Abstract
We investigated the effect of streptozotocin-induced short-term maternal diabetes upon fetal rat myocardial and skeletal muscle glucose transporter Glut 1 (basal form) and Glut 4 (insulin-responsive form) protein concentrations by Western blot analysis. In the severely diabetic group(SEVERE-D, n = 17), a 3-fold increase in maternal and fetal glucose concentrations (p < 0.01) was associated with a 3-fold decline in maternal (p < 0.01) with no change in fetal insulin levels when compared with the streptozotocin-treated nondiabetic (n = 10) and vehicle-treated control (control, n = 14) groups. These changes in the SEVERE-D group when compared with controls were associated with a 30 and 65% decline, respectively, in fetal myocardial and skeletal muscle (forelimb and hind limb) Glut 1 protein concentrations. The fetal myocardium also demonstrated a 45% decline in Glut 4 protein levels. Fetal skeletal muscle Glut 4 protein, which was expressed only at very low levels in controls showed no change in SEVERE-D. Immunohistochemical analysis revealed a myocyte-plasma membrane association of Glut 1 and an intracellular Glut 4 distribution in the fetal myocardium and skeletal muscle. No Glut 1 immunoreactivity was noted in either the fetal myocardial or skeletal muscle perineural sheaths, blood vessels, or the entrapped fetal red blood cells. This subcellular localization pattern was unaltered in all three treatment groups. We conclude that maternal diabetes causing fetal hyperglycemia with normoinsulinemia suppresses fetal myocardial Glut 1 and Glut 4 and fetal skeletal muscle Glut 1. The decline in the plasma membrane associated Glut 1 concentrations may serve a protective function by reducing the glucose transport rate into fetal myocardial and skeletal muscle cells, which otherwise could be vulnerable to high circulating glucose. The in-utero maternal diabetes induced decrease in fetal myocardial intracellular-Glut 4 concentration could herald the emergence of insulin resistance.
Similar content being viewed by others
Main
In the fetus, the predominant insulin-responsive tissues are skeletal muscle and myocardium. The fetal myocardium utilizes a large portion of the glucose substrate for oxidative metabolism(1, 2).In utero perturbations in circulating glucose concentrations result in fetal and neonatal myocardial dysfunction(3, 4), as well as alterations in skeletal muscle glucose utilization(2, 5). The rate-limiting step of glucose entry into cardiomyocytes and skeletal myocytes is that of glucose transport(6, 7). This process is mediated by a family of membranespanning glycoproteins that transport glucose across bilipid plasma membranes along its concentration gradient in a nonenergy-dependent manner(8, 9). Of the six facilitative glucose transporter isoforms characterized to date, two specific types, namely Glut 1(erythrocyte-form) and Glut 4 (insulin-responsive form) are expressed by insulin responsive tissues(8, 9). In the adult rat myocardium, alterations in circulating glucose and insulin, specifically in states of streptozotocin-induced diabetes, obesity, and starvation, were observed to decrease the expression of myocardial glucose transporters(10–14), thereby leading to a suppression of basal glucose transport (Glut 1) and favoring insulin resistance (Glut 4). In contrast, in adult skeletal muscle, although a decline in Glut 4 occurs, there is no effect upon Glut 1 expression(10, 15). Recent developmental studies in rats demonstrate the predominant presence of Glut 1 over Glut 4 in immature myocardium and skeletal muscle(16, 17). Although some information with respect to the effect of in utero metabolic perturbations upon the regulation of fetal skeletal muscle glucose transporters exists(18–20), no information regarding fetal myocardial glucose transporters is available.
Previous studies investigating the fetal skeletal muscle glucose transporters have used a long-term streptozotocin-induced maternal diabetes model which led to significant intrauterine growth retardation of the fetus(20). Because uteroplacental insufficiency associated with intrauterine growth retardation is known to alter fetal glucose transporter proteins(21), it is essential to examine the effect of maternal diabetes in the absence of any alteration in fetal body weight. Further, because subcellular localization of a glucose transporter isoform determines its ability to transport glucose intracellularly(12), knowledge in this regard is essential. However, no information exists with respect to subcellular localization of glucose transporter isoforms in either fetal skeletal muscle or heart. In the present study, we examined the effect of maternal diabetes upon fetal myocardial glucose transporter protein levels and subcellular localization in comparison with that of the fetal skeletal muscle. This was accomplished by using the previously described streptozotocin-induced short-term diabetic pregnancy rat model, where no substantive change in the fetal body weight is encountered(22), along with quantitative Western blot analysis and immunohistochemical analysis followed by confocal microscopy.
METHODS
Animals. Gestationally timed pregnant Sprague-Dawley rats(Taconic Farm's Inc., Germantown, NY) were housed in individual cages, exposed to 12-h light-dark cycles, and allowed access to standard rat chow (Purina Co., St. Louis, Mo.) ad libitum. As approved by the St. Louis University School of Medicine's Animal Care Committee, the National Institutes of Health guidelines in the care and use of animals were followed. The pregnant animals were allowed at least 1 d of acclimatization before experimental manipulation.
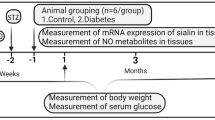
Diabetic pregnancy model. All animals, on d 12-13 of gestation, received either 65 mg/kg streptozotocin (Sigma Chemical Co., St. Louis, MO) that was freshly prepared at the time of administration and kept on ice or an equal volume of vehicle intraperitoneally. Maternal tail vein glucoses were monitored with a One Touch glucose analyzer (Lifescan, Inc., Milpitas, CA), and the animals were divided into three groups based on the glucose values. The vehicle-injected animals demonstrated blood glucoses of less than 10 mM and were assigned to the control group (n = 14). The streptozotocin-injected animals (n = 27) were further divided into two groups. The animals failing to develop overt diabetes were assigned to the STZ-ND (n = 10), and had glucoses <10 mM. This group served as an additional intermediate group that helped to distinguish either the effects of streptozotocin or that of chemical maternal diabetes from the effects of overt maternal diabetes. The rest of the animals that received streptozotocin were found to have glucose levels greater than 13.5 mM, and were assigned to the SEVERE-D (n = 17). There were no animals with glucose values between 10 and 13.5 mM.
All animals continued to feed ad libitum until d 20 of an expected 21-d gestation, when pregnant rats were anesthetized with pentobarbital and subjected to hysterotomy. Maternal blood was collected for plasma glucose and insulin assessments. Urine was checked for ketonuria. Fetal blood was obtained and pooled from single litters for the analysis of plasma glucose and insulin. Plasma glucose levels were analyzed by the glucose oxidase method, and insulin by double antibody RIA(23). Of the total number of litters used in the study, a subset of litters was used for Western blot analysis and a separate subset for immunohistochemical analysis. Maternal and pooled fetal red blood cells, fetal hearts, and skeletal muscle from the fore- and hind limbs were collected, pooled from single litters consisting of 10 pups on an average, and stored at -70°C for protein estimation and Western blot analysis. To obtain adequate amounts of fetal heart or skeletal muscle tissue for Western blot analysis, at times two litters had to be pooled for a single “n,” accounting for the differences in “n” values depicted for protein estimation (Table 1) and Western blot analysis (Figs. 1 and 3). Also, as mentioned above, pooled tissues from a separate subset of litters were obtained for the preparation of cryosections.
Fetal myocardial Western blot analysis. One hundred micrograms of myocardial homogenates prepared from pooled fetal hearts of a single/two litters from vehicle control, STZ-ND, and SEVERE-D experimental groups were resolved on SDS-PAGE and subjected to immunoblotting with 1:500 dilution of the rabbit anti-rat Glut 1 IgG (A) or 1:250 dilution of a rabbit anti-rat Glut 4 IgG (C). The replicate lanes shown represent separate pooled fetal heart samples. A 45-50-kD Glut 1 (A) and a 45-kD Glut 4 (C) protein band are noted. The broad nature of the bands is typical of these glycosylated proteins. One hundred microgrms of fetal rat red blood cell (RBC) homogenate from the vehicle control(C) and the severely diabetic (SD) experimental groups along with adult human red blood cell homogenates (HRBC) were treated with a 1:500 dilution of rabbit anti-rat Glut 1 IgG (B). Densitometric quantitation of fetal myocardial Glut 1 (D) and Glut 4(E) protein bands from vehicle control, STZ-ND, and SEVERE-D groups was performed and the values compared by the one-way ANOVA (p = 0.05 in D and p = 0.0018 in E), and intergroup differences validated by the Neuman Kuel's test (#p < 0.05). The severely diabetic group was compared with the vehicle control group by t test (*p < 0.05) as well.
Fetal skeletal muscle Western blot analysis. One hundred micrograms of fetal skeletal muscle (forelimb, top panel; and hind limb, lower panel) homogenates from vehicle control (C), STZ-ND, and SEVERE-D (A); SEVERE-D (S-D) (B) experimental groups were treated with 1:500 dilution of the rabbit anti-rat Glut 1 IgG(A) or 1:250 dilution of a rabbit anti-rat Glut 4 IgG (B). The replicate lanes for each experimental group represent separate pooled fetal skeletal muscle samples. The 45-50-kD Glut 1 (A) and a 45-kD Glut 4 (B) protein bands are noted. In addition, note larger and smaller Glut 4 immunoreactive bands (B). Radioactivity quantitation of the ≈45-kD fetal skeletal muscle Glut 1 (C) and Glut 4(D) protein bands from vehicle control, STZ-ND, and SEVERE-D groups was performed, and the values compared by the one-way ANOVA (p = 0.001), and intergroup differences validated by the Neuman Kuel's test(#p < 0.05). The severely diabetic group was compared with the vehicle control group by t test (*p < 0.05) as well.
Western blot analysis. From each of the three experimental groups of the diabetic pregnancy model, 100 μg of pooled fetal heart and skeletal muscle homogenates were solubulized in Laemmli's buffer(24). Protein content was determined by the Bradford's dye-binding microassay(25). The samples were then separated by 10% discontinuous SDS-PAGE. The proteins were transferred to nitrocellulose filters by electroblotting, and the filters were subjected to Western blot analysis as described previously(23). The primary antibodies used were 2 μg/mL of a protein A affinity-purified rabbit anti-rat Glut 1-C terminus peptide antibody(23) or rabbit anti-rat Glut 4-C terminus peptide antibody(26). The secondary antibody consisted of an125 I-labeled goat anti-rabbit IgG (ICN, Boston, MA) to allow detection by autoradiography. The autoradiographs were subjected to densitometry (Biomed Instruments, Fullerton, CA), or the radioactivity in the glucose transporter proteins was determined by cutting the nitrocellulose filters in areas corresponding to the autoradiographically detected glucose transporter protein bands and assessing the counts/min incorporated in these strips with a gamma counter (Beckman, Columbia, MD). The glucose transporter band densitometry or radioactivity was standardized for inter-lane loading variability by dividing these values by the OD of a dye-stained internal control protein band present in all lanes. These standardized values were then represented as a percent of the mean of the control values per given blot to overcome interblot variability and to allow assessment of the variability within the control group as a whole.
Immunohistochemical analysis. Fetal myocardium and skeletal muscle (from the fore- and hind limbs) were obtained from the three experimental groups. In addition, certain control adult myocardium and skeletal muscle were obtained. Tissues to be sectioned were immediately rinsed in ice-cold PBS, quick frozen in acetone-dry ice, and stored at -70°C. This frozen tissue was embedded in OCT compound, and 5-μm sections were prepared using a Reichert Frigocut 2800 cryostat, placed on slides coated with 3-aminopropyltriethoxysilane, and allowed to air dry. Sections were initially blocked by incubation with 5% goat serum and 2% BSA in PBS for 15 min at room temperature. For immunolabeling, sections were incubated with either the primary antibodies used for the Western blot analysis or commercially available antibodies. The commercial antibodies consisted of the rabbit polyclonal anti-Glut 1 (1:200) (RaGluTrans, East Acres Biologicals, Southbridge, MA) and the anti-Glut 4 (1:80) antibodies (East Acres Biologicals). Primary antibody incubation occurred for 60 min at room temperature followed by washing with three exchanges of PBS at room temperature for 10 min each. Secondary antibody incubation was carried out for 30 min with fluorescein-conjugated goat anti-rabbit IgG (IgG 1:80) at room temperature for 30 min followed by washing as above. Specificity of the Glut 1 and Glut 4 antibodies was evident in that both rabbit polyclonal antibodies labeled different cell structures (Figs. 2 and 3), indicating lack of reactivity by non-glucose transporter immune components of rabbit sera. For example, compare the distribution of Glut 1 and Glut 4 in Figures 2,A and B,and 4,A and B. Also, our Glut 4 antibody brightly labeled adult skeletal myocytes, wherein Glut 1 staining was almost undetectable (data not shown). Specificity was further confirmed by lack of staining upon incubating with either the Glut 1 or Glut 4 antibody preabsorbed with 1 mg/mL of the respective peptide to which the antibody was raised. After incubation with the secondary antibody and washing, the nuclear DNA was stained with propidium iodide (Sigma Chemical Co.), which has an affinity for DNA and which stains cell nuclei bright orange. The slides were mounted with 90% glycerol in PBS with 1% p-phenylenediamine (Sigma Chemical Co.) to prevent fading. With the use of the confocal microscope(Bio-Rad MRC 600), 1-μm optically sectioned images were obtained. Images were processed with the Bio-Rad software package and reproduced on a Sony laser printer(27).
Fetal myocardial immunohistochemical analysis.(A) Glut 1 immunolocalization (green) in fetal (left panel) and adult (right panel) heart muscles compared by confocal imaging. Glut 1 in adult heart localizes to sarcolemma and intercalated discs with some staining along z-lines (right panel). In fetal tissue, which lacks such ordered structure, Glut 1 appears along the plasma membrane (left panel). The red to yellow staining represents the propidium iodide stained nuclei.(B) Glut 4 immunolocalization (green) in cryosections of fetal (left panel) and adult (right panel) heart muscle prepared and imaged in an identical fashion. Glut 4 which is more abundant in the adult when compared with the fetus by Western blotting, stains brightly along sarcolemma and intercalated discs. In contrast fetal tissue stains weakly and diffusely within cells. (C) Immunohistochemical localization of Glut 1 and Glut 4 in cryosections of fetal cardiac muscle is seen as green staining. Glut 1 staining appears along plasma membranes (top panel), whereas Glut 4 is distributed in a much more diffuse fashion with no apparent membrane localization (lower panel). Nuclei (n) are visible through autofluorescence as evident by their appearance in the absence of Glut 1 or Glut 4 antibody and by bright red staining by propidium iodide which labels DNA. Double immunofluorescent staining of fetal heart cryosection using anti-Glut 1 labeled with FITC-conjugated goat anti-rabbit IgG (green) and mouse anti-neurofilament (D) or anti-α-actin (E) MAb labeled with rhodamine (red). Arrows surround an area of anti-neurofilament staining (rhodamine, red) corresponding to an intracardiac nerve fiber(D) or of α-actin staining (rhodamine, red) corresponding to a blood vessel (E). Nc Glut 1 (FITC staining, green) was evident within or surrounding these areas demonstrating the absence of Glut 1 in the perineural region or in the blood vessels.
Fetal skeletal muscle immunohistochemical analysis. Immunohistochemical localization of Glut 1 (A) and Glut 4(B) in cryosections of fetal skeletal muscle. Glut 1 staining seen in green (and identified by an arrow) appears along plasma membranes(A), whereas Glut 4 also seen in green is distributed in a much more diffuse fashion with no apparent membrane localization (B). Nuclei(n) are visible through autofluorescence as evident by their appearance in the absence of Glut 1 or Glut 4 antibody and by bright red staining by propidium iodide which labels DNA. Double immunofluorescent staining of fetal skeletal muscle cryosection using anti-Glut 1 labeled with FITC-conjugated goat anti-rabbit IgG (green) and mouse anti-neurofilament(C) or anti-α-actin (D) MAb labeled with rhodamine(red). Arrows surround an area of anti-neurofilament staining (rhodamine, red) corresponding to a nerve fiber (C) or α-actin staining(rhodamine, red) corresponding to a blood vessel (D) as evident under phase-contrast. No Glut 1 (seen in the left periphery in C; or above and below the arrows in D) staining (FITC, green) was evident within or surrounding these areas, demonstrating the absence of Glut 1 in the perineural region or in the blood vessels.
Dual immunolabeling. Certain fetal myocardial and skeletal muscle sections were subjected to dual staining(27). Double immunofluorescent labeling was performed by sequential incubation with the rabbit anti-rat Glut 1 (1:200) at room temperature for 30 min followed by mouse anti-rat neurofilament (1:40 dilution) at room temperature for 30 min or mouse anti-rat smooth muscle α-actin (1:200 dilution) at room temperature for 30 min. Secondary antibody incubation was then carried out with both fluorescein-conjugated goat anti-rabbit IgG (1:200 dilution) and rhodamine-conjugated goat anti-murine IgG (1:32 dilution at room temperature for 30 min).
Data analysis. All data presented are expressed as a mean± SEM. All three groups were compared by the one-way ANOVA, and intergroup differences were validated with the Newman Kuel's test. Additionally nonparametric testing was also conducted using Kruskal-Wallis with tied ranks, followed by the Dunn test, to ensure that the conclusions drawn were not skewed due to either small numbers or a heteroscedastic distribution of observations. Using both parametric and nonparametric testing, statistically significant differences between groups were similar. When the SEVERE-D group alone was compared with the vehicle control group, a t test was used.
RESULTS
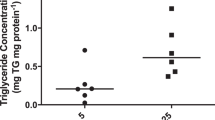
Animal model. Table 1 demonstrates the animal demographics. No significant change in maternal weight, number of pups/litter, or mean fetal weight was noted between the vehicle-treated control, streptozotocin nondiabetic, and severely diabetic groups. Further, no increased fetal loss was observed in either the streptozotocin-diabetic or nondiabetic groups when compared with the vehicle control group. Despite considerable interlitter variability in skeletal muscle mass, the mean hind limb skeletal muscle weight was consistently lower than the corresponding mean forelimb skeletal muscle weight. Further, no significant intergroup differences in mean fetal heart or skeletal muscle weights or protein content were observed. However, the skeletal muscle weight in the severely diabetic group demonstrated a trend toward an increase (Table 1). As per the study design, there were no differences in maternal or fetal glucose concentrations between the control and the STZ-NDs(Table 2). Maternal and fetal insulin values were likewise no different in these two groups (Table 2). In contrast, the SEVERE-D demonstrated a 3-fold increase in maternal and fetal glucose values (Table 2). A 3-fold decline in maternal insulin levels was evident. Typical of this streptozotocin-diabetic pregnancy model(22, 28), despite fetal hyperglycemia no significant change in fetal insulin concentrations was noted(Table 2), although a trend toward an increase existed.
Fetal myocardial glucose transporter concentrations. A modest decrease in Glut 1 protein (≈45-50 kD) band density (Fig. 1A), which translates into a 30% decline upon quantitation, is evident in the severely diabetic group when compared with the vehicle control group (Fig. 1D). To distinguish the fetal myocardial Glut 1 levels from the entrapped red blood cell Glut 1 concentrations, fetal red blood cell Glut 1 protein bands were examined in the vehicle control and the severely diabetic groups and found to be undetectable when compared with the positive control human red blood cells (Fig. 1B). A 45% decline in fetal myocardial Glut 4 protein (≈45 kD) concentrations was observed when compared with the vehicle control group (Fig. 1,C and E). The mean values for the streptozotocin-treated nondiabetic group are intermediate (8% decline, Glut 1; 20% decline, Glut 4) to the vehicle control and the severely diabetic groups. However, in this experimental group, Glut 1 and Glut 4 levels are not statistically different from the vehicle-injected control group, but Glut 1 demonstrates a trend toward a difference, and Glut 4 is significantly different from the severely diabetic group.
Fetal myocardial glucose transporter immunolocalization. Glut 1 localization in the fetal myocardium was distinctly different from Glut 4, the former being plasma membrane-associated, whereas the latter was intracellular (Fig. 2,A-C). Higher amounts of Glut 1 were noted in the fetal myocardium as opposed to the adult, whereas higher amounts of Glut 4 were observed in the adult when compared with the fetal myocardial cells (Fig. 2,A and B). This subcellular distribution of fetal Glut 1 and Glut 4 was no different in the three treatment groups.
Fetal skeletal muscle glucose transporter protein concentrations. Significantly higher amounts of Glut 1 in skeletal muscle obtained from the hind limb when compared with the forelimb was observed (Fig. 3A). Similar differences were not evident with Glut 4 levels (Fig. 3B). A visible decline in Glut 1 concentrations is observed in the severely diabetic group when compared with both the streptozotocin-nondiabetic and the vehicle-treated control groups(50%, forelimb; 65%, hind limb). Again the levels of Glut 1 in the STZ-ND group were intermediate between the vehicle control and the SEVERE-D treatment groups. This intermediacy represented a 15% decline in the forelimb and 30% in the hind limb when compared with the vehicle-treated control, although these differences failed to achieve statistical significance (Fig. 3,A and C). In all three experimental groups, minimal amounts of Glut 4 were noted, warranting longer exposure of the autoradiographs leading to detection of other non-45-kD bands (Fig. 3B). Quantitation of the fore- and hind limb 45-kD Glut 4 protein band revealed no difference between the three groups (Fig. 3D).
Fetal skeletal muscle glucose transporter immunolocalization. Similar to fetal myocardium, plasma membrane-associated (Fig. 4A) and intracellular distribution (Fig. 4B) of Glut 1 and Glut 4 were, respectively, observed in fetal rat skeletal muscle tissue sections as well. Again no difference in this subcellular distribution of glucose transporters was observed between the control, STZ-ND, and SEVERE-D. Unlike the abundant distribution of Glut 1 in perineural sheaths within adult skeletal muscle(29) and pulmonary tissue(30), no Glut 1 immunoreactivity was detected in perineural sheaths within the fetal rat skeletal muscle (Fig. 4C) of any experimental group. In addition, no Glut 1 immunoreactivity was observed in the intraskeletal muscular blood vessels (Fig. 4D).
DISCUSSION
We have demonstrated the presence of both Glut 1 and Glut 4 in the fetal myocardium and skeletal muscle, with Glut 1 being the predominant isoform. This relative distribution contrasts to that in adult tissues(15, 29). The predominance of Glut 1 in the fetal heart and skeletal muscle is instrumental in providing substrate (glucose) under basal metabolic conditions for the growing and developing myocardial and skeletal myocytic cells(16–18). Subcellular distribution of Glut 1 in the fetal myocardium and skeletal muscle is in association with the plasma membrane. This plasma membrane association of Glut 1 in the basal state reiterates the easy availability and the essential role of Glut 1 in providing adequate substrate to fetal tissues. In fetal myocardium, and similar to what has been noted in adult myocardium(27), Glut 1 was not observed in perineural sheaths of neurofilament immunoreactive intracardiac nerves. Interestingly, Glut 1 was also not observed in skeletal muscle perineural sheaths, where in Glut 1 is abundant in adult rats when studied using the identical technique(27). The intracellular distribution of Glut 4 in fetal myocardial and skeletal myocytic cells without evidence of membrane association is markedly different from Glut 1. This suggests a need for either insulin(31, 32), muscle contraction(33, 34), or hypoxia(35–37), in inducing translocation of fetal Glut 4 to the plasma membrane to mediate glucose transport into the fetal myocardium or skeletal muscle. Within the technical limitations of immunodetection, fetal hyperglycemia or maternal diabetes associated metabolic changes did not alter the subcellular distribution of Glut 1 or Glut 4 in either fetal skeletal muscle or myocardium.
Because erythrocytes in the adult human(37) and murine fetus(30) are replete with the Glut 1 protein, it was imperative to demonstrate the contribution of the entrapped fetal red blood cell Glut 1 toward the total myocardial and skeletal muscle Glut 1. By Western blot analysis and immunohistochemistry, fetal rat erythrocytes failed to demonstrate sizeable amounts of Glut 1. This is contrary to our previous observations of Glut 1 expression in fetal murine erythrocytes(30). However, previously in fetal rat brain studies, we were similarly unable to demonstrate Glut 1 immunoreactivity within entrapped red blood cells(38). Thus, the level of expression of Glut 1 in fetal erythrocytes may be species-specific, being high in the human(37), moderate in the mouse(30), and minimal if any in the rat species(38). Thus, a majority of the Glut 1 protein assessed by Western blot analysis arises from the fetal tissue-specific cells being examined.
The effect of streptozotocin-induced maternal diabetes upon fetal myocardial and skeletal muscle glucose transporter protein concentrations was examined in the present investigation. The chemical diabetic pregnancy rat model was chosen to make it feasible to compare the fetal results with previously reported results in the adult diabetic nonpregnant rat(39). Varied dosing of streptozotocin preconceptionally and at earlier gestational ages (0-5 d) has been used by different investigators(20, 28). However, in all cases, administration of streptozotocin in early gestation leads to a severe degree of maternal diabetes with significant compromise to the fetal body weight(20, 28, 40). Based upon previous studies in such a model which demonstrated significant fetal hyperglycemia, hyperinsulinemia, and a pretranslational increase in fetal skeletal muscle Glut 1 expression(20), we carefully chose the present dose and timing of streptozotocin administration to cause minimal fetal loss and minimal compromise to fetal well being, which was reflected as no significant change in fetal body weights. Because streptozotocin was administered during gestation, the chemical could possibly cross the placenta and exert teratogenic effects. However, unlike the early gestational streptozotocin administration model(20), the gestational time frame of drug administration in the present model is beyond the gastrulation and neurulation phases of development, so the chances of fetal teratogenicity are remote.
In this more controlled model of maternal diabetes lasting for a shorter duration of gestation, a certain percentage of rats failed to develop overt diabetes. This could reflect differential absorption of streptozotocin or a selective resistance of the maternal pancreatic β-islet cells to the chemical. Preliminary studies by other groups have demonstrated the presence of subtle abnormalities in the maternal glucose tolerance tests in the STZ-ND which has also been referred to as the mildly diabetic group. Despite these cryptic alterations in the maternal glucose homeostasis, no changes were evident in the fetal glucose and insulin concentrations, and the rate of fetal tissue glucose utilization. Thus, this STZ-ND could potentially serve as an additional group for examination of the fetal effects of streptozotocin alone.
In the severely diabetic group, in addition to maternal hypoinsulinemia and hyperglycemia, significant fetal hyperglycemia with no change in fetal insulin concentrations were noted. The presence of fetal normoinsulinemia in the presence of severe fetal hyperglycemia has previously been reported(41), making the present model highly desirable for examining the isolated effects of either fetal hyperglycemia or other maternal diabetes-induced fetal metabolic changes in the absence of gross fetal insulin perturbations. However, the subtle trend toward an increase in fetal insulin concentrations noted in this group heralds the emergence of fetal insulin resistance.
The decline in fetal myocardial Glut 1 and Glut 4 protein concentrations observed in our present study mimicks the decline previously reported in streptozotocin-treated adult diabetic nonpregnant rats(39), although in the latter the decline was in the range of 65% (Glut 1) to 85% (Glut 4). This exaggerated decline in the adult may reflect the more acute rise in blood glucose and the concomitant decline in insulin concentrations(39) when compared with the observed present changes in the fetus. Further, in the adult, insulin therapy caused an increase in myocardial Glut 4 levels(39), strongly supporting an added insulin effect upon Glut 4. Our present fetal studies demonstrate that fetal hyperglycemia (or other associated metabolic changes) in the absence of a substantive insulin alteration leads to a decline in myocardial Glut 1 and Glut 4 concentrations (Glut 1 < Glut 4), despite myocardial muscle fibers being primarily of the oxidative type in the fully differentiated state.
In contrast to the diabetes-induced changes in myocardial glucose transporters, adult skeletal muscle Glut 4 levels diminish in response to hyperglycemia and hypoinsulinemia(10). This diminution is particularly observed in adult glycolytic as opposed to the oxidative skeletal muscle fibers(10). In our studies, the fetal Glut 1 and Glut 4 changes were similar in both the fore- and hind limb muscle groups examined. This is perhaps related to the fact that, at this stage of development, rat skeletal muscle fails to demonstrate the differentiated phenotype consistent with either the glycolytic or oxidative fibers(42). In the present study, fetal hyperglycemia (or associated metabolic changes) in the absence of associated insulin alterations led to a significant decline (skeletal muscle > myocardial Glut 1) in fore- and hind limb skeletal muscle-plasma membrane-associated Glut 1 levels. In contrast, minimal levels of Glut 4 are observed in fetal fore- and hind limb skeletal muscle when compared with fetal myocardium, and no significant decline in Glut 4 is observed. Our present observations contrast previous observations of a pretranslational increase in fetal rat skeletal muscle Glut 1 levels in response to streptozotocin-induced severe and prolonged maternal diabetes(20). This difference may stem from the fact that, in this previously reported model, significant intrauterine growth retardation and fetal hyperinsulinemia were observed, both of which could potentially modify the in vivo effect of fetal hyperglycemia upon the expression and levels of fetal skeletal muscle Glut 1 concentrations(21).
In summary, Glut 1, the plasma membrane-associated isoform, is the predominant fetal myocardial and skeletal muscle glucose transporter when compared with Glut 4, the intracellular form. Streptozotocin-induced maternal diabetes leading to fetal hyperglycemia with normoinsulinemia causes a decrease in fetal myocardial and skeletal muscle Glut 1 and fetal myocardial Glut 4 protein levels. The decline in Glut 1 may serve a protective mechanism in preventing excessive entry of glucose into the developing insulin-responsive tissues (skeletal muscle > myocardium). The functional significance of a decrease in the intracellular fetal myocardial Glut 4 protein levels remains unknown. This in utero decline in myocardial Glut 4 concentrations in association with the existing low levels of Glut 4 in skeletal muscle may herald the emergence of insulin resistance.
Abbreviations
- Glut 1:
-
glucose transporter isoform 1
- Glut 4:
-
glucose transporter isoform 4
- SEVERE-D:
-
streptozotocin-treated severely diabetic group
- STZ-ND:
-
streptozotocin-treated nondiabetic group
- ANOVA:
-
analysis of variance
References
Clark CM Jr 1971 Carbohydrate metabolism in the isolated fetal rat heart. Am J Physiol 220: 583–588.
Lueder FL, Ogata ES 1990 Uterine artery ligation in the maternal rat alters fetal tissue glucose utilization. Pediatr Res 28: 464–468.
Amatayakul O, Cumming GR, Hawarth JC 1970 Association of Hypoglycemia with cardiac enlargement and heart failure in newborn infants. Arch Dis Child 45: 717–720.
Gutgesell HP, Mullins CE, Gillette PG, Speer M, Rudolph AJ, McNamara DG 1976 Transient hypertrophic subaortic stenosis in infants of diabetic mothers. J Pediatr 89: 120–123.
Hay WW, Meznarich HK, DiGiacomo JE, Hirst K, Zerbe G 1988 Effects of insulin and glucose concentrations on glucose utilization in fetal sheep. Pediatr Res 23: 381–387.
Ren J-M, Marshall BA, Gulve EA, Gao J, Johnson DW, Holloszy JO, Mueckler M 1993 Evidence from transgenic mice that glucose transport is rate-limiting for glycogen deposition and glycolysis in skeletal muscle. J Biol Chem 268: 16113–16115.
Opies LHK, Mansford RL, Owen P 1971 Effects of increased heart work and glycolysis and adenine nucleotides in the perfused heart of normal and diabetic rats. Biochem J 124: 475–490.
Devaskar SU, Mueckler M 1992 The mammalian glucose transporters. Pediatr Res 31: 1–13.
Bell GI, Burant CF, Takeda J, Gould GW 1993 Structure and function of mammalian facilitative sugar transports. J Biol Chem 268: 19161–19164.
Kainulainen H, Breiner M, Schurmann A, Marttinen A, Virjo A, Joost HG 1994 In vivo glucose uptake and glucose transporter proteins Glut 1 and Glut 4 in heart and various types of skeletal muscle from streptozotocin-diabetic rats. Biochim Biophys Acta 1225: 275–282.
Camps M, Castello A, Munoz P, Monfar M, Testar X, Palacin M, Zorzano A 1992 Effect of diabetes and fasting on Glut 4(muscle/fat) glucose transporter expression in insulin-sensitive tissues. Biochem J 282: 765–772.
Kraegen EW, Sowden JA, Halstead MB, Clark PW, Rodnick KJ, Chisholm DJ, James DE 1993 Glucose transporters and in vivo glucose uptake in skeletal and cardiac muscle: fasting, insulin stimulation and immunoisolation studies of Glut 1 and Glut 4. Biochem J 295: 287–293.
Woloschak M, Shen-Orr Z, LeRoith D, Roberts CT Jr 1993 Nutritional regulation of insulin-sensitive glucose transporter gene expression in rat cardiac muscle. Proc Soc Exp Biol Med USA 203: 172–174.
Machado UF, Shimizu Y, Saito M 1993 Decreased glucose transporter (Glut 4) content in insulin-sensitive tissues of obese aurothioglucose- and monosodium glutamate-treated mice. Horm Metab Res 25: 462–465.
Garvey WT, Huecksteadt TP, Birnbaum MJ 1989 Pretranslational suppression of an insulin-responsive glucose transporter in rats with diabetes mellitus. Science 245: 60–63.
Santalucia T, Camps M, Castell A, Munoz P, Nuel A, Testar X, Palacin M, Zorzano A 1992 Developmental regulation of Glut 1(erythroid/Hep G2) and Glut 4 (muscle/fat) glucose transporter expression in rat heart, skeletal muscle, and brown adipose tissue. Endocrinology 130: 837–846.
Postic C, Leturque A, Printz RL, Maulard P, Loizeau M, Granner DK, Girard J 1994 Development and regulation of glucose transporter and hexokinase expression in rat. Am J Physiol 266:E548–E559.
Guillet-Deniau I, Leturque A, Girard J 1994 Expression and cellular localization of glucose transporters (Glut 1, Glut 3, Glut 4) during differentiation of myogenic cells isolated from rat foetuses. J Cell Sci 107: 487–496.
Simmons RA, Flozak AS, Ogata ES 1993 Glucose regulates Glut 1 function and expression in fetal rat lung and muscle in vitro. Endocrinology 132: 2312–2318.
Atkins V, Flozak AS, Ogata ES, Simmons RA 1994 The effects of severe maternal diabetes on glucose transport in the fetal rat. Endocrinology 135: 409–415.
Simmons RA, Flozak AS, Ogata ES 1993 The effect of insulin and insulin-like growth factor-1 on glucose transport in normal and small for gestational age fetal rats. Endocrinology 259: 1361–1368.
Devaskar S, Holtzclaw L, Sadiq F 1988 The heterogeneity of the developing brain insulin receptor. Pediatr Res 24: 683–692.
Schroeder RE, Devaskar UP, Trail SE, deMello DE, Cole DP, Devaskar SU 1993 Effect of maternal diabetes on the expression of genes regulating fetal brain glucose uptake. Diabetes 42: 1487–1496.
Laemmli UK 1970 Cleavage of structural proteins during assembly of the head bacteriophage T4. Nature 227: 680–685.
Bradford MM 1976 A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem 72: 248–254.
Haney PM, Slot JW, Piper RC, James DE, Mueckler MM 1991 Intracellular targeting of the insulin-regulatable glucose transporter (Glut 4) is isoform specific and independent of cell type. J Cell Biol 114: 689–699.
Doria-Medina CL, Lund DD, Pasley A, Sandra A, Sivitz WI, 1993 Immunolocalization of Glut-1 glucose transporter in rat skeletal muscle and in normal and hypoxic cardiac tissue. Am J Physiol E454–E464
Gewolb IH, Barrett C, Wilson CM, Warshaw JB 1982 Delay in pulmonary glycogen degradation in fetuses of streptozotocin diabetic rats. Pediatr Res 16: 869–873.
Handberg AL, Kayser PE, Hoyer PE, Vinten J 1992 A substantial part of Glut 1 in crude membranes from muscle originates from perineural sheaths. Am J Physiol 262:E721–E727.
Mantych G, Devaskar U, deMello De, Devaskar SU 1991 Glut 1 glucose transporter protein in adult and fetal mouse lung. Biochem Biophys Res Commun 180: 367–373.
Rodnick KJ, Slot JW, Studelska DR, Hanpeter DE, Robinson LJ, Geuze HJ, James DE 1992 Immunocytochemical and biochemical studies of Glut 4 in rat skeletal muscle. J Biol Chem 267: 6278–6285.
Slot JW, Gueze HJ, Gigengack S, James DE, Leinhard GE 1991 Translocation of the glucose transporter Glut 4 in cardiac myocytes of the rat. Proc Natl Acad Sci USA 88: 7815–7819.
Douen AG, Ramlal T, Rastogi S, Bilan PJ, Cartee GD, Vranic M, Holloszy JO, Klip A 1990 Exercise induces recruitment of the insulin-responsive glucose transporter. Evidence for distinct intracellular insulin- and exercise-recruitable transporter pools in skeletal muscle. J Biol Chem 265: 13427–13430.
Kolter T, Uphues I, Wichelhaus A, Reinauer H, Eckel J 1992 Contraction-induced translocation of the glucose transporter Glut 4 in isolated ventricular cardiomyocytes. Biochem Biophys Res Commun 189: 1207–1214.
Sivitz WI, Lund DD, Yorek B, Grover-McKay M, Schmid PG 1992 Pretranslational regulation of two cardiac glucose transporters in rats exposed to hypobaric hypoxia. Am J Physiol 263:E562–E569.
Bashan N, Burdett E, Hundal HS, Klip A 1992 Regulation of glucose transport and Glut 1 glucose transporter expression by O2 in muscle cells in culture. Am J Physiol 262:C682–C690.
Mueckler M, Caruso C, Baldwin SA, Panico M, Blench I, Morris HR, Allard WJ, Leinhard GE, Lodish HF 1985 Sequence and structure of a human glucose transporter. Science 229: 941–945.
Devaskar S, Zahm DS, Holtzclaw L, Chundu K, Wadzinski BE 1991 Developmental regulation of the distribution of rat brain insulin-insensitive (Glut 1) glucose transporter. Endocrinology 129: 1530–1540.
Garvey WT, Hardin D, Juhaszova M, Dominguez JH 1993 Effects of diabetes on myocardial glucose transport system in rats: implications for diabetic cardiomyopathy. Am J Physiol 264:H837–H844.
Guttentag SH, Phelps DS, Warshaw JB, Floros J 1992 Delayed hydrophobic surfactant protein (SP-B, SP-C) expression in fetuses of streptozotocin-treated rats. Am J Respir Cell Mol Biol 9: 190–197.
Bihoreau M-T, Ktorza A, Kervran A, Picon L 1986 Effect of gestational hyperglycemia on insulin secretion in vivo and in vitro by fetal rat pancreas. Am J Physiol 251:E86–E91.
Kelly AM, Rosser BWC, Hoffman R, Panettieri RA, Schiaffino S, Rubinstein NA, Nemeth PM 1991 Metabolic and contractile protein expression in developing rat diaphragm muscle. J Neurosci 11: 1231–1242.
Acknowledgements
We thank Dr. M. Mueckler, Washington University School of Medicine, St. Louis, MO, for the generous gift of the rabbit anti-rat Glut 1 and anti-rat Glut 4 antibodies that were used in the Western blot analyses, and some of the immunohistochemical analyses.
Author information
Authors and Affiliations
Additional information
Supported by the American Diabetes Association (S.U.D.), the National Institutes of Health HD-25024 (S.U.D.), and DK-25295 (W.I.S.), and American Heart Association 93012980 (W.I.S.). R.E.S. was a recipient of the American Heart Association-Missouri Affiliate Fellowship Award.
Presented in part in an abstract form at the Society for Pediatric Research held in 1993 in Washington, D.C.
Rights and permissions
About this article
Cite this article
Schroeder, R., Doria-Medina, C., Das, U. et al. Effect of Maternal Diabetes upon Fetal Rat Myocardial and Skeletal Muscle Glucose Transporters. Pediatr Res 41, 11–19 (1997). https://doi.org/10.1203/00006450-199701000-00002
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199701000-00002
This article is cited by
-
Regulation of Cardiac Energy Metabolism in Newborn
Molecular and Cellular Biochemistry (2006)