Abstract
The purpose of this study was to evaluate pediatric patients with systemic lupus erythematosus (SLE) to determine 1) the incidence of thrombosis, 2) the incidence of antiphospholipid antibodies, and 3) whether there is an association between the presence of antiphospholipid antibodies and thrombosis. We performed a cross-sectional cohort study in 59 consecutive SLE patients who had been managed at rheumatology clinics in two pediatric hospitals. A history, questionnaire, and chart review were completed by the study nurse blinded to laboratory results. Only the thrombotic events that could be substantiated by review of radiographic tests were accepted. The presence of antiphospholipid antibodies was determined by prospective analysis for a lupus anticoagulant and anticardiolipin antibodies on two separate occasions at least 3 mo apart. Patients were considered to be positive if one or more tests were positive on both occasions. Thirteen thrombotic events occurred in 10 of the 59 patients(17%). Fourteen patients (24%) were classified as positive for lupus anticoagulant, and 19 patients (27%) were classified as positive for anticardiolipin antibodies. A significant relationship between the presence of a lupus anticoagulant and a thrombotic event was shown: odds ratio 28.7(95% confidence interval 4.03-138.2, p < 0.001). A nonsignificant trend was seen for the presence of an anticardiolipin antibody and a thrombotic event: odds ratio 2.12 (95% confidence interval 0.71-22.8,p = 0.08). We conclude that in pediatric patients with SLE:1) a significant proportion of patients have thrombotic events,2) a significant proportion of patients have antiphospholipid antibodies, and 3) there is a significant relationship between the presence of a lupus anticoagulant and thrombotic events.
Similar content being viewed by others
Main
SLE is an inflammatory disease of unknown etiology which is characterized by damage to tissues and cells resulting from deposition of pathogenic autoantibodies and immune complexes. The clinical manifestations of the disease are varied and determined by the antibodies present. A significant percentage of adult patients with SLE have antiphospholipid antibodies(1–6). Antiphospholipid antibodies are a heterogenous group of antibodies, a majority of which react with proteins bound to phospholipids(7). There are two major categories of antiphospholipid antibodies, lupus anticoagulants and anticardiolipin antibodies. Antiphospholipid antibodies recognize phospholipid-bound plasma proteins such as human prothrombin andβ2-glycoprotein 1(8–10). Recent studies show that adults with SLE who are persistently positive for antiphospholipid antibodies have an increased incidence of thrombotic events and spontaneous abortions(1–6,11–16).
In contrast to the adult literature, there is only anecdotal evidence in the pediatric literature (nine case reports and one retrospective analysis), that link antiphospholipid antibodies to thrombotic events in children with SLE(3,17–24). The objective our study was to determine in patients with SLE: 1) the incidence of thrombotic events;2) the incidence of antiphospholipid antibodies; and 3) and whether the presence of antibodies is associated with thrombotic events.
METHODS
Study design. The design was a cross-sectional cohort study of consecutive unselected pediatric patients managed through SLE clinics at two Canadian tertiary care centers, Hospital for Sick Children, Toronto, Canada, and Hôpital Ste. Justine, Quebec, Canada. Tests for the presence of antiphospholipid antibodies were assessed prospectively at two time points 1) study entry and 2) repeated again a minimum of 3 mo later. The occurrence of a thromboembolic event was determined both retrospectively and prospectively by an independent, blinded review of confirmatory radiographic tests. The study was approved by both hospitals' institutional review boards. Informed consent was obtained from guardians and patients when appropriate.
Study population. The study population consisted of 59 pediatric patients (ages 4-19 y) with SLE who were treated in SLE rheumatology clinics at the two centers. There was no referral bias in the study population as 1) patients had been referred to the centers for suspected SLE by either primary care physicians or subspecialists who would be unaware of the study, and 2) pediatric patients with SLE in Canada are managed in specialized SLE clinics located in the closest pediatric hospital. There were no exclusions, and consent was obtained for all eligible patients. All patients fulfilled the 1982 revised American Rheumatism Association criteria for SLE and were studied between June 1991 and June 1994(25). A disease activity index was determined at each visit, using a validated scoring system(26).
Plasma from an age-matched healthy control population was required to determine age appropriate normal ranges for the laboratory tests used to detect antiphospholipid antibodies. Thirty-eight healthy children who were having minor elective surgery formed the control population. Informed consent was obtained from the patient and/or guardians, and an additional 5-mL blood sample was drawn by venipuncture from these children with preoperative blood work. Control subjects were not matched based on gender as previous studies in children have shown that there is no difference between male and female subjects in levels of coagulation proteins(27).
Intervention. All eligible patients and/or parents were interviewed, and blood was drawn for laboratory testing at study entry and again on a separate occasion during a follow-up visit at least 3 mo after the initial visit. Patients who developed acute thrombotic events during the study period had blood drawn at the time of the event and at a later visit at least 3 mo from the acute event.
Evaluation for Prior Thromboembolic Disease. Patient interview. All eligible patients and/or parents were interviewed by the nurse study coordinator blinded to the laboratory results, a detailed history of previous thrombotic events obtained, and a standardized questionnaire completed. Specific information was collected on concurrent medications, use of warfarin and/or oral contraceptives. Questionnaires were updated, and a second SLE activity index was determined at the second visit. A chart review was also performed, and if a thrombotic event was noted, the radiographic test used to diagnose the event was reviewed by an independent panel of experts. Accepted radiographic tests included venography or ultrasound for deep venous thrombosis in a limb, a ventillation perfusion scan for pulmonary embolism, and either a computerized tomography scan or magnetic resonance imaging for thrombotic events in the CNS. Patients were classified as having a thrombotic event if the independent review of the radiographic test confirmed the original diagnosis.
Laboratory methods. Venous blood was drawn into a vacutainer tube (Becton Dickinson) containing 1.05 mM buffered citrate solution for a final ratio of one part anticoagulant to nine parts of blood. Plasma was immediately separated from cellular elements by double centrifugation at 1500× g for 15 min at 4°C. In addition, samples to be tested for lupus anticoagulant assays were filtered through a sterile 0.020-µm screen (Acrodisk, Gelman Sciences, Ann Arbor, MI) to achieve complete platelet removal. Plasma was subsequently aliquotted and frozen at -70°C. Normal pooled plasma used in the 1:1 mix in lupus anticoagulant assays was obtained under the same conditions from 14 healthy adult donors, pooled, and frozen at -70°C providing a single lot of plasma. The pooled plasma contained fewer than 109 platelets/L.
Assays to detect a lupus anticoagulant included: a kaolin clotting time performed on the Diagnostica Stago ST4 (France) using a 2% solution of kaolin in veronal buffer and 0.025 M calcium chloride(28). An APTT was done on patient plasma on an Automated Coagulation Laboratory(Milan, Italy) using a commercially available sensitive reagent (Actin FSL, Dade International, Miami, FL)(29). A dilute prothrombin time using a 1/400 dilution of rabbit brain phospholipid(Thromboplastin C, Dade) in a saline/CaCl2 mixture was conducted on an Automated Coagulation Laboratory(30). All patient plasma was mixed 1:1 with normal pooled plasma and the above assays were repeated. A nonspecific inhibitor was suspected if the patient result did not correct into the normal range. The dRVVT was assayed by two methods:1) a commercial kit (DRVT; American Diagnostica Inc., Greenwich, CT) and 2) using the Behring ST4 clotting machine with Russell viper venom, ionophore-treated platelets, and bovine phospholipid(31). Both dRVVT assays were initially performed with phospholipid sensitive to the lupus anticoagulant and then repeated with phospholipid insensitive to the lupus anticoagulant. This was to confirm the presence of a lupus anticoagulant. Results that were 2 SD above the mean of age-matched controls were considered abnormal.
Detection and quantitation of IgG and IgM anticardiolipin antibodies were performed by ELISA (Advanced Biological Products Inc., Mississauga, Ontario, Canada) calibrated against Harris standards from the University of Louisville, Kentucky. Patient results were considered abnormal if values were 3 SD above the mean of the age-matched controls.
All assays were performed in one central laboratory at the Hamilton Civic Hospitals Research Centre by the same technologist blinded to the patients' clinical status. Lot numbers of all reagents were constant during the study.
Classification of patients according to the presence or absence of antiphospholipid antibodies. Patients were classified as persistently positive for an antiphospholipid antibody if one or more tests were positive on both occasions; transiently positive if one or more tests were positive on one occasion only; and negative if all tests were negative on both occasions, analogous to previous adult studies(32–34).
Statistics. Data were organized into contingency tables according to patients thrombotic event status and results of tests for antiphospholipid antibodies. Odds ratios were considered statistically significant when the lower limit of the 95% confidence interval was greater than 1.0. A Fisher exact test was calculated, and a p < 0.05 was considered statistically significant.
RESULTS
Study population. Fifty-nine patients with SLE (49 female, 10 male) were studied. The ages ranged from 4 to 19 y, with a median of 14 y.Table 1 describes the demographic characteristics of the patients and the healthy normal controls. All but two patients with SLE were receiving corticosteroids during the study period. Oral contraceptives were taken by two patients who did not have a thrombotic event. The disease activity score was similar in patients with thrombotic events compared with all other patients (data not shown). There was no difference in the platelet counts or levels of antithrombin, heparin cofactor II,α2-macroglobulin, protein C, and protein S (total and free) in patients with thrombotic events compared with patients without such events(data not shown). Eight patients had significantly prolonged diluted APTT values due to the presence of a lupus anticoagulant.
Thrombotic events. Thirteen thrombotic events occurred in 10 of the 59 (17%) patients with SLE. The median age of patients with thrombotic events was similar to that of the entire SLE population (14.5versus 14 y). Four events were deep venous thrombosis in the lower extremities, two were pulmonary emboli, one was a portal vein thrombosis, and six involved the CNS of which three were venous (sagittal sinus thrombosis) and three ischemic infarction. All deep venous thromboses were proximal in location and caused significant swelling and pain. In both cases of pulmonary embolism, pleuritic chest pain was the clinical presentation and ventillation perfusion scans showed high probability. Thrombotic complications in the CNS caused a variety of neurologic symptoms dependent on thrombus location. There were no deaths. All thrombotic events were managed with heparin followed by warfarin for at least 3 mo. Six patients had a thrombotic event before study entry and three of these patients had recurrent events during the study period when they were not receiving warfarin (Table 2). All other thrombotic events developed during the study period.
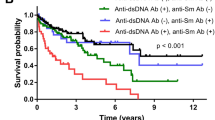
Antiphospholipid antibodies in pediatric patients with SLE. Twenty-four of 59 pediatric patients with SLE (41%) were classified as persistently or transiently positive for a lupus anticoagulant, 10 of these patients (17%) were transiently positive and 14 (24%) were persistently positive. All 10 patients with a thrombotic event were positive for a lupus anticoagulant, 8 of the 10 pediatric patients were persistently positive for a lupus anticoagulant. The lupus anticoagulant remained positive in an additional third testing of all 10 patients with a thrombotic event. Of the 49 pediatric patients with SLE who did not have a thrombotic event, six were persistently positive for a lupus anticoagulant (12%) and eight were transiently positive for a lupus anticoagulant (16%). The relationship between thrombotic events and persistent presence of a lupus anticoagulant was highly statistically significant (p < 0.001), odds ratio of 28.7 (95% confidence interval: 4.03-138.2) (Table 3). The relationship between thrombotic events and transiently positive for the presence of a lupus anticoagulant was also highly significant (p< 0.001), odds ratio of 141 (95% confidence interval: 11.4-infinite) (data not shown). The relationship between the individual lupus anticoagulant assays and thrombotic events is shown in Table 4. The dilute prothrombin time was the most sensitive test, detecting 8 of the 10 patients with thrombotic events, followed by the diluted APTT which detected 4 of the 10 patients. There was no difference between the sensitivities of the two dRVVT assays.
Thirty of the 59 pediatric patients with SLE (51%) were classified as persistently or transiently positive for an anticardiolipin antibody, 11 of these patients (19%) were persistently positive, and 19 (27%) were transiently positive. Seven patients with a thrombotic event were positive for an anticardiolipin antibody, four were persistently positive and three were transiently positive. There was a nonsignificant trend between the presence of a thrombotic event and the persistent presence of an anticardiolipin antibody (p = 0.08), odds ratio of 2.12 (95% confidence interval: 0.71-22.8). There was a trend to higher mean plasma levels of IgG and IgM anticardiolipin antibodies in patients with thrombosis compared with those patients without thrombosis, but this was not statistically significant (data not shown). The persistent presence of both a lupus anticoagulant and anticardiolipin antibody did not strengthen the relationship between patients with thrombotic events and a lupus anticoagulant(odds ratio 7.5, 95% confidence interval 1.16-52.1,p = 0.022).
DISCUSSION
SLE is a disease that primarily affects young women, with 20% of patients presenting before 18 y of age. The incidence of thrombotic events, the incidence of antiphospholipid antibodies, and whether an association exists between thrombosis and the presence of antiphospholipid antibodies are unknown in pediatric patients with SLE. The ability to predict pediatric patients who are at risk for thrombotic events is critically important to the development of strategies focused on prevention. In our cross-sectional cohort study of 59 pediatric patients with SLE, 10 patients had either a venous or arterial thrombosis for an overall incidence of 17%. The latter may be an underestimation because thrombotic events were, in part, identified by retrospective review of the hospital charts. Twenty-four percent of patients(14/59) were persistently positive for lupus anticoagulant. Fifty-seven percent (8/14) of patients with SLE who were persistently positive for a lupus anticoagulant had one or more thrombotic events compared with only 4%(2/45) of patients who were negative for a lupus anticoagulant. We found that pediatric patients with SLE who were persistently positive for a lupus anticoagulant had a 28-fold increased risk of thrombotic events compared with patients who were negative for a lupus anticoagulant. Of probable significance is the conversion of two patients who were transiently positive for a lupus anticoagulant to a persistently positive status after a thrombotic event. Nineteen percent of patients were persistently positive for anticardiolipin antibodies. Although there was a trend, there was no statistically significant association between the persistent presence of anticardiolipin antibodies and thrombotic events.
The design of our study, choice of tests, and frequency of testing were modeled on adult studies that form the basis of international recommendations(35). Current recommendations for the detection of lupus anticoagulants in adults are that a minimum of three sensitive assays be used as there is no single test that will identify all lupus anticoagulants(35). We prospectively tested five different assays for lupus anticoagulants as the sensitivities of tests for detecting a lupus anticoagulant in pediatric patients was unknown. We also established age-matched reference ranges for each assay using plasmas from healthy children. International recommendations for determining that an assay for a lupus anticoagulant is positive are the following: there is no evidence of another coagulopathy, at least one phospholipid-dependent clotting test is prolonged, evidence of inhibitory activity is demonstrated when the test sample is mixed (1:1) with normal pooled plasma, and the inhibitory activity depends on the concentration of phospholipid in the assay. These recommendations were followed in our study. In addition, we tested our patients on two separate occasions, at least 3 mo apart, because similar repeated testing in adults with SLE showed a more significant relationship with thrombotic events compared with testing on a single occasion(4,34).
Our study identified some similarities and differences in the relationship between the persistent presence of antiphospholipid antibodies with thrombotic events in pediatric patients with SLE compared with adults with SLE. First, adults with SLE who are negative for antiphospholipid antibodies are at considerable risk for thrombotic events (41% of patients)(4). In our study pediatric patients with SLE who were negative for antiphospholipid antibodies rarely developed thrombotic events(2/45 or 4% of patients). The latter likely reflects additional risk factors for thrombosis in adults, such as duration of disease. Second, although there are several reports showing an association of thrombotic events in adults with SLE and presence of antiphospholipid antibodies, the reports conflict on the type of antibody that is associated with these events(1–5,11–16). The largest most comprehensive study to date evaluated 175 patients on the relationship between the presence of lupus anticoagulants, anticardiolipin antibodies, prothrombin antibodies,β2-glycoprotein 1 antibodies, and thrombosis. This study demonstrated that the presence of lupus anticoagulant is the strongest risk factor for thrombotic events, which agrees with the findings in our current study(1).
A review of the literature pertaining to the relationship of antiphospholipid antibodies and thrombotic events in pediatric patients identified several case reports(3,17–24) and one retrospective study from France(20). Many of the results from our study are consistent with these previous reports. First, thrombotic events in pediatric patients with SLE are both venous and arterial in location and can occur in the CNS. Second, thrombotic events occur early and often at the time of the diagnosis of SLE. Third, lupus anticoagulants are present in the vast majority of pediatric patients with SLE who have thrombotic events. Our study extends the results of previous studies in several ways. First, the presence of a lupus anticoagulant was shown to have a significantly stronger association with thrombotic events in pediatric patients with SLE compared with the presence of an anticardiolipin antibody. Second, more than one assay must be used in pediatric patients with SLE to identify all patients with a lupus anticoagulant. Third, the dilute prothrombin time was the most sensitive test to detect a lupus anticoagulant in pediatric patients with SLE who develop thrombotic events. Fourth, there was a relatively low incidence of thrombotic events in pediatric patients with SLE who did not have a lupus anticoagulant.
The incidence of anticardiolipin antibodies in our study (30/59 patients or 51%) is consistent with the incidences reported in two studies of pediatric patients with SLE, 26/30 patients or 87%, and 16/32 patients or 50%(36,37). The possible importance of persistently positive tests for anticardiolipin antibodies was not assessed in these two studies. Neither study examined the relationship of the presence of anticardiolipin antibodies and thrombotic events as a primary objective. However, one study followed 20 pediatric patients who were positive for a anticardiolipin antibody for a median of 51 mo. They reported a thromboembolic complication in one patient who also had a lupus anticoagulant(36).
In conclusion, a significant proportion of pediatric patients with SLE and a lupus anticoagulant are at risk for thrombotic events compared with pediatric patients with SLE who do not have a lupus anticoagulant. Pediatric patients with SLE should be routinely screened for lupus anticoagulants and, if antibodies are present on more than one occasion, they should be counseled on the presenting symptoms of thrombotic events. Intervention trials are required to determine whether anticoagulants can prevent initial and recurrent thrombotic events in pediatric patients with SLE and a lupus anticoagulant.
Acknowledgment. The authors thank Lu Ann Brooker for her contributions to the preparation of this manuscript.
Abbreviations
- SLE:
-
systemic lupus erythematosus
- APTT:
-
activated partial thromboplastin time
- dRVVT:
-
dilute Russell's viper venom time
References
Horbach DA, van Oort E, Donders RC, Derksen RH, de Groot PG 1996 Lupus anticoagulant is the strongest risk factor for both venous and arterial thrombosis in patients with systemic lupus erythematosus. Comparison between different assays for the detection of antiphospholipid antibodies. Thromb Haemost 76: 916–924.
Puurunen M, Vaarala O, Julkunen H, Aho K, Palosuo T 1996 Antibodies to phospholipid-binding plasma proteins and occurrence of thrombosis in patients with systemic lupus erythematosus. Clin Immunol Immunopathol 80: 16–22.
Alarcon-Segovia D, Deleze M, Oria CV, Sanchez-Guerrero J, Gomez-Pacheco L, Cabiedes J, Fernandez L, Ponce De Leon S 1989 Antiphospholipid antibodies and the antiphospholipid syndrome in systemic lupus erythematosus: a prospective analysis of 500 consecutive patients. Medicine 68: 353–365.
Long AA, Ginsberg JS, Brill-Edwards P, Johnston M, Turner C, Denburg JA, Bensen WG, Cividino A, Andrew M, Hirsh J 1991 The relationship of antiphospholipid antibodies to thromboembolic disease in systemic lupus erythematosus: a cross-sectional study. Thromb Haemost 66: 520–524.
Love PE, Santoro SA 1990 Antiphospholipid antibodies: anticardiolipin and the lupus anticoagulant in systemic lupus erythematosus(SLE) and in non-SLE disorders. Ann Intern Med 112: 682–698.
Harris E, Boey M, Mackworth-Young C, Gharavi AE, Patel BM, Loizou S, Hughes GRV 1983 Anticardiolipin antibodies: detection by radioimmunoassay and association with thrombosis in systemic lupus erythematosus. Lancet 2: 1211–1214.
Roubey RAS 1994 Autoantibodies to phospholipid-binding plasma proteins: a new view of lupus anticoagulants and other‘antiphospholipid’ autoantibodies. Blood 84: 2854–2867.
Bevers EM, Galli M, Barbui T, Comfurius P, Zwaal RFA 1991 Lupus anticoagulant IgG's (LA) are not directed to phospholipids only, but to a complex of lipid-bound human prothrombin. Thromb Haemost 66: 629–632.
McNeil HP, Simpson RJ, Chesterman CN, Krilis SA 1990 Anti-phospholipid antibodies are directed against a complex antigen that includes a lipid-binding inhibitor of coagulation: β2-glycoprotein I (apolipoprotein H). Proc Natl Acad Sci USA 87: 4120–4124.
Bevers EM, Galli M 1990 Beta 2-glycoprotein I for binding of anticardiolipin antibodies to cardiolipin. Lancet 336: 952–953.
St Clair W, Jones B, Rogers JS, Crouch M, Hrabovsky E 1981 Deep venous thrombosis and a circulating anticoagulant in systemic lupus erythematosus. Am J Dis Child 135: 230–232.
Khamashta MA, Hughes GR 1994 Antiphospholipid antibodies. A marker for thrombosis and recurrent abortion. Clin Rev Allergy 12: 287–296.
Asherson RA, Hughes GR 1992 Vascular disease and thrombosis: relationship to the antiphospholipid antibodies. Contrib Nephrol 99: 17–25.
Ishii Y, Nagasawa K, Mayumi T, Niho Y 1990 Clinical importance of persistence of anticardiolipin antibodies in systemic lupus erythematosus. Ann Rheum Dis 49: 387–390.
Feinstein D 1985 Lupus anticoagulant, thrombosis and fetal loss. N Engl J Med 313: 1348–1350.
Harris E, Chan J, Asherson R, Aber V, Gharavi AE, Hughes GRV 1986 Thrombosis, recurrent fetal loss and thrombocytopenia. Predictive value of the anticardiolipin antibody test. Arch Intern Med 146: 2153–2156.
Dungan DD, Jay MS 1992 Stroke in an early adolescent with systemic lupus erythematosus and coexistent antiphospholipid antibodies. Pediatrics 90: 96–99.
Pelkonen P, Simell O, Rasi V, Vaarala O 1988 Venous thrombosis associated with lupus anticoagulant and anticardiolipin antibodies. Acta Pediatr Scand 77: 767–772.
Appan S, Boey ML, Lim KW 1987 Multiple thrombosis in systemic lupus erythematosus. Arch Dis Child 62: 739–741.
Bersntein ML, Salunsinsky-Sternbach M, Bellefleur M, Esseltine DW 1984 Thrombotic and hemorrhagic complications in children with lupus anticoagulant. Am J Dis Child 138: 1132–1135.
Olive D, Brocard O, Labrude P, Alexandre P 1979 Lupus Erythemateux dissemine revele par des thrombophlebites des membres inferieurs. Arch Fr Pediatr 36: 807–811.
Ostuni PA, Lazzarin P, Pengo V, Ruffatti A, Schiavon F, Gambari P 1990 Renal artery thrombosis and hypertension in a 13 year old girl with antiphospholipid syndrome. Ann Rheum Dis 49: 184–187.
Kwong T, Leonidas JC, Ilowite NT 1994 Asymptomatic superior vena cava thrombosis and pulmonary embolism in an adolescent with SLE and antiphospholipid antibodies. Clin Exp Rheum 12: 215–217.
Rider LG, Clarke WR, Rutledge J 1992 Pulmonary hypertension in a seventeen-year-old boy. J Pediatr 120: 149–159.
Tan EM, Cohen AS, Fries JF, Masi AT, McShane DJ, Rothfield NF, Schaller JG, Talal N, Winchester RJ 1982 The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 25: 1271–1277.
Bombardier C, Gladman DD, Urowitz MB, Caron D, Chang CH 1992 Derivation of the SLEDAI. A disease activity index for lupus patients. The Committee on Prognosis Studies in SLE. Arthritis Rheum 35: 630–640.
Andrew MA, Vegh PA, Johnston M, Bowker J, Ofuso F, Mitchell L 1992 Maturation of the hemostatic system during childhood. Blood 80: 1998–2005.
Proctor R, Rapaport S 1961 The partial thromboplastin time with kaolin. Am J Clin Pathol 36: 212–219.
Alving BM, Baldwin PE, Richards RL, Jackson BJ 1985 The dilute phospholipid APTT: a sensitive assay for verification of lupus anticoagulants. Thromb Haemost 54: 709–714.
Schleider M, Nachman R, Jaffe E, Coleman M 1976 A clinical study of the lupus anticoagulant. Blood 48: 499–509.
Thiagarajan P, Pengo V, Shapiro S 1986 The use of dilute Russell Viper Venom time for the diagnosis of lupus anticoagulants. Blood 68: 869–874.
Ginsberg JS, Brill-Edwards P, Johnston M, Denburg JA, Andrew M, Burrows RF, Bensen W, Cividino A, Long AA 1992 Relationship of antiphospholipid antibodies to pregnancy loss in patients with systemic lupus erythematosus: a cross-sectional study. Blood 80: 975–980.
Ginsberg JS, Demers C, Brill-Edwards P, Johnston M, Bona R, Burrows RF, Weitz J, Denburg JA 1993 Increased thrombin generation and activity in patients with systemic lupus erythematosus and anticardiolipin antibodies: evidence for a prothrombotic state. Blood 81: 2958–2963.
Ginsberg JS, Wells PS, Brill-Edwards P, Donovan D, Moffat K, Johnston M, Stevens P, Hirsh J 1995 Antiphospholipid antibodies and venous thromboembolism. Blood 86: 3685–3691.
Brandt JT, Triplett DA, Alving B, Scharrer I 1995 Criteria for the diagnosis of lupus anticoagulants: an update. Thromb Haemost 74: 1185–1190.
Ravelli A, Caporali R, Di Fuccia G, Zonta L, Montecucco C, Martini A 1994 Anticardiolipin antibodies in pediatric systemic lupus erythematosus. Arch Pediatr Adolesc Med 148: 398–402.
Shergy W, Kredich D, Pisetsky D 1988 The relationship of anticardiolipin antibodies to disease manifestations in pediatric systemic lupus erythematosus. J Rheumatol 15: 1389–1394.
Author information
Authors and Affiliations
Additional information
Supported by a grant-in-aid from the Hospital for Sick Children, Toronto. M.A. is a Career Investigator of the Heart and Stroke Foundation of Canada. C.B. is a research fellow of the McLaughlin Foundation
Rights and permissions
About this article
Cite this article
Berube, C., Mitchell, L., Silverman, E. et al. The Relationship of Antiphospholipid Antibodies to Thromboembolic Events in Pediatric Patients with Systemic Lupus Erythematosus: A Cross-Sectional Study. Pediatr Res 44, 351–356 (1998). https://doi.org/10.1203/00006450-199809000-00014
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199809000-00014
This article is cited by
-
Pediatric APS: State of the Art
Current Rheumatology Reports (2020)
-
Antiphospholipid antibodies in children with systemic lupus erythematosus: a long-term clinical and laboratory follow-up status study from northwest India
Rheumatology International (2014)