Abstract
This study reports the clearance of plasma triglyceride and phospholipid fatty acids during Intralipid 20% infusion (Pharmacia, Sweden) in nine ventilated preterm infants receiving parenteral nutrition. Blood samples were taken during lipid infusion and over a subsequent period of 36 h of fat-free parenteral nutrition. Plasma triglyceride fatty acids showed a uniform and rapid decline after lipid was stopped from the peak values recorded during infusion. In contrast, plasma phospholipid fatty acids showed a variable decline during fat-free nutrition. This variability appeared to be the result of a differing contribution of infused egg yolk phospholipid fatty acids to the measured plasma values, and to changing fatty acid composition of endogenous phospholipid in response to fat free nutrition. Red cell phospholipid fatty acid composition was stable over the 36-h clearance study period. These results indicate the complexity of interpretation of plasma fatty acids during lipid infusion. We conclude that red cell phospholipid fatty acids provide the only stable measure of tissue fatty acid composition in parenterally fed preterm infants.
Similar content being viewed by others
Main
Intravenous fat emulsions are an important component of parenteral nutrition regimens in premature infants. The metabolism of these emulsions has received considerable attention in the literature in recent years(1–3). However, the in vivo clearance of individual triglyceride and phospholipid fatty acids infused in the emulsion has not been previously documented. In addition, the influence of lipid infusions on red cell composition has not been assessed. These issues are important to address to provide a basis for the assessment of fatty acid status in the parenterally fed neonate and for the interpretation of fatty acid data in comparative trials of i.v. fat emulsions, as well as to contribute to a better understanding of the metabolism of i.v. administered fat.
This pilot study of parenteral lipid requirements of preterm infants aimed to characterize the clearance of triglyceride and phospholipid fatty acids during i.v. administration of Intralipid 20% (Pharmacia, Sweden). Plasma and red cell fatty acid composition were assessed during lipid infusion and over a subsequent period of 36 h of fat-free parenteral nutrition.
METHODS
Patients. Nine preterm, appropriate for gestational age infants, who required ventilation and the placement of an arterial catheter for clinical care, were entered into the study. Infants who were malnourished in utero (birth weight or ponderal index <10th percentile for gestation) or with proven congenital sepsis were excluded, as these conditions may potentially alter normal fatty acid metabolism. Informed parental consent was obtained for all infants, and the experimental protocol was approved by the Flinders Medical Centre Committee on Clinical Investigation.
A blood sample for baseline fatty acid analysis was taken from each infant's arterial catheter within 30 min of insertion. The arterial catheter was kept patent with normal saline 0.5 mL/h (1 U of heparin/mL) throughout the study. All baseline samples were taken within 12 h of delivery. Cord blood was not utilized as a baseline because obtaining a cord sample was found to be impractical under conditions of urgent delivery.
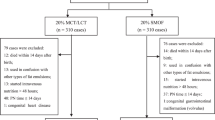
A 10% dextrose infusion was commenced at birth in all infants, and parenteral feeding begun within 36 h of life, as per a neonatal unit protocol which provides approximately 1 g/kg/d protein and 55 kcal/kg/d energy in week 1(4). An Intralipid 20% infusion was commenced on d 2-5 at 0.5 g/kg/d. Fat-soluble vitamins were admixed with the Intralipid. The rate of Intralipid infusion was increased on subsequent days, as ordered by the attending clinician and based on lipid tolerance and the severity of accompanying conditions such as lung disease and jaundice. On each day, the lipid was infused over 20 h with a break between 0400 and 0800 h daily. All infants tolerated the lipid infusion, as defined by the maintenance of a plasma triglyceride level of <105 mg/dL (1.2 mmol/L) at a point 4 h after stopping the infusion. The fatty acid composition of Intralipid is shown in Table 1.
A study of plasma lipid clearance was performed before any elective blood transfusions were required and before the commencement of milk feeding, thus avoiding an alteration of the infants' red cell or plasma fatty acid status by the infusion of adult red cells or ingestion of milk. When either of these interventions was considered imminent, Intralipid was ceased and a series of five 400-μL blood samples for fatty acid analyses were withdrawn from the arterial catheter over a period of 36 h of fat-free parenteral nutrition. The time points for sampling were: T = 0 (just before stopping the infusion at 0400 h), 4, 12, 24, and 36 h.
The lipid clearance study was performed after the maximum duration of lipid treatment when, due to a clinical decision, the infant was designated to receive either a blood transfusion or some enteral feed. This allowed an opportunity to study the change in plasma and red cells of infants receiving total parenteral nutrition. In addition this design allowed as far as possible for plasma phospholipid levels to establish an equilibrium. No attempt was made to influence clinical care, and hence the duration and dose of lipid were variable.
Fatty acid analysis. Plasma and red cell fractions were separated by centrifugation, and the plasma was frozen at -80°C for latter analysis. The lipids from washed red cells were extracted immediately using propanol and chloroform(5). Lipid extraction from plasma samples followed the method of Bligh and Dyer(6), with the addition to the plasma of diheptodecanoyl glycero-3-phosphocholine and triheptadecanoic acid as phospholipid and triglyceride internal standards, respectively. Red cell and plasma phospholipids were separated by thin layer chromatography and transesterified with sulfuric acid and methanol, and the fatty acid methylesters were analyzed using gas chromatography(7).
Fatty acid methodology was validated before the study of infants by repeating 10 analyses of a single sample of adult blood. For red cells, the coefficient of variance ranged from 0.5 to 1.5% (mean 1.0%) for fatty acids composing >10% of total phospholipid fatty acids, and 0.5-7.0% (mean 2.5%) for fatty acids composing from 1 to 10% of the total. For plasma triglyceride and phospholipid fatty acid concentrations of ≥2.0 μg/mL, coefficients of variance ranged from 4.5 to 12.5% (mean 7.0%), and 2.0 to 6.5% (mean 3.3%), respectively.
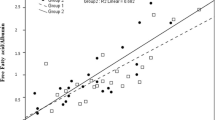
Red cell phospholipid fatty acids were reported as percentages of total membrane fatty acid to reflect composition of the membrane. Plasma phospholipid and triglyceride fatty acids were expressed as micrograms/mL of plasma, because it was considered that lipid infusion would render the measurement of percentages of total fatty acid insensitive to change in quantitatively minor fatty acids such as DHA (22:6n-3) due to a large denominator. Furthermore, percentages may be difficult to interpret due to shifts in the denominator as a result of lipid clearance.
Statistics. Change over time within the clearance study was determined by repeated measures ANOVA, with post hoc analysis using the least significant difference multiple comparison test. In one patient, data were missing at a single time point (T = 12 h) due to a failure to obtain the blood sample. This was managed by substituting a value derived by averaging the data values for the same patient on either side of the missing value. Formal statistical comparisons were not made between baseline plasma triglyceride and phospholipid fatty acids, red blood cell phospholipid fatty acids, and those obtained at the time of the clearance study, because the lipid regimen of each infant was not standardized and there was consequently a wide interpatient variation in dose and duration of lipid infusion. The baseline data were therefore utilized for reference only.
RESULTS
The characteristics of the infants receiving parenteral nutrition with Intralipid are shown in Table 2. All infants were delivered by cesarean section and were ventilated for either hyaline membrane disease(8) or transient tachypnea(1). All infants received >50 kcal/kg/d, which is greater than the energy expenditure of a ventilated infant receiving parenteral nutrition(8).
Three infants were infused with 10 mL/kg fresh frozen plasma within the first 3 d of life, which in all cases was given after the baseline blood sample and more than 2 d before the clearance study. One patient received 10 mL/kg packed red cells and volume-reduced platelets between the 12- and 24-h time points in the clearance study. This infant was still included because the blood transfusion would have no influence on red cell samples taken at birth or during the early part of the clearance study (T = 0-, 4-, or 12-h samples) and the pooled red cell composition at points T = 24 and 36 did not change after the transfusion (consistent with observations in the other infants).
Plasma triglyceride fatty acid levels showed a rapid and uniform decline from peak levels at T = 0 (Table 3). This pattern of decline was not restricted to the primary soybean triglyceride fatty acids of the emulsion, but was also noted in long chain polyunsaturated fatty acids. The bulk of clearance for all triglyceride fatty acids occurred within 4 h of stopping lipid.
Plasma phospholipid fatty acids also declined from peak values at T = 0 (during the infusion) after Intralipid was stopped, although the extent of decline was more variable than observed in triglycerides(Table 4). DHA showed a rapid decline over 12 h and was stable in plasma phospholipids beyond this point. AA (20:4n-6) levels, however, showed minimal change over the entire clearance period. Phospholipid LA (18:2n-6) was conspicuous in demonstrating a very slow decline which was ongoing beyond 36 h of fat-free parenteral nutrition. In comparison with reference values, the extent of change induced in plasma phospholipids by Intralipid infusion was less than that observed in triglycerides.
Red cell phospholipid fatty acids remained stable over the period of plasma lipid clearance (Table 5). LA showed a statistically significant reduction toward the end of the clearance period which was small in practical terms.
DISCUSSION
The metabolism of the triglyceride and phospholipid components of i.v. fat emulsions has been extensively reviewed(1–3). However, it has hitherto been unreported how individual fatty acids of triglycerides and phospholipids infused with the emulsion are cleared from plasma lipid fractions. Furthermore, it has been uncertain whether red cells are a stable reflection of fatty acid status during the i.v. infusion of fat.
The principal finding of this study is the stability of red cell phospholipid fatty acid composition during plasma lipid clearance. This finding indicates that red cells provide a stable parameter of fatty acid status during Intralipid infusion, and that reliable analysis can be performed at any time within a period of 36 h after stopping lipid infusion. It also shows that standard methods of preparation of red cells and extraction of lipid are not confounded by emulsion phospholipid particles or FFA closely associated with the red cell membrane.
Conversely, the results indicate a complex interaction between infused and endogenously generated triglyceride and phospholipid fatty acids. This creates an impediment to interpretation of plasma fatty acid data during parenteral nutrition.
During the i.v. infusion of fat, measured plasma triglyceride and phospholipid fatty acid values represent the net effect of the combined fatty acid composition of endogenous and infused triglyceride and phospholipid species. Endogenous triglyceride and phospholipid composition reflects the metabolic consequences of lipid infusion and should therefore have an interpretable association with tissue composition. In addition, the synthesis of endogenous triglyceride and phospholipid has a definable relationship to the triglyceride fraction of the emulsion, which constitutes the bulk of infused fat. The emulsion triglyceride determines which fatty acids are immediately available for incorporation into endogenous lipids in the liver, and also the synthesis by tissues of long chain polyunsaturated fatty acids through provision of precursor fatty acids.
In contrast, infused triglyceride and phospholipid moieties exist in a state that is unmodified by tissue metabolism. It is likely therefore that such infused material is irrelevant to the assessment of tissue fatty acid composition. By contributing to measured (net) plasma values, infused triglyceride and phospholipid will confuse the assessment of the composition of endogenous lipid fractions. Therefore, the measurement of plasma fatty acids is of value only if the endogenous lipid fractions are separable from infused lipids. In this study an attempt was made to achieve this separation by allowing a period of time for infused lipid to clear.
Infused triglyceride dominated measured triglyceride fatty acids during lipid infusion. The elevated levels of AA and DHA in plasma triglycerides indicate incorporation of endogenously synthesized AA and DHA into VLDL triglyceride in the liver, as AA and DHA are absent from soybean triglyceride. However, the small quantities are difficult to interpret within the error of the method. Although stable composition of triglyceride was obtained 12-24 h after stopping Intralipid, a modulating effect of fat-free nutrition on composition cannot be excluded. This effect is suggested by the trend to a late increase in synthesis of monounsaturates.
The large increase in plasma phospholipid LA and ALA (18:3n-3) in comparison with reference values and to other plasma phospholipid fatty acids during lipid infusion is likely to predominantly reflect an increase in endogenous phospholipid LA and ALA, rather than accumulation of egg yolk phospholipid. This is supported by the abundance of infused LA and ALA(reflected in the plasma triglycerides), by the low concentration of these fatty acids in emulsion phospholipid, and by the disproportionate increase in these fatty acids in comparison with others more heavily represented in egg yolk phospholipid.
In the case of DHA however, infused egg yolk phospholipid appeared to have a considerable influence on plasma phospholipid fatty acid levels taken during lipid infusion. This is supported by the rapid reduction in levels after stopping Intralipid, which suggests clearance of infused phospholipid. A similar trend that did not reach statistical significance was noted with AA, although the extent of change was of little practical significance in view of the large basal AA levels.
Although this result may suggest that endogenous phospholipid long chain polyunsaturated fatty acid levels are more reliably assayed after a 12-h lipid-free interval, the data need to be interpreted with caution. This is because endogenous phospholipid composition can be only indirectly inferred, and also because phospholipids are quickly modified as a consequence of fat-free nutrition. This latter assertion is supported by the data for LA, which show a slow decline in plasma phospholipids after stopping the lipid infusion that extends beyond 36 h. This finding is most likely the result of an ongoing modification of endogenous phospholipid from the abnormally high levels sustained by Intralipid infusion.
In summary, the results of this characterization study support the importance of red cell phospholipid fatty acids in the assessment of fatty acid status during parenteral lipid infusion. Red cell phospholipid fatty acids represent a stable and interpretable measure of the end point of changes in plasma fatty acids. Plasma fatty acid measurements are confounded by the use of i.v. fat emulsions, and interpretation of levels during and after lipid infusion is difficult.
Abbreviations
- AA:
-
arachidonic acid
- ALA:
-
linolenic acid
- DHA:
-
docosahexaenoic acid
- LA:
-
linoleic acid
References
Stahl GE, Spear ML, Hamosh M 1986 Intravenous administration of lipid emulsions to premature infants. Clin Perinatol 13: 133–162.
Carpentier YA 1989 Intravascular metabolism of fat emulsions. Clin Nutr 8: 115–125.
Bach AC, Férezou J, Frey A 1996 Phospholipid-rich particles in commercial parenteral fat emulsions, an overview. Prog Lipid Res 35: 133–153.
Simmer K, Metcalf R, Daniels L 1997 The use of breastmilk in a neonatal unit and its relationship to protein and energy intake and growth. J Paediatr Child Health 33: 55–60.
Broekhuyse RM 1974 Improved lipid extraction of erythrocytes. Clin Chim Acta 51: 341–343.
Bligh EG, Dyer WJ 1959 A rapid method of total lipid extraction and purification. Can J Biochem Physiol 37: 911–917.
Makrides M, Neumann MA, Byard RW, Simmer K, Gibson RA 1994 Fatty acid composition of brain, retina, and erythrocytes in breast- and formula-fed infants. Am J Clin Nutr 60: 189–194.
Forsyth JS, Crighton A 1995 Low birthweight infants and total parenteral nutrition immediately after birth. I Energy expenditure and respiratory quotient of ventilated and non-ventilated infants. Arch Dis Child 73:F4–F7.
Acknowledgements
The authors acknowledge and thank Dr. Peter Marshall, Dr. Simon James, and Mark Neumann for advice and support.
Author information
Authors and Affiliations
Additional information
Supported jointly from a Flinders 2000 Clinician's Trust Fund Scholarship, a National Health and Medical Research Council Medical Postgraduate Scholarship, and Scotia Pharmaceuticals (UK).
Rights and permissions
About this article
Cite this article
Morris, S., Simmer, K. & Gibson, R. Characterization of Fatty Acid Clearance in Premature Neonates during Intralipid Infusion. Pediatr Res 43, 245–249 (1998). https://doi.org/10.1203/00006450-199802000-00015
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199802000-00015
This article is cited by
-
Lipid emulsion enhances cardiac performance after ischemia–reperfusion in isolated hearts from summer-active arctic ground squirrels
Journal of Comparative Physiology B (2017)
-
Lipid-mediated muscle insulin resistance: different fat, different pathways?
Journal of Molecular Medicine (2015)
-
Utilization of docosahexaenoic acid from intravenous egg yolk phospholipid
Lipids (2000)