Abstract
A factor V506 Arg-Gln mutation is the most common inherited cause of thrombophilia in adults. To date, there are no data regarding the detection of this mutation in neonatal blood or the relationship of this dysfunctional factor V to neonatal thrombosis. This study compared a modified activated protein C resistance functional assay with the PCR-based DNA assay for the factor V mutation in 115 prospectively collected umbilical cord blood samples. The incidence of activated protein C resistance in cord blood was 6%. The sensitivity and specificity of the modified assay for the factor V Leiden mutation was 100%.
Similar content being viewed by others
Main
A mutation in the coagulation factor V gene (factor V Leiden) causes hypercoagulability and venous thrombosis because the activated form of mutant factor V is resistant to physiologic inactivation by its regulator, activated protein C(1–5). This highly conserved point mutation (factor V506 Arg-Gln) has been reported to be present in 3-8% of the adult population and is the most common cause of inherited thrombophilia(1, 6–9).
Although the sick neonate is at increased risk for thrombosis due both to low plasma concentrations of coagulation inhibitor proteins as well as vascular damage caused by frequent use of indwelling catheters(10, 11), the relationship of the factor V mutation to newborn thrombosis has not been studied. Screening for the factor V mutation in adults is commonly with a functional assay for APCR based upon the APTT. We previously showed that a functional assay for activated protein C resistance using native neonatal plasma was not accurate because of both the baseline APTT prolongation and exaggerated prolongation of the APTT after the addition of activated protein C(12). A modified assay has been developed that overcomes prolongations due to deficiencies of clotting proteins other than factor V or inhibitors by mixing the test plasma in dilutions of factor V-deficient plasma(13). We performed this study to determine whether the modified functional assay for APCR was sufficiently sensitive and specific to detect the factor V Leiden mutation in neonates.
METHODS
Clinical protocol. This study was approved by the Colorado Multi-Institutional Review Board. Infants born in University Hospital, Denver, were entered into the study with written, informed consent of the mother. Umbilical cord blood was collected into 3.2% buffered sodium citrate anticoagulant using a two-syringe technique at the time of vaginal or cesarean section delivery. Samples were transported to the laboratory on ice and centrifuged at 2500 × g for 20 min. Plasma for determination of functional APCR was aliquoted and frozen at -70°C. An aliquot of well mixed whole blood was removed for the PCR-based assay before centrifugation. The whole blood was used as a source of DNA for a PCR-based assay of the factor V mutation.
Demographic information as well as a history of arterial or venous thromboses in the neonate's mother, father, siblings, aunts, uncles, or grandparents was collected. Each mother was asked whether she wanted to be informed of the study results; follow-up counseling was based upon the mother's request. Blood samples collected from 31 healthy adults using no medication were used to derive reference values.
Laboratory methods. The modified assay is a prothrombin-based test using thromboplastin. To correct for low levels of plasma coagulation proteins, dilutions of infant plasma are added to factor V-deficient plasma as described by Le et al.(13). The clotting time is determined before and after addition of activated protein C, and expressed as a ratio called the activated protein C ratio. Results of functional APCR are expressed using a ratio obtained by dividing the activated protein C ratio of the test sample by the activated protein C ratio of normal pooled plasma. This correction overcomes variables in test runs. A ratio greater than or equal to 2 SD below the lower limit of the normal range indicates APCR.
The PCR assay was performed on DNA isolated from whole blood based upon the procedure of Bertina et al.(3) as previously described(14). Genomic DNA was isolated from whole blood using commercially prepared reagents exactly as suggested by the manufacturer(Gentra Systems, Minneapolis, MN). To determine the presence of the factor V Leiden mutation, genomic DNA was amplified and assayed for loss of a cleavage site for the restriction enzyme MnlI. A portion of the factor V gene including A to G substitution at nucleotide 1691 which produces the Arg506 to Gln amino acid substitution was amplified by PCR using primers and reaction conditions as described by Ridker et al.(9). The amplification product was digested overnight withMnl I and size fractionated by electrophoresis in 3% agarose gel, and bands were visualized by ethidium bromide staining. Using this technique a person with two wild type factor V alleles displays bands of 37, 82, and 104 bp, whereas those who are heterozygous for the factor V Leiden mutation display bands of 82 and 141 bp.
Data analysis. The prevalence of APCR and the factor V Leiden mutation in the newborn cohort was determined.
RESULTS
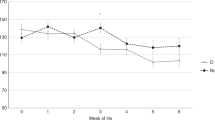
Blood samples from 31 healthy adults were assayed. Thirty control subjects were homozygous for wild type (normal) factor V by PCR; these 30 control subjects had a mean modified functional APCR ratio of 1.15 (SD 0.25) and an observed range of 0.76 to 1.94 (Fig. 1). One control adult had an APCR ratio of 0.26; this adult was heterozygous for the factor V Leiden mutation by PCR and had a positive family history for thrombosis(Fig. 2). One hundred and fifteen random cord blood samples were analyzed. None of the infants manifested signs of thrombosis at birth or while hospitalized. One hundred and eight cord blood samples were homozygous wild type by PCR. The normal cord blood samples had a mean functional APCR ratio of 1.13 (SD 0.22), observed range 0.73 to 1.90. Seven of the cord blood samples were heterozygous for APCR by PCR; the mean functional APCR ratio of these seven samples was 0.38 (SD 0.10), observed range 0.21 to 0.49. There was no overlap in modified APCR ratios between wild type and heterozygotes for the factor V mutation.
The sample population was white (50%), Hispanic (32%), African American(15%), and Asian (3%). This compares with the demographics of the Denver metropolitan area which are: white (79.5%), Hispanic (12%), African American(5.4%), Asian (2.3%), and Native American (0.8%). The demographics of births at University Hospital is the same as the sample population.
The prevalence of the factor V Leiden mutation relative to ethnicity was: 5% (3 of 58) in white, 11% (4 of 37) in Hispanic, 0% (0 of 16) in African American, and 0% (0 of 4) in Asian cord blood samples. Fourteen neonates (14%) had a positive family history of thrombosis. Of these neonates, only 2 (14%) had the factor V Leiden mutation. Five neonates with a negative family history of thrombosis had the factor V Leiden mutation.
DISCUSSION
APCR conveyed by factor V506 Arg-Gln is the most common cause of inherited thrombophilia. Heterozygous mutant factor V is prevalent in the general population and increases the risk of venous thrombosis 5-10-fold(8). Our prevalence of the factor V Leiden mutation relative to ethnicity was comparable to that previously reported in the literature with the exception of the Hispanic group where we found a substantially higher prevalence of this mutation(16). Our Hispanic group is of Mexican-American background. A larger study would be necessary to confirm this finding.
Many clinically affected adults with the factor V Leiden mutation have had one or more additional risk factors for thrombosis at the time of a clinical event(8). Although in the pediatric population, genetic thrombophilia most often presents in adolescence after onset of puberty, thromboses also occur in increased frequency in neonates, especially sick neonates with indwelling vascular access devices.
Genetic heterozygous deficiencies of antithrombin III(17–19), protein C(20–22), and protein S(22), have all been reported in association with neonatal thrombosis. To date, one neonate has been reported with neonatal purpura fulminans in association with heterozygous factor V Leiden(23). No other risk factors for thrombosis were found in the reported infant. It is highly unlikely that factor V Leiden alone was etiologically related to purpura fulminans as the heterozygous mutation should be present in approximately 150,000 infants born in the United States each year, and the frequency of neonatal purpura fulminans is much less.
There has been no information regarding functional APCR in the neonate, or the application of the modified functional assay for APCR to neonates. The factor V mutation should be diagnosable by functional assay at birth as the plasma concentration of factor V is within the adult normal range, even in extremely premature infants(24). We found complete correlation between the modified functional assay for APCR employing factor V deficient plasma and a PCR-based assay in neonatal blood. A partial thromboplastin time-based APCR assay using a lesser dilution of test plasma into factor V-deficient plasma has recently been studied in adults(15). The specificity of that assay is 98.8% with a sensitivity of 100%. It performed well in plasma from adults suspected of acute thrombosis as well as in control plasma.
Genetic APCR can be determined in neonates using either the modified functional or PCR assay. Compared with the PCR assay, the functional assay requires substantially less time to perform and is less costly. Either of these tests can be applied to future studies to determine the role of APCR in spontaneous or catheter-related thromboses in the neonate.
Acknowledgments. The authors thank the neonatal CRC nurses for their assistance in subject recruitment, as well as in sample and data collection.
Abbreviations
- APCR:
-
activated protein C resistance
- APTT:
-
partial thromboplastin time
References
Koster T, Rosendaal FR, DeRonde H. Briët E, Vandenbrouke JP, Bertina RM 1993; Venous thrombosis due to poor anticoagulant response to activated protein C: Leiden thrombophilia study. Lancet 342: 1503–1506.
Griffin JH, Evatt B, Wideman C. Fernandez JA 1993; Anticoagulant protein C pathway defective in majority of thrombophilic patients. Blood 82: 1989–1993.
Bertina RM, Koeleman BPC, Koster T, Rosendaal FR, Dirven RJ, de Ronde H, van der Velden PA, Reitsma PH 1994; Mutation in blood coagulation factor V associated with resistance to activated protein C. Nature 369: 64–67.
Greengard JS, Sun X, Xu X. Fernandez JA, Griffin JH, Evatt B 1994; Activated protein C resistance caused by Arg506Gln mutation in factor Va. Lancet 343: 1361–1362.
Voorberg J, Roelse J, Koopman R, Buller H, Berends F, ten Cate JW, Mertens K, van Mourik SA 1994; Association of idiopathic venous thromboembolism with single point mutation at Arg 506 of factor V. Lancet 343: 1535–1536.
Svensson PJ, Dahlbäck B 1994; Resistance to activated protein C as a basis for venous thrombosis. N Engl J Med 330: 517–522.
Rees DC, Cox M. Cless JB 1995; World distribution of factor V Leiden. Lancet 346: 1133–1134.
Dahlback B 1995; Inherited thrombophilia: resistance to activated protein C as a pathogenic factor of venous thrombosis. Blood 85: 607–614.
Ridker PM, Hennekens CH. Lindpaintner K, Stampfer MJ, Eisenberg PR, Miletich JP 1995; Mutation in the gene coding for coagulation factor V and the risk of myocardial infarction, stroke, and venous thrombosis in apparently healthy men. N Engl J Med 332: 912–917.
Manco-Johnson MJ 1994; Disseminated intravascular coagulation and other hypercoagulable syndromes. Int J Pediatr Hematol Oncol 1: 1–23.
Manco-Johnson MJ 1990; Diagnosis and management of thromboses in the perinatal period. Semin Perinatol 14: 393–402.
Manco-Johnson MJ, Nuss R. Jacobson LJ, Hathaway WW 1994; Activated protein C cofactor is increased in neonates. Blood 84:A330.
Le DT, Griffin JH, Greengard JS, Mujumdar V, Rapaport SI 1995; Use of generally applicable tissue factor dependent factor V assay to detect activated protein C resistant factor Va in patients receiving warfarin and in patients with a lupus anticoagulant. Blood 85: 1704–1711.
Sifontes MT. Nuss R, Hunger SP. Wilimas J, Jacobson LJ, Manco-Johnson MJ 1997; The factor V Leiden mutation in children with cancer and thrombosis. Br J Haematol 96: 484–489.
Svensson PJ, Zoller B, Dahlbäck B 1997; Evaluation of original and modified APC-resistance tests in unselected outpatients with clinically suspected thrombosis and in healthy controls. Thromb Haemostasis 77: 332–335.
Ridker PM, Miletich JP, Hennekens CH, Buring JE 1997; Ethnic distribution of factor V Leiden in 4047 men and women. Implications for venous thromboembolism screening. JAMA 277: 1305–1307.
De Stefano V 1987; Antithrombin III in full-term and pre-term newborn infants: three cases of neonatal diagnosis of ATIII congenital defect. Thromb Haemostasis 57: 329–331.
Brenner B 1988; Cerebral thrombosis in a newborn with a congenital deficiency of antithrombin III. Am J Hematol 27: 209–211.
Jochmans K 1994; Antithrombin-Gly 424 Arg: a novel point mutation responsible for type 1 antithrombin deficiency and neonatal thrombosis. Blood 83: 146–151.
Rogers PC, Silva MP, Carter JE, Wadsworth LD 1989; Renal vein thrombosis and response to therapy in a newborn due to protein C deficiency. Eur J Pediatr 149: 124–125.
Goodwin TM, Gazit G, Gordon EM 1995; Heterozygous protein C deficiency presenting as severe protein C deficiency and peripartum thrombosis: successful treatment with protein C concentrate. Obstet Gynecol 86: 662–664.
Formstone CJ, Hallam PJ, Tuddenham EG, Voke J, Layton M, Nicolaides K, Hann IM, Cooper DN 1996; Severe perinatal thrombosis in double and triple heterozygous offspring of a family segregating two independent protein S mutations and a protein C mutation. Blood 87: 3731–3737.
Pipe SW, Schmaier AH, Nichols WC. Ginsburg D, Bozynski MEA, Castle VP 1996; Neonatal purpura fulminans in association with factor V R506Q mutation. J Pediatr 128: 706–709.
Hathaway WE, Bonnar J 1987; Hemostatic Disorders of the Pregnant Woman and Newborn Infant. Elsevier Publishing. New York, 58
Author information
Authors and Affiliations
Additional information
Supported by Grant 5 MO1 RR00069 from the General Clinical Research Centers Program for National Center for Research Resources, National Institutes of Health, and the Cancer Center and The Children's Hospital Research Institute, The Children's Hospital, Denver, Colorado. S.P.H. is the recipient of a Blood/ASH Scholar Award.
Rights and permissions
About this article
Cite this article
Sifontes, M., Nuss, R., Hunger, S. et al. Correlation between the Functional Assay for Activated Protein C Resistance and Factor V Leiden in the Neonate. Pediatr Res 42, 776–778 (1997). https://doi.org/10.1203/00006450-199712000-00009
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199712000-00009