Abstract
We studied the effects of exogenously administered adrenomedullin on fetal pulmonary arterial blood flow in near-term fetal sheep. The hemodynamic effects of a single injection of adrenomedullin into the left pulmonary artery were compared with those of acetylcholine; the effects of repeated injections of adrenomedullin were also studied. In seven unanesthetized fetal sheep, catheters were inserted into the left pulmonary artery to administer drugs, and into the main pulmonary and carotid arteries to measure pressures. An ultrasonic flow transducer was placed around the left pulmonary artery to measure flow continuously. A single 5-μg injection of adrenomedullin (1.90± 0.35 μg/kg of fetal weight) increased pulmonary arterial blood flow significantly, from 17 ± 10 to 120 ± 21 mL/min (p< 0.001). Two micrograms of acetylcholine (0.74 ± 0.14 μg/kg of fetal weight) also increased left pulmonary arterial blood flow, from 18± 16 to 113 ± 37 mL/min, but the effect of adrenomedullin on flow was more prolonged than was that of acetylcholine. Additionally, adrenomedullin and acetylcholine similarly decreased mean pulmonary arterial pressure by 11 and 16%, respectively, but adrenomedullin did not decrease mean carotid arterial pressure to the same degree as acetylcholine (2versus 19%, respectively). Five sequentially repeated injections of adrenomedullin, once every 5 min, increased left pulmonary arterial blood flow significantly in a stepwise manner without significantly changing heart rate or mean pulmonary and carotid arterial pressures. We conclude that exogenously administered adrenomedullin is a pulmonary vasodilator in fetal sheep and has the ability to increase pulmonary blood flow significantly; there is less effect on the systemic circulation. This finding might be important in considering the therapeutic use of this peptide in the management of persistent pulmonary hypertension in the perinatal period.
Similar content being viewed by others
Main
Pulmonary blood flow is low in the normal fetus and, with the onset of pulmonary ventilation at birth, increases approximately 8-10-fold due to a rapid fall in pulmonary vascular resistance(1, 2). The mechanisms involved in this dramatic change in the pulmonary circulation, however, have not been fully elucidated. Previous experimental studies have shown that the low pulmonary blood flow in the fetus can be increased by mechanical factors or by administration of various vasoactive factors. Mechanical factors, such as lung distention, probably increase pulmonary blood flow through the cyclooxygenase pathway and the stimulation of prostacyclin production(3–5), whereas K+ channel activation or vasoactive factors, such as ATP, acetylcholine, or bradykinin, probably increase flow through receptor-mediated stimulation of nitric oxide production(6–12). These phenomena are important in considering the normal increase in pulmonary blood flow during the transitional period.
Adrenomedullin is a peptide recently isolated from extracts of human pheochromocytoma tissue(13). Recent studies have revealed that adrenomedullin also is found in several peripheral tissues, including the adrenal glands, kidney, and lung, and that this peptide has a potent and long-lasting hypotensive effect(13–17). Further studies demonstrated that exogenously administered adrenomedullin induced pulmonary vasodilatation and an increase of pulmonary blood flow in adult rats and cats in which pulmonary blood flow had been decreased by exogenously administered vasoconstrictors(18–20). These observations suggested that this peptide may play an important hormonal role in the regulation of pulmonary vascular tone and regional blood flow in the adult, and we have speculated that adrenomedullin also may play a role in the transitional changes in pulmonary blood flow. However, the effects of adrenomedullin on the fetal pulmonary circulation have not been examined yet. Therefore, the goal of this study was to determine whether exogenously administered adrenomedullin has any effect on pulmonary blood flow in the chronically instrumented sheep fetus.
METHODS
Animals. Seven mixed Western pregnant sheep were studied at 125-127-d gestational age (full term is about 145 d). Animal husbandry and the study design followed the guidelines of the National Institutes of Health and were approved by the Committee on Animal Research of the University of California, San Francisco.
Surgical preparation. The surgical preparation has been described in detail previously(2, 5, 6). Briefly, under ketamine anesthesia, a midline laparotomy was performed on the ewe, and the fetus was exposed through a small uterine incision. After administering local lidocaine anesthesia to the fetus, a skin incision was made in the fetal forelimb, and catheters were advanced into the ascending aorta from the brachial artery and into the superior vena cava from the brachial vein, respectively. The incision was then closed, and a new incision was made over the left chest of the fetus. After a left thoracotomy, a catheter was advanced into the ascending aorta from the internal mammary artery. After the pericardium was opened, catheters were inserted directly into the main and left pulmonary arteries. Formalin (10%) colored with a few drops of sterile indigo carmine solution was infiltrated into the adventitia and media of the ductus arteriosus to prevent vasoactivity during the subsequent experimental protocol(21). For continuous measurement of left pulmonary arterial blood flow, a 4-6-mm ultrasonic transit time Doppler flow transducer was placed around the left pulmonary artery. The thoracotomy and fetal skin were closed. After antibiotics were instilled, amniotic fluid losses were replaced with warm saline. A catheter was placed in the amniotic cavity, then the uterine incision was closed. All vascular catheters were filled with heparin, sealed, and exteriorized to the left flank of the ewe with the transducer cable. The laparotomy was closed in layers, and the ewe was returned to the cage for recovery. Antibiotics were administered daily i.v. to the ewe and into the amniotic cavity.
Experimental protocol. We performed experiments 1 or 2 d after surgery. The ewe was placed in a study cage and allowed free access to alfalfa pellets and water during experiments. After a steady period of at least 20 min, 2 μg of acetylcholine (Miochol, Iolab Pharmaceuticals, Clairmont, CA) were injected initially as a bolus (over about 5 s) into the left pulmonary artery to confirm normal vasoactivity of the pulmonary vascular bed in response to a stimulus mediated through endothelial cell nitric oxide production(8, 11). After left pulmonary arterial blood flow and pulmonary arterial pressures had returned to baseline values, 5μg of adrenomedullin (Bachem California, Torrance, CA) were injected as a bolus (over about 5 s) into the left pulmonary artery. This injection of 5μg of adrenomedullin was then repeated every 5 min for a total of five injections (first injection = time 0 min; second injection = time 5 min; and so forth). Hemodynamic variables were measured throughout the experiment, and blood gas samples were obtained before and after each experiment. Upon completion of the experiment, the ewe was killed by injection of an overdose of sodium pentobarbital. After removing the fetus from the uterus, we measured fetal body weight, checked catheter positions, and examined the lungs macroscopically.
Hemodynamic measurements. We measured left pulmonary arterial blood flow, phasic and mean systemic and pulmonary arterial blood pressures, and heart rate. Left pulmonary arterial blood flow was measured continuously with an ultrasonic flow transducer and flow meter (Transonic Systems, Ithaca, NY). Vascular catheters connected to Statham P23Db strain-gauge transducers(Statham Instruments, Oxnard, CA) were used to measure phasic and mean systemic and pulmonary arterial blood pressures. Additionally, heart rate was obtained using a cardiotachometer triggered by the phasic pulmonary arterial pressure tracing. All these variables were recorded continuously on a direct writing polygraph (Gould, Inc., Cleveland, OH). Blood samples were obtained from the carotid artery for determination of pH, Pco2, and Po2(Corning 158 Blood Gas Analyzer, Corning Medical, Medfield, MA) and of Hb concentration and oxygen saturation (OSM2 hemoximeter, Radiometer, Copenhagen, Denmark).
Data collection and analysis. Each experiment included two analyses: 1) the hemodynamic effects of the first injection of adrenomedullin, compared with the acetylcholine injection, and 2) the prolonged effects of adrenomedullin associated with the five repeated injections. For the comparison between the initial injections of acetylcholine and adrenomedullin, data were acquired at three points: 1) immediately before injection (baseline data), 2) at the point of maximal response in left pulmonary arterial blood flow, and 3) 5 min after the injection. To evaluate the significance in these hemodynamic changes, we used the paired sample t test. In the analysis of the repeated injections of adrenomedullin, data were acquired 5 min after each sequential injection of adrenomedullin; the significance of the changes in these hemodynamic variables was determined by simple regression analysis. Changes in blood gases before and after the experiment were assessed by paired sample t test. We considered statistical significance present when p < 0.05. Data are presented as mean ± 1 SD except for those presented as a box plot.
RESULTS
Fetal body weight ranged from 2200 to 3800 g (median: 2600 g), and the macroscopic lung examination revealed no evidence of hemorrhage. Fetal blood gases before and after the experiments are summarized in Table 1. Paired analysis showed a significant decrease in pH and Hb after the experiments.
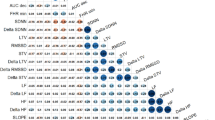
We found that exogenously administered adrenomedullin (5 μg) significantly increased fetal left pulmonary arterial blood flow in all seven fetal sheep. Changes in left pulmonary arterial blood flow with the first injections of adrenomedullin or acetylcholine (2 μg) are shown in Figure 1; the variables are summarized in Table 2. After the first adrenomedullin injection, left pulmonary arterial blood flow increased significantly from baseline, and similar changes were observed with acetylcholine; however, the patterns of return toward baseline flow after 5 min were quite different. With acetylcholine, left pulmonary arterial blood flow decreased to baseline well before 5 min, whereas with adrenomedullin, flow decreased more slowly after reaching the maximum point and was still significantly higher than baseline after 5 min (p < 0.05). These changes in pulmonary blood flow were accompanied by significant changes in mean pulmonary arterial blood pressure. After the initial adrenomedullin injection, mean pulmonary arterial blood pressure decreased significantly, then returned to baseline after 5 min. A similar trend was observed with acetylcholine; however, the fall from baseline did not reach statistical significance (Table 1). Adrenomedullin induced a smaller decrease in mean carotid arterial blood pressure than acetylcholine, 2 versus 19%, respectively. Heart rate increased significantly after adrenomedullin, but decreased after acetylcholine.
Box plot showing the 10th, 25th, 50th (median), 75th, and 90th percentiles of left pulmonary blood flow before (baseline value), at maximal response, and 5 min after a single injection of 5 μg of adrenomedullin or 2 μg of acetylcholine. Values above the 90th and below the 10th percentile are shown as circles. *p < 0:05,**p < 0.001. LPA, left pulmonary artery.
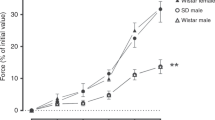
Repeated bolus injections of 5 μg of adrenomedullin every 5 min produced a stepwise increase in left pulmonary arterial blood flow (Fig. 2). As shown in Figure 2, for the first four of the sequential injections, the magnitude of absolute increase in flow after each injection was similar; only after the final injection was this blunted as an overall maximal vasodilatation appeared to have been achieved. The duration and pattern of response were similar between injections. No tachyphylaxis was observed. After the fifth injection of adrenomedullin, left pulmonary arterial blood flow returned to baseline within 90-120 min. The results of the regression analyses of the variables measured at five time points (immediately before the 2nd, 3rd, 4th, and 5th injections and 5 min after the 5th injection) are shown in Figure 3. There was a significant linear increase only in left pulmonary arterial blood flow associated with the five injections of adrenomedullin (p < 0.001, r = 0.74, y = 12.3 + 4.6x), and no significant changes were found in heart rate, pulmonary arterial blood pressure, or carotid arterial blood pressure: heart rate, r = 0.24,y = 202 + x; pulmonary arterial blood pressure,r = 0.19, y = 53 + 0.1x; carotid arterial pressure, r = 0.20, y = 47 - 0.2x. With repeated injections of acetylcholine, even when given closer together, flow always returned to baseline, generally within 2-3 min each time.
Example of the stepwise increase in left pulmonary arterial blood flow after five sequential bolus injections of 5 μg of adrenomedullin, given at 5-min intervals. Left pulmonary arterial(LPA) blood flow was assessed every 5 s for 5 min after each injection. •, First injection; ○, second injection 5 min after the first; ▪, third injection 10 min after the first; □, fourth injection 15 min after the first; ▴, fifth injection 20 min after the first.
DISCUSSION
In adults, the peptide adrenomedullin has been shown to produce pulmonary(18–20) as well as systemic vasodilatation(13–17). The exact mechanism by which the pulmonary vasodilatation occurs is unclear, although in perfused adult rat lungs, Heaton et al.(20) were unable to find any role for cyclooxygenase products, endothelium-derived relaxing factor, ATP-dependent K+ channels, or a variety of other known vasoactive systems. They suggested that adrenomedullin might represent a novel regulatory peptide in the lung.
In our intact fetal lambs, exogenously administered adrenomedullin also markedly increased left pulmonary arterial blood flow and decreased pulmonary arterial blood pressure. In previous studies in fetal animals, various vasoactive factors such as acetylcholine, ATP, bradykinin, or K+ channel activation, have been shown to decrease pulmonary vascular resistance and increase pulmonary flow(6–11). Our study demonstrates that the novel peptide, adrenomedullin, should be added to this list, although the underlying mechanisms involved are not yet established and remain purely speculative. These include the role of endothelial-derived nitric oxide release with subsequent activation of a cGMP-mediated pathway, a cAMP-mediated effect, stimulated possibly by a specific receptor-activated phenomenon or an ATP-sensitive K+ channel-mediated mechanism. The role of endothelin acting via the endothelin receptor, type B, also is a consideration.
Pulmonary blood flow is determined mainly by pulmonary vascular resistance, heart rate, and right ventricular stroke volume. Although adrenomedullin increased fetal left pulmonary arterial blood flow nearly 10-fold, heart rate increased less than 20%. Also, previous studies have demonstrated the limited ability of fetal lambs to increase stroke volume(22, 23). Therefore, in the present study, the main determinant of the increase in fetal pulmonary blood flow appears to be a significant decrease in pulmonary resistance after adrenomedullin injection. This was confirmed in two animals in which we placed a left atrial catheter and thus were able to calculate pulmonary vascular resistance. In these, pulmonary vascular resistance fell from 4.5 mm Hg/mL/min to 0.4 mm Hg/mL/min in one, and from 3.5 mm Hg/mL/min to 0.5 mm Hg/mL/min in the second.
Acetylcholine decrease pulmonary vascular resistance and increases blood flow in fetal lambs, probably through endothelium-dependent vasodilatation(8). In this study, adrenomedullin and acetylcholine similarly decreased mean pulmonary arterial blood pressure and increased left pulmonary arterial blood flow. However, the patterns of increasing flow and of hemodynamic changes were not same. Five minutes after the acetylcholine injection, left pulmonary arterial blood flow was completely restored to baseline; however, at the same time point after adrenomedullin injection, left pulmonary arterial blood flow was still significantly higher than baseline (Fig. 1). This indicates the potent and prolonged effect of adrenomedullin on the fetal pulmonary circulation, an effect quite similar to that found in previous studies in adult animals, both in vivo and in vitro(13, 14, 16). Likewise, as we have shown previously(11), heart rate decreased slightly after acetylcholine infusion, but increased transiently after adrenomedullin infusion, which might indicate that adrenomedullin has chronotropic actions in the fetus. Furthermore, it was interesting that adrenomedullin did not alter mean carotid arterial blood pressure whereas acetylcholine decreased it nearly 20%. Thus adrenomedullin appears to have less of a systemic hypotensive effect than acetylcholine when injected into the pulmonary circulation.
With repeated injections of adrenomedullin, left pulmonary arterial blood flow increased significantly in a stepwise manner, whereas heart rate and mean pulmonary and carotid arterial blood pressures showed no significant change (Fig. 3). The mechanism of this prolonged effect is not clear, but we speculate that it could be explained by the existence of at least two different types of adrenomedullin receptors, perhaps with different affinities. For example, with relatively low plasma concentrations of adrenomedullin, the effect could be mediated by a receptor with high affinity but a short duration of action, whereas above a given concentration, another receptor could be activated with a lower affinity but a more prolonged response. Other possibilities include either activation of enzymes involved in the production of factors that produce vasodilatation, such as endothelial nitric oxide synthase or endothelin-converting enzyme, or inhibition of enzymes that break down the products responsible for vasodilatation, such as phosphodiesterase V, which metabolizes cGMP. Further studies are needed to elucidate the underlying mechanisms of these increases in pulmonary blood flow.
Blood gas analysis showed a small but significant decrease in pH and Hb concentration after the experiments. In the fetal circulation, a continuous increase in pulmonary blood flow may be associated with a decrease of blood flow through the ductus arteriosus with resultant poor perfusion of postductal areas, particularly the placenta. Thus the decrease of pH might indicate a hypoxic metabolic response. Macroscopic investigation of the lungs after the experiments showed no signs of pulmonary hemorrhage to account for possible effects on pH. The decrease in Hb probably is due to dilution both by the repeated injections of adrenomedullin and by normal saline used to flush the catheters.
Two of the fetuses had hypoxic blood gas conditions before the experiments, with the lowest O2 saturation being 30.6% (Table 1). As these fetuses showed no apparent abnormality or differences in responses during the experiments, they were pooled with the others. However, analysis of the effect of adrenomedullin on the hypoxic fetus is a separate issue, which requires a different study design.
In summary, exogenously administered adrenomedullin produces an enormous increase in pulmonary blood flow and decreases mean pulmonary arterial blood pressure in fetal sheep, with less of a hypotensive effect on the systemic circulation. Because this peptide has been found in human lungs and plasma, it could play a physiologic role in the dramatic increase in pulmonary blood flow that occurs shortly after birth. Therefore, these findings may be important in considering therapy for cardiopulmonary adaptation failure in the perinatal period, as in the persistent pulmonary hypertension syndrome of the newborn.
References
Heymann MA, Soifer SJ 1989 Control of the fetal and neonatal pulmonary circulation. In: Weir EK, Reeves JT (eds) Pulmonary Vascular Physiology and Pathophysiology. Marcel Dekker, New York, pp 33–50
Teitel DF, Iwamoto HS, Rudolph AM 1990 Changes in the pulmonary circulation during birth-related events. Pediatr Res 27: 372–378
Cassin S, Dawes GS, Mott JC, Ross BB, Strang LB 1964 The vascular resistance of the foetal and newly ventilated lung of the lamb. J Physiol (Lond) 171: 61–79
Leffler CW, Hessler JR, Green RS 1984 Mechanism of stimulation of pulmonary prostacyclin synthesis at birth. Prostaglandins 28: 877–887
Velvis H, Moore P, Heymann MA 1991 Prostaglandin inhibition prevents the fall in pulmonary vascular resistance as a result of rhythmic distension of the lungs in fetal lambs. Pediatr Res 30: 62–68
Heymann MA, Rudolph AM, Nies AS, Melmon KL 1969 Bradykinin production associated with oxygenation of the fetal lamb. Circ Res 25: 521–534
Abman SH, Chatfield BA, Hall SL, McMurtry IF 1990 Role of endothelium-derived relaxing factor during transition of pulmonary circulation at birth. Am J Physiol 259:H1921–H1927
Tiktinsky MH, Cummings JJ, Morin FC 1992 Acetylcholine increases pulmonary blood flow in intact fetuses via endothelium-dependent vasodilation. Am J Physiol 262:H406–H410
Glasgow RE, Heymann MA 1990 Endothelium-derived relaxing factor as a mediator of bradykinin-induced perinatal pulmonary vasodilatation. Clin Res 38: 211A( abstr)
Konduri GG, Gervasio CT, Theodorou AA 1993 Role of adenosine triphosphate and adenosine in oxygen-induced pulmonary vasodilation in fetal lambs. Pediatr Res 33: 533–539
Chang J-K, Moore P, Fineman JR, Soifer SJ, Heymann MA 1992 K+ channel pulmonary vasodilatation in fetal lambs: role of endothelial derived nitric oxide. J Appl Physiol 73: 188–194
Moore P, Velvis H, Fineman JR, Soifer SJ, Heymann MA 1992 EDRF inhibition attenuates the increase in pulmonary blood flow due to oxygen ventilation in fetal lambs. J Appl Physiol 73: 2151–2157
Kitamura K, Kangawa K, Kawamoto M, Ichiki Y, Nakamura S, Matsuo H, Eto T 1993 Adrenomedullin: a novel hypotensive peptide isolated from human pheochromocytoma. Biochem Biophys Res Commun 192: 553–560
Ishiyama Y, Kitamura K, Ichiki Y, Nakamura S, Kida O, Kangawa K, Eto T 1993 Hemodynamic effects of a novel hypotensive peptide, human adrenomedullin, in rats. Eur J Pharmacol 241: 271–273
Nishikimi T, Kitamura K, Saito Y, Shimada K, Ishimitsu T, Takamiya M, Kangawa K, Matsuo H, Eto T, Omae T, Matsuoka H 1994 Clinical studies on the sites of production and clearance of circulating adrenomedullin in human subjects. Hypertension 24: 600–604
Gardiner SM, Kemp PA, March JE, Bennett T 1995 Regional haemodynamic effects of human and rat adrenomedullin in conscious rats. Br J Pharmacol 114: 584–591
Parkes DG 1995 Cardiovascular actions of adrenomedullin in conscious sheep. Am J Physiol 268:H2574–H2578
Lippton H, Chang JK, Hao Q, Summer W, Hyman AL 1994 Adrenomedullin dilates the pulmonary vascular bed in vivo. J Appl Physiol 76: 2154–2156
Cheng DY, DeWitt BJ, Wegmann MJ, Coy DH, Bitar K, Murphy WA, Kadowitz PJ 1994 Synthetic human adrenomedullin and ADM 15-52 have potent short-lasting vasodilator activity in the pulmonary vascular bed of the cat. Life Sci 55: PL251–256
Heaton J, Lin B, Chang J-K, Steinberg S, Hyman A, Lippton H 1995 Pulmonary vasodilation to adrenomedullin: a novel peptide in humans. Am J Physiol 268:H2211–H2215
Rudolph AM, Heymann MA, Fishman N, Lakier JB 1975 Formalin infiltration of the ductus arteriosus: a method for palliation of infants with selected congenital cardiac lesions. N Engl J Med 292: 1263–1268
Friedman WF 1972 The intrinsic physiologic properties of the developing heart. Prog Cardiovasc Dis 15: 87–111
Thornburg KL, Morton MJ 1986 Filling and arterial pressures as determinants of left ventricular stroke volume in fetal lambs. Am J Physiol 251:H961–H968
Acknowledgements
The authors thank Julien Hoffman, M.D., for statistical consultation. We also acknowledge the expertise and assistance of Mario Trujillo, Bruce D. Payne, and Paul Sagan.
Author information
Authors and Affiliations
Additional information
Supported by U.S. Public Health Service Grant HL 40473.
Rights and permissions
About this article
Cite this article
De Vroomen, M., Takahashi, Y., Gournay, V. et al. Adrenomedullin Increases Pulmonary Blood Flow in Fetal Sheep. Pediatr Res 41, 493–497 (1997). https://doi.org/10.1203/00006450-199704000-00007
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199704000-00007