Abstract
Lower birth weight and growth retardation has been found in studies with laboratory animals, in children born of mothers exposed to accidental high levels of polychlorinated biphenyls (PCBs) and related compounds, and in children born of mothers who consumed PCB-contaminated fish. The effect of background exposure to PCBs and dioxins on birth size and growth in human newborns, however, is still unknown. This study examined birth size and postnatal growth of term newborns in relation to their background PCB and dioxin exposure. Birth weight and weight, length, and head circumference were measured at 10 d and 3, 7, 18, and 42 mo of age in 207 children, of whom 105 were breast-fed and 102 were formula-fed during infancy. The effect of in utero exposure to PCBs on birth size, assessed by cord and maternal plasma PCB levels, was investigated in the whole group. The effect of prenatal PCB exposure on postnatal growth was studied in the formula-fed group, whereas the effect of prenatal as well as lactational exposure to PCBs and dioxins on postnatal growth was studied in the breast-fed group. After adjustment for covariates, cord and maternal plasma PCB levels where both negatively associated with birth weight. Infants with high cord plasma PCB levels (P90 = 0.80 µg/L) weighed 165 g less compared with infants with low cord plasma PCB levels (P10 = 0.20 µg/L). Cord and maternal plasma PCB levels where both significantly associated with lower growth rate, defined as change in SD score (SDS) of weight, length, and head circumference from birth to 3 mo in the formula-fed group (all p values <0.05). No negative effects of prenatal PCB exposure on growth rate were found from 3 to 42 months of age. Postnatal PCB and dioxin exposure was not negatively associated with growth rate in the breast-fed group. In utero exposure to environmental levels of PCBs is negatively associated with birth weight and postnatal growth until 3 mo of age. Although this growth delay was described in healthy term born infants, intrauterine and postnatal growth retardation are potentially harmful to the developing human and should be avoided by reducing maternal PCB and dioxin body burden, and consequently fetal exposure to these pollutants.
Similar content being viewed by others
Main
PCBs and dioxins (PCDDs and PCDFs), summarized as dioxins, are widespread environmental contaminants that are lipophilic and resistant to either chemical and biological degradation. PcBs and dioxins frequently occur simultaneously in the environment and accumulate especially in fat tissue (1,2). The half-lives of the congeners are fairly long, for instance 7 y for 2,3,7,8-tetrachlorodibenzo-p-dioxin (3). In western industrial countries, e.g. The Netherlands, considerable amounts of PCBs and dioxins have been found in fish, meat, dairy products, and, in particular, in human milk (4). Human exposure to PCBs and dioxins is mainly through the food chain (5,6). The human fetus is exposed to PCBs and dioxins through placental transport (7,8), and large quantities of PCBs and dioxins are transferred to the infant during breast-feeding (8,9).
Studies in rhesus monkeys (10) and rats (11,12) showed that prenatal exposure to PCBs was associated with reduced birth weight. The negative effect of prenatal PCB exposure may persist beyond the newborn period; exposed rats gained weight more slowly than did controls during the first 4 mo of lief (12). Intrauterine growth retardation was reported in two incidents in Asia (Japan and Taiwan) in which pregnant women consumed cooking oil accidentally contaminated with PCBs and related compounds, referred as the Yusho and Yu-Cheng incidents (13,14). Yu-Cheng children were smaller and weighed less compared with their matched controls at school age (14,15). In the United States, reduced birth weight and a shorter gestation was also observed in infants with elevated cord PCB levels whose mothers consumed contaminated fish from Lake Michigan (16).
We reported previously that in Dutch infants subtle signs of neurologic dysfunctioning (17), small delay in psychomotor development (18), alterations in thyroid hormone (19), and immunologic status (20) are associated with perinatal PCB and dioxin exposure. In this report we describe the effect of pre-and postnatal exposure to PCBs and dioxins on birth size and growth in children from birth until 42 mo of age. This study is part of the Dutch PCB/dioxin project and an EC funded collaborative study, a prospective follow-up study on possible adverse effects of environmental exposure to PCBs and dioxins on growth and development of young children.
METHODS
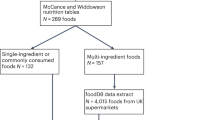
Subjects. From 1990 to 1992, infants born at term (37-42 wk of gestation), without congenital anomalies or diseases were recruited for this study. Pregnancy and delivery had to be without complications or serious illnesses. All mother-infant pairs included were Caucasian. To study the effects of prenatal and postnatal exposure to PCBs and dioxins, women were included who intended to give formula-feeding (FF group) next to women who intended to breast-feed their child for at least 6 wk (BF group). All FF infants received formula from a single batch (Almiron M2, Nutricia NV, The Netherlands) from birth until 7 mo of age. In this formula, concentrations of both PCBs and dioxins were negligible. Participants lived in Rotterdam or its immediate surroundings, a highly industrialized and densely populated area in the western part of The Netherlands. The study design and chemical analysis methods are described elsewhere (9).
This study was approved by the Medical Ethics Committee of the Sophia Children's Hospital Rotterdam. During the last month of pregnancy, mothers were visited at home for an explanation of the study protocol. Informed consent was given by the parents.
Outcome measures. Weight at birth was measured by the obstetrician or midwife. Weight, length or height, and head circumference were measured at the ages of 10 d and 3, 7, 18, and 42 mo. Because length and head circumference at birth were not measured in most newborns, length and head circumference measured at 10 d and birth weight were used as measurements for birth size. Until 7 mo of age, infants were weighed naked on a baby scale up to the nearest 5 g, and length was measured on a length board up to the nearest millimeter. At 18 and 42 mo of age, children were weighed on a beam scale in kilograms, and their height was measured with a Harpenden stadiometer in centimeters. Head circumference was measured in centimeters with a standard tape at all ages.
Weight, length or height, and head circumference at each time point were converted into SDS using weight, height, and head circumference standards of healthy Dutch children as reference data (21). Growth rate per time interval, e.g. 0-3 mo, was defined as change in SD score of weight (ΔwSDS), length (ΔhSDS), and head circumference (ΔhcSDS) between 3 mo and birth/10 d. Growth rate from 3 to 7 mo was defined as change in SDS of weight, height, and head circumference between 7 and 3 mo. The same definition was used for growth rate from 7 to 18 mo and 18 to 42 mo of age.
Exposure variables. Analysis of four PCB congeners, International Union for Pure and Applied Chemistry (IUPAC) nos. 118, 138, 153, and 180 in maternal plasma samples, collected during the last month of pregnancy and in cord plasma samples, was performed at the Nutrition and Food Research Institute, Zeist, The Netherlands (9). The PCB sum (ΣPCB) was calculated by adding up the four congeners in each plasma sample and was reported on a volume basis (µg/L).
A 24-h representative breast milk sample was collected from nursing mothers in the 2nd wk after delivery and was analyzed for the 17 most abundant 2,3,7,8-substituted PCDD and PCDF congeners, three planar PCBs IUPAC nos. 77, 126, and 169; three mono-ortho PCBs IUPAC nos. 105, 118, 156; two di-ortho PCBs IUPAC nos. 170, 180; and 18 other nonplanar PCBs IUPAC nos. 28, 52, 66, 70, 99, 101, 128, 137, 138, 141, 151, 153, 177, 183, 187, 194, 195, and 202 (9,22). To express the total toxic potency of dioxins and planar, mono-ortho, and di-ortho PCBs (dioxin-like PCBs), the TEQ factor approach was used according to Safe and WHO (23,24). By multiplying the concentration in breast milk (nanograms/kg of milk fat) and its TEQ factor value, the TEQ of each congener was calculated (nanograms of TEQs/kg of milk fat). By adding up the TEQs of all congeners the total TEQ value was obtained. Levels of all exposure variables have been published elsewhere (9).
Prenatal PCB exposure was assessed from the ΣPCB in maternal and cord plasma. Postnatal PCB and dioxin exposure was calculated by multiplying the total TEQ levels measured in breast milk with the number of weeks of breast-feeding as reported by the mother.
Other variables. Potential confounding variables for birth size and growth were selected from a list of pertaining data on socioeconomic background, maternal (health) history, pregnancy and delivery, gestational age, parity, gender, and fetal exposure to alcohol and cigarette smoking. Parent's height served to calculate the TH (centimeters) as predicting variable for birth size and growth. TH was calculated according to the formulas: (father's height + mother's height + 12)/2 + 3 cm for boys and (father's height + mother's height - 12)/2 + 3 cm for girls (25). TH in centimeters was converted into target hSDS, using Dutch standards for final height (21).
Statistics and data analysis. Maternal and cord plasma PCB levels were normalized by natural logarithmic transformation. The t test, χ2, and Mann Whitney U test were used to compare differences between the BF and FF group.
The influence of prenatal PCB exposure on birth size was studied in the whole group. Multiple linear regression analyses were carried out to study the influence of prenatal PCB exposure on birth weight, length, and head circumference at 10 d (SDS). Potential confounding variables were considered to be included in the regression model if they were related to the outcome variable, known from literature and clinical knowledge. Furthermore, variables were also included in the final model when they influenced the regression coefficient of the exposure variable in such a way that confounding exists. If the crude and adjusted estimates were meaningfully different, then confounding was present and one or more control variables were included in the regression model (26).
The influence of PCB and dioxin exposure through formula-feeding is negligible, therefore the FF group represents infants prenatally exposed to PCBs and dioxins. The influence of cord and maternal plasma PCB levels on changes in SDS of weight, length, and head circumference per time interval, e.g. growth rate from 0-3, 3-7, 7-18, and 18-42 mo was studied in the FF group. The BF group represents infants who were also post-natally exposed to PCBs and dioxins. The influence of PCB and dioxin exposure through breast milk on growth rate from 0-3, 3-7, 7-18, and 18-42 mo was therefore studied in the BF group. Multiple linear regression analyses were also carried out in both groups as described above. Furthermore, the effect of feeding type in relation to growth rate was investigated in the whole group in the same manner. Results are considered statistically significant at a p value ≤0.05.
RESULTS
In this study 207 mother-infant pairs were enrolled, of whom 105 were in the BF group and 102 in the FF group. Table 1 represents the general characteristics of all mother-infant pairs. There were no differences between both feeding groups except a smaller number of boys (p < 0.05) and a lower level of maternal education in the FF group (p < 0.001). In Table 2 levels of PCBs and dioxins measured in plasma and maternal milk samples are given. The sum of four PCB congeners could be calculated in 206 maternal and 182 cord plasma samples. In human milk, representative dioxin, planar, and mono- and di-ortho PCB congeners were available in 83, 95, 100, and 100 milk samples, respectively. The remaining plasma and human milk samples missed or were not analyzed due to organizational failure. The sum of PCB- and dioxin-TEQ (total TEQ) could be calculated for 80 breast milk samples.
Anthropometric data for both feeding groups are given in Table 3. All children were in the normal range when compared with the standards of Dutch children as reference data (21). There were no differences in birth weight between the two feeding groups. At 10 d a significantly higher mean body length in BF girls was found compared with the FF counterparts (p = 0.02). Significantly higher mean body weights at 7, 18, and 42 mo of age were found in FF boys compared with BF boys (all p values <0.05). A smaller number of children at 42 mo are presented; 14 children were lost to follow-up due to lack of interest (n = 10) and migration (n = 4).
The effect of prenatal PCB exposure on birth size was analyzed by means of multiple linear regression analyses with birth weight, length at 10 d, and head circumference at 10 d as dependent variables and lnΣPCB in cord plasma as exposure variable. Table 4 shows that, after adjustment for parity, gestational age, TH, smoking, and alcohol use during pregnancy, lnΣPCB in cord plasma is negatively associated with birth weight (p = 0.03). An infant with a median PCB level (P50 = 0.41 µg/L) in cord plasma has a birth weight of 86 g less than an infant with a cord PCB level at P10 (0.20 µg/L). An infant with a cord PCB level at P90 (=0.80 µg/L) has a birth weight of 165 g less than an infant with a cord PCB level at the P10 level. Almost similar results were found with lnΣPCB in maternal plasma as a measure for prenatal PCB exposure (Table 5). Parity, gestational age, TH, smoking, and alcohol use during pregnancy have a significant effect on birth weight as well. Infants exposed to maternal smoking and alcohol use during pregnancy have predicted birth weights of 144 g, respectively, 138 g lower compared with infants not exposed to maternal smoking and alcohol use (Table 4). There were no significant negative effects of InΣPCB in cord and InΣPCB in maternal plasma on length/hSDS and head circumference/hcSDS measured at 10 d. According to the regression model presented in Table 4, a prediction was made for birth weight in infants exposed to different levels of ΣPCB in cord plasma with or without exposure to cigarette and alcohol use during pregnancy (Fig. 1). Prediction for birth weight is given when gestational age is 40.1 wk (mean value), TH is 178.8 cm (mean value), and parity is zero (first born).
The prediction of birth weight in relation to cord plasma PCB levels is shown. In addition, the relation of fetal exposure to cigarette smoking and alcohol during pregnancy and birth weight is given. Prediction is given for birth weight when gestational age is 40.1 wk (mean value), TH is 178.8 cm (mean value), parity is zero (first born). Predicted birth weight (g) = -5789 - 119.4·(lnΣPCBcord) - 144.1·(smoking) - 138.4·(alcohol) + 150.1·(40.1) + 17.3·(178.8) + 163.8·(0) ΣPCBcord = the sum of PCB congeners 118, 138, 153, and 180 in cord blood. Smoking, 0 = no; 1 = yes. Alcohol use, 0 = no; 1 = yes.
The effect of prenatal PCB exposure on growth rate between 0-3, 3-7, 7-18, and 18-42 mo was studied by multiple linear regression analysis in the FF group. After adjustment for covariates, InΣPCB in cord plasma was negatively associated with ΔwSDS, ΔhSDS, and ΔhcSDS between 0 and 3 mo (all p values < 0.05, Table 6). This means that there is a significant negative effect of cord plasma PCB levels on growth rate of weight, length, and head circumference from 0 to 3 mo. Similar results were found when InΣPCB in maternal plasma was entered in the regression analyses as a measure for prenatal PCB exposure. After adjustment for the same covariates as presented in Table 6, regression coefficients (standard errors) for InΣPCB in maternal plasma on ΔwSDS, ΔhSDS, and ΔhcSDS between 0 and 3 mo are -0.51 (0.18), -0.40 (0.14), and -0.30 (0.14), respectively (all p values < 0.05). There were no negative associations found between prenatal PCB exposure and growth rate between 3-7, 7-18, and 18-42 mo of age in the FF group.
The effect of pre- as well as postnatal PCB and dioxin exposure on growth rate between 0-3, 3-7, 7-18, and 18-42 mo was studied in the BF group. Neither an effect of prenatal PCB exposure nor an effect of total TEQs in breast milk multiplied by the number of weeks of breast-feeding (lactational exposure), was found on growth rate between 0 and 3 mo in the BF group (Table 7). After adjustment for covariates, postnatal PCB and dioxin exposure was negatively associated with change in length SDS (ΔhSDS) (regression coefficient = -0.21, p = 0.04) but not with change in SD of weight (ΔwSDS) and head circumference (ΔhcSDS) from 3 to 7 mo. Growth rate studied from 7-18 and 18-42 mo, were neither influenced by pre- nor postnatal PCB and dioxin exposure in the BF group.
In addition, the effect of feeding type during infancy on growth rate was studied in the whole group. No significant effect of feeding type on growth rate was found between 0-3, 7-18, and 18-42 mo of age. Growth rate between 3 and 7 mo, however, was significantly influenced by feeding type; infants from the BF group showed a lower ΔwSDS (regression coefficient (SE) = -0.16 (0.08) p = 0.05) and ΔhSDS (regression coefficient SE = -0.16 (0.07) p = 0.04) from 3 to 7 mo compared with infants from the FF group, after adjustment for maternal education, gender, TH, and SDS of weight and length at 3 mo. There was no effect of feeding type on growth rate of head circumference from 3 to 7 mo.
DISCUSSION
We report that in utero exposure to environmental levels of PCBs negatively influences birth weight. Furthermore, prenatal PCB exposure was negatively associated with growth rate of weight, length, and head circumference from birth to 3 mo of age.
These results are partly consistent with studies in laboratory animals (10,12) and human studies concerning exposure by accident, the Yusho (13) and Yu-Cheng incidents (14). In the Yu-Cheng incident reduced growth was found until school age (14,15), and in the Yusho incident female children with lower birth weights remained smaller and lighter at later ages, e.g. school age, and these differences correlated with the PCB concentration in breast milk of the Japanese mothers. This phenomenon, however, was not observed in male children (27). Taylor et al. (28) studied the relation between birth weight and gestational age among live offspring of women occupationally exposed to PCBs and reported a significant association between increased serum PCB levels and lower birth weight and gestational age. Jacobson et al. (29) reported a decrease in birth weight of 160-190 g as well as a 0.6-0.7-cm smaller head circumference in infants of mothers who consumed contaminated fish from Lake Michigan. A weight deficit of 1.8 kg at 4 y age was described in the same cohort, associated with prenatal PCB exposure (16,29).
Rogan et al. (30) studied the effects of environmental exposure to PCBs in North Carolina, but did not find an effect of prenatal PCB exposure on birth weight, whereas we report that prenatal PCB exposure is associated with reduced birth weight and growth rate until 3 mo of age. In North Carolina, as well as in Michigan, total PCB levels were measured in cord and maternal blood with the Webb McCall method, using packed column gas chromatography (8,30), whereas in our study PCB levels were measured by gas chromatography with electron capture detection, which provides information of individual PCB congeners (9). Although state-of-the-art at the time of the study, the Webb McCall method is a crude measure of PCB levels and gives no information of individual congeners. Differences between results from the North Carolina and Dutch cohort can be explained by the following. Environmental levels of PCBs and dioxins are probably lower in the United States compared with background levels in The Netherlands (4). This might explain why effects on birth weight in the Michigan cohort are similar to what we have found, but not with the findings in the North Carolina cohort. Probably levels of exposure in the Michigan cohort, which are slightly above background PCB levels, are comparable to levels measured in the Dutch cohort. On the other hand, levels could be similar in North Carolina and the Netherlands, but due to a presumably more accurate measure of exposure in the Netherlands, effects on birth weight and growth were found in the Dutch cohort and not in the North Carolina cohort. Differences in analytical measurements of exposure data still makes it difficult to compare PCB levels from different regions (4).
Both cord and maternal plasma PCB levels were negatively associated with birth weight and postnatal growth rate until 3 mo of age. Although PCB levels in cord plasma are a direct measure of fetal exposure to PCBs when compared with maternal plasma PCB levels measured during pregnancy, the analytical precision of PCB determination in cord plasma is lower than for maternal plasma, due to a lower lipid content in cord plasma. However, our results for cord as well as maternal plasma PCB levels are similar and therefore support the hypothesis that in utero exposure to PCBs affects fetal growth (birth weight) and growth during early infancy.
Growth retardation as described in this study might be due to the transplacental transfer of the four PCB congeners measured, but could also be due to other contaminants, e.g. PCB, dioxins, and PCB metabolites. At the time of this study, it was not possible to determine dioxins and dioxin-like PCB congeners in plasma, as these measurements required a large volume of blood (100-200 mL). Only the four most prevalent PCB congeners could be analyzed. There is a good correlation between PCB congeners measured by us in maternal and cord plasma and other PCB and dioxin congeners in human milk (9). It is not possible to rule out the effect of other toxic substances, nor is it possible to determine the mechanism by which prenatal exposure to PCBs and related compounds causes a reduction in birth weight and postnatal growth. Additional studies in which more PCB and dioxin congeners, as well as their metabolites are measured, need to clarify which congeners are responsible for diminished growth. The biochemical effects of 2,3,7,8-tetrachlorodibenzo-p-dioxin and related compounds including dioxin-like PCBs, can be grouped in three classes; altered metabolism, resulting from changes in enzyme levels; altered homeostasis, resulting from changes in hormones and their receptors; and altered growth and differentiation, resulting from changes in growth factors and their receptors (31).
In this study a lower growth rate in relation to prenatal PCB exposure was observed up to 3 mo of age in the FF group. In the BF group, however, this prenatal effect was not observed. Except for a lower growth rate for body lenth between 3 and 7 mo, no effects of lactational exposure to PCBs and dioxins on growth rate from birth to 42 mo of age was observed. This effect of lactational exposure on growth rate for body weight and head circumference from 3 to 7 mo was not found. The results for postnatal PCB and dioxin exposure on growth rate are not consistent in time and therefore could be a chance finding. We presented results only from postnatal PCB and dioxin TEQ exposure on growth rate in BF infants, but results were similar when postnatal exposure was measured from the four PCB congeners (IUPAC nos. 118, 138, 153, and 180) in breast milk. This further supports our finding that lactational exposure to PCBs as well as dioxins and dioxin-like PCBs are not negatively associated with postnatal growth rate until 42 mo of age. We could speculate on the positive influences of breast milk or breast-feeding, despite the high levels of PCBs and dioxins transferred to the infant. Numerous studies on infant nutrition show that breast-feeding has a beneficial effect on growth, morbidity, and neurologic and cognitive functioning later in life (32). Breast milk contains certain hormones, e.g. thyroid hormone, prolactin, gonadotrophin hormone, adrenal gland hormones, and long-chain polyunsatured fatty acids, nucleotides, and epidermal growth factors (33), which are not available in formula-feeding. Perhaps these factors, or factors associated with breast-feeding, e.g. socioeconomic environment, overcome the diminished growth observed in the FF group.
We reported that growth in BF infants differs from that of FF infants. BF boys weighed significantly less than their FF counterparts at 7, 18, and 42 mo of age, and BF infants had a lower growth rate for weight and length from 3 to 7 mo of age compared with that of FF infants. These findings are partly in accordance with previous reports. Dewey et al. (34) described that weight patterns of BF infants differed from those of FF infants and from current reference data.
The following is more a thorough discussion of the significance of the reduced birth weight and postnatal growth rate in term infants. It is generally known that growth before birth is vitally important to the child's future well being. According to the studies of Barker and colleagues, a relationship exists between a lower birth weight and a number of diseases in adult life, such as a higher incidence of cardiovascular diseases and type II diabetes (35,36). Barker and colleagues suggested that these diseases are programmed by an inadequate supply of nutrients or oxygen in utero or immediately after birth. The phenomenon of programming suggests that undernutrition in early life permanently changes body structure and function. This conclusion has been strengthened by animal studies which show that experimentally induced low birth weight is followed by raised systolic blood pressure in adult rats (37). Furthermore, results from the Dutch Famine Birth Cohort Study (38) showed that birth weight from offspring born at the time of severe famine in 1944-1946 was 257 g lower than that of control subjects when femine exposure was in the third trimester of pregnancy, and 133 g elevated when famine exposure was in the first trimester. Another study reported that women born during this period of acute famine had twice the risk to become schizophrenic (39). Offspring from the second generation showed that first born infants of women prenatally exposed to acute famine during the first trimester of pregnancy showed 73-g higher birth weights compared with control subjects, and second borns showed 96-g lower birth weights compared with control subjects (40). It was concluded that maternal undernutrition early in pregnancy may have had an effect in offspring birth weight and a moderate effect on birth weight in the second generation. Undernutrition might have led to a permanent effect on the uterus of the female newborn, and during pregnancy later this would have an effect on birth weight of her offspring in the second generation. Among male infants subjected to in utero famine exposure and examined at 18 y, mid-pregnancy exposure was associated with reduced body mass index, whereas an increased prevalence of obesity was observed among male infants exposed in the first trimester (41). Results from the above-mentioned studies show that events during pregnancy can have consequences after birth and later in life.
In conclusion, it is not clear what is being programmed in utero when exposed to PCBs and dioxins and what the impact of a lower birth weight has for later development, but given the results of these studies and what we have reported, all factors that negatively influence fetal and postnatal growth should be regarded as harmful. Therefore, all efforts should be directed toward reduction of maternal body burden long before pregnancy to reduce prenatal PCB exposure and consequently avoid reduced fetal and infant growth.
Abbreviations
- PCB:
-
polychlorinated Biphenyl
- PCDD:
-
polychlorinated dibenzo-p-dioxin
- PCDF:
-
polychlorinated dibenzo-p-furan
- TEQ:
-
toxic equivalent
- hSDS:
-
height SD score
- wSDS:
-
weight SD score
- hcSDS:
-
head circumference SD score
- ΔSDS:
-
change in SD score
- TH:
-
target height
- FF:
-
formula-fed
- BF:
-
breast-fed
REFERENCES
de Voogt P, Brinkman UAT 1989 Production, properties and usage of polychlorinated biphenyls. In: Kimbrough Rd, Jensen A (eds) Halogenated Biphenyls, Terphenyls, Naphtalenes, Dibenzodioxins and Related Products, 2nd Ed. Elsevier, Amsterdam, 3–46.
Eitzer BD, Hites RA 1989 Atmosferic transport and deposition of polychlorinated dibenzo-p-dioxins and dibenzofurans. Environ Sci Toxicol 23: 1396–1401
Van den Berg M, De Jongh J, Poiger H, Olson JR 1994 The toxicokinetics and metabolism of polychlorinated dibenzo-p-dioxins (PCDDs) and dibenzofurans (PCDFs) and their relevance for toxicity. Crit Rev Toxicol 24: 1–74
Yrjänheikki, EJ (ed) 1989 Levels of PCBs, PCDDs, and PCDFs in Breastmilk; Results of WHO-Coordinated Interlaboratory Quality Control Studies and Analytical Field Studies. Regional office for Europe, FADL, World Health Organization, Copenhagen, 13–19.
Theelen RMC, Liem AKD, Slob W, van Wijnen JH 1993 Intake of 2,3,7,8-chlorine substituted dioxins, furans, and planar PCBs from food in The Netherlands: median and distribution. Chemosphere 27: 1625–1635
Fürst P, Beck H, Theelen R 1992 Assessment of human intake of PCDDs and PCDFs from different environmental sources. Toxic Substances Journal World Health Organization 12: 133–150
Masuda Y, Kagawa R, Kuroki H, Kuratsune, M., Yoshimura, T, Taki, I, Kusada, M, Yamashita, F, Hayashi, M 1978 Transfer of polychlorinated biphenyls from mothers to foetuses and infants. Food Cosmet Toxicol 16: 543–546
Jacobson JL, Feinn GG, Jacobson SW, Schwartz PM, Dowler JK 1984 The transfer of polychlorinated biphenyls (PCBs) and polybrominated biphenyls (PBBs) across the human placenta and into maternal milk. Am J Public Health 74: 378–379
Koopman-Esseboom C, Huisman M, Weisglas-Kuperus N, Van der Paauw CG, Tuinstra LG, Boersma R, Sauer PJJ 1994 PCB and Dioxin levels in plasma and human milk of 418 Dutch women and their infants. Predictive value of PCB congener levels in maternal plasma for fetal and infant's exposure to PCBs and Dioxins. Chemosphere 28: 1721–1732
Allen JR, Barsotti DA, Carstens LA 1980 Residual effects of polychlorinated biphenyls on adult nonhuman primates and their offspring. J Toxicol Environ Health 6: 55–66
Overmann SR, Kostas J, Wilson LR, Shain W, Bush B 1987 Neurobehavioral and somatic effects of perinatal PCB exposure in rats. Environ Res 44: 56–70
Brezner E, Terkel J, Perry AS 1984 The effect of Aroclor 1254 (PCB) on the physiology of reproduction in the female rat. I. Comp Biochem Physiol C 77: 65–70
Harada M 1976 Intrauterine poisoning: Clinical and epidemiological studies and significance of the problem. Bull Inst Const Med Kumamoto Univ 25( suppl): 1–69
Rogan WJ, Gladen BC, Hung KL, Koong, SL, Shih, LY, Taylor, JS, Wu, YC, Yang, D, Ragan, NB, Hsu, CC 1988 Congenital poisoning by polychlorinated biphenyls and their contaminants in Taiwan. Science 241: 334–336
Guo YL, Lin CJ, Yao WJ, Ryan JJ, Hsu CC 1994 Musculoskeletal changes in children prenatally exposed to polychlorinated biphenyls and related compounds (Yu-Cheng children). J Toxicol Environ Health 41: 83–93
Fein GG, Jacobson JL, Jacobson SW, Schwartz PM, Dowler JK 1984 Prenatal exposure to polychlorinated biphenyls: effects on birth size and gestational age. J Pediatr 105: 315–320
Huisman M, Koopman-Esseboom C, Fidler V, Hadders-Algra M, van der Paauw CG, Tuinstra LG, Weisglas-Kuperus N, Sauer PJ, Touwen BC, Boersma ER 1995 Perinatal exposure to polychlorinated biphenyls and dioxins and its effect on neonatal neurological development. Early Hum Dev 41: 111–127
Koopman-Esseboom C, Weisglas-Kuperus N, de Ridder MA, Van der Paauw CG, Tuinstra LG, Sauer PJ 1996 Effects of polychlorinated biphenyl/dioxin exposure and feeding type on infants' mental and psychomotor development. Pediatrics 97: 700–706
Koopman-Esseboom C, Morse DC, Weisglas-Kuperus N, Lutkeschipholt, IJ, Van der Zwan CG, Tuinstra LG, Brouwer A, Sauer PJ 1994 Effects of dioxins and polychlorinated biphenyls on thyroid hormone status of pregnant women and their infants. Pediatr Res 36: 468–473
Weisglas-Kuperus N, Sas TC, Koopman-Esseboom C, van der Zwan CW, De Ridder MA, Beishuizen A, Hooijkaas H, Sauer PJ 1995 Immunologic effects of background prenatal and postnatal exposure to dioxins and polychlorinated biphenyls in Dutch infants. Pediatr Res 38: 404–410
Roede MJ, van Wieringen JC 1985 Growth diagrams 1980. Netherlands third nation-wide biometric survey. Tijdschr Soc Gezondheidszorg 63( suppl): 1–34
van Rhijn JA, Traag WA, van de Spreng PF, Tuinstra LG 1993 Simultaneous determination of planar chlorobiphenyls and polychlorinated dibenzo-p-dioxins and -furans in Dutch milk using isotype dilution and gas chromatography-high-resolution mass spectrometry. J Chromatogr 5: 297–306
Safe SH 1994 Polychlorinated Biphenyls (PCBs): environmental impact, biochemical and toxic responses, and Implications for risk assessment. Crit Rev Toxicol 24: 87–149
Ahlborg UG, Becking GC, Birnbaum LS, Brouwer, A, Derks, HJGM, Feeley, M, Golor, G, Hanberg, A, Larsen, JC, Liem, AKD, Safe, SH, Schlatter, C, Waern, F, Younes, M, Yrjänheikki, E 1994 Toxic equivalency factors for dioxin-like PCBs. Report on a WHO-ECEH and IPCS consultation, December 1993. Chemosphere 28: 1049–1067
van de Brande JL, van Gelderen HH, Monnens AH, (eds) 1990 In Kindergeneeskunde, Chap. 11. Bunge, Utrech, The Netherlands, 179–219.
Kleinbaum DG 1988 Applied Regression Analysis and Other Multivariable Methods, Chap. 11. Wadsworth Publishing Co., Belmont, CA, 163–165.
Yamashita F, Hayashi M 1985 Fetal PCB syndrome: clinical features, intrauterine growth retardation and possible alteration in calcium metabolism. Environ Health Perspect 59: 41–45
Taylor PR, Stelma JM, Lawrence CE 1989 The relation of polychlorinated biphenyls to birth weight and gestational age in the offspring of occupationally exposed mothers. Am J Epidemiol 129: 395–406
Jacobson JL, Jacobson SW, Humphrey HE 1990 Effects of exposure to PCBs and related compounds on growth and activity in children. Neurotoxicol Teratol 12: 319–326
Rogan WJ, Gladen BC, McKinney JD, Carreras, N, Hardy, P, Thullen, J, Tinglestad, J, Tully, M 1986 Neonatal effects of transplacental exposure to PCBs and DDE. J Pediatr 109: 335–341
Birnbaum LS 1994 The mechanism of dioxin toxicity: relationship to risk assessment. Environ Health Perspect 102( suppl 9): 157–167
Gordon N 1997 Nutrition and cognitive function. Brain Dev 19: 165–170
Koldovsky O, Thornburg W 1987 Hormones in milk, review. J Pediatr Gastroenterol Nutr 6: 172–196
Dewey KG, Heinig MJ, Nommsen LA, Peerson JM, Lönnerdal B 1992 Growth of breast-fed and formula-fed infants from 0 to 18 months: the DARLING study. Pediatr 89: 1035–1041
Barker DJ 1994 Outcome of low birthweight. Horm Res 42: 223–230
Martyn CN, Barker DJP, Osmond C 1996 Mothers' pelvic size, fetal growth, and death from stroke and coronary heart disease in men in the UK. Lancet 348: 1264–1268
Langley SC, Jackson AA 1994 Increased systolic blood pressure in adult rats induced by fetal exposure to maternal low protein diets. Clin Sci (Colch) 86: 217–222; discussion 121
Stein AD, Ravelli AC, Lumey LH 1995 Famine, third-trimester pregnancy weight gain, and intrauterine growth: the Dutch Famine Birth Cohort Study. Hum Biol 67: 135–150
Susser E, Neugebauer R, Hoek HW, Brown, AS, Lin, S, Labovitz, D, Gorman, JM 1996 Schizophrenia after prenatal famine. Further evidence [see comments]. Arch Gen Psychiatry 53: 25–31
Lumey LH, Stein AD, Ravelli AC 1995 Timing of prenatal starvation in women and birth weight in their first and second born offspring: the Dutch Famine Birth Cohort study. Eur J Obstet Gynecol Reprod Biol 61: 23–30
Ravelli GP, Stein ZA, Susser MW 1976 Obesity in young men after famine exposure in utero and early infancy. N Engl J Med 295: 349–353
Acknowledgements
The authors thank A. C. S. Hokken-Koelega, Pediatric Endocrinologist at the Sophia Children's Hospital Rotterdam, The Netherlands, for critical review of the manuscript, and all parents and their children for participating in this study.
Author information
Authors and Affiliations
Additional information
Supported by the Programme Committee Toxicology (PCT), Dutch Health Research Promotion Programme (SGO), and the European Commission for Environmental and Health Programmes Contract EV5V-CT92-0207.
Rights and permissions
About this article
Cite this article
Patandin, S., Koopman-Esseboom, C., De Ridder, M. et al. Effects of Environmental Exposure to Polychlorinated Biphenyls and Dioxins on Birth Size and Growth in Dutch Children. Pediatr Res 44, 538–545 (1998). https://doi.org/10.1203/00006450-199810000-00012
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199810000-00012
This article is cited by
-
Enantioselective Toxicity Effects of 2,2’,3,5’,6-Pentachloro Biphenyl (PCB-95) on Developing Brains in Zebrafish Larvae
Bulletin of Environmental Contamination and Toxicology (2021)
-
Dioxin-like and non-dioxin-like PCBs differentially regulate the hepatic proteome and modify diet-induced nonalcoholic fatty liver disease severity
Medicinal Chemistry Research (2020)
-
Effects of perinatal dioxin exposure on development of children: a 3-year follow-up study of China cohort
Environmental Science and Pollution Research (2019)
-
The relationship of maternal PCB, toxic, and essential trace element exposure levels with birth weight and head circumference in Chiba, Japan
Environmental Science and Pollution Research (2019)
-
Effects of intrauterine exposures to polychlorinated biphenyls, methylmercury, and lead on birth weight in Japanese male and female newborns
Environmental Health and Preventive Medicine (2017)