Abstract
Infants with congenital diaphragmatic hernia (CDH) have a high neonatal mortality and morbidity owing to lung hypoplasia and persistent pulmonary hypertension. Pulmonary neuroendocrine cells produce bombesin-like peptide (BLP), a peptide with growth factor-like properties involved in lung development. We examined the expression of BLP immunostaining in pulmonary neuroendocrine cells (PNEC), and in clusters of these cells called neuroepithelial bodies (NEB), in the lungs of three groups of infants: patients with CDH, newborns with lung hypoplasia due to other causes, and control subjects without lung abnormalities. Morphometric analysis included: 1) percent immunostained airways; 2) percent immunostained epithelium (i.e. frequency of PNEC and NEB); and 3) NEB size. Controls and infants with lung hypoplasia did not differ with respect to BLP immunostaining. The ipsilateral and the contralateral lungs in CDH had a similar BLP immunostaining pattern of PNEC and NEB. The BLP immunostaining varied between CDH cases, possibly due to the differences in clinical presentation. The mean NEB size was significantly increased in infants with CDH compared with the other two groups (p = 0.02). Some CDH cases with large NEBs also showed a high percentage of immunostained epithelium. Lung-body weight ratio correlated positively with percent immunostained airways, and negatively with the NEB size. We conclude that in lungs of CDH patients BLP immunostaining in PNEC and NEB differs from that of infants with lung hypoplasia due to other causes and controls. The increased BLP immunostaining observed in some cases of CDH might reflect a compensatory mechanism related to impaired lung development and/or failure of neuropeptide secretion during neonatal adaptation.
Similar content being viewed by others
Main
NEB are clusters of innervated PNEC that produce amines and peptides(1, 2). Distributed throughout the airway mucosa, PNEC and NEB might play an important role in lung development(3–7) and during neonatal adaptation(3, 4) as NEB are transducers of the hypoxic stimulus and could, therefore, act as airway chemoreceptors in the regulation of respiration(8).
The principal peptide produced by PNEC is GRP, the mammalian counterpart of bombesin(4). Antibodies against BLP or GRP are most widely used as a marker of PNEC in human lungs, because BLP immunopositive cells have been identified in fetal lungs from 7 to 10 wk of gestation onward(2, 9, 10). BLP immunoreactive PNEC differentiate in a craniocaudal direction, and the highest number of cells is found in the small peripheral airways toward the end of gestation(3, 10). Experimental studies revealed that BLP regulates lung branching morphogenesis(7, 11) and stimulates lung growth and maturation(6). A recent study revealed that in mammalian lung the expression of the GRP receptor is developmentally regulated and that the GRP receptor plays an important role, especially during the canalicular stage of lung development(12).
Infants with CDH have abnormal morphologic development of lungs and intrapulmonary blood vessels(13, 14). The high neonatal mortality and morbidity in these children are ascribed to the extent of lung hypoplasia and persistent pulmonary hypertension(15). We have previously reported the expression of CGRP-positive PNEC in a rat model of CDH(16). Lungs of full-term rat pups with CDH contained increased numbers of CGRP-immunostained PNEC compared with the lungs of controls. In the rat, CGRP immunoreactivity has been studied during normal lung development and has been proven to be a reliable marker of PNEC(17), whereas no BLP immunostaining can be detected in this animal species(18). In the human lung the reverse is true. CGRP immunoreactivity has been reported from gestational wk 20 onward(19), but inconsistently and only in a limited number of cells(18, 19).
In this study, using morphometric methods, we investigated the expression of BLP immunostaining in PNEC of lungs from patients with CDH and compared them to lungs from infants with lung hypoplasia due to other causes, and to lungs from control infants without lung abnormalities who died during the perinatal period.
METHODS
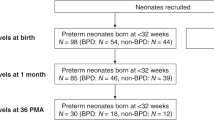
Patients. Cases of CDH and of lung hypoplasia due to other causes were selected from the autopsy files of the Departments of Pathology in a large Pediatric Center in Canada (The Hospital for Sick Children in Toronto), and in 10 different hospitals in the Netherlands, spanning the period from 1967 to 1995. Age-matched controls without lung abnormalities were selected from the files of The Hospital for Sick Children in Toronto. The cases for this study were selected on the basis of the clinical diagnosis, of the fixative that had been used (only formalin-fixed tissues were examined), and of good histologic preservation of lung tissue with the presence of intact airway epithelium to identify PNEC and NEB. The use of artificial ventilation for a longer period with high inspiratory peak pressures, especially in cases of CDH, leads to diffuse epithelial damage and hence precludes examination of this lung cell population. Consequently, cases with severe epithelial damage were excluded. Lung hypoplasia was established according to the lung body weight ratio, using the criteria of Askenazi and Perlman(20). Most CDH patients were born at term, and cases from both other groups were therefore selected to obtain the best possible match for gestational age. Control cases were further selected to obtain the best possible match for age at death. Thus, 10 CDH patients were included, as well as seven children with lung hypoplasia and four controls (see Tables 1–3). The autopsy records of all patients were examined for the presence of brainstem pathology.
Histologic examination. Routine 4-μm sections of formalin-fixed, paraffin-embedded lung tissue were immunostained for BLP using the indirect avidin biotin complex staining procedure as previously described(21). All sections were digested with 0.5% pepsin (Sigma Chemical Co.) and incubated overnight with the primary MAb (dilution 1:800) against BLP (Boehringer Mannheim, Germany). Counterstaining was performed with hematoxylin.
With the aid of a projecting microscope (magnification ×700), the total area of airway epithelium of 20 noncartilaginous airways per section and the BLP-immunostained epithelium of these airways were traced on paper(22). The same procedure was done for the 20 largest NEB, located mainly in the medium sized airways, in each section. All drawings were scanned at similar brightness and contrast level, using a Hewlett Packard Scanjet connected to an Apple Macintosh computer. Morphometric analysis included measurements of the total epithelial surface area of 20 airways containing BLP-immunostained cells (referred to as immunostained airways), the BLP-positive areas of airway epithelium in these 20 airways, and the surface area (size) of 20 bronchial NEBs, using the Apple Macintosh National Institutes of Health Image 1.53 program. The BLP-immunostained area in relation to the total epithelial area, referred to as the%IMS-epithelium(22) was calculated from the resulting data. In addition, the%IMS-airways was determined for all sections by counting(23). The average%IMS-epithelium, NEB size, and%IMS-airways were determined per section.
All available sections per case (range 2-5, 62 in total) were studied; 15 sections contained less than 20 noncartilaginous airways to determined the%IMS-epithelium. The median number of airways studied in these sections was 15 (range 6-19). The%IMS-epithelium per case was measured in a median of 40 airways in the CDH group (range 35-80), of 60 airways for the lung hypoplasia group (range 40-85), and of 60 airways (range 52-60) for the controls. Twenty bronchial NEBs could be obtained in all sections. The mean values from the different sections of each case were calculated and compared with other cases.
Data analysis. All data presented are median (range). Differences between groups were tested by one-way ANOVA with the Student-Newman-Keuls test for multiple comparisons or by the nonparametric Kruskal-Wallis test if appropriate. The relationship between clinical data and morphometric results was studied by least square regression. For statistical analysis of the morphometric data, two prematurely born infants (one with CDH and one with lung hypoplasia without CDH; cases 10 and 17, respectively), and two other patients with CDH (one with multiple congenital anomalies, and one with prolonged artificial ventilation; cases 8 and 9, respectively) were excluded to obtain homogeneous groups. Statistical significance was assumed at a two-tailed 5% level.
RESULTS
The clinical data are shown in Tables 1–3. Gestational age, birth weight, and age at death were not significantly different between the three groups; the lung-body weight ratio was significantly higher in control subjects than in both other groups (p < 0.001), whereas the lung hypoplasia cases without CDH had a higher lung-body weight ratio than did CDH patients (p < 0.05).
BLP immunostaining was positive in all sections studied. Qualitative analysis of immunostaining revealed a variable intensity of positive immunostaining. The presence of intensely immunostained NEB was observed in six CDH cases (cases 2, 3, and 4-7), in two cases of lung hypoplasia (cases 11 and 17), and in one control case (case 19). Brown, moderately immunostained NEB were found in one CDH case (case 8), two cases of lung hypoplasia (case 15 and 16), and in three control cases (case 18, 20, and 21). Pale-stained NEB were found in three CDH cases (case 1, 9, and 10) and in three lung hypoplasia cases (case 12-14). In three cases of CDH (case 2, 3, and 7) large NEB, sometimes located “beneath” the epithelium, were found in the large airways and at the bronchoal-veolar junctions (Figs. 1 and 2). This phenomenon was not observed in lung hypoplasia cases (Fig. 3) or in control subjects (Fig. 4).
Morphometric data in CDH cases were similar for the ipsilateral and contralateral lungs. Therefore, data from all lung sections of each case were averaged. Statistical analysis of 17 cases (seven CDH cases, six lung hypoplasia cases, and four control cases) of both lungs together showed a higher%IMS-airways in controls than in CDH patients (95 (86-97)% versus 80 (67-85)%, respectively; p = 0.02). The NEB size was significantly larger in lungs of infants with CDH compared with the other two groups (467 (293-656) μm2 in CDH versus 327 (252-472) μm2 in lung hypoplasia, and 312 (215-339) μm2 in controls; p = 0.02). The lung-body weight ratio correlated positively with the%IMS-airways (p = 0.05) and negatively with the NEB size (p = 0.02). The%IMS-epithelium was not significantly different between the groups. However, some cases of CDH with large NEB (Table 1, cases 2, 3, 5, and 7) had also a high value for%IMS-epithelium (Fig. 5).
The mean NEB size and the%IMS-epithelium of the ipsilateral and contralateral lungs are shown for CDH patients included in statistical analysis (n = 7); the three CDH patients who were excluded from statistical analysis include cases with multiple congenital anomalies (case 8), prolonged exposure to hyperoxia (case 9), and prematurity, prolonged artificial ventilation, and hyaline membrane disease (case 10); lung hypoplasia cases (n = 6); one prematurely born infant was excluded (case 17), and controls (n = 4). For CDH patients the data from the ipsilateral and contralateral lungs are shown separately; from some slides it was not clear whether they represented the ipsilateral or the contralateral lung. These are indicated as separate symbols (CDH, side unknown). For both other groups the mean value of both lungs is shown. The dashed lines indicate the median NEB size and median%IMS-epithelium of the control cases.
Statistical analysis of the separate left and right lungs could be performed in 14 cases-five CDH cases, [three with left-sided CDH (cases 1, 2, and 4), one with right-sided CDH (case 3), and one with bilateral CDH (case 5)], five lung hypoplasia cases (cases 12-16), and four controls. The results are shown in Table 4. No significant differences were observed between the groups.
DISCUSSION
We found that the expression of BLP immunostaining in GRP in lungs of patients with CDH was different from that in lungs of infants with lung hypoplasia due to another cause, and also differed from those without pulmonary abnormalities. Controls had a higher%IMS-airways, which was also reflected in the positive correlation between the%IMS-airways and the lung-body weight ratio. In some CDH cases very large NEBs were found concomitant with a high percentage of immunostained epithelium.
The BLP immunostaining in PNEC and NEB of lungs of infants and children has been investigated for several different pulmonary diseases(2). Only few data on BLP immunostaining in lungs of patients with hypoplastic lungs are available. Absent or very low BLP immunostaining has been reported in preliminary studies of a small number of infants with lung hypoplasia or CDH(4, 24). Jaramillo et al.(25) reported that the density of GRP-immunoreactive cells in lungs of children with anencephaly and lung hypoplasia was similar to that of anencephalic patients without lung hypoplasia and that of normal control subjects. But more GRP-positive cells were located in the airways in anencephalic patients with lung hypoplasia than in those of patients without lung hypoplasia(25). It is not clear whether differences in tissue processing, methodology, or the gestational ages might explain the differences with our observations.
An important prerequisite for our study was the preservation of airway epithelium. Therefore, patients with extensive epithelial damage who had been ventilated for more than a few hours had to be excluded. This resulted in a selection of CDH patients with severe lung hypoplasia resulting in death shortly after birth. Most children had died within the first 2 h after birth, and only two children had lived for more than 2.5 h. The number of cases studied was the maximal number that could be retrieved from files of the Pathology Departments of 10 institutions in the Netherlands and in The Hospital for Sick Children in Toronto between 1967 and 1996. (Before this period, Zenker's fixative has been used, precluding immunostaining for BLP). This represents the first study of BLP immunostaining in a comprehensive cohort of infants with CDH.
The variation in BLP immunostaining observed in CDH cases might be partly explained by the differences in clinical history. The lungs of the patients who survived longest (cases 9 and 10) and of a dysmaturely stillborn patient with multiple congenital anomalies (case 8) showed pale immunostaining, relatively small NEB, and the lowest%IMS-epithelium. Patient number 10 was prematurely born and had hyaline membrane disease, a condition that is known to decrease BLP immunostaining(4, 9, 26). It can be assumed that the prolonged treatment with artificial ventilation and oxygen therapy in cases 9 and 10 and the renal abnormalities in case 8 might have influenced the BLP immunostaining in the lungs. These cases were not included in the statistical analysis, to maintain uniform clinical parameters.
The largest NEB and the highest%IMS-epithelium were found in lungs from CDH patients with severe hypoplasia who could not be ventilated adequately and died shortly after birth. Whether the function of these large NEB is abnormal is speculative. It is known that NEB are transducers of the hypoxic stimulus(8), and that increased exocytosis with secretion of neurotransmitters occurs during hypoxia(27). We speculate that large NEB might indicate failure of neuropeptide release, i.e. that the hypoxic secretory response has not occurred. Such a phenomenon has been reported in infants with asphyxia and loss of brainstem function who generally died after more than 24 h(28). In the present study the brainstem was examined in most infants, and no evidence of brainstem damage was observed. This could, therefore, not explain our findings.
On the other hand, it can be assumed that, during resuscitation of the CDH patients using artificial ventilation and a high inspired oxygen fraction, the local concentration of oxygen in the airways was high, which might have inhibited exocytosis. This is supported by the findings of Lauweryns et al.(29), who reported that a low oxygen concentration of the inhaled air, but not hypoxemia, stimulates secretion of serotonin by NEB.
The lungs of children with lung hypoplasia, secondary to renal or genitourinary abnormalities, showed variation in BLP immunostaining. The pattern of BLP immunostaining was, however, different from that in CDH patients. Half of the cases with lung hypoplasia showed pale immunostaining, and the NEB size and the%IMS-epithelium were within the same range as that found in control subjects. The differences in BLP immunostaining between the lung hypoplasia cases could not be explained by differences in gestational age or in clinical presentation.
In conclusion, we found that the BLP immunostaining in lungs of CDH patients differs from that of age-matched controls and from that of infants with lung hypoplasia due to other causes. Infants with the most severe lung hypoplasia and persistent pulmonary hypertension, as reflected by their very early age at death, have increased BLP immunostaining. Because BLP stimulates lung growth and lung maturation(6) it might be assumed that the increased BLP immunostaining reflects a maximal response of the lung to compensate for the abnormal growth in CDH. In an experimental setting using a rat model of CDH enlarged NEB and increased expression of CGRP have been reported(16, 30). In the developing rat lung, CGRP immunoreactivity reaches its maximum near term(17), a developmental pattern similar to that of BLP in the human lung(3). We therefore propose that the rat model of CDH is suitable for the performance of further studies of the altered expression of neuroendocrine cells and their peptides in the lungs in CDH.
It can also be assumed that the increased BLP immunostaining, observed in some CDH patients, reflects the extent of persistent pulmonary hypertension. This assumption is supported by a study that reported increased BLP immunostaining in older patients with primary pulmonary hypertension(31), although BLP itself exerts no effect on the pulmonary vascular tone(32, 33). The large BLP-positive NEBs in lungs of CDH patients might, however, contain other peptides, such as leuenkephalin(21), endothelin(2), or serotonin(2), which are known to induce pulmonary vasoconstriction(2, 32). However, our present data do not allow for conclusions regarding the role of NEB in abnormal lung development in CDH.
Abbreviations
- BLP:
-
bombesin-like peptide
- CDH:
-
congenital diaphragmatic hernia
- CGRP:
-
calcitonin gene-related peptide
- GRP:
-
gastrin-releasing peptide
- NEB:
-
neuroepithelial bodies
- PNEC:
-
pulmonary neuroendocrine cells
- % IMS-airways:
-
percentage immunostained airways
- % IMS-epithelium:
-
percentage immunostained epithelium
References
Lauweryns JM, Peuskens JC 1972 Neuro-epithelial bodies (neuroreceptor or secretory organs?) in human infant bronchial and bronchiolar epithelium. Anat Rec 172: 417–482.
Cutz E, Gillan JE, Perrin DG 1995 Pulmonary neuroendocrine cell system: an overview of cell biology and pathology with emphasis on pediatric lung disease. Perspect Pediatr Pathol 18: 32–70.
Cutz E, Gillan JE, Bryan AC 1985 Neuroendocrine cells in the developing human lung: morphologic and functional considerations. Pediatr Pulmonol 1( suppl): S21–S29.
Sunday ME, Kaplan LM, Motoyama E, Chin WW, Spindel ER 1988 Gastrin-releasing peptide (mammalian bombesin) gene expression in health and disease. Lab Invest 59: 5–24.
Li K, Nagalla SR, Spindel ER 1994 A rhesus monkey model to characterize the role of gastrin releasing peptide (GRP) in lung development. J Clin Invest 94: 1605–1615.
Sunday ME, Hua J, Dai HB, Nusrat A, Today JS 1990 Bombesin increases fetal lung growth and maturation in utero and in organ culture. Am J Respir Cell Mol Biol 3: 199–205.
King KA, Torday JS, Sunday ME 1995 Bombesin and [Leu8]phylloitorin promote fetal mouse lung branching morphogenesis via a receptor-mediated mechanism. Proc Natl Acad Sci USA 92: 4357–4361.
Youngson C, Nurse C, Yeger H, Cutz E 1993 Oxygen sensing in airway chemoreceptors. Nature 365: 153–155.
Ghatei MA, Sheppard MN, Henzen-Logman S, Blank MA, Polak JM, Bloom SR 1983 Bombesin and vasoactive intestinal polypeptide in the developing lung: marked changes in acute respiratory distress syndrome. J Clin Endocrinol Metab 57: 1226–1232.
Spindel ER, Sunday ME, Hofler H, Wolfe HJ, Habener JF, Chin WW 1987 Transient elevation of messenger RNA encoding gastrin-releasing peptide, a putative pulmonary growth factor in human fetal lung. J Clin Invest 80: 1172–1179.
Aguayo SM, Schuyler WE, Murtagh JJ, Roman J 1994 Regulation of lung branching morphogenesis by bombesin-like peptides and neutral endopeptidase. Am J Respir Cell Mol Biol 10: 635–642.
Wang D, Yeger H, Cutz E 1996 Expression of gastrin-releasing peptide receptor gene in developing lung. Am J Respir Cell Mol Biol 14: 409–416.
George DK, Cooney TP, Chiu BK, Thurlbeck WM 1987 Hypoplasia and immaturity of the terminal lung unit (acinus) in congenital diaphragmatic hernia. Am Rev Respir Dis 136: 947–950.
Levin DL 1978 Morphologic analysis of the pulmonary vascular bed in congenital left-sided diaphragmatic hernia. J Pediatr 107: 457–464.
Molenaar JC, Bos AP, Hazebroek FWJ, Tibboel D 1991 Congenital diaphragmatic hernia, what defect? J Pediatr Surg 26: 248–254.
IJsselstijn H, Perrin DG, de Jongste JC, Cutz E, Tibboel D 1995 Pulmonary neuroendocrine cells in neonatal rats with congenital diaphragmatic hernia. J Pediatr Surg 30: 413–415.
Wada C, Hashimoto C, Kameya T, Yamaguchi K, Ono M 1988 Developmentally regulated expression of the calcitonin gene related peptide (CGRP) in rat lung endocrine cells. Virchows Archiv B Cell Pathol 55: 217–223.
Sorokin SP, Hoyt RF 1989 Neuroepithelial bodies and solitary small-granule cells. In: Massaro D (ed) Lung Cell Biology. Marcel Dekker, New York, pp 191–344.
Johnson DE, Wobken JD 1987 Calcitonin gene-related peptide immunoreactivity in airway epithelial cells of the human fetus and infant. Cell Tissue Res 250: 579–583.
Askenazi SS, Perlman M 1979 Pulmonary hypoplasia: lung weight and radial alveolar count as criteria of diagnosis. Arch Dis Child 54: 614–618.
Cutz E, Chan W, Track NS 1981 Bombesin, calcitonin and len-enkephalin immunoreactivity in endocrine cells of human lung. Experientia 37: 765–767.
Perrin DG, McDonald TJ, Cutz E 1991 Hyperplasia of bombesin-immunoreactive pulmonary neuroendocrine cells and neuroepithelial bodies in sudden infant death syndrome. Pediatr Pathol 11: 431–447.
Gillan JE, Cutz E 1993 Abnormal pulmonary bombesin-immunoreactive cells in Wilson-Mikity syndrome (pulmonary dysmaturity) and bronchopulmonary dysplasia. Pediatr Pathol 13: 165–180.
Durbin J, Thomas P, Langston C, Goswami S, Alba Greco M 1996 Gastrin-releasing peptide in hypoplastic lungs. Pediatr Pathol Lab Med 16: 927–934.
Jaramillo MA, Gutiérrez JA, Margraf LR 1995 Pulmonary gastrin-releasing peptide expression in anencephaly. Pediatr Pathol 15: 377–387.
Johnson DE, Lock JE, Elde RP, Thompson TR 1982 Pulmonary neuroendocrine cells in hyaline membrane disease and bronchopulmonary dysplasia. Pediatr Res 16: 446–454.
Lauweryns JM, De Bock V, Guelinckx P, Decramer M 1983 Effects of unilateral hypoxia on neuroepithelial bodies in rabbit lungs. J Appl Physiol 55: 1665–1668.
Gillan JE, Pape KE, Cutz E 1986 Association of changes in bombesin immunoreactive neuroendocrine cells in lungs of newborn infants with persistent fetal circulation and brainstem damage due to birth asphyxia. Pediatr Res 20: 828–833.
Lauweryns JM, Cokelaere M, Lerut T, Theunynck P 1978 Cross-circulation studies on the influence of hypoxia and hypoxaemia on neuro-epithelial bodies in young rabbits. Cell Tissue Res 193: 373–386.
Yamataka T, Puri P 1996 Increased intracellular levels of calcitonin gene-related peptide-like immunoreactivity in pulmonary endocrine cells in an experimental model of congenital diaphragmatic hernia. Pediatr Surg Int 11: 448–452.
Gosney J, Heath D, Smith P, Harris P, Yacoub M 1989 Pulmonary endocrine cells in pulmonary arterial disease. Arch Pathol Lab Med 113: 337–341.
Gillespie MN, Reinsel CN, Bowdy BD 1984 Pulmonary vasoactivity of lung endocrine cell-related peptides. Peptides 5: 21–24.
Kulik TJ, Johnson DE, Elde RP, Lock JE 1983 Pulmonary vascular effects of bombesin and gastrin-releasing peptide in conscious newborn lambs. J Appl Physiol 55: 1093–1097.
Acknowledgements
The authors thank the members of the Association of Pediatric Pathologists from the Netherlands for the opportunity to select CDH cases, and the Departments of Pathology of the University Hospital Leiden (Prof. Dr. G. J. M. Fleuren), of the Radboud Hospital Nijmegen (Prof. Dr. D. J. Ruiter), and of the Drechtsteden Hospital Dordrecht (Dr. Heinhuis) for the opportunity to use autopsy material. The authors also thank W. Chan, I. Leitis, and V. Wong for technical assistance, and E. Farkas for computer assistance (all staff members of the Department of Pathology of the Hospital for Sick Children in Toronto).
Author information
Authors and Affiliations
Additional information
Supported by the Netherlands Asthma Fund (Project No. 91.56), and the Ter Meulen Fund, Royal Netherlands Academy of Arts and Sciences.
Rights and permissions
About this article
Cite this article
Ijsselstijn, H., Gaillard, J., De Jongste, J. et al. Abnormal Expression of Pulmonary Bombesin-Like Peptide Immunostaining Cells in Infants with Congenital Diaphragmatic Hernia. Pediatr Res 42, 715–720 (1997). https://doi.org/10.1203/00006450-199711000-00026
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199711000-00026
This article is cited by
-
Distinct roles for SOX2 and SOX21 in differentiation, distribution and maturation of pulmonary neuroendocrine cells
Cellular and Molecular Life Sciences (2023)
-
Real-time prediction of patient immune cell modulation during irreversible electroporation therapy
Scientific Reports (2019)
-
Assessment of the nitrofen model of congenital diaphragmatic hernia and of the dysregulated factors involved in pulmonary hypoplasia
Pediatric Surgery International (2019)
-
Oxygen Sensing in Early Life
Lung (2016)