Abstract
Previous studies have shown that the endogenous inflammatory mediator platelet-activating factor (PAF) plays an important role in the pathophysiology of neonatal necrotizing enterocolitis (NEC). This study was designed to investigate the role of the PAF-degrading enzyme acetylhydrolase(PAF-AH) in a neonatal rat model of NEC. To study the absorption, localization, and activity of human recombinant PAF-AH (rPAF-AH), newborn rats were treated with enteral rPAF-AH, and plasma and intestines were sampled at 8 and 24 h for determination of PAF-AH enzyme activity and rPAF-AH concentration using a specific enzyme-linked immunoassay. To study the effect of rPAF-AH on neonatal NEC, rats were treated with rPAF-AH via the enteral route every 3 h, and then subjected to formula feeding and asphyxia per an established neonatal rat protocol for NEC. Pretreatment with enteral rPAF-AH significantly reduced the incidence of NEC compared with controls (6/26 versus 19/26,p < 0.001). We found that enteral rPAF-AH administration resulted in significant intestinal PAF-AH activity but no circulating PAF-AH activity despite immunohistochemical localization of the administered rPAF-AH to the intestinal epithelial cells. These findings suggest that rPAF-AH is functional and stable in the gut of neonatal rats. We conclude that enteral administration of rPAF-AH remains locally active and reduces the incidence of NEC in our experimental animal model.
Similar content being viewed by others
Main
NEC is an overwhelming gastrointestinal disease of premature newborns that afflicts approximately 11% of the babies born weighing less than 1500 g(1). Despite extensive research into the pathogenesis of this disease, the etiology has remained elusive. A reasonable hypothesis suggests that many risk factors including prematurity, hypoxia and/or intestinal ischemia, feeding, and bacterial colonization stimulate the inflammatory cascade that in some circumstances results in neonatal NEC(2).
A large body of experimental evidence suggests that the potent phospholipid mediator PAF plays a critical role in the final common pathway of NEC. Exogenous PAF infused into the mesenteric circulation or i.v. into experimental rats results in gross and microscopic intestinal damage that is similar to NEC(3). Furthermore, endotoxin-induced intestinal injury, hypoxia-induced intestinal injury, and tumor necrosis factor-induced intestinal injury in adult rats can be prevented by pretreatment with PAF receptor antagonists(4–6). Finally, blood and stool samples from premature infants with NEC have significantly higher PAF concentrations when compared with age-matched controls(7,8).
PAF-AH is a PAF-specific enzyme that catalyzes the hydrolysis of PAF to a biologically inactive molecule lyso-PAF(9). Considerable evidence indicates that the altered regulation of PAF-AH may play a contributory role in neonatal NEC because 1) PAF-AH activity is decreased in human newborns(10), 2) PAF-AH activity is deficient in sick neonates with NEC(7), and3) breast milk has measurable PAF-AH activity (formula has none) and reduces the incidence of NEC(11, 12). Recently the plasma form of human rPAF-AH was sequenced and cloned, and the product was shown to have antiinflammatory activities(13). We have previously shown that newborn rats stressed with formula feeding and asphyxia develop clinical and pathologic findings similar to human newborns with neonatal NEC(14). The purpose of this study was to1) evaluate the pharmacology of rPAF-AH in newborn rats, and2) investigate the effect of rPAF-AH in this neonatal rat model of NEC.
METHODS
Animal protocol. Time-dated pregnant Sprague-Dawley rats(Harlan Sprague-Dawley, Indianapolis, IN) were anesthetized with CO2 and delivered via abdominal incision. Newborn animals were collected, dried, and maintained in a neonatal incubator for the duration of the experiment. NEC was induced using our previously published protocol(14). Briefly, animals were fed with newborn puppy formula reconstituted from powder (Esbiliac, Borden Inc.) every 3 h via an orogastric silastic feeding tube inserted and removed each feeding. Although this formula differs somewhat from rat breast milk in protein and carbohydrate composition, the caloric provision is similar and approximates 150 cal/100 mL. The feeding volume began at 0.1 mL/feed initially and advanced 0.05 mL/4 feedings up to a maximum of 0.4 mL/feed by the 4th d of the protocol. This feeding protocol differs from normally reared newborn rats who are almost continually suckled; however, this approach is impossible in an experimental setting. Weight gain for pups using our experimental protocol lags slightly behind normally reared pups, suggesting that less enteral volume is supplied by the artificial approach. All animals were challenged with asphyxial insults twice daily by breathing 100% nitrogen for 50 s in a closed plastic chamber and then exposure to cold (4°C) for 10 min. Bowel and bladder function was stimulated with gentle manipulation after every feeding to simulate maternal grooming behavior. For the NEC protocol, animals were maintained for 96 h or until they showed signs of distress. Morbid animals had abdominal distention, bloody stools, respiratory distress, cyanosis, and lethargy, and were killed by decapitation. At this time, the intestine was examined grossly for signs of necrosis and then formalin-fixed for later histologic analysis. Specimens were paraffin-embedded, sectioned with a microtome, stained with hematoxylin and eosin, and evaluated by two independent observers blinded to the study groups. Intestinal injury was scored as 1+ for epithelial cell lifting or separation, 2+ for sloughing of epithelial cells to the mid-villous level, 3+ for necrosis of entire villi, and 4+ for transmural necrosis. To assess the efficacy of rPAF-AH in this model, separate groups of rats were treated with the compound. After the pharmacokinetic study described below, animals were given 25 μL(80 U) enterally via the orogastric tube diluted into each feeding (every 3 h; initial formula volume was 75 μL for a total of 0.1 mL). The rPAF-AH preparation had 0.8 mg/mL protein and approximately 4000 U/mg PAF-AH activity. The material has <0.5 enzyme units/mg endotoxin/protein ratio. Control animals received appropriate volumes of rPAF-AH dilution buffer (25 μL of NaPO4, 20 mM, pH = 7.4, with 75 μL of formula, pH also 7.4) without the rPAF-AH and were studied simultaneously with the experimental group. This animal protocol was reviewed and approved by the Evanston Hospital Corporation Institutional Animal Care and Use Committee.
Pharmacokinetic study. Separate groups of animals were used to assess the dosing and absorption characteristics of rPAF-AH. Newborn rat pups were given enteral rPAF-AH (25 μL, a maximum volume that allowed significant formula supplementation) every 3 h, and blood and intestine collected after 8 and 24 h for assessment of plasma and intestinal PAF-AH activity and rPAF-AH immunoreactivity. PAF-AH activity was measured using a substrate incubation assay (described below) and a standard ELISA method using an anti-human rPAF-AH MAb (90 G11D) for each sample. For selected samples, immunohistochemical analysis was performed using two different MAb developed against human rPAF-AH (90 F2D and 90 G11D, ICOS Corporation). Immunohistochemistry was done with standard techniques using a 1:100 dilution of the antibody and overnight incubations.
PAF-AH enzymatic activity assay. PAF substrate (250 μM unlabeled PAF and 10 μCi of [3H]PAF) was dried in nitrogen, resuspended in substrate buffer (25 mM Tris, pH 7.5, and 10 mM CHAPS), and sonicated. Serial dilutions of samples containing PAF-AH were prepared in duplicate in enzyme dilution buffer (25 mM Tris, pH 7.5, 10 mM CHAPS, 0.5 M NaCl, 1 mM EDTA), placed into a 96-well microtiter plate (Costar) with enzyme dilution buffer and the PAF substrate working solution. The enzyme reaction was allowed to proceed for 15 min at 37°C, then stopped with activated charcoal. The microtiter plate was centrifuged, and the supernatant containing the [3H]acetate hydrolyzed from the PAF substrate was transferred onto another 96-well sample plate and counted on a liquid scintillation counter. Plasma samples were added directly into the reaction. Intestinal samples were homogenized (1 part intestine to 9 parts 0.25 M sucrose) and centrifuged at 600 × g. The supernatant was centrifuged again at 15 000× g for 15 min, the resulting supernatant centrifuged at 105 000 × g for 1 h, and the final supernatant (cytosol) frozen at-20°C for addition into the reaction.
Statistics. Differences between groups of death and NEC were analyzed using Fischer's exact test. Differences between PAF-AH activity were analyzed using a t test. A p value of <0.05 was considered significant.
RESULTS
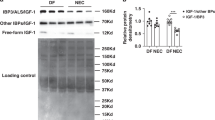
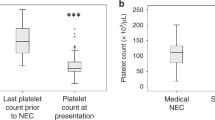
After enteral dosing of rPAF-AH in normal or stressed newborn rats, there was no measurable change in plasma PAF-AH activity using the enzyme activity assay, and no immunoreactive rPAF-AH in plasma by the ELISA technique. Intestinal PAF-AH activity increased dramatically after enteral rPAF-AH administration both at 8 and 24 h later (Table 1). Similarly, immunoreactive rPAF-AH was elevated at 8 and 24 h after enteral dosing, but absent in the control animals (as expected).
Immunohistochemical analysis revealed the presence of rPAF-AH in the epithelial cells of the intestinal mucosa after enteral administration(Fig. 1). The reactivity clustered mostly in the intestinal villi with minimal staining present in the crypt cells. There was more staining in the ileum than jejunum, and some rPAF-AH was immunochemically identified in portions of colon. There was no demonstrable rPAF-AH activity in any control samples, but trace positivity noted in the submucosal environment from animals dosed via the intraperitoneal route.
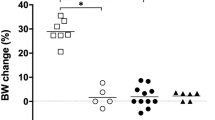
To test rPAF-AH for efficacy in the rat model, the enzyme was administered to neonatal rats with each feeding. Enteral rPAF-AH significantly reduced the incidence of NEC and death compared with control animals(Table 2). Results from four different enterally dosed experiments showed that pretreatment with rPAF-AH decreased the incidence of NEC from 19/26 (control) to 6/26 (p < 0.001). Intestinal injury was variable among treated and control animals, but in most cases was characterized by mid-villous necrosis in some segments, total villous necrosis in other areas, occasional areas of transmural necrosis, and remaining portions of normal intestinal histology (Fig. 2). The worst degree of degree of NEC in treated and controls with intestinal injury was similar (median score 2.8 control versus 2.4 rPAF-AH,p > 0.05). Necropsy findings in nonintestinal organs from animals dying with NEC were unremarkable in the majority of animals. Four of the controls and one pup from the rPAF-AH treatment group revealed inflammatory changes in pulmonary parenchyma; in these animals except for the intestinal necrosis, the remaining histology was normal. Two animals died in the control group without NEC, and one died in the rPAF-AH treatment group; all were septic with Escherichia coli and showed histologic changes of inflammatory lung disease.
Small intestinal histology in neonatal rats subjected to asphyxia and formula feeding (hematoxylin and eosin staining).(A) Control animal showing mid-villous necrosis, (B) control animal with complete villous necrosis, (C) rPAF-AH-pretreated animal showing normal intestinal villous architecture,(D) rPAF-AH-pretreated animal with normal ileal histology.
DISCUSSION
In this report, we have shown that pretreatment with the PAF-degrading enzyme PAF-AH can reduce the incidence of NEC in a newborn rat model. PAF is a potent phospholipid inflammatory mediator with diverse biologic actions(15, 16), which may contribute to intestinal injury and the development of neonatal NEC(3–8). Furthermore, recent studies suggest that dysregulation of PAF-AH activity may contribute to the pathophysiology of neonatal NEC. Human neonates have depressed plasma PAF-AH activity in the first several days of life and approach adult enzyme activity only after 6 wk of life(10). In addition, plasma PAF-AH activity in patients with NEC is significantly lower than age-matched controls(7). Interestingly, human milk has significant PAF-AH activity, whereas neonatal formulas have no measurable PAF-AH enzyme function(11), and this discrepancy may contribute to the lower incidence of NEC in breast milk-fed neonates(12). In experimental NEC in adult rats, hormonal up-regulation of plasma PAF-AH activity reduces the incidence of PAF-induced intestinal injury, whereas down-regulation of PAF-AH worsens the bowel necrosis(17). The results of this study further support the protective role of PAF-AH in a neonatal model of non-PAF-induced NEC.
In this study, the neonatal rat model of NEC includes common risk factors for the disease including asphyxia and formula feeding(14). Using this approach approximately 70-80% of animals develop gross and microscopic intestinal injury similar to neonatal NEC by the 3rd d of life. Previous reports have described the role of bacteria(18), breast milk(19), corticosteroids(20), and asphyxia(14) in this model. In this study and in others(14), the majority of neonatal rats die from NEC and not from other organ dysfunction. The studies taken together confirm the reproducibility and reliability of this experimental model for neonatal NEC.
It was surprising to find that enteral administration of rPAF-AH resulted in local mucosal epithelial accumulation of enzyme by immunohistochemical analysis without any systemic absorption and measurable circulating activity. This finding was confirmed by identifying no circulating immunoreactive rPAF-AH in neonatal rats using a specific anti-human rPAF-AH MAb in a standard ELISA assay. Furthermore, intestinal PAF-AH enzyme activity was markedly increased in intestine of treated animals, thereby confirming the functional importance of local PAF-AH in this model. The fact that enteral pretreatment with rPAF-AH prevented intestinal necrosis in our neonatal rats suggests that systemic PAF blockade is not necessary to prevent NEC in this model. PAF has multiple effects on intestinal mucosal pathophysiology including 1) perturbations in mucosal permeability(21), 2) activation of secondary mediators that promote the inflammatory cascade(22), and 3) alterations in intestinal blood flow(23). The exciting findings from this study suggest that local PAF degradation without systemic toxicity can reduce the risk of NEC in neonates. We hypothesize that the local action of PAF-AH in the intestinal mucosal epithelial cells is critical for down-regulating the effects of PAF that subsequently result in the initiation of increased mucosal permeability, bacterial translocation and endotoxinemia, and the activation of the secondary inflammatory response, which leads to the development of intestinal necrosis.
Although recent evidence from our laboratory has shown that PAF receptor antagonists protect against NEC in this model(24), the beneficial effects of PAF-AH in this disease are of critical importance and provide additional support for the role of PAF in neonatal NEC. Recent studies have shown that the PAF receptor is an important determinant of bacterial(Streptococcus) adhesion and invasion in endothelium and epithelium(25). Furthermore, these investigators have shown that the PAF receptor mechanism is a key factor involved in the pathophysiology of inflammatory disease associated with Streptococcus(26). In fact, they speculate that PAF receptor blockade can be used to successfully treat infection without the use of antibiotics. These findings suggest that PAF receptor blockade in the neonatal NEC model may be effective not because of the physiology of PAF but instead due to the protection against bacterial invasion of mucosal epithelium with subsequent translocation and activation of the inflammatory cascade. Because PAF degradation with exogenous PAF-AH would not alter bacterial adhesion and invasion in epithelial cells, results from this study provide further evidence of the important pathophysiologic role of PAF in neonatal NEC.
In summary, we found that enteral administration of rPAF-AH (a human protein) protected against the development of NEC in a neonatal rat model, although the enzyme was not absorbed into the systemic circulation. In addition, intestinal PAF-AH enzyme activity was significantly elevated after enteral administration, supporting the potency of the recombinant enzyme. These findings suggest that the action of PAF in the pathophysiology of NEC may be localized to the intestinal mucosal environment. We speculate that PAF-AH supplementation into feedings of premature newborns at risk for NEC may be a safe and effective approach for reducing the incidence of this devastating disease.
Abbreviations
- PAF:
-
platelet-activating factor
- AH:
-
acetylhydrolase
- rPAF:
-
human recombinant PAF
- NEC:
-
necrotizing enterocolitis
- CHAPS:
-
3-[(3- cholahippocampalopropyl)dimethylammonio]-1-propanesulfonic acid
References
Uauy RD. Fanaroff AA. Korones SB, Philips EA, Philips JB, Wright LL 1991; Necrotizing enterocolitis in very low birth weight infants: biodemographic and clinical correlates. J Pediatr 119: 630–638.
Caplan MS, MacKendrick W 1993; Necrotizing enterocolitis: a review of pathogenetic mechanisms and implications for prevention. Pediatr Pathol 13: 357–369.
Gonzalez-Crussi F, Hsueh W 1983; Experimental model of ischemic bowel necrosis: the role of platelet-activating factor and endotoxin. Am J Pathol 112: 127–135.
Hsueh W, Gonzalez-Crussi F, Arroyave JL 1987; Platelet activating factor is an endogenous mediator for bowel necrosis in endotoxemia. FASEB J 1: 403–405.
Caplan MS, Sun XM, Hsueh W 1990; Hypoxia causes ischemic bowel necrosis in rats: the role of platelet activating factor (PAF-acether). Gastroenterology 99: 979–986.
Sun XM, Hsueh W 1988; Bowel necrosis induced by tumor necrosis factor in rats is mediated by platelet-activating factor. J Clin Invest 81: 1328–1331.
Caplan MS, Sun XM, Hsueh W, Hageman JR 1990; Role of platelet activating factor and tumor necrosis factor-alpha in neonatal necrotizing enterocolitis. J Pediatr 116: 960–964.
Amer MD, Hedlund E, Rochester J, Caplan MS 1997; Stool PAF levels are increased following feeding and in neonatal NEC. J Pediatr (in press)
Farr RS, Wardlow ML, Cox CP, Meng KE, Greene DE 1983; Human serum acid-labile factor is an acylhydrolase that inactivates platelet-activating factor. Fed Proc 42: 3120–3122.
Caplan M, Hsueh W, Kelly A, Donovan M 1990; Serum PAF acetylhydrolase increases during neonatal maturation. Prostaglandins 39: 705–714.
Moya FR, Eguchi H, Zhao B, Furukawa M, Sfeir J, Osorio M, Ogawa Y, Johnston JM 1994; Platelet-activating factor acetylhydrolase in term and preterm human milk: a preliminary report. J Pediatr Gastroenterol Nutr 19: 236–239.
Lucas A, Cole TJ 1990; Breast milk and neonatal necrotising enterocolitis. Lancet 336: 1519–1523.
Tjoelker LW, Wilder C, Eberhardt C, Stafforini DM, Dietsch G, Schimpf B, Hooper S, Trong HL, Cousens LS, Zimmerman GA, Yamada Y, McIntyre TM, Prescott SM, Gray PW 1995; Anti-inflammatory properties of a platelet-activating factor acetylhydrolase. Nature 374: 549–553.
Caplan MS, Hedlund E, Adler L, Hsueh W 1994; Role of asphyxia and feeding in a neonatal rat model of necrotizing enterocolitis. Pediatr Pathol 14: 1017–1028.
Hanahan DJ 1986; Platelet activating factor: a biologically active phosphoglyceride. Annu Rev Biochem 55: 483–509.
Snyder F 1990; Platelet-activating factor and related acetylated lipids as potent biologically active cellular mediators. Am J Physiol 259:C697–C708.
Furukawa M, Lee E, Johnston JM 1993; Platelet-activating factor-induced ischemic bowel necrosis: the effect of PAF acetylhydrolase. Pediatr Res 34: 237–241.
Barlow B, Santulli TV, Heird WC, Pitt J, Blanc WA, Schullinger JN 1974; An experimental study of acute neonatal enterocolitis-the importance of breast milk. J Pediatr Surg 9: 587–594.
Pitt J, Barlow B, Heird WC 1977; Protection against experimental necrotizing enterocolitis by maternal milk. I. Role of milk leukocytes. Pediatr Res 11: 906–909.
Israel EJ, Schiffrin EJ, Carter EA, Freiberg E, Walker WA 1990; Prevention of necrotizing enterocolitis in the rat with prenatal cortisone. Gastroenterology 99: 1333–1338.
Kubes P, Arfors KE, Granger DN 1991; Platelet-activating factor-induced mucosal dysfunction: role of oxidants and granulocytes. Am J Physiol 260:G965–G971.
Hsueh W, Gonzalez-Crussi F, Arroyave JL 1986; Platelet-activating factor-induced ischemic bowel necrosis: An investigation of secondary mediators in its pathogenesis. Am J Pathol 122: 231–235.
Zhang C, Hsueh W 1991; PAF-induced bowel necrosis: Effects of vasodilators. Dig Dis Sci 36: 634–640.
Caplan MS, Hedlund E, Adler L, Lickerman M, Hsueh W 1997; The PAF receptor antagonist WEB 2170 prevents neonatal necrotizing enterocolitis in rats. J Pediatr Gastroenterol Nutr 24: 296–301.
Cundell DR, Gerard NP, Gerard C, Idanpaan-Heikkila I 1995; Streptococcus pneumoniae anchor to activated human cells by the receptor for platelet-activating factor. Nature 377: 435–438.
Cabellos C, MacIntyre, Forrest M, Burroughs M, Prasad S, Tuomanen E 1992; Differing roles for platelet-activating factor during inflammation of the lung and subarachnoid space. The special case ofStreptococcus pneumoniae. J Clin Invest 90: 612–618.
Acknowledgements
The authors thank Dr. Jack Johnston for assistance in measuring PAF-AH activity.
Author information
Authors and Affiliations
Additional information
Supported in part by National Institutes of Health Grant HD-00999, a grant from the March of Dimes, and the ICOS Corporation.
Rights and permissions
About this article
Cite this article
Caplan, M., Lickerman, M., Adler, L. et al. The Role of Recombinant Platelet-Activating Factor Acetylhydrolase in a Neonatal Rat Model of Necrotizing Enterocolitis. Pediatr Res 42, 779–783 (1997). https://doi.org/10.1203/00006450-199712000-00010
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199712000-00010
This article is cited by
-
Pathogenesis of neonatal necrotizing enterocolitis
Pediatric Surgery International (2015)
-
Necrotizing Enterocolitis in Preterm Infants is Related to Enteral Feeding, But the Mechanisms Remain Uncertain and Have Changed Over Time
Current Pediatrics Reports (2014)
-
Human Milk is the Feeding Strategy to Prevent Necrotizing Enterocolitis
Current Pediatrics Reports (2014)
-
The prevalence of platelet activating factor acetylhydrolase single nucleotide polymorphisms in relationship to necrotizing enterocolitis in Northwest Louisiana infants
SpringerPlus (2013)
-
Novel Treatments for NEC: Keeping IBD in Mind
Current Gastroenterology Reports (2012)