Abstract
We have measured mean concentrations and have appraised the pulsatile nature of thyrotropin (TSH) and prolactin (PRL) release in children with classical GH deficiency (GHD; n = 4) and neurosecretory GH dysfunction (NSD; n = 4) and have compared the results with those obtained in children with constitutional delay (control; n = 4). Blood samples were obtained at 20-min intervals for 24 h. Pulse analysis of TSH and PRL was undertaken using the Cluster pulse detection algorithm. Circadian rhythmicity of TSH and PRL was assessed using cosinor analysis. The mean 24-h concentration of GH in the control subjects was significantly higher than that obtained in the GHD and NSD groups. With regard to TSH, the mean serum concentration in the GHD and NSD group were higher than that of the control subjects. This augmentation reflects TSH pulses of large amplitude and area, and a higher interpulse valley mean rather than a difference in peak number or peak duration. No differences in mean PRL concentration or characteristics of PRL pulses were found between the control and GHD and NSD subjects. When the 24 h data sets were divided into day (0800-2000 h) and night (2000-0800 h), the mean nighttime TSH concentration was higher than the daytime concentration in the control, GHD, and NSD groups. Although there were no day versus night differences in TSH pulse frequency in either group, peak amplitude, area, and interpulse valley means were increased during the night in the control group, and peak area, duration, and amplitude mean in the NSD group. The nighttime mean PRL concentrations in the control, GHD, and NSD subjects were higher than those found during the day. This increase was accounted for by increases in PRL peak amplitude, area in the control group, and peak area, amplitude, and interpulse valley mean in the GHD and NSD groups. Cosinor analysis of the 24-h TSH and PRL data revealed clear circadian rhythmicity in all groups of subjects. These data suggest that GHD and NSD are associated with an increase in pulsatile TSH secretion due to an increase in pulse amplitude and interpulse valley mean.
Similar content being viewed by others
Main
It is now well established that TSH release is pulsatile in nature and has a circadian periodicity, characterized by a nocturnal surge that begins in the late afternoon and reaches a peak around midnight, remains relatively stable for several hours, and declines thereafter(1–7). Although neither the neuroendocrine mechanisms governing the pulsatile release of TSH nor its circadian rhythm in man is established, considerable evidence indicates that the dopaminergic system, timing of sleep, serum cortisol, and somatostatin tone inhibit TSH secretion(8–15). Abnormal basal serum TSH concentrations and altered response of TSH to TRH in patients suffering from GHD have been reported(16–19). Due to these abnormal responses, such patients have been diagnosed as having pituitary hypothyroidism (hyporesponsiveness) or hypothalamic hypothyroidism (delayed, prolonged, and/or exaggerated TSH response to TRH).
The increased basal TSH levels and exaggerated TSH response to TRH could result from decreased inhibition of TSH release due to a reduction in somatostatin and/or dopamine tone associated with growth hormone deficiency(19, 20). In experimental animals hypothalamic deafferentation abolishes the circadian TSH rhythm(21), explaining the absence of the nocturnal surge of TSH(22) in hypothalamic (central) hypothyroidism.
Recently Municchi et al.(23) assessed the nocturnal TSH surge in GHD children during the afternoon and night periods, but to our knowledge the analysis of a circadian and pulsatile secretion of serum TSH during the 24-h period in GHD has not been previously reported. The purpose of the current study was to characterize pulsatile and circadian TSH and PRL release, examine the nocturnal secretion pattern of TSH and PRL in GHD, and evaluate the relationships among thyroid hormone, GH, PRL, and TSH secretion in children with GH deficiency.
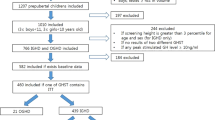
METHODS
Subjects. Twelve children were investigated and divided in three groups according to the 24-h serum GH, GH stimulation tests, and growth velocity. 1) Control subjects consisted of four healthy subjects(one girl and three boys) with constitutional delay(24)(24-h GH greater than 3 μg/L), without endocrinologic abnormalities. All but one (male subject with pubic hair development no greater than Tanner stage II) were considered to be in prepuberty development, and all boys' present plasma testosterone was less than 20 ng/mL. 2) Classical GHD including four prepuberal patients (one boy and three girls), who were diagnosed as GHD by at least two stimulation tests: insulin-induced hypoglycemia(25), clonidine(25), and L-dopa(26). Patients 1-4 had been previously treated with human GH, but therapy was interrupted at least 3 mo before our evaluation. Two patients (nos. 2 and 4) had received T4 because of clinical and laboratory diagnosis of central hypothyroidism during treatment with GH. In these patients thyroid hormone was stopped at least 60 d before this study. 3) NSD according to Spiliotis et al.(27) including four prepubertal patients (nos. 5-8) with short stature (one girl and three boys). Two of these NSD patients (nos. 6 and 7) did not have a delay in bone age, and patients 7 and 8's present IGF-I levels were in the normal range. The clinical and radiologic data for all groups of subjects are presented in Table 1. Bone age was assessed according to Greulich and Pyle(28) standards and pubertal development according to Tanner(29).
Experimental design. Written informed consent for the study from at least one parent of every patient (approved by the University's Institutional review board). The children were admitted to the Hospital on the day before testing to allow one night for accommodation to the setting and were encouraged to maintain their usual diet and ambulatory activity.
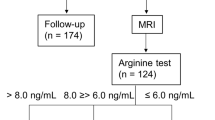
A blood sample was drawn at 0700 h for the baseline measurement of serum T4 and T3 and plasma IGF-I. Beginning at 0800 h, blood samples(1.5 mL) were obtained every 20 min for 24 h for GH, TSH, and PRL determination, through an indwelling venous catheter, with special effort made not to disturb sleep. The children were allowed to ambulate, and a record of their meals and sleep was kept. Serum was immediately separated after blood withdrawal and stored at -20°C until assay. On the following day, TRH (200μg; Biophysics Laboratory, Escola Paulista de Medicina, São Paulo, Brazil), regular insulin (0.1 IU/kg; Lilly, Indianapolis, IN) were administered by i.v. bolus. Blood samples were drawn -30 min and immediately before and 15, 30, 60, 90, and 120 min after the provocative stimulus for GH, TSH, and cortisol determinations. All of the tests were started at 0800 h, at least 10 h after the last meal.
Assays. All measurements were made in duplicate. TSH and GH concentrations were determined by IRMA methods (Pharmacia, Uppsala, Sweden), the detection limit being, respectively, 0.3 mIU/L and 0.1 μg/L for TSH and GH. Serum T3, T4, and cortisol were measured by kits provided by Clinical Assays Diagnostics (Boston, MA). The sensitivities for these methods were 0.3 nmoL/L (T3), 10.3 nmoL/L (T4), and 0.14 μg/dL(cortisol). PRL was measured with kits obtained from Diagnostics Products Corp. (Los Angeles, CA), with a sensitivity of 0.37 μg/L. For measurement of IGF-I, kits from Nichols Laboratories (San Juan Capristano, CA) were used with a sensitivity of 0.10 IU/mL. For all RIA methods the intrassay coefficients of variation were below 11% considering samples of low and high values.
Pulse and statistical analysis. To detect significant serum TSH and PRL hormone excursions (pulses) cluster analysis(30) was used. This program defines a pulse as a statistically significant increase in a cluster of hormone values, followed by a statistically significant decrease in a second cluster value. For TSH, the number of points for nadir and peak clusters, respectively, were two and two, with t statistics of 2.08 for the peak upstroke and 2.08 for peak downstroke. For PRL the number of points for nadir and peak clusters were two and one, respectively, with t statistics of 3.95 and 1.5 for the upstrokes and downstrokes, respectively. These parameters were chosen to constrain the false-positive pulse detection rate to less than 5%. The TSH and PRL data series were analyzed as the intact 24-h set and as two 12-h segments(0800-2000 and 2000-0800 h). If the pulse fell on a sampling time between these two segments, it was assigned to the preceding one.
Comparisons were made by Scheffe's test after analysis of variance or byt test proceeded by logarithmic transformation for nonnormal data. The normality of distribution was examined by using the Kolmogorov-Smirnov test. Statistical significance was assumed when p was less than 0.05. Results were expressed as the mean ± SE. Circadian variations in TSH and PRL were analyzed using the method of least squares to fit the mean hormone values to a cosine function(31). The mesor(value about which the oscillations occur), amplitude (half the difference between the highest and lowest values), and acrophase (timing of high point in clock hours) were studied in group control, GHD, and NSD groups.
RESULTS
The 24-h GH concentrations. The mean 24-h serum concentrations measured in the control, GHD, and NSD subjects are indicated inTable 2. As can be seen, the mean 24-h concentration(μg/L) in the control children (6.1 ± 0.8) was significantly higher than that documented in the GHD (0.9 ± 0.1; p = 0.0003) or NSD (2.1 ± 0.3; p = 0.0015) groups.
The 24-h TSH and PRL concentrations and pulse characteristics. The results of the characterization of pulsatile TSH and PRL release using cluster analysis are shown in Tables 3 and 4 and Figure 1 (A and B), respectively. With regard to TSH, the 24-h mean serum concentration observed in the GHD and NSD groups was higher than in the control subjects (p < 0.05). This elevation could not be explained by a change in TSH pulse frequency or duration, given that there were no differences between the control and GHD or NSD groups. However, data from the GHD and NSD subjects revealed increases in TSH pulse amplitude(p = 0.0004), pulse area (p = 0.0059), and interpulse valley mean (p = 0.001) when compared with the control subjects. Concerning PRL, the 24-h mean serum concentration observed in the GHD and NSD group was no different from that observed in the control subjects. Moreover, there were no differences in the frequency of PRL pulses or in any PRL pulse characteristic when the control and GHD and NSD subjects were compared.
Twenty-four-hour TSH (A) and PRL(B) secretion pattern (sampling every 20 min). The closed squares(▪) indicate the mean serum TSH and PRL concentration of control(n = 4), the open squares (□) and the closed diamonds (♦) represent the mean serum TSH and PRL concentrations of GHD (n = 4) and NSD (n = 4), respectively.
The 12-h TSH and PRL concentrations and pulse characteristics. When the data were analyzed according to 12-h daytime (0800-2000 h) and 12-h nighttime (2000-0800 h) segments, both control and NSD subjects demonstrated a rise in mean serum concentrations during the night but no change in pulse frequency. Data from control subjects revealed an increase at night in TSH pulse amplitude, pulse area, and interpulse valley, but not in pulse duration. Data from the NSD subjects demonstrated an increase at night in the pulse area, pulse duration, and amplitude mean; GHD subjects demonstrated a rise in the mean of interpulse valley. Analysis of the day versus night PRL data from control, GHD, and NSD subjects demonstrated a rise in mean serum concentration during the night but no day/night changes in pulse frequency or duration. The control, GHD, and NSD groups demonstrated nighttime increases in PRL pulse amplitude and pulse area mean.
TSH and PRL circadian rhythms. When the 24-h TSH and PRL data were fitted to a cosinor function, clear circadian TSH and PRL rhythms were disclosed in all groups (control, GHD, and NSD). The acrophases were similar with a range 23:37 to 02:23 h and 01:46 to 04:20 h to TSH and PRL, respectively.
DISCUSSION
Both the circadian rhythms and pulsatile patterns of TSH and PRL release were markedly consistent in control children and agree with previous studies that identified episodic release of TSH and PRL(1–8);i.e. hormonal concentrations exhibited a nocturnal rise beginning in the late afternoon or evening for TSH and PRL, respectively. The acrophase occurs around midnight for TSH and approximately 2 h later for PRL. The circadian TSH and PRL periodicities are composed of series of secretory pulses, with greater magnitudes during the nocturnal hours.
In all subjects studied, mean TSH and PRL concentrations were higher at night than during the day, consistent with the known nocturnal rise in TSH and PRL release(6, 32). Accordingly, increases in pulse amplitude and area means were observed in the nocturnal segment in control and NSD, with GHD subjects having a significantly interpulse valley mean at night. The greater 24-h TSH pulse amplitude, area, and interpulse valley mean found in GHD and NSD compared with those in the control children suggest that the increased TSH release of GHD and NSD is independent from changes in pulse frequency and width (duration).
It has been proposed that the nocturnal surge of TSH is mediated by increased hypothalamic secretion of TRH(3), given the significant correlation between the value of nocturnal peaks and TRH-induced TSH peaks(7). As a group, these data suggest that patients with hypothalamic GHD, responsive to exogenous GH-releasing hormone, may have TRH pulses of greater magnitude than in normal subjects.
Our results demonstrate that children with GHD and NSD have increased circadian TSH secretion. These findings suggest that the GH secretory reserve status is a determinant of or at least contributes to the TSH release profile. Somatostatin, the inhibitory physiologic hormone for GH(33, 34), has been shown to inhibit TSH secretion(35). Experiments in animals have suggested that GH may exert short-loop positive feedback control over hypothalamic secretion of somatostatin(36–38). If a similar GH-dependent feedback mechanism operates in man, as has been suggested by Cobbet al.(19), it is reasonable to assume that GHD may result in reduced hypothalamic somatostatin production that, in turn, may result in increased TSH secretion. Several investigators have administered TRH to GHD and acromegalic subjects with normal basal serum T3 and T4 and have demonstrated that the TSH responses are significantly greater in the former group but blunted in the latter(16, 18, 19). In addition, in GHD patients who exhibit an exaggerated TSH response to TRH, a blunting of the TSH response has been reported during treatment with GH with a return of TSH responsiveness to control when GH treatment is discontinued(17).
In central idiopathic hypothyroidism, Faglia et al.(39) have found production of biologically inactive TSH due to an excess of TSH β subunits and have suggested that TRH signals the secretion of TSH with biologic potency. Morrow et al.(40) have shown that multiple TRH injections correct both quantitative and qualitative defects in TSH secretion in hypothalamic hypothyroidism and concluded that TRH regulates not only TSH secretion but also its bioactivity. It has been recently demonstrated that patients with central hypothyroidism do not have a normal nocturnal increase in TSH pulse amplitude(41). In contrast, the present observations reveal a nocturnal TSH increase in two patients with hypothalamic hypothyroidism (cases 2 and 4) as assessed by cosinor function (acrophase 0.03 and 23.46 h, respectively). That TSH of low biologic activity is being secreted is a possibility with the preservation of circadian rhythms in patients with hypothalamic hypothyroidism representing a less severe degree of tertiary hypothyroidism.
Considerable evidence indicates that the dopaminergic system inhibits TSH and PRL secretion(42, 43). Acute dopamine receptor blockade resulting from i.v. metoclopramide administration has been shown to induce a greater increase in serum TSH and PRL levels during the night as opposed to during the day in men(44, 45). Rossmanith et al.(46) confirmed previous observations that dopamine infusion or bromocriptine administration inhibits TSH secretion and abolishes the nocturnal surge of TSH, and proposed a decrease in dopaminergic activity as assessed by TSH pulse amplitude in response to an infusion of metoclopramide for a 24-h period. These investigators concluded that dopamine inhibits TSH secretion. Our current data suggested that there are no differences between mean PRL concentrations and any pulse parameters in NSD GHD and control subjects, rendering it unlikely that increased TSH secretion in both groups of patients reflects a decrease in dopaminergic tone, different from Shulman et al.(47) data. If this was the case, increased prolactin secretion should be observed, because lactotrophs are remarkably sensitive to dopamine blockage.
Thyroid hormone may influence pulsatile TSH secretion. In effect, T3 rapidly decreases TSH secretion in vitro and in vivo(46). Short-term variations in serum T3 and T4 have been previously described(5) despite the very long half-lives of these hormones. Similar short-term variations were found in patients receiving exogenous T4 replacement with little correlation between peripheral serum T4 or T3 concentrations and pulsatile TSH secretion patterns(32). Brabant et al.(9) found a decrease in TSH pulse amplitude but no change in pulse frequency in response to infusion of T3 and T4. These observations, taken together, suggest that circadian variations in pulsatile TSH release could not account for short-term thyroid hormone variations. Consistent with these findings, when free T4 values were fitted to a cosinor function, there were no circadian rhythms in control and GHD patients (data not shown).
In summary, we have investigated the profile of TSH and PRL secretion in control GHD and NSD children using frequent sampling in conjunction with recently developed techniques to quantitate statistically hormone rhythmicity and pulsatility. These combined approaches demonstrate circadian and episodic pulsatility for TSH and PRL secretion. Furthermore, the degree of integrity of GH secretion from adenohypophysis has an important role in the control of TSH secretion, with GHD patients demonstrating increased TSH release and reflecting increased pulse amplitude and interpulse concentrations rather than changes in pulse frequency and duration.
Abbreviations
- TRH:
-
TSH-releasing hormone
- GHD:
-
growth hormone deficiency
- PRL:
-
prolactin
- NSD:
-
neurosecretory GH dysfunction
- T4:
-
thyroxine
- T3:
-
triiodothyronine
References
Patel YC, Alford FP, Burger HG 1972 The 24-hour plasma thyrotrophin profile. Clin Sci 43: 71–77.
Vanhaelst L, Van Cauter E, Degaute JP, Golstein J 1972 Circadian variation of serum thyrotropin levels in men. J Clin Endocrinol Metab 35: 479–482.
Weeke J 1973 Circadian variation of thyrotropin levels in normal subjects. Scand J Clin Lab Invest 31: 337–342.
Azukizawa M, Pekary AE, Hershman JM, Parker DC 1976 Plasma thyrotropin, thyroxine and triiodothyronine relationships in man. J Clin Endocrinol Metab 43: 533–542.
Brabant G, Ranft U, Ocran K, Hesch RD, Von Zur Muhlen A 1986 Thyrotropin-an episodically secreted hormone. Acta Endocrinol 112: 315–322.
Chan V, Jones A, Liendo-Ch P, McNeilly A, Landon J, Besser GM 1986 The relationship between circadian variations in circulating thyrotropin, thyroid hormones and prolactin. Clin Endocrinol 9: 337–349.
Rose SR, Nisula BC 1989 Circadian variation of thyrotropin in childhood. J Clin Endocrinol Metab 68: 1086–1090.
Branbant G, Ocran K, Ranft U, Von Zur Muhlen A, Hesch RD 1989 Physiological regulation of thyrotropin. Biochimie 71: 293–301.
Brabant G, Brabant A, Ranft U, Ocran K, Kohrle R, Hesch RD, Von Zur Muhlen A 1987 Circadian and pulsatile thyrotropin secretion in euthyroid man under the influence of thyroid hormone and glucocorticoid administration. J Clin Endocrinol Metab 65: 83–88.
Brabant G, Prank K, Ranft U, Schuermeyer TH, Wagner TOF, Hauser H, Kummer B, Feistner H, Hesch RD, Von Zur Muhlen A 1990 Physiological regulation of circadian an pulsatile thyrotropin secretion in normal man and woman. J Clin Endocrinol Metab 70: 403–409.
Parker DC, Rossman LG, Perkary AE, Hershman JM 1987 Effect of 64-hour sleep deprivation on the circadian waveform of thyrotropin(TSH): further evidence of sleep-related inhibition of TSH release. J Clin Endocrinol Metab 64: 157–161.
Parker DC, Pekary AE, Hershman JM 1976 Effect of normal and reversed sleep-wake cycles upon nyctohemeral rhythmicity of plasma thyrotropin: evidence suggestive of an inhibitory influence in sleep. J Clin Endocrinol Metab 43: 318–329.
Van Cauter E, Leclercq R, Vanhaelst L, Golstein J 1974 Simultaneous study of cortisol and TSH daily variations in normal subjects and patients with hyperadrenal-corticism. J Clin Endocrinol Metab 39: 645–652.
Weeke J, Christensen SE, Hansen AP, Laurberg, Lundbaek K 1980 >Somatostatin and the 24 h levels of serum TSH, T3, T4 and reverse T3 in normals, diabetics and patients treated for myxoedema. Acta Endocrinol 94: 30–37.
Patel YC, Baker HWG, Burger HG, Johns MW, Ledinek JE 1974 Suppression of the thyrotropin circadian rhythm by glucocorticoids. J Endocrinol 62: 421–422.
Illig R, Krawczynska H, Torresani T, Prader A 1975 Elevated plasma TSH and hypothyroidism in children with hypothalamic hypopituitarism. J Clin Endocrinol Metab 41: 722–728.
Porter BA, Refetoff S, Rosenfield RL, DeGroot LJ, Fang US, Stark V 1975 Abnormal thyroxine metabolism in hyposomatotrophic dwarfism and inhibition of responsiveness to TRH during GH therapy. Pediatrics 51: 668–674.
Nery M, Liberman B, Wajchenberg BL, Goldman J 1985 Hypothalamic-pituitary function in patients with idiopathic growth hormone deficiency. J Pediatric Endocrinol 1: 109–118.
Cobb EW, Reichlin S, Jackson IMD 1981 Growth hormone secretory status is a determinant of thyrotropin response to thyrotropin-releasing hormone in euthyroid patients with hypothalamic pituitary disease. J Clin Endocrinol Metab 52: 324–329.
Prescott RW, Weightman DR, Kendall-Taylor P, Johnston DG 1984 Differential TSH and PRL responses to dopamine receptor blockade in acromegaly. Clin Endocrinol 21: 369–375.
Fukada H. Greer MA 1975 The effect of basal hypothalamic deafferention on the nyctohemeral rhythm of plasma TSH. Endocrinology 97: 749–753.
Caron PJ, Nieman LK, Rose SR, Nisula BC 1986 Deficient nocturnal surge of thyrotropin in central hypothyroidism. J Clin Endocrinol Metab 62: 960–964.
Municchi G, Malozowski S, Nisula BC, Cristiano A, Rose SR 1992 Nocturnal thyrotropin surge in growth hormone-deficient children. J Pediatr 121: 214–220.
Moore KC, Donaldson DL, Ideus PL, Gifford RA, Moore WV 1993 Clinical diagnoses of children with extremely short stature and their response to growth hormone. J Pediatr 122: 687–692.
Frazer NC, Seth J, Brown NS 1983 Clonidine is a better test for growth hormone deficiency that insulin hypoglycemia. Arch Dis Child 58: 355–358.
Batista MC, Arnhold IJP, Mendonca BB, D'Abronzo FH, Bloise W, Nicolau W 1987 Low-dose oral clonidine: effective growth hormone releasing agent in children but not adolescents. J Pediatr 111: 564–567.
Spiliotis BE, August GP, Hung W, Sonis W, Mendelson W, Bercu BB 1984 Growth hormone neurosecretory dysfunction. JAMA 251: 2223–2230.
Greulich WW, Pyle SI 1959 Radiographic Atlas of Skeletal Development of the Hand and Wrist. Sanford University Press, Stanford, CA
Tanner JM 1962 Growth at Adolescence, 2nd Ed. Blackwell, Oxford, UK
Veldhuis JD, Johnson ML 1986 Cluster analysis: a simple, versatile and robust algorithm for endocrine pulse detection. Am J Physiol 250:E486–E493.
Nelson W, Tong YL, Lee JK, Halberg F 1979 Methods for cosinor-rhythmometry. Chronobiologia 6: 305–323.
Greenspan SL, Klibanski A, Schoenfeld D, Chester Ridgway E 1986 Pulsatile secretion of thyrotropin in man. J Clin Endocrinol Metab 63: 661–668.
Tannenbaum GS 1988 Somatostatin as physiological regulator of pulsatile growth hormone secretion. Horm Res 29: 70–74.
Siler TM, Vandenberg G, Yen SSC, Brazeau P, Vale W, Guillemin R 1973 Inhibition of growth hormone release in humans by somatostatin. J Clin Endocrinol Metab 37: 632–634.
Oliver G, Girard P, Lissitzky JC, Cote J, Boudouresque F, Gillioz L, Conte-Devolx B 1982 Influence of endogenous somatostatin on growth hormone and thyrotropin secretion in neonatal rats. Endocrinology 110: 1018–1022.
Sheppard MC, Kronheim S, Pimpstone BL 1978 Stimulation by growth hormone of somatostatin release from the rat hypothalamus. Clin Endocrinol 9: 583–588.
Terry LC, Crowley WR 1980 The effect of hypophysectomy on somatostatin-like immunoreactivity in discrete hypothalamic and extrahypothalamic nuclei. Endocrinology 107: 1771–1775.
Baker BL, yen YY 1976 The influence of hypothysectomy on the stores of somatostatin in the hypothalamus and pituitary stem. Proc Soc Exp Biol Med 151: 599–602.
Faglia G, Bitensky L, Pinchera A, Ferrari C, Paracchi A, Beck-Peccoz P, Ambrosi B, Spada A 1979 Thyrotropin secretion in patient with central hypothyroidism: evidence for reduced biological activity of immunoreactive thyrotropin. J Clin Endocrinol Metab 48: 989–998.
Morrow JS, Joshi L, Amr S, Weintraub BD 1983 Quantitative and qualitative defects in thyrotropin are correct by repeated thyrotropin releasing hormone injections in hypothalamic hypothyroidism. Clin Res 31: 472A
Samuels MH, Lillehei K, Kleinschmidt-Demasters BK, Stears L, Ridgway EC 1990 Patterns of pulsatile glycoprotein secretion in central hypothyroidism and hypogonadism. J Clin Endocrinol Metab 70: 391–395.
Besses GS, Burrow GN, Spaulding SW, Donabedian RN 1975 Dopamine infusion acutely inhibits the TSH and prolactin response to TRH. J Clin Endocrinol Metab 41: 985–987.
Scalon MF, Weightman DR, Shale DJ, Mora B, Heath M, Snow MH, Hall R 1979 Dopamine is a physiological regulator of thyrotropin(TSH) secretion in normal man. Clin Endocrinol 10: 7–15.
Scalon MF, Weetman AP, Lewis M, Pourmand M, Rodrigues Arnao MD, Weightman DR, Hall R 1980 Dopaminergic modulation of circadian thyrotropin rhythms and thyroid hormone levels in euthyroid subjects. J Clin Endocrinol Metab 51: 1251–1256.
Sowers C 1982 Evidence for dopaminergic control circadian variations in thyrotropin secretion. J Clin Endocrinol Metab 54: 673–675.
Rossmanith WG, Mortola JF, Laughlin GA, Yen SSC 1988 Dopaminergic control of circadian and pulsatile pituitary thyrotropin release in women. J Clin Endocrinol Metab 67: 560–564.
Shulman DI, Hu CS, Root AW, Bercu BB 1989 Pooled prolactin measurements in the evaluations of short children. J Clin Endocrinol Metab 69: 1261–1267.
Author information
Authors and Affiliations
Additional information
Supported by a grant from the “Coordenação de Aperfeiçoamento de pessoal de Nivel Superior (CAPES), Brasilia, Brazil(to S.M.F.V.).
Rights and permissions
About this article
Cite this article
Villares, S., Knoepfelmacher, M., Salgado, L. et al. Pulsatile Release and Circadian Rhythms of Thyrotropin and Prolactin in Children with Growth Hormone Deficiency. Pediatr Res 39, 1006–1011 (1996). https://doi.org/10.1203/00006450-199606000-00013
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199606000-00013