Abstract
Disturbed sleep regulation is often observed in neonates of women who drank heavily during pregnancy. It is unknown if (and how) an occasional drink affects fetal sleeping behavior. In 28 near-term pregnant women we examined the effects on fetal behavioral state organization of two glasses of wine (0.25 g of ethanol/kg of maternal body weight). Simultaneous 2-h recordings of fetal heart rate and body, eye, and breathing movements were made on two successive days, once without alcohol exposure and once during maternal alcohol consumption. The study was standardized for time of day and fetal sleep state, i.e. the start of recording was either during quiet sleep (n = 16) or during active sleep (n = 12). Alcohol intake reduced fetal eye movements, disorganized behavioral state organization (rapid eye movement sleep was affected in particular), and suppressed fetal breathing activity almost completely. Modest maternal alcohol intake affects fetal behavioral state organization, which reflects an immediate effect on fetal brain function.
Similar content being viewed by others
Main
Maternal alcohol abuse during pregnancy may adversely affect the developing fetus, both structurally and functionally, resulting in lifetime handicaps (1–3). Newborn infants prenatally exposed to excessive amounts of alcohol have been reported to exhibit disturbances in behavior, neurologic status, EEG power spectra, and the organization of sleep states (1,4–7). Affected sleep organization is also demonstrable in neonates prenatally exposed to low to moderate alcohol levels (7). The underlying mechanism is completely unknown.
To date, a safe level of maternal alcohol intake in pregnancy (if any) has not been established conclusively (1). This uncertainty poses considerable difficulty to patient counseling and public education, and is reflected by absence of guidelines for sensible drinking in most countries. In some countries, women are recommended to refrain from alcohol when pregnant, whereas pregnant women in Britain are advised that drinking one or two drinks once or twice a week is unlikely to affect fetal development (8).
Knowledge of the acute effects of an occasional alcoholic drink on fetal sleeping behavior is nonexistent. We studied the immediate effects of maternal alcohol intake (two glasses of wine) on the organization of fetal behavioral states ("sleep-wake cycles") in 28 women who had either abstained from alcohol during pregnancy or were social drinkers.
METHODS
Subjects. Twenty-eight healthy volunteers participated in this study, which consisted of two subsets, series A (n = 16) and series B (n = 12). Local ethical committee approval was obtained. All women (19 nulliparous and 9 multiparous) were outpatients with normal singleton pregnancies between 37 and 40 wk of gestation; the median test gestational age was 38 2/7 wk. They had abstained from alcohol during pregnancy (n = 15) or were social-drinking (n = 12; <4 drinks/wk); only one woman used one drink daily.
Delivery at 40 5/7 wk (median) was uneventful, and all infants (16 female, 12 male) were appropriate-for-dates (median birth weight 3570 g; range 2850-5440 g), showed no anomalies, and did well after birth.
Recording procedures. Simultaneous, continuous on-line recording sessions lasting 2 h were carried out between 1800 and 2200 h, starting about 1 h after the evening meal. Recorded were FHR and fetal body and EMs (the three state variables), and FEBMs (9,10).
FHR was monitored with a cardiotocograph by means of Doppler ultrasound (Hewlett Packard 8040A). The signal was fed into a computer running the System 8000 FHR analysis program (Oxford Sonicaid Ltd., Chichester, UK). This program yields information on basal FHR (beats/min) and its variation (mean minute range, in milliseconds) (11). The FHR tracings were also visually judged and divided into episodes of fetal HRPs A-D (9,12).
Fetal body, eye, and breathing movements were identified using two linear-array real-time ultrasound scanners (10,13). These movements were recorded on an event recorder (paper speed 1 mm/s) together with the FHR signal and also stored in a personal computer for off-line analysis.
Each fetus acting as his/her own control was studied on two successive days, once after maternal alcohol intake (experimental day) and once without alcohol exposure (control day) in a randomized counterbalanced fashion. As soon as the women lay comfortably on the bed, FHR monitoring and time-lapse viewing of the fetal eyeball were started to assess the fetal state. The start of both the experimental and control recordings was at 10 min after a transition had occurred from fetal active into quiet sleep (series A) or from fetal quiet into active sleep (series B). At that time (t = 0 min), the women also started to drink on the experimental days. They ingested two glasses of white wine (11% vol/vol); the volume per woman corresponded with 0.25 g of pure ethanol/kg of maternal body weight. The median volume ingested was 245 mL (range, 160-300 mL), which they consumed within 30 min of recording (median, range 10-67 min).
The maternal blood glucose level was determined at the start of each recording session and subsequently at 30-min intervals (five determinations per recording) by using a device for blood glucose self-monitoring (Haemo-Glukotest 1-44R).
Analysis of fetal behavior. Tonic movements of the trunk occurring within 1 s of each other were regarded to be one single burst of body movement; only bursts lasting ≥2 s were considered. A bout of continuous breathing was considered when the intervals between successive breaths were <6 s; for fetal EMs, an interval of 10 s represented a pause between two consecutive bouts (10). The incidences were expressed as a percentage of observation time and as the number of movements per hour.
The presence of behavioral states (or coincidence) 1F-4F was identified according to predefined criteria (9,12). Episodes of 1F ("quiet sleep") are defined by a stable heart rate with a small oscillation bandwidth (HRP A) and absence of body and EMs. In 2F episodes ("active sleep"), body and EMs are present and FHR has a wide oscillation bandwidth between the frequent accelerations (HRP B). During 3F, body movements are absent and EMs present; there is a stable FHR pattern (HRP C) without accelerations ("quiet awake"). Characteristic for 4F episodes ("active awake") are frequent vigorous body movements in the presence of EMs, and an unstable HRP with large and prolonged accelerations (HRP D). Episodes to which none of the four specified combinations could be applied were called episodes of NoC. The incidences of HRPs A-D and coincidence 1F-4F were expressed as a percentage of observation time.
Statistics. Data will be presented as medians and interquartile ranges. Statistical analyses were carried out using the Wilcoxon signed rank test, the Mann-Whitney U test, or the Spearman rank correlation test. With all tests, significance was considered at the level of p < 0.05 (two-tailed).
RESULTS
During both the control and experimental sessions, the fetuses alternated predominantly between quiet sleep (C1F) and active sleep (C2F), with only brief occasional episodes of "wakefulness" (C3F and C4F). The sequence of the control and experimental sessions, i.e. the control session carried out on either d 1 or 2, had no significant effect on the occurrence of any of the parameters listed in Table 1 (Mann-Whitney U test). Also, there were no statistically significant differences in the studied parameters between the abstainers and social drinkers (Mann-Whitney U test). In either series, therefore, the data of the control days were pooled for further analysis and so were the data obtained on the experimental days.
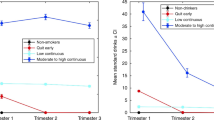
In series A (start of recording during fetal quiet sleep), maternal alcohol intake had no effect on fetal body movements (Table 1), the distribution of the fetal HRPs (Table 1), the duration of the HRP A episode during which recording started (Table 2), and the time between alcohol administration and the onset of the next successive episode of HRP A ("latency"; Table 2). However, alcohol intake altered the normal cyclic pattern of fetal EMs as observed during the control sessions (Fig. 1A). The number of EMs decreased between 45 and 60 min of recording (about 15 min earlier than on the control days) and remained lower than control values during the second hour of observation (p < 0.05, Table 1). The effect on EMs was directly associated with a steady increase in the %NoC in the course of the experimental sessions. (Fig. 1B). During the second hour of observation, the %NoC was higher on the experimental days than on the control days (p < 0.01), at the expense of the incidence of active sleep (C2F), whereas quiet sleep (C1F) remained unaffected (Table 1). The overall results of series A are presented schematically in Fig. 2.
Schematic presentation of the results obtained on the control and experimental (alcohol) days in series A (start of recording during fetal quiet sleep). The drawn profiles indicate the presence of fetal HRP A or B, and the presence (+) or absence (-) of fetal body (GM) and EMs. The start of the recording is indicated by the arrows (t = 0 min); the horizontal bar represents the median time the women needed to ingest the amount of wine.
In series B (start of recording during fetal active sleep), alcohol influenced the occurrence of HRPs B-D during the first (but not the second) hour of recording and a commensurate increase was seen in the incidence of HRP A (both p < 0.05, Table 3). After the onset of maternal drinking, transitions from HRPs B-D into an A pattern occurred sooner than on the control days (p < 0.05; Table 2). The duration of these HRP A episodes was unaltered (the median values were 23 and 27 min on the control and experimental days, respectively, NS), and the time between alcohol administration and the onset of the next episode of HRP B was shorter (p < 0.05; Table 2). The degree of HRP B suppression was not significantly related to the time the women needed to complete the first drink (range 6-18 min, r(S) = 0.27) or both drinks (range 10-67 min, r(S) = 0.21). The early transitions into HRP A during the first hour of the experimental days were accompanied by a reduced number of fetal EMs between 30 and 60 min of recording (p < 0.05, Table 3; Fig. 3A), but body movements, in general, did not decrease simultaneously, as shown by the unchanged incidence parameters (Table 3). The incidence of HRP A and C1F did therefore not correspond well (median values 38.0% and 17.5%, respectively), resulting in increased %NoC during the first hour (p < 0.05, Table 3; Fig. 3A). During the second hour of the experimental sessions, the %NoC was still increased compared with the control sessions (p < 0.01, Table 3) and resulted from a decrease in %C2F-4F. Fetal EMs were reduced during the second hour of recording (lower medians between 75 and 105 min; Fig. 3B), but their incidence was not significantly different from that on the control days (Table 3). The overall results of series B are presented schematically in Fig. 4.
Schematic presentation of the results obtained on the control and experimental (alcohol) days in series B (start of recording during fetal active sleep). The drawn profiles indicate the presence of fetal HRP A or B, and the presence (+) or absence (-) of fetal body (GM) and EMs. Start of recording is indicated by the arrows (t = 0 min); the horizontal bar represents the median time the women needed to ingest the amount of wine.
FBM were dramatically reduced after maternal alcohol intake in both series A and series B (Fig. 5). The reduction in FBM was apparent from about 30 min after the onset of drinking; during the second hours of observation breathing activity had ceased almost completely (Tables 1 and 3; Fig. 5). The effect of alcohol on FBM was much more pronounced in series A (start of maternal drinking during fetal quiet sleep) than in series B, as the incidence of FBM was already significantly reduced (p < 0.01; Mann-Whitney U test) during the first 15 min of recording in series A (Fig. 5). In either series, the extinction of FBM was not significantly related to the time the women needed to ingest 25, 50, 75, or 100% of the total amount of wine.
Maternal alcohol intake had no effect on FHR and its variation in either series (data not shown). The maternal blood glucose levels gradually declined during the 2 h of recording and the trends did not significantly differ between the control and experimental days in either series. At the end of recording, the values were 5-10% lower as compared with the initial glucose levels (range, 3.7-5.6 mmol/L).
DISCUSSION
Acute low dose intake of alcohol (0.25 g/kg of maternal body weight) by social or nondrinking near-term pregnant women transiently suppressed fetal EMs and breathing activity and disturbed behavioral state organization, without affecting fetal body movements. FHR, or FHR variation. This study corroborates previous observations in social-drinking pregnant women (<4 drinks/wk) by McLeod et al. (14), who found unaltered fetal body movements and FHR and a considerable reduction in breathing movements after consumption of alcohol in the same dose we used. However, the effects of alcohol on fetal behavioral state organization, i.e. on the concordant association between three state variables, had never before been the subject of investigation.
The healthy near-term human fetus exhibits four behavioral states (1F-4F), which recur repeatedly in a nonrandom manner (9,12). Each state is defined by a specific combination of the parameters of three selected variables: FHR pattern, body movements, and EMs. Such a combination is relatively stable, i.e. is maintained uninterruptedly over long periods, and at transitions from one state into another the variables change almost simultaneously. Both the building up and the maintenance of a particular state require normal undisturbed brain function. The organization of behavioral states is therefore considered a measure of neurophysiologic development, integrity, and maturity (15,16). Assessment of behavioral state regulation has proven to be useful in fetal and neonatal studies concerning the effects of maternal and environmental factors on the (development of the) CNS (15–17). We described, for instance, abnormal fetal state cycling with unique but properly synchronized transitions from state 1F into 4F in a case of heavy maternal alcohol consumption (18).
The present findings have shown evidence of a disorganizing effect of acute low dose maternal alcohol ingestion on fetal behavioral state cycling. The concordant association between the three state parameters was more frequently disrupted on the experimental days than on the control days as reflected by the increased %NoC. The %NoC may be considered a measure of functional chaos and is often called unclassified or indeterminate sleep in other studies using different criteria and/or variables to determine sleep states. The dissociation between state parameters resulted mainly from an alcohol-induced reduction in fetal EMs. Data of both series were consistent with regard to the reduction in EMs and the increased %NoC during HRPs B-D. In series B, the first transition out of HRP B was also affected, and the %NoC was increased during the next successive A pattern. Overall, the disturbances during active sleep (C2F) were much more pronounced than those during quiet sleep (C1F), which demonstrate that the effect of alcohol is state-dependent.
The effects of an occasional drink were transient (i.e. they lasted <24 h), as the sequence of the control and experimental sessions did not significantly influenza the results. The consequence of acute alcohol-induced alteration of active or REM sleep is unknown. However, as normal development of REM sleep is thought to be a prerequisite for normal brain function in later life (19), repeated alteration of fetal REM sleep by frequent exposure to alcohol could be an important etiologic factor in the increased incidence of CNS dysfunctions seen in infants of alcoholic mothers (1–4). Neonates exposed to moderate or high alcohol levels throughout pregnancy have also been described to exhibit disturbed behavioral states. Although the absolute amounts of neonatal quiet and active sleep were generally unchanged, characteristic disturbances comprised a greater proportion of indetermine sleep, poorer quality of quiet sleep (i.e. the neonates had more difficulty reaching quiet sleep, and this sleep state was also more often interrupted by indeterminate sleep epochs), more gross body movements during sleep (restlessness), more EEG arousals, and increased power in the EEG in all sleep states (4–7).
Our results resemble observations in the fetal lamb made by Patrick et al. (20). They described dramatic changes in ECoG and electrooculographic activities after a single i.v. dose of ethanol (1 g/kg of maternal body weight) infused over 1 h into the near-term pregnant ewe. The electrooculographic activity decreased rapidly (within 30 min after the onset of infusion) and remained suppressed by about 50% during the next 3 h. In this period, intermediate ECoG activity was seen (an unusual ECoG pattern) which increased from 12% before to 56% after the onset of ethanol infusion. Although these effects in the fetal lamb were brought about by an alcohol dosage four times higher than used in the human fetus, the comparable effect of alcohol on the occurrence of EMs in the human and sheep fetus is probably due to the same mechanism. In addition, disruptive effects of alcohol ingestion on ocular motor function (velocity and coordination of the eyes) have been known for a long time in the human adult (21). A possible location for the influence on CNS pathways controlling ocular motor behavior may be mesencephalic and pontine areas which are also known to control sleep and wakefulness (22).
It is open to question whether the alcohol-induced suppression of EMs in the human fetus does also imply disturbances in cortical brain activity as found in the fetal lamb. However, EEG changes in neonates who had been frequently exposed to moderate to high alcohol levels during pregnancy leave open the possibility that also fetal brain activity is affected after acute maternal alcohol intake. At present, such evidence cannot be obtained for obvious reasons.
FBM were reduced from about 30 min after the onset of maternal drinking and they disappeared sooner when the recording started in quiet sleep (series A). The latter might be explained by the fact that fetuses are less prone to breathe when in quiet sleep and adverse stimuli may attenuate this (23). McLeod et al. (14) also found that maternal alcohol intake suppresses FBM. In their study, FBM were abolished within 45 min after the onset of maternal drinking (0.25 g/kg of maternal body weight over 15 min), and remained almost completely suppressed for 3 h. The fall in breathing incidence coincided with the time at which maternal blood ethanol concentration was highest (∼0.3 mg/mL). In sheep, i.v. infusion of alcohol (1 g ethanol/kg of maternal body weight) over 1 h into the near-term pregnant ewe suppressed FBM for 9 h (20). A role of prostaglandins has been incriminated for the alcohol-induced suppression of fetal breathing activity (24). The sudden fall in FBM found on the experimental days cannot be explained by a difference in maternal glucose content, because the glucose level showed similar trends on the control and experimental days both in our study and the one by McLeod et al. (14). The gradual fall in breathing activity on the control days, on the other hand, can be explained by the well known decrease in maternal glucose level with time (23).
Maternal alcohol intake during pregnancy is a major although avoidable cause of impaired infant development. Permanent adverse effects of alcohol on the fetus have already been found after a daily intake of 1-2 drinks (3,25). The present study clearly shows that a modest alcohol intake by the pregnant woman has an acute effect on fetal behavioral state organization. This prenatal effect shows a resemblance to the disorganized sleep patterns found in neonates of alcoholic mothers. Knowledge of alteration of fetal brain function immediately after alcohol intake might be more convincing in an effort to discourage pregnant women from drinking than the warning against increased risks of neurobehavioral handicaps in later life. Our results, therefore, are of importance when counseling women about the risks of prenatal alcohol consumption.
Abbreviations
- FHR:
-
fetal heart rate
- HRP:
-
heart rate pattern
- C1F:
-
coincidence of state 1F parameters (F for fetal)
- NoC:
-
no coincidence of state parameters
- EM:
-
eye movements
- FBM:
-
fetal breathing movements
- REM:
-
rapid eye movement
- ECoG:
-
electrocorticographic
References
Day NL, Richardson GA 1991 Prenatal alcohol exposure: a continuum of effects. Semin Perinatol 15: 271–279
Spohr HL, Willms J, Steinhausen HC 1993 Prenatal alcohol exposure and long-term developmental consequences. Lancet 341: 907–910
Streissguth AP, Sampson PD, Barr HM 1989 Neurobehavioral dose-response effects of prenatal alcohol exposure in humans from infancy to adulthood. Ann NY Acad Sci 562: 145–158
Coles CD 1993 Impact of prenatal alcohol exposure on the newborn and the child. Clin Obstet Gynecol 36: 255–266
Ioffe S, Chernick V 1988 Development of the EEG between 30 and 40 weeks' gestation in normal and alcohol-exposed infants. Dev Med Child Neurol 30: 797–807
Rosett HL, Snyder P, Sander LW, Lee A, Cook P, Weiner L, Gould J 1979 Effects of maternal drinking on neonate state regulation. Dev Med Child Neurol 21: 464–473
Scher MS, Richardson GA, Coble PA, Day NL, Stoffer DS 1988 The effects of prenatal alcohol and marijuana exposure: disturbances in neonatal sleep cycling and arousal. Pediatr Res 24: 101–105
Dillner L, Josefson D, Karcher H, Sheldon T, Dorozynski A, Zinn C 1996 Alcohol-pushing the limits. BMJ 312: 7–9
Mulder EJH, Visser GHA, Bekedam DJ, Prechtl HFR 1987 Emergence of behavioural states in fetuses of type-1 diabetic women. Early Hum Dev 15: 231–252
Mulder EJH, O'Brien MJ, Lems YL, Visser GHA, Prechtl HFR 1990 Body and breathing movements in near-term fetuses and newborn infants of type-1 diabetic women. Early Hum Dev 24: 131–152
Dawes GS, Redman CWG, Smith JH 1985 Improvements in the registration and analysis of fetal heart rate records at the bedside. Br J Obstet Gynaecol 92: 317–325
Nijhuis JG, Prechtl HFR, Martin CB, Bots RSGM 1982 Are there behavioural states in the human fetus? Early Hum Dev 6: 177–195
Bots RSGM, Nijhuis JG, Martin CB, Prechtl HFR 1981 Human fetal eye movements: detection in utero by ultrasonography. Early Hum Dev 5: 87–94
McLeod W, Brien J, Loomis C, Carmichael L, Probert C, Patrick J 1983 Effect of maternal ethanol ingestion on fetal breathing movements, gross body movements, and heart rate at 37 to 40 weeks' gestational age. Am J Obstet Gynecol 145: 251–257
Visser GHA, Mulder EJH, Prechtl HFR 1992 Studies on developmental neurology in the human fetus. Dev Pharmacol Ther 18: 175–183
Groome LJ, Watson JE 1992 Fetal behavioural states. J Maternal Fetal Invest 2: 183–194
Prechtl HFR 1974 The behavioural states of the newborn infant (a review). Brain Res 76: 185–212
Mulder EJH, Kamstra A, O'Brien MJ, Visser GHA, Prechtl HFR 1986 Abnormal fetal behavioural state regulation in a case of high maternal alcohol intake during pregnancy. Early Hum Dev 14: 321–326
Mirmiran M 1986 The importance of fetal/neonatal REM sleep. Eur J Obstet Gynecol Reprod Biol 21: 283–291
Patrick J, Richardson B, Hasen G, Clarke D, Wlodek M, Bousquet J, Brien J 1985 Effects of maternal ethanol infusion on fetal cardiovascular and brain activity in lambs. Am J Obstet Gynecol 151: 859–867
Gale BW, Abel LA, Christian JC, Sorbel J, Yee RD 1996 Saccadic characteristics of monozygotic and dizygotic twins before and after alcohol administration. Invest Ophthalmol Vis Sci 37: 339–344
Hobson A, Lydic R, Baghdoyan H 1986 Evolving concepts of sleep cycle generation: from brain centers to neuronal populations. Behav Brain Sci 9: 371–448
Mulder EJH, Boersma M, Meeuse M, van der Wal M, van de Weerd E, Visser GHA 1994 Patterns of breathing movements in the near-term human fetus: relationship to behavioural states. Early Hum Dev 36: 127–135
Smith GN, Patrick J, Sinervo KR 1991 Effects of ethanol exposure on the embryofetus: experimental considerations, mechanisms, and the role of prostaglandins. Can J Physiol Pharmacol 69: 550–569
Ernhart CB, Sokol RJ, Martier S, Moron P, Nadler D, Ager JW, Wolf A 1987 Alcohol teratogenicity in the human: A detailed assessment of specificity, critical period, and threshold. Am J Obstet Gynecol 156: 33–39
Author information
Authors and Affiliations
Additional information
No financial support was provided from extramural sources.
Rights and permissions
About this article
Cite this article
Mulder, E., Morssink, L., Van Der Schee, T. et al. Acute Maternal Alcohol Consumption Disrupts Behavioral State Organization in the Near-Term Fetus. Pediatr Res 44, 774–779 (1998). https://doi.org/10.1203/00006450-199811000-00022
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199811000-00022
This article is cited by
-
Fetal heart rate, heart rate variability, and heart rate/movement coupling in the Safe Passage Study
Journal of Perinatology (2019)
-
Fetal heart rate and motor activity associations with maternal organochlorine levels: results of an exploratory study
Journal of Exposure Science & Environmental Epidemiology (2014)
-
Selective Serotonin Reuptake Inhibitors Affect Neurobehavioral Development in the Human Fetus
Neuropsychopharmacology (2011)