucosae were gently washed twice in cold Ca2+/Mg2+-free PBS, and the wet weight was determined. The specimen was then incubated with 10 mM calcium ionophore A23187 (Calbiochem-Behring, La Jolla, CA) for 15 min at 37°C. After centrifugation at 4°C, the supernatant was removed and stored at -80°C until the assay was performed. LTB4 and LTC4 were purified by HPLC following the method of Odlander et al. (20). The elute was evaporated to dryness and resuspended in the RIA buffer. Finally LTB4 and LTC4 immunoreactivities were evaluated in duplicate, using LTB4 and LTC4 3H assay kits (Amersham International, Buckinghamshire, UK) according to the manufacturer's instructions. Production of LTB4 and LTC4 was expressed as micrograms/g of wet sample.
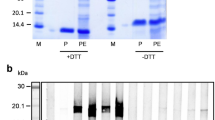
Immunohistochemistry of the intestinal mucosa. The freshly obtained jejunal mucosae were rapidly frozen in OCT embedding medium using liquid nitrogen-cooled isopentane and stored at -80°C until processing. Frozen sections 4 µm thick were cut and air-dried before further processing. To examine the expression of ICAM-1 in the intestinal mucosa, samples were fixed in 4% paraformaldehyde for 10 min and then dipped in 0.3% H2O2 containing methanol for 20 min to inactivate endogenous peroxidase. After blocking with 5% normal goat serum, the sections were stained with rat anti-mouse ICAM-1 MAb (PharMingen, San Diego, CA) using the indirect immunoperoxidase technique. To examine the expression of IAd and the infiltration of CD8+ cells, sections were fixed with cold acetone for 10 min and incubated with rat anti-mouse IAd MAb (PharMingen) after blocking with normal goat serum. After washing, the sections were incubated with Cy3-conjugated goat anti-rat IgG antibody (Amersham Life Sciences, Inc., Arlington Heights, IL). The sections were then incubated with FITC-conjugated rat anti-mouse CD8 MAb (PharMingen) and examined by fluorescence microscopy. Nonspecific staining was evaluated by means of sections stained with control IgG (PharMingen).
Results are expressed as mean ± SD. Statistical significance was evaluated by the Mann-Whitney U test.
RESULTS
TNP37-HSA was orally administered to evaluate the symptoms of anaphylactic reactions in hybridoma-bearing mice displaying serum anti-TNP IgE levels of more than 600 ng/mL. Diarrhea, and mucosal edema, and hyperemia were observed 30 min to 1 h after antigen challenge in the hybridoma-bearing mice. These responses decayed within 2 h. Prolonged diarrhea was observed in hybridoma-bearing mice upon chronic antigen exposure, in animals antigen challenged continuously for 10 d. No remarkable changes were observed in the hybridoma-nonbearing control mice during the study period.
Alcian blue and safranin staining was carried out to examine the infiltration of mast cells into the intestinal mucosa. Mucosal-type mast cells, containing three to six granules stained with Alcian blue dye but not with safranin dye, were found to have infiltrated into the lamina propria of the hybridoma-bearing mice after antigen challenge. As shown in Figure 1, the number of infiltrating mast cells was significantly greater in the hybridoma-bearing mice than in either hybridoma-nonbearing control mice during the same period or hybridoma-bearing mice before antigen challenge (p < 0.01 in both). The number of mast cells in hybridoma-bearing mice upon chronic antigen exposure was significantly elevated compared with that in hybridoma-nonbearing control mice (p < 0.01), but was not significantly greater than the number evident in the hybridoma-bearing mice at either 1 h or 9 h post challenge.
The number of mast cells per mm2 in jejunal mucosa of hybridoma-bearing mouse models at 1 and 9 h after oral antigen challenge, and upon chronic antigen exposure for 10 d is shown (closed columns). Open columns show that of hybridoma-nonbearing mouse controls. Data are presented as the mean ± SD of 10 animals for each group (*p < 0.01). Similar results were obtained in three independent experiments.
Hansel's staining was performed to examine eosinophil infiltration (Fig. 2). The number of eosinophils, which contain pinkish granules, was determined, and noticeable eosinophil infiltration was confirmed 1 h after antigen challenge (p < 0.01). However, unlike the case of mast cells, the number of eosinophils continued to increase in the intestine of the hybridoma-bearing mice after antigen challenge. Upon chronic antigen exposure, the number of eosinophils in the intestine of these mice was greater than that observed either 1 or 9 h postchallenge, and greater than that in time-matched hybridoma-nonbearing controls (p < 0.01).
The number of eosinophils per mm2 in jejunal mucosa of hybridoma-bearing mouse models at 1 and 9 h after oral antigen challenge, and upon chronic antigen exposure for 10 d is shown (closed columns). Open columns show that of hybridoma-nonbearing mouse controls. Data are presented as the mean ± SD of 10 animals for each group (*p < 0.01). Similar results were obtained in three independent experiments.
To evaluate the production of chemical mediators during the anaphylactic reaction, serum histamine levels after antigen challenge and the levels of synthesis of LTB4 and LTC4 in the jejunal mucosa after stimulation with the calcium ionophore A23187 were determined as shown in Figure 3. A substantial increase in serum histamine levels was observed 1 h after antigen challenge in the hybridoma-bearing mice as evident by comparison with the level before challenge (p < 0.01). Serum histamine levels declined to the prechallenged level 9 h after antigen challenge. The level of mucosal LTC4 synthesis was significantly elevated 1 h after antigen challenge, and remained high for 9 h, in the hybridoma-bearing mice compared with the level before challenge (p < 0.01 for both). LTB4 synthesis, however, continued to increase gradually after antigen challenge, and the increase in LTB4 synthesis was significant at 9 h postchallenge (p < 0.01). No increase in serum histamine levels or the levels of LTB4 or LTC4 was observed in the hybridoma-nonbearing control mice after antigen challenge.
Serum histamine levels (left), and levels of LTB4 (middle), and LTC4 (right) produced in jejunal mucosa stimulated with calcium ionophore A23187 were measured before, and at 1 and 9 h after antigen challenge in hybridoma-bearing mouse models (closed columns). Open columns show that of hybridoma-nonbearing mouse controls. Data are presented as the mean ± SD of 10 animals for each group (*p < 0.05, **p < 0.01). Similar results were obtained in three independent experiments.
It is well known that the expression of adhesion molecules is enhanced in inflammatory mucosa, resulting in the migration of inflammatory cells to this lesion (21). To confirm the expression of adhesion molecules, jejunal mucosa was stained with anti-ICAM-1 MAb by an immunohistochemical technique. The expression of ICAM-1 by vascular endothelial cells was confirmed in the hybridoma-nonbearing control mice and hybridoma-bearing mice before antigen challenge (Fig. 4, A-D). The intensity of staining gradually increased in the hybridoma-bearing mouse 9 h after single antigen challenge (Fig. 4E). The expression of ICAM-1 by these cells was remarkably enhanced in the intestine of the hybridoma-bearing mice upon chronic antigen exposure, as shown in Figure 4F.
Expression of ICAM-1 was examined in the jejunal mucosa by immunohistochemical staining. (A) The jejunal mucosa from the hybridoma-nonbearing mouse control before antigen challenge, (B) that of 9 h after antigen challenge, (C) that of after chronic antigen exposure, (D) the jejunal mucosa from the hybridoma-bearing mouse model before antigen challenge, (E) that of 9 h after antigen challenge, and (F) that of after chronic antigen exposure for 10 d. Representative samples from 10 mice each are presented.
In an effort to confirm the activation of epithelial cells, the major histocompatibility complex class II molecule IAd, expressed by these cells, was stained. Epithelial cells were stained with anti-IAd MAb (red) in the hybridoma-bearing mice before antigen challenge (Fig. 5A). The intensity of IAd was not changed significantly 9 h after antigen challenge (Fig. 5B); however, it was strongly enhanced upon chronic antigen exposure (Fig. 5C). Interestingly, marked infiltration of CD8+ cells, stained with FITC (green), was also confirmed both in the epithelial layer and in the lamina propria upon chronic antigen exposure in hybridoma-bearing mice (Fig. 5C). The intensity of IAd and the number of IEL remain constant before and after single antigen challenge as well as chronic antigen challenge in hybridoma-nonbearing mice. The number of IELs, which were mostly CD8+ cells, was significantly increased in hybridoma-bearing mice upon chronic antigen exposure compared with the number observed 9 h postchallenge, as shown in Figure 6 (p < 0.01). The number of IELs did not change with time in the hybridoma-nonbearing controls after antigen challenge.
Expression of IAd (Cy-3) and CD8+ cells (FITC) in the jejunal mucosa was examined by immunohistochemical staining. (A) The jejunal mucosa from the hybridoma-bearing mouse model before antigen challenge, (B) that of 9 h after antigen challenge, and (C) that of after chronic antigen exposure for 10 d. Representative samples from 10 mice each are presented.
The number of IELs per 100 epithelial cells in jejunal mucosa of hybridoma-bearing mouse models 9 h after single oral antigen challenge, and after chronic antigen exposure for 10 d are shown (closed columns). Open columns show that of hybridoma-nonbearing mouse controls. Data are presented as the mean ± SD of 10 animals for each group (*p < 0.01). Similar results were obtained in three independent experiments.
DISCUSSION
Curtis et al. (12) reported a study of chronic antigen exposure in actively immunized rats. In their study, it was suggested that mucosal mast cells were involved in chronic allergic reactions, as suggested by findings of an increased number of mast cells, together with evidence of mast cell degranulation, and increased levels of serum RMCP II. We confirmed that not only mast cells but also eosinophils and IELs infiltrated into the intestinal mucosa upon chronic antigen exposure in our mouse model. A decrease in serum levels of anti-egg albumin IgE, from > 1/64 to O-, was observed in their study, and it was suggested that these IgE had become bound to mast cells. There is a possibility that the IgE levels were not high enough to induce infiltration of eosinophils and IELs upon chronic antigen exposure in their model. Such a decrease in IgE levels is rarely observed during the period of antigen exposure in patients suffering from food allergy. In an effort to confirm this hypothesis, an antigen-specific IgE-producing hybridoma was implanted into mice, and in this manner an animal model displaying high serum IgE levels for a prolonged period was established. These mice showed IgE levels higher than 600 ng/mL, and these high IgE levels were sustained upon chronic antigen exposure (13). This observation suggested that IgE-mediated reactions occur continuously during the period of antigen exposure in our model, which may be more relevant to the clinical situation, particularly in the case of food allergy, as the antigens are encountered on a regular basis.
The specific IgE bound to high affinity IgE receptors on the surface of mast cells becomes cross-linked upon exposure to allergens, and intracellular signals are transduced to activate the mast cells to release chemical mediators such as histamine, LTB4, LTC4, tumor necrosis factor-α, IL-4, and other cytokines (22). The findings of infiltration of mast cells in the intestine, elevation of serum histamine levels, and mucosal production of both LTB4 and LTC4 in the early phase after antigen challenge, suggest that mast cell degranulation and activation occurred in the intestinal mucosa upon antigen challenge. It is very likely that these mediators induce a local increase in vascular permeability, lymph duct dilatation, and mucus production, and elicit watery diarrhea, resulting in blood hypocirculation in these mice. Taken together, these histologic and immunologic changes suggest that the mast cells that have infiltrated the intestinal mucosa are deeply involved in the early phase of anaphylactic reactions induced by oral antigen challenge. The level of synthesis of LTB4 in the mucosa was elevated until 9 h after antigen challenge, although the increase in number of mast cells occurred not later than 1 h after antigen challenge. Tumor necrosis factor-α produced from mast cells may stimulate infiltration of neutrophils, and these neutrophils are considered to contribute to this further elevation of LTB4 synthesis (23,24).
A previous study suggested that no infiltration of eosinophils occurs (12). However, in our hybridoma-bearing mouse model, the number of eosinophils gradually increased, and the infiltration of eosinophils was significant upon chronic antigen exposure. We consider that this discrepancy in findings is attributable to the high serum IgE levels expressed in these mice, which display more severe symptoms of IgE-mediated inflammation in the intestine than is observed in actively immunized models. The eosinophils are considered to participate in IgE-mediated inflammation directly by responding to food antigens, as these cells have low affinity receptors for IgE (25), and also indirectly by responding to eosinophil chemotactic factors, such as platelet-activating factor (26), histamine, and LTB4 derived from mast cells and basophils, and by responding to the stimulus of IgE-antigen complexes bound to the high affinity receptor for IgE. The finding that infiltration of eosinophils occurs suggests that these cells are essential for the late phase and chronic phase symptoms, because eosinophils liberate an abundance of highly cytotoxic and proinflammatory mediators, such as major basic protein, eosinophil cationic protein, and eosinophil peroxidase (27), and these mediators may contribute to the symptoms of the late phase and the chronic phase of the IgE-mediated allergic response.
In the intestinal mucosa of the hybridoma-bearing mice upon chronic antigen exposure, we observed a marked enhancement of expression of ICAM-1 on endothelial cells, and IAd on epithelial cells, and a noticeable infiltration of lymphocytes. The expression of ICAM-1 is considered to be up-regulated as a result of continuous stimulation with cytokines, especially tumor necrosis factor-α, and other chemical mediators derived from mast cells in response to chronic antigen exposure (23,24,28). The enhancement of ICAM-1 expression leads to infiltration of lymphocytes into the mucosa. These lymphocytes that have migrated, especially CD8+ cells, produce interferon-γ, which would up-regulate antigen presentation by promoting IAd expression on the epithelial cells (29), and this would promote further reactions against food antigen in the intestine.
Patients who suffered from cell-mediated reactions show persistent diarrhea with dehydration, malnutrition, and failure to thrive. Mucosal damages, such as villous atrophy and crypt hyperplasia, are observed in biopsy specimens taken from these patients (5–7). However, these mucosal damages, except some infiltration of mast cells and edema, could not been seen in IgE-mediated allergic models (3,4). Because infiltration of intraepithelial and lamina propria lymphocytes, but not with mast cells and eosinophils, are confirmed in a prolonged phase of biopsy specimens, these infiltrated lymphocytes are considered to be one of the pathogenic causes of mucosal damage (5–7). Cell-mediated reactions and their effects on intestinal morphology have been investigated in detail during graft versus host reactions (30,31), because there is a striking morphologic similarity between the mucosal damage seen in food-sensitive enteropathy. Further evidence for an important T cell-mediated process in the pathogenesis of a mucosal lesion has been presented in tissue culture experiments of human fetal gut explants, in which only explants with activated lymphocytes present responded to mitogen stimulation with mucosal atrophy (32). This hypothesis is further supported by the finding in animal models of food-sensitive enteropathy in which migrated lymphocytes in the intestinal mucosa are capable of proliferation in response to stimulation with specific antigen (17). Therefore, the findings of migrated lymphocytes in the intestinal mucosa suggest that the cell-mediated reactions are introduced in the IgE-mediated mouse models after chronic antigen exposure.
These findings suggest that oral antigen exposure actually induces anaphylactic reactions in the intestine mediated by mast cells and eosinophils in response to the IgE-antigen complex in the early phase. They also induce lymphocyte migration after chronic antigen exposure, which may cause cell-mediated reactions in the intestinal mucosa in the chronic phase.
Abbreviations
- HSA:
-
human serum albumin
- IEL:
-
intraepithelial lymphocyte
- LT:
-
leukotriene
- TNP:
-
trinitrophenyl
- ICAM-1:
-
intercellular adhesion molecule-1
References
Kosnai I, Kuitunen P, Savilahti E, Sipponen P 1984 Mast cells and eosinophils in the jejunal mucosa of patients with intestinal cow's milk allergy and celiac disease of childhood. J Pediatr Gastroenterol Nutr 3: 368–372.
Selbekk BH 1985 A comparison between in vitro jejunal mast cell degranulation and intragastric challenge in patients with suspected food intolerance. Scand J Gastroenterol 22: 299–303
Sampson HA 1997 Food allergy. JAMA 278: 1888–1894
Walker-Smith JA, Ford RPK, Phillips AD 1984 The spectrum of gastrointestinal allergies to food. Ann Allergy 53: 629–636
Phillips AD, Rice SJ, France NE, Walker-Smith JA 1979 Small intestinal intraepithelial lymphocyte levels in cow's milk protein intolerance. Gut 20: 509–512
Manluenda C, Phillips AD, Briddon A, Walker-Smith JA 1984 Quantitative analysis of small intestinal mucosa in cow's milk-sensitive enteropathy. J Pediatr Gastroenterol Nutr 3: 349–356
Nagata S, Yamashiro Y, Ohtsuka Y, Shioya T, Oguchi S, Shimizu T, Maeda M 1995 Quantitative analysis and immunohistochemical studies on small intestinal mucosa of food-sensitive enteropathy. J Pediatr Gastroenterol Nutr 20: 44–48
Ferguson A 1992 Definitions and diagnosis of food intolerance and food allergy: consensus and controversy. J Pediatr 121: S7–S11
Perdue MH, Chung M, Gall DG 1984 Effect of intestinal anaphylaxis on gut function in the rat. Gastroenterology 86: 391–397
Gall DG, Perdue MH 1986 Experimental models of intestinal allergy. Front Gastrointest Res 13: 45–54
Snider DP, Marshall JS, Perdue MH, Liang H 1994 Production of IgE antibody and allergic sensitization of intestinal and peripheral tissues after oral immunization with protein Ag and cholera toxin. J Immunol 153: 647–657
Curtis GH, Patrick MK, Gatto-Smith AG, Gall DG 1990 Intestinal anaphylaxis in the rat: effect of chronic antigen exposure. Gastroenterology 98: 1558–1566
Naito K, Hirama M, Okumura K, Ra C 1995 Soluble form of the human high affinity receptor for IgE inhibits recurrent allergic reaction in a novel mouse model of type I allergy. Eur J Immunol 25: 1631–1637
Rudolph AK, Burrows D, Wabl MR 1981 Thirteen hybridomas secreting hapten-specific immunoglobulin E from mice with Iga or Igb heavy chain haplotype. Eur J Immunol 11: 527–529
Strobel S, Ferguson A 1981 Human intestinal mucosal mast cells: evaluation of fixation and staining techniques. J Clin Pathol 34: 851–858
Sasaki Y, Araki A, Koga K 1977 The mast cell and eosinophil in nasal secretion. Ann Allergy 39: 106–109
Ohtsuka Y, Yamashiro Y, Maeda M, Oguchi S, Shimizu T, Nagata S, Yagita H, Yabuta K, Okumura K 1996 Food antigen activates intraepithelial and lamina propria lymphocytes in food-sensitive enteropathy in mice. Pediatr Res 39: 862–866
Verburg KM, Bowsher RR, Henry DP 1988 Quantification of urinary histamine by a new radioenzymatic assay: documentation of assay specificity and establishment of normal excretion rates. J Allergy Clin Immunol 82: 339–347
Ohtsuka Y, Yamashiro Y, Shimizu T, Nagata S, Oguchi S, Yabuta K 1997 Reducing cell membrane n-6 fatty acid attenuates intestinal damage in food sensitive enteropathy in mice. Pediatr Res 42: 835–839
Odlander B, Claesson HE 1987 A rapid and sensitive method for measurement of leukotrienes based on HPLC. Biomed Chromatogr 2: 145–147
Nakamura S, Ohtani H, Watanabe Y, Fukushima K, Matsumoto T, Kitano A, Kobayashi K, Nagura H 1993 In situ expression of the cell adhesion molecules in inflammatory bowel disease: evidence of immunologic activation of vascular endothelial cells. Lab Invest 69: 77–85
Gordon JR, Burd PR, Galli SJ 1990 Mast cells as a source of multifunctional cytokines. Immunol Today 11: 458–464
Wershil BK, Furuta GT, Wang Z-S, Galli SJ 1996 Mast cell-dependent neutrophil and mononuclear cell recruitment in immunoglobulin E-induced gastric reactions in mice. Gastroenterology 110: 1482–1490
Furuta GT, Schimidt-Choudhury A, Wang MY, Wang ZS, Lu L, Furlano RI, Wershil BK 1997 Mast cell-dependent tumor necrosis factor a production participates in allergic gastric inflammation in mice. Gastroenterology 113: 1560–1569
Capron M, Capron A, Dessaini J, Torpier G, Gunnar S, Johannson O, Prin L 1981 Fc receptors for IgE on human and rat eosinophils. J Immunol 126: 2087–2092
Wardlaw AJ, Moqbel R, Cromwell O, Kay AB 1986 Platelet-activating factor. A potent chemotactic and chemokinetic factor for human eosinophils. J Clin Invest 78: 1701–1706
Venge P, Hakansson L, Peterson CGB 1987 Eosinophil activation in allergic disease. Int Arch Allergy Appl Immunol 82: 333–337
Dustin ML, Springer TA 1988 Lymphocyte function-associated antigen-1 (LFA-1) interaction with intercellular adhesion molecule-1 (ICAM-1) is one of at least three mechanisms for lymphocyte adhesion to cultured endothelial cells. J Cell Biol 107– 321–331
Steinger B, Falk P, Lohmuller M, Van Der Meide PH 1989 Class II MHC antigens in the rate digestive system. Normal distribution and induced expression after interferon-γ treatment in vivo. Immunology 68: 507–513
MacDonald TT, Ferguson A 1976 Hypersensitivity reactions in the small intestine. 2. Effects of allograft rejection on mucosal architecture and lymphoid cell infiltrate. Gut 17: 81–91
MacDonald TT, Ferguson A 1977 Hypersensitivity reactions in the small intestine. 3. The effects of allograft rejection and graft-versus-host disease on epithelial cell kinetics. Cell Tissue Kinet 10: 301–312
MacDonald TT, Spencer J 1988 Evidence that activated mucosal T cells play a role in the pathogenesis of enteropathy in human small intestine. J Exp Med 167: 1341–1349
Author information
Authors and Affiliations
Additional information
Supported by grants from Morinaga Milk Industry Co., Ltd., Kanagawa, Japan, and also by a Grant-in-Aid for Scientific Research, The Ministry of Education, Science, Sports and Culture, Japan.
Rights and permissions
About this article
Cite this article
Ohtsuka, Y., Suzuki, R., Nagata, S. et al. Chronic Oral Antigen Exposure Induces Lymphocyte Migration in Anaphylactic Mouse Intestine. Pediatr Res 44, 791–797 (1998). https://doi.org/10.1203/00006450-199811000-00025
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199811000-00025
This article is cited by
-
Eosinophilic gastroenteritis: A problem of the mucosal immune system?
Current Allergy and Asthma Reports (2003)
-
The mechanism for the contraction induced by leukotriene C4 in guinea‐pig taenia coli
British Journal of Pharmacology (2001)