Abstract
To verify some animal experimental results in humans, we have studied urinary epidermal growth factor (EGF) excretion in normal children as well as children with acute renal failure (ARF). Urinary EGF excretion was expressed as a ratio of urinary EGF to urinary creatinine concentration (EGF/Cr) for random and 24-h urine, and a daily total urinary EGF for 24-h urine. The highest urinary EGF/Cr in children was found at 1 mo to 3 y of age. There was a highly significant correlation between random urine EGF/Cr and 24-h urine EGF/Cr (r = 0.92, p < 0.001), whereas no correlation of urinary EGF/Cr with daily total urine EGF was found. During the course of ARF, a decline in urinary EGF/Cr from the period before peak serum creatinine to the period after the declination of serum creatinine was noted (p = 0.013, n = 13, by repeated measure analysis), with a constant low daily total urine EGF (p value not significant). However, a rise in both urinary EGF/Cr and daily total urine EGF was found between the period of serum creatinine decline and the period of completely normal serum creatinine(p < 0.001). Serum EGF remained unchanged throughout the course of ARF. These results suggest 1) the possible role of EGF in renal growth or maturation during the first 2 or 3 y of life, 2) the possible renal origin of human urinary EGF, and 3) decreased urinary EGF excretion in children with ARF. In particular, EGF/Cr is not a reliable indicator for the expression of actual urinary EGF excretion in ARF. Instead of urinary EGF/Cr, urinary EGF concentration may be used to predict the daily total urinary EGF excretion during ARF. These results provide the pattern of urinary EGF excretion during ARF in children and may be of help for further clinical studies.
Similar content being viewed by others
Main
ARF arises from a complex interplay between cellular and hemodynamic events where renal tubular cell injury or dysfunction results in a reduced excretion of urinary creatinine. Recovery from ARF depends on the repair and regeneration of injured tubular cells. EGF, one of the most potent mitogens for renal epithelial cells(1), may be involved in this process of regeneration and play an important role in renal repair after injury.
Urine contains high concentrations of EGF(2, 3). Although the source of urinary EGF in the human is unknown, evidence from the mouse(3, 4) suggests it may be of renal origin. Renal prepro-EGF mRNA and urinary EGF excretion have been found to be decreased during ARF in the rat(5). In contrast, EGF binding increases in the mouse kidney after ischemic injury(6, 7). These animal experimental findings provide important information with regard to EGF in ARF and prompted us to study the levels of urinary EGF in children with ARF.
Urinary EGF/Cr has been traditionally used to express urinary EGF excretion. Accordingly, we examined the age distribution of urinary EGF/Cr in healthy children. Our preliminary results on urinary EGF/Cr in ARF children showed that urinary EGF/Cr measures before peak serum creatinine from children with ARF were not statistically different from those of healthy children, whereas the measures after peak serum creatinine from patients decreased significantly when compared with normal control. These unexpected results raised the question of the actual urinary EGF excretion in ARF. We thus conducted this study to characterize the actual urinary EGF excretion and to determine whether the EGF/Cr is a reliable estimate of urinary EGF excretion during the course of ARF.
METHODS
Subjects and samples. Random urine specimens were obtained for analysis of normal urinary EGF excretion from 360 healthy Chinese neonates, infants, and children with an equal number of each sex. Random urine samples followed by 24-h urine collection was also obtained from 25 children(including four patients with stable chronic renal failure) for comparison of the random and 24-h urinary EGF levels. The age of these children ranged from 1 mo to 15 y. The serum creatinine levels of four patients with chronic renal failure were 301, 486, 619, and 672 μmol/L (3.4, 5.5, 7.0, and 7.6 mg/dL) respectively.
Thirteen children with ARF at the National Taiwan University Hospital were enrolled in our study from February 1992 to July 1993. ARF was defined as a sudden rise in serum creatinine concentration of at least 44 μmol/L (0.5 mg/dL) daily(8) with a serum creatinine level of over 133μmol/L (1.5 mg/dL) for older children, and over 106 μmol/L (1.2 mg/dL) for infants. Only patients with clinically diagnosed ARF of possible acute tubular necrosis or other tubular dysfunctions were enrolled in this study. They were considered when renal function did not improve after correction of possible prerenal causes, and when hepatorenal syndrome, vascular, glomerular, and obstructive etiologies were excluded. Marked increase in urinaryN-acetyl-β-glucosaminidase and/or fractional excretions of sodium greater than 2-3% provided additional evidence. The causes of acute renal failure included hypoxemia, shock, sepsis, uric acid nephropathy, and administration of nephrotoxic drugs. Because the calculated creatinine clearance is not a reliable estimate for actual GFR in ARF, it is just as simple to separate ARF into three stages according to the serum creatinine levels: 1) initial phase, the period before peak serum creatinine, indicating renal injury, stopped or ongoing; 2) recovery phase, the period after peak serum creatinine, indicating renal function recovery; and3) normal stage, the period after completely normal serum creatinine, indicating near-normal or normal renal function. These children(four neonates, five infants and preschool children, and four school children) had at least three 24-h urine aliquots and simultaneous serum samples taken during the course of urinary and serum EGF determinations. The mean peak serum creatinine for these patients was 371 ± 194 μmol/L (4.2 ± 2.2 mg/dl) with a range from 141 to 884 μmol/L (1.6-10.0 mg/dL), and the mean duration between onset and peak serum creatinine was 6.5 ± 3.6 d (range from 1 to 14 d). Serum creatinine and the timing of measures were 292 ± 203 μmol/L (3.3 ± 2.3 mg/dL) and 3.0 ± 2.8 d before the peak for initial phase and 248 ± 141 μmol/L (2.8 ± 1.6 mg/dL) and 4.1 ± 3.7 d after the peak for recovery phase, respectively. Measures in the normal stage were taken at 1-42 d after evidence of normal serum creatinine.
Urine aliquots and serum samples were frozen at -70°C until used. All studies were performed with informed consent and approved by the Research Committee of National Taiwan University Hospital.
EGF assay and creatinine measurements. EGF concentrations were measured using a human EGF kit from Amersham Corp. Human recombinant EGF(Collaborative Biomedical Products, Bedford, MA) was used as a standard. An antiserum (0.2 mL) raised in rabbits and 125I-EGF (0.1 mL) was added to urine aliquots or serum samples (0.1 mL) in a test tube and incubated for 3 h at room temperature. This antiserum exhibited 100% cross-reactivity with human EGF and 88% with mouse EGF. The second antibody Amerlex-M (0.5 mL) was then added to the tubes. After incubation for 10 min at room temperature, the tubes were centrifuged for 10 min at 1500 × g. The supernatants were discarded, and the tubes were counted with a gamma scintillation counter. All samples were measured in duplicate. The intra- and interassay coefficients of variation were 5.7 and 8.6%, respectively. Urinary creatinine concentration was determined with a Beckman Creatinine Analyzer II chemistry analyzer(Beckman Instruments Inc., Fullerton, CA).
Statistical analysis. Excretion of EGF was expressed as a ratio of urinary EGF to urinary creatinine concentration for all samples and a daily total urinary EGF if available. Data were reported as mean ± SD when appropriate. One-way analysis of variance followed by Tukey's test was used to compare urinary EGF/Cr in different age groups. Linear regression analysis was used to examine the relationship between random and 24-h urinary EGF excretions. Comparison of urinary EGF and serum EGF during the course of ARF was made by repeated measure analysis using a generalized estimating equation approach(9), and dummy variables for regression models were used to specify groups of stage and age. Wilcoxon's rank sum test was used for comparison of urinary EGF between the patients in normal stage of ARF and age-matched healthy controls. Statistical significance was set atp < 0.05.
RESULTS
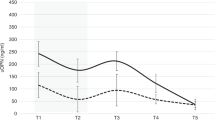
Normal urinary EGF levels. The developmental changes in urinary EGF levels in children are illustrated in Fig. 1. The highest urinary EGF/Cr was found during 1 mo to 3 y of age (F = 48.41, p < 0.001 by analysis of variance). The levels declined and remained constant after the age of 6 y.
Random versus 24-h urinary EGF excretions. A highly significant correlation was found between the random urine EGF/Cr and 24-h urine EGF/Cr(r = 0.92, p < 0.001) (Fig. 2). There was no correlation of urinary EGF/Cr with daily total urine EGF(r = 0.21, p = 0.33).
Urinary EGF excretions in ARF. Figure 3 illustrates the classical trend of changes in urinary EGF/Cr and daily total urine EGF during the course of ARF in three patients. There was a decline in urinary EGF/Cr with a relatively constant, low daily urinary EGF excretion after ARF followed by a rise of both parameters toward normal(Fig. 4). The lowest urinary EGF/Cr values were found in the recovery phase. The urinary EGF/Cr levels in initial phase were also lower when compared with those of the normal stage in the same individual. Both urinary EGF/Cr and daily total urine EGF in the normal stage of these patients were not statistically different from those of age- and sex-matched healthy children (536 ± 369 versus 502 ± 324 pmol/mmol for urinary EGF/Cr, and 982 ± 881 versus 881 ± 809 pmol for daily urinary EGF excretion).
The urine EGF concentrations during the course of ARF, regardless of the urine volume, were parallel to the trend of the changes of daily total urinary EGF excretions. Low urinary EGF levels were noted in initial and recovery phases, whereas a higher concentration was found in the normal stage(Fig. 4). Table 1 shows details of regression analysis between the two parameters with age adjustment.
Serum EGF levels during the course of ARF were 566 ± 132, 554± 129, and 569 ± 134 pmol/L for initial, recovery, and normal phases, respectively. Statistically, serum EGF level remained unchanged during ARF.
The daily urinary creatinine in the initial phase was 1.49 ± 2.20 mmol (168 ± 249 mg), which was significantly lower than 2.94 ± 3.37 mmol (332 ± 381 mg) in the recovery phase (p = 0.011 by paired t test). In contrast, the fractional excretion of sodium showed no statistical difference between initial and recovery phases (14.9± 18.3% versus 9.3 ± 10.0%, p = 0.19 by paired t test), suggesting that the integrity of tubular function had not yet been restored during the recovery phase.
DISCUSSION
There is a high correlation between random and 24-h urinary EGF/Cr. It is thus reasonable to use random urine tests for monitoring urinary EGF excretion. Urinary EGF/Cr has been widely used as a reference for EGF excretion. This ratio correlates well with urine creatinine concentrations in normal adults(10) and with creatinine clearance in patients with various renal diseases(11). The specific developmental patterns of urinary EGF/Cr have also been reported in children(2), newborns(12), premature infants(13), and infants with congenital renal disease(14). In contrast to adult data, normal urinary EGF/Cr in children seems to be age (growth)-dependent rather than urine creatinine- and/or corrected creatinine clearance-related. The finding of highest urinary EGF excretions during the first 3 y of life is interesting. Potential physiologic roles for EGF in the kidney have been recently reviewed(15–17). Although the exact role of EGF in renal development remains obscure, a postnatal rise in renal EGF content(18) as well as urinary EGF excretion(12, 13) suggests a role for EGF in renal maturation. Several physiologic or laboratory situations in children such as GFR(19), p-aminohippuric acid clearance(19), urinary N-acetyl-β-glucosaminidase levels(20), and renal cortical echogenicity(21) reach adult status after 2 or 3 y of age. These findings may suggest the rapid growth or maturation of kidneys during the first few years of life. If EGF is indeed involved in renal development, it is not surprising that urinary EGF excretion maintains at a high level in this period.
The role of EGF in ARF has recently received much attention. There are scanty studies concerning EGF in human ARF. A decreased urinary EGF/Cr during the acute phase in adult patients with ARF has been recently reported with the ratio returning toward normal after recovery(22). Our results from children with ARF provide more conclusive data which confirm part of previous experimental work in adult rats(5, 6). In contrast to persistent low daily total urinary EGF for a time, the urinary EGF/Cr showed a decrease after the onset of ARF and dropped further after the declination of serum creatinine. It is apparent that the latter finding should be the result of increased urine creatinine excretion due to improving renal function. The initial low urinary EGF excretion may be the result of either reduced glomerular filtration or decreased renal production. However, the low daily total urinary EGF and decreased urinary EGF/Cr at the recovering stage accompanied by unchanged serum EGF during the course of ARF suggest renal production, rather than through glomerular filtration, as the source of urinary EGF.
It has been suggested that EGF was produced endogenously in the kidney and was secreted into the tubular lumen(16, 17).In situ hybridization localization of prepro-EGF in the mouse indicates the sites of renal synthesis to be thick ascending limb of Henle and early distal convoluted tubule(4). There is considerable information regarding the role and the origin of urinary EGF in the mouse(15–17). However, the source of urinary EGF in humans is still not clear. Several studies(10, 12) indirectly suggest renal origin of human urinary EGF. Our results also strongly support this view. Recently, positive in situ hybridization for EGF mRNA in the nuclei of human glomerular mesangial cells, distal convoluted tubules and collecting tubules has been reported(23). Labeled human EGF infusion study revealed that plasma-derived EGF constituted only a small part of the urinary EGF(23). These studies provide more direct evidence of the renal source of human urinary EGF.
Because of the luminal site of EGF synthesis and basolateral location of EGF receptors in the tubular cells(17, 24), the exact physiologic role of urinary EGF remains unknown. However, a paracrine function of EGF may exist in the kidney, particularly during disruption of tubular integrity(16, 17). Urinary excretion of EGF and renal prepro-EGF mRNA decrease rapidly, whereas specific binding of EGF increases soon after the onset of ARF in the animal model(5–7). Increased renal-soluble EGF after ischemia accompanied by a decrease in membrane-associated precursors has also been reported recently(25). The increased EGF receptor number may suggest the important role of EGF for renal repair or regeneration. It would not be surprising that endogenous soluble EGF increased in ischemia-injured rat kidney(25) and exogenous EGF administration could accelerate functional recovery from experimental ARF(7, 26). Whether the persistent low urinary EGF in our patients is a nonspecific result of cellular damage or a result of enhanced receptor binding, or even a specific response to injury that is linked to the up-regulation of EGF receptors and increased sensitivity to EGF remains to be determined.
Although urinary EGF/Cr is generally accepted to express urinary EGF excretion, the physiologic significance of this ratio may be questioned. Under a normal steady condition, urinary EGF/Cr may reflect a functional relationship between glomerular filtration and the process of renal EGF excretion(10). In patients with stable chronic renal failure, the decreased urinary EGF/Cr(11) may indicate a more profound reduction in urinary EGF (renal EGF production) than urinary creatinine excretion (glomerular filtration plus secretion). While in ARF, urinary EGF/Cr seems not to be a good indicator for actual urinary EGF excretion, particularly in children. The initial low or low normal EGF/Cr may be explained by a concomitant reduction in EGF production and urinary creatinine excretion relatively of the same degree, whereas persistent low urinary EGF with increased urinary creatinine excretion at the recovery stage results in the nadir of EGF/Cr during the course. From our data, instead of urinary EGF/Cr, urine EGF concentration may be used as a simpler parameter to monitor daily total urinary EGF excretion during the course of ARF. The therapeutic effect of EGF in animal model of ARF may justify human clinical trials in the future. Our results provide some information with regard to understanding the pattern of urinary EGF in children with ARF and may be of help for further clinical studies.
Abbreviations
- ARF:
-
acute renal failure
- EGF:
-
epidermal growth factor
- EGF/Cr,:
-
ratio of EGF to creatinine
References
Norman J, Badie-Dezfooly B, Nord EP, Kurtz I, Schlosser J, Chaudhari A, Fine LG 1987 EGF-induced mitogenesis in proximal tubular cells: potentiation by angiotensin II. Am J Physiol 253:F299–F309
Mattila A-L, Perheentupa J, Pesonen K, Viinikka L 1985 Epidermal growth factor in human urine from birth to puberty. J Clin Endocrinol Metab 61: 997–1000
Perheentupa J, Lakshmanan J, Fisher DA 1985 Urine and kidney epidermal growth factor: ontogeny and sex difference in the mouse. Pediatr Res 19: 428–432
Rall LB, Scott J, Bell GI, Crawford RJ, Penschow JD, Niall HD, Coghlan JP 1985 Mouse prepro-epidermal growth factor synthesis by the kidney and other tissues. Nature 313: 228–231
Safirstein R, Zelent AZ, Price PM 1989 Reduced renal prepro-epidermal growth factor mRNA and decreased EGF excretion in ARF. Kidney Int 36: 810–815
Safirstein R, Price PM, Saggi SJ, Harris RC 1990 Changes in gene expression after temporary renal ischemia. Kidney Int 37: 1515–1521
Norman J, Tsau YK, Bacay A, Fine LG 1990 Epidermal growth factor accelerates functional recovery from ischemic acute tubular necrosis in the rat: role of the epidermal growth factor receptor. Clin Sci 78: 445–450
Feld LG, Springate JE, Fildes RD 1986 Acute renal failure: I. pathophysiology and diagnosis. J Pediatr 109: 401–408
Zeger SL, Liang KY, Albert PS 1988 Models for longitudinal data: a generalized estimating equation approach. Biometrics 44: 1049–1060
Callegari C, Laborde NP, Buenaflor G, Nascimento CG, Brasel JA, Fisher DA 1988 The source of urinary epidermal growth factor in humans. Eur J Appl Physiol 58: 26–31
Mattila A-L, Pasternack A, Viinikka L, Perheentupa J 1986 Subnormal concentrations of urinary epidermal growth factor in patients with kidney disease. J Clin Endocrinol Metab 62: 1180–1183
Watanabe K, Ono A, Hirata Y, Fukuda Y, Kojima T, Kobayashi Y 1989 Maturational changes and origin of urinary human epidermal growth factor in the neonatal period. Biol Neonate 56: 241–245
Scott SM, Guardian CM, Angelus P, Backstrom C 1991 Developmental pattern of urinary epidermal growth factor in the premature infant and the influence of gender. J Clin Endocrinol Metab 72: 588–593
Scott SM, Guardian C, Rogers C, Angelus P, Werner S 1989 Effect of congenital renal disease and neonatal thyroid status on urinary human epidermal growth factor concentrations. Acta Endocrinol 121: 505–512
Fisher DA, Salido EC, Barajas L 1989 Epidermal growth factor and the kidney. Annu Rev Physiol 51: 67–80
Harris RC 1991 Potential physiologic roles for epidermal growth factor in the kidney. Am J Kidney Dis 17: 627–630
Hamm LL, Hering-Smith KS, Vehaskari VM 1993 Epidermal growth factor and the kidney. Semin Nephrol 13: 109–115
Gattone VH, Sherman DA, Hinton DA, Niu FW, Topham RT, Klein RM 1992 Epidermal growth factor in the neonatal mouse salivary gland and kidney. Biol Neonate 61: 54–67
Rubin MI, Bruck E, Rapoport M 1949 Maturation of renal function in childhood: clearance studies. J Clin Invest 28: 1144–1162
Tsau YK, Chen CH, Teng RJ, Tsai WS, Sheu JN 1991 UrinaryN-acetyl-β-glucosaminidase in normal Chinese children and children with pyelonephritis. Acta Paediatr Sin 32: 24–30
Liao MH, Tsau YK, Chu JM 1993 Using quantitative ultrasound to estimate renal maturation. Acta Paediatr Sin 34: 367–371
Taira T, Yoshimura A, Ideura T, Koshikawa S 1992 Clinical significance of urinary epidermal growth factor levels in patients with acute renal failure. Nephron 60: 375
Lev-Ran A, Hwang DL, Ben-Ezra J, Williams LE 1992 Origin of urinary epidermal growth factor in humans: excretion of endogenous EGF and infused 131I-human EGF and kidney histochemistry. Clin Exp Pharmacol Physiol 19: 667–673
Salido EC, Yen PH, Shapiro LJ, Fisher DA, Barajas L 1989 In situ hybridization of prepro-epidermal growth factor mRNA in the mouse kidney. Am J Physiol 256:F632–F638
Schaudies RP, Johnson JP 1993 Increased soluble EGF after ischemia is accompanied by a decrease in membrane-associated precursors. Am J Physiol 264:F523–F531
Humes HD, Cieslinski DA, Coimbra TM, Messana JM, Galvao C 1989 Epidermal growth factor enhances renal tubule cell regeneration and repair and accelerates the recovery of renal function in postischemic acute renal failure. J Clin Invest 84: 1757–1761
Author information
Authors and Affiliations
Additional information
Supported by a grant from the National Science Council of the Republic of China (NSC-81-0412-B002-625).
Rights and permissions
About this article
Cite this article
Tsau, YK., Sheu, JN., Chen, CH. et al. Decreased Urinary Epidermal Growth Factor in Children with Acute Renal Failure: Epidermal Growth Factor/Creatinine Ratio Not a Reliable Parameter for Urinary Epidermal Growth Factor Excretion. Pediatr Res 39, 20–24 (1996). https://doi.org/10.1203/00006450-199601000-00003
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199601000-00003
This article is cited by
-
A novel urinary biomarker profile to identify acute kidney injury (AKI) in critically ill neonates: a pilot study
Pediatric Nephrology (2013)
-
A pilot study of urinary fibroblast growth factor-2 and epithelial growth factor as potential biomarkers of acute kidney injury in critically ill children
Pediatric Nephrology (2013)
-
Effect of asphyxia on urinary epidermal growth factor levels in newborns
Journal of Tongji Medical University (1997)