Abstract
The role of nitric oxide (NO) as well as its interaction with prostaglandins (PG) in setting the limits of autoregulation of retinal blood flow (RBF) and choroidal blood flow (ChBF) were studied in newborn pigs (1-5 d old). Blood flows were measured by the microsphere technique. Low and high ocular perfusion pressures (OPP) were induced by inflating balloon-tipped catheters placed at the aortic root and isthmus, respectively. Animals were treated with the NO synthase inhibitors, NG-nitro-L-arginine methyl ester (L-NAME, 1 mg/kg followed by 50 μg/kg/min; n = 12) or NG-monomethyl-L-arginine (L-NMMA, same dose as L-NAME;n = 3), or with saline (n = 12). In separate animals(n = 42), guanosine 3′,5′-cyclic monophosphate (cGMP), the second messenger for NO, and PG were measured at an average OPP of 90 mm Hg and 125 ± 6 mm Hg; cGMP levels served as an index of NO release. The effect of the NO donor sodium nitroprusside on choroidal vessel diameter was determined using video imaging of isolated eyecup preparations. In control animals RBF was constant only within a range of 30 to 80 mm Hg OPP(r = 0.03, p > 0.9). There was no autoregulation of ChBF which increased as a function of OPP (τ = 0.58-0.72, p < 0.01). L-NAME and L-NMMA prevented a change in RBF and ChBF from 30 to 146 mm Hg [the highest OPP studied (r < 0.3, p > 0.15)] and caused an increase in retinal as well as choroidal vascular resistance as OPP was raised; these agents did not affect ocular blood flow at OPP < 30 mm Hg. Elevated OPP caused increases in cGMP, 6-keto-PGF1α, and PGE2 in the choroid (a vascular tissue), which were prevented by L-NAME and L-NMMA. Sodium nitroprusside caused a dilatation of choroidal vessels in isolated eyecup preparations, which was significantly attenuated by indomethacin. Data suggest a role for NO in the autoregulation of RBF and ChBF in the newborn such that a release of NO during a rise in OPP prevents adequate constriction necessary for maintaining RBF and ChBF constant; data also suggest that the vasodilator effect of NO might in part be mediated through a release of PG.
Similar content being viewed by others
Main
RBF and ChBF are maintained constant over a wider range of perfusion pressure in the adult than in the newborn(1–3). Consequently, a mild rise in perfusion pressure above the reduced upper limit of blood flow autoregulation in the newborn leads to a marked increase in blood flow and oxygen delivery to the retina(3, 4), which has been speculated as predisposing to retinopathy of prematurity(4, 5). However, the mechanisms that govern the limits of perfusion pressure over which RBF and ChBF are autoregulated, especially in the newborn, remain largely unknown.
We have previously suggested that cyclooxygenase products, which include PG and free radicals, exert a significant role in the autoregulation of ocular blood flow(3, 4). It has been proposed that NO, which is also a reactive oxygen species, is likewise released from the vasculature during an increase in perfusion pressure(6) and has been implicated in the autoregulation of coronary blood flow in isolated heart preparations(7). Recent evidence suggests that NO can stimulate cyclooxygenase(8, 9). Although prostanoids and free radicals exert significant vasomotor properties(4, 10, 11), the effects of NO have largely been attributed to increases in cGMP(12, 13). The role of NO as well as its interaction with PG in setting the perfusion pressure limits of RBF and ChBF autoregulation, particularly of the newborn, have not been investigated. In the present study, we investigated the role of NO in contributing to the narrow range of RBF and ChBF autoregulation in newborn animals and assessed the possible existence of interactions between NO and PG. For this purpose, we determined the effects of the NO synthase inhibitors L-NMMA and L-NAME on RBF, ChBF, and ocular PG and cGMP levels as a function of perfusion pressure, as well as ascertained the contribution of PG in the vasomotor effects of NO in isolated eye cup preparations.
METHODS
Surgical preparation. Newborn pigs (1-5 d old) weighing 1.2-2.2 kg were used in this study according to a protocol approved by the Animal Care Committee of the Research Center of Ste-Justine Hospital. RBF and ChBF were studied in 27 animals as previously described(4, 14). Briefly, animals were anesthetized with 1.5% halothane for tracheotomy and catheterization of various blood vessels. The left subclavian artery was catheterized with a polyethylene catheter for the withdrawal of blood samples including reference samples. A similar catheter was placed into the left ventricle via the right subclavian artery for the injection of radiolabeled microspheres and another one in the descending thoracic aorta via a femoral artery for continuous BP recording by means of a Statham pressure transducer connected to a Gould multichannel recorder (TA240). A silicone-coated balloon-tipped catheter (Berman Angiocath) was positioned in the distal thoracic descending aorta via a femoral artery; inflation of this balloon produces hypertension in the aortic arch. A second balloon-tipped catheter was placed at the root of the aorta via the right common carotid artery, and its inflation produces hypotension in the aortic arch. A polyethylene catheter was placed in the femoral vein for i.v. administration of drugs. To measure IOP, a 27-gauge butterfly needle attached to a catheter was introduced into the anterior chamber of the eye through the cornea, and the site of entry was sealed with cyanoacrylate glue. Animals were ventilated by means of a Harvard small animal respirator with a gas mixture of 21% O2 and 79% N2. Halothane was discontinued after surgery; animals were maintained onα-chloralose (bolus i.v. injection of 50 mg/kg followed by infusion of 10 mg/kg/h) and paralyzed with pancuronium (0.1 mg/kg i.v.). Body temperature was maintained at 38°C with an overhead radiant lamp, and the animals were allowed to recover from the surgery for 2 h before starting the experiments.
Experimental protocols. Animals were assigned to receive i.v. either saline (1.5 mL; n = 7) or L-NAME (1 mg/kg followed by 50μg/kg/min; n = 9). Protocols used to study the response of RBF and ChBF to changes in perfusion pressure were similar to those we have previously reported(3, 4). Basal RBF and ChBF were recorded 45 min after the injections and 10 min later one of the two balloon-tipped catheters was inflated to produce hypotension or hypertension. Once a steady state BP was achieved (within 30-40 s of balloon inflation), RBF and ChBF were determined again; autoregulation of blood flow is known to be of rapid onset and establishes within 10 s(15). The balloons were deflated after the blood flow measurements, and animals were allowed to recover for 40 min. At the end of this recovery period, a second baseline RBF and ChBF was recorded and 10 min later, final measurement of RBF and ChBF were made after inflating the other balloon-tipped catheter. Hence each animal was subjected to one hypotensive and one hypertensive episode performed in a random order; for each treatment group of animals BP was scaled at intervals of 5 ± 1.8 mm Hg to cover a range of 5 to 146 mm Hg.
Measurements of retinal and ChBF. RBF and ChBF were determined using the radionuclide-labeled microsphere technique as previously described(3, 4). In brief, approximately 106 microspheres (15-μm diameter) labeled with 141Ce, 95Nb,46 Sc, and 113Sn (DuPont NEN, Boston, MA) were injected in a random sequence into the left ventricle. Withdrawal of reference blood samples from the left subclavian artery catheter was started 10 s before the injection of each type of radionuclide-labeled microspheres and was continued for 70 s at a rate of 2 mL/min using a Harvard infusion-withdrawal pump. The number of microspheres exceeded 1000 in each reference sample and 400 in each retina and choroid. Immediately after each injection of microspheres, blood samples were withdrawn from the left subclavian artery to determine blood gases, O2 content (ABL 300; Radiometer, Copenhagen, Denmark), and Hb concentrations. After the experiment, animals were killed with pentobarbital (120 mg/kg i.v.), the location of catheters was verified, and the eyes were removed.
The eyes were weighed, the anterior structures of the eye and the vitreous were gently removed, and the retina and choroid were separated. Radioactivity in the retina, choroid, and reference blood samples were counted in a gamma scintillation counter (Cobra II, Canberra Packard, Downers Grove, IL). The percent interference between radionuclides was subtracted. Because there was no disproportionate distribution of microspheres to the two eyes, the radioactivity in the retina and choroid from both eyes were combined to determine blood flow to these organs(3, 4). Blood flow (mL/min/g) was calculated as (cpm/g of tissue × reference blood withdrawal rate)/(cpm in the reference blood). Oxygen delivery to the retina and choroid was calculated as RBF and ChBF × arterial O2 content(mL/min/g). Retinal and ChVR (mm Hg/mL/min/g) were calculated by dividing the OPP (mean BP minus IOP) by RBF and ChBF, respectively.
Measurements of cGMP and PG. Forty-two additional pigs were prepared as described above to determine the changes in PG and cGMP, a second messenger for NO(12, 13), and to assess the contribution of NO in PG synthesis in the ocular vasculature. For this purpose we measured PGE2, 6-keto-PGF1α (stable metabolite of PGI2), and cGMP levels in a purely vascular ocular tissue, the choroid, in animals treated with saline or NO synthase inhibitors, L-NAME, or L-NMMA. Animals were killed either at an average OPP of 90 mm Hg or immediately after increasing OPP to 125 ± 6 mm Hg (for 2 min, as per blood flow studies), a level greater than the upper OPP limit of autoregulation of RBF and ChBF of newborn pigs(4); this enabled comparable increases in OPP in all treatment groups. Two different NO synthase inhibitors (L-NAME and L-NMMA) were used to ensure that effects of these agents were due to inhibition of NO synthase because arginine alkyl esters such as L-NAME have been recently suggested to possess atropine-like properties(16). Immediately after the animals were killed, liquid N2 was poured on each eye; eyes were then removed and stored at-80°C until assays were performed within 1 mo of storage. On the day of the assay, choroids were thawed on ice and suspended in a cold buffer (pH 7.4) containing 5 mM Tris-HCl, 0.67 mM acetylsalicylic acid, and 0.5 mM EGTA. The tissue was homogenized and centrifuged at 1,000 × g for 10 min; the protein in the pellet was measured by the dye-binding method(17). The supernatant was used to assay cGMP by RIA and to extract and measure PGE2 and 6-keto-PGF1α by RIA as well(4, 10, 18); recovery efficiency was>90%.
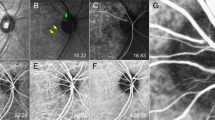
Effects of sodium nitroprusside on choroidal vasculature in vitro. Another group of piglets was killed with pentobarbital, their eyes were removed, and eyecup preparations set up to study the response of the relatively undisturbed choroid vessels as previously described for the retinal vessels(10, 19). Briefly, a circular incision was made 3-4 mm posterior to the ora serrata, and the anterior structures, vitreous body, and retina were removed. The remaining eyecup containing the choroid attached to the sclera was fixed with pins to a wax base in a 20-mL tissue bath containing Krebs buffer of the following composition (mM): NaCl 120, KCl 4.5, CaCl2 2.5, MgSO4 1.0, NaHCO3 27, KH2PO4 1.0, sodium edetate 0.01, glucose 10, to which 1.5 U/mL heparin was added; the buffer was equilibrated with 20% O2, 5% CO2, and 75% N2 and maintained at 37°C and pH 7.35-7.45. Segments of choroidal vessels measuring 80-120 μm in diameter were randomly selected; vessels of this size have been shown to be particularly important in the control of autoregulation of blood flow(20). Experimental conditions appropriate for retinal vessels(10, 19) were found suitable for a study of choroidal vessel responses. To determine concentration-vasorelaxant response curves to the NO donor, sodium nitroprusside (10-12 to 10-5 M), choroidal vessels were precontracted with 0.1 μM U46619 (thromboxane A2 analog). The outer vessel diameter was recorded before and after topical application of the drug with a video camera mounted on a dissecting microscope (Zeiss M-400). To determine any contribution of PG in the vasorelaxant responses to NO, a number of choroidal vessel preparations were pretreated with indomethacin (1 μM) for 30 min; vessels were then contracted with U46619, and responses to sodium nitroprusside determined as described above. The digital images were analyzed using the software, Sigma Scan (Jandel Scientific, Corte Madera, CA). Each measurement was repeated three times and had a variability of <1%. The responses were expressed as a percent reversal of the U46619-induced constriction.
Chemicals. L-NMMA, L-NAME, sodium nitroprusside, and indomethacin were purchased from Sigma Chemical Co., St. Louis, MO; drugs were freshly prepared in normal saline. Radionuclide microspheres were purchased from DuPont NEN, Boston, MA. RIA kits for PGE2 and 6-keto-PGF1α were obtained from Advanced Magnetics (Boston, MA) and those for cGMP from Amersham Corp. (Oakville, Ont). All other chemicals were purchased from Fisher (Montreal, Quebec).
Statistical analysis. Data were analyzed by paired t test, analysis of variance for repeated measures and comparison among means tests, and by linear and nonlinear correlation and regression analysis, as previously described in detail(3, 4, 14). For linear and nonlinear correlation, the Pearson's product moment coefficient(r) and the Kendall's coefficient of rank correlation (τ) were, respectively, calculated. The best fit line for the relationship between blood flow and perfusion pressure was determined by using the method of least squares of a polynomial regression analysis and by calculating the coefficient of determination (R2) as we previously reported for other studies on autoregulation of blood flow(3, 4, 14). We tested stepwise the significance for each increase in order of the polynomial function to examine whether the line fit was improved. The best-fit line was established as that having the last sequentially entered polynomial order to produce a significant improvement in the coefficient of determination. In addition, the relationship of blood flow to perfusion pressure was examined by the method of LOWESS smoothing, and based on these curves separate linear regressions were performed using the random effects model for longitudinal data, as previously used in studies on autoregulation of blood flow(4, 21); these analyses confirmed those determined by polynomial regression analysis. Linear regressions were compared by regression equality test using the method of least squares(22). Statistical significance was set at p< 0.05.
RESULTS
Stability of preparations. Arterial pH, Po2, and IOP remained stable throughout the course of an experiment(Table 1); RBF and ChBF also did not differ between the first and second baselines. L-NAME caused an increase in basal BP and consequently OPP and a decrease in ChBF at baseline.
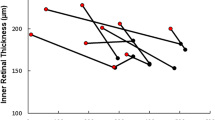
Effects of L-NAME on RBF and ChBF autoregulation. RBF and ChBF plotted as a function of OPP are shown in Fig. 1. In saline-treated animals RBF and ChBF correlated nonlinearly with OPP (τ = 0.58 and 0.72, respectively, p < 0.01). RBF was constant between 30 and 80 mm Hg of OPP (r = 0.03, p > 0.9, based on polynomial and LOWESS curves), and varied with OPP above and below this range(respectively, r = 0.97, p < 0.01; and 0.67,p < 0.05; Fig. 1). ChBF increased as a function of OPP over the entire range of OPP studied (τ = 0.6, p< 0.01).
Retinal and ChBF autoregulation as a function of OPP in newborn pigs treated with L-NAME (1 mg/kg followed by 50 μg/kg/min;n = 9) or saline (n = 7). Each animal was subjected to one hypotensive and one hypertensive episode to cover for each treatment group a range of OPP from 5 to 146 mm Hg. In saline-treated animals, the best fit regression line was a third-order polynomial for RBF (R2 = 0.89, p < 0.001) and a second-order polynomial for ChBF(R2 = 0.80, p < 0.05). In L-NAME-treated pigs a second-order polynomial regression fitted best the points for RBF and ChBF(R2 = 0.75 and 0.80, respectively, p < 0.001).
Treatment with L-NAME significantly extended the upper limit of autoregulation of RBF from 80 to 146 mm Hg (the maximum OPP studied) and allowed ChBF to be maintained constant between 30 and 146 mm Hg (r< 0.3, p > 0.15); L-NAME did not affect RBF and ChBF when OPP was reduced below 30 mm Hg. Moreover, when OPP was raised to its highest levels (>100 mm Hg) RBF and ChBF increased by 38-44% after saline treatment and only by 5-9% after L-NAME (saline versus L-NAME-treated,p < 0.01). Above an OPP of 80 mm Hg retinal and ChVR was unrelated to OPP in saline-treated animals (r < 0.02, p> 0.85), whereas it increased linearly with OPP in L-NAME-treated pigs(respectively, r = 0.84 and 0.92, p < 0.001).
Changes in oxygen delivery to the retina and choroid paralleled those in blood flow. Oxygen delivery to the eye remained constant between 30 and 146 mm Hg OPP after L-NAME (r < 0.1, p > 0.9) but increased as a function of OPP in saline-treated animals (τ = 0.51-0.62, p< 0.01).
To ascertain our findings regarding the effects of L-NAME on the upper limit of RBF and ChBF autoregulation, separate groups of piglets received either L-NAME (1 mg/kg followed by 50 μg/kg/min; n = 3), L-NMMA(dose as L-NAME; n = 3) or saline (n = 5), and RBF and ChBF were studied at OPP ≥ 90 mm Hg. For this purpose each animal was subjected to stepwise acute increases in OPP for 2-min periods from baseline to approximately 90, 105, and 125 mm Hg; OPP varied by 5 ± 2 mm Hg for each of these preset values. In the saline-treated animals RBF and ChBF increased linearly with OPP (r = 0.59-0.88, p < 0.01)(Fig. 2). Basal ChBF (mL/min/g) after L-NAME was lower(12.6 ± 1.1) than that after L-NMMA (29.1 ± 2.3, p< 0.01). L-NAME and L-NMMA prevented the change in RBF and ChBF as a function of OPP (L-NAME: r = 0.11 - 0.2, p > 0.5; L-NMMA: r = 0.26-0.39, p ≥ 0.1); regressions for saline-treated animals differed significantly from those treated with L-NAME and L-NMMA (p < 0.05, by regression equality test). Furthermore, when OPP was increased from 90 to 125 mm Hg, the percent changes in RBF and ChBF were significantly greater in saline-treated pigs than in those treated with L-NAME or L-NMMA (p < 0.01; Table 2); consequently, the changes in retinal and ChVR were higher after L-NAME and L-NMMA than after saline (p < 0.01).
Retinal and ChBF as a function of increased OPP in newborn pigs treated with saline (n = 5), L-NAME (n = 3) or L-NMMA (n = 3); both drugs were given at 1 mg/kg followed by 50μg/kg/min. For these experiments, which are distinct from those presented in Fig. 1, each animal was subjected to stepwise acute increases in OPP from baseline to approximately 90, 105, and 125 mm Hg; OPP varied by 5 ± 2 mm Hg for each of these preset values. The faint lines correspond to the regressions for individual animals, and the thick lines represent the mean regressions for all animals in the group. In saline-treated animals RBF and ChBF increased linearly with OPP (r = 0.59-0.88,p < 0.01). In animals treated with L-NAME and L-NMMA, RBF and ChBF did not change as a function of OPP (r = 0.11-0.39, p≥ 0.1); regressions for saline-treated animals differed from those given L-NAME and L-NMMA (p < 0.05, by regression equality test).
Effects of NO synthase inhibitors on choroidal cGMP and PG levels. A rise in OPP was associated with an increase in the levels of cGMP, 6-keto-PGF1α, and PGE2 in the choroid of saline-treated pigs; this was prevented by L-NAME and L-NMMA(Table 3).
Effects of sodium nitroprusside on choroidal vessel diameters. Sodium nitroprusside produced a concentration-dependent relaxation of choroidal vessels precontracted with the thromboxane A2 analog U46619(Fig. 3). Pretreatment of choroidal vessels with indomethacin attenuated the vasorelaxant response to sodium nitroprusside by approximately 40%; indomethacin by itself did not affect choroidal vascular diameter.
Effect of sodium nitroprusside on choroidal vessel diameter in eyecup preparations of newborn pigs pretreated with saline(empty circles) or indomethacin (1 μM; filled circles). Vessel diameter was measured by video imaging technique. Relaxant responses are expressed as a percent reversal of U46619-induced constriction. Each point is the mean ± SEM of four experiments. *p < 0.05 compared with corresponding values after saline (by analysis of variance and comparison among means tests).
DISCUSSION
In the newborn, there is no autoregulation of ChBF and the upper limit of RBF autoregulation is reduced(3, 4). Inasmuch as autoregulation of ChBF does exist in the adult(2), its absence in the newborn could be expected to be of important pathophysiologic significance. However, the mechanisms of autoregulation of blood flow to the eye are not fully understood. PG have been shown to play a role in cerebral and ocular blood flow autoregulation in the newborn(3, 4, 14, 23). The potent vasodilator NO has also been implicated in coronary blood flow autoregulationin vitro(7). Moreover, NO has also been found to stimulate cyclooxygenase activity(8, 9). It is thus possible that PG and NO interact with each other in the control of autoregulation of circulation. We therefore studied the role of NO and its interactions with PG in setting the limits of RBF and ChBF autoregulation in the newborn.
We have previously demonstrated the suitability of the protocol used in the present experiments for a study of blood flow autoregulation(3, 4, 14, 23). The autoregulatory ranges of RBF and ChBF observed in the control animals of this study are virtually identical to those previously reported(3, 4). In addition to studying autoregulation of blood flow as we have formerly described(3, 4, 14, 23), different animals were subjected to similar gradual increases in perfusion pressure. First the regression lines for ocular blood flow as a function of OPP ≥ 90 mm Hg in the saline-treated pigs did not differ in the two experimental protocols (p ≥ 0.25). Second, NO synthase inhibitors maintained blood flow constant over the full range of OPP studied in both types of experiments. Thus the results obtained have been substantiated.
Data of this study indicate an involvement of NO in the autoregulation of RBF and ChBF in newborn pigs. This is suggested by two main observations. First, cGMP, a second messenger for NO(12, 13), increased in the choroid (a vascular tissue) in response to increased perfusion pressure, and this effect was prevented by the NO synthase inhibitors, L-NAME and L-NMMA (Table 3). Second, and more important, an inhibition of NO synthase by both L-NAME and L-NMMA maintained RBF and ChBF constant over a range of OPP wider than in control animals(Figs. 1 and2) and increased the vascular resistance during high OPP (Table 2). Assuming that an increase in cGMP is indicative of an increase in NO, it would appear that NO is released during a rise in perfusion pressure, as previously reported(6), and NO directly or, in part through PG, contributes to setting the upper limit of autoregulation of RBF and ChBF in the newborn animal. Thus, results of this study indicate that NO is involved in the upper limit of autoregulation of ocular blood flow.
NO does not seem to contribute to the RBF and ChBF response at the lower limit of perfusion pressure (Fig. 1); this is in conformity with data of other workers(7, 24, 25). A reduction in oxygen delivery to tissues during hypotension may decrease the O2-dependent NO synthesis so that NO synthase inhibitors may not cause further inhibition. NO also does not appear to contribute to basal RBF as opposed to ChBF (Tables 1 and 3), as previously reported(26). Several authors have suggested that the role of NO in the control of basal blood flow differs among tissues; for instance, NO seems to be important in resting circulation to certain areas of the brain(27) and in the kidneys(28), but not in the heart(29), which may partly explain the heterogeneity in endothelium-dependent responses of different blood vessels(30–33).
Certain observations made in this study also suggest that NO might activate cyclooxygenase and its hemodynamic effects might in part be contributed by PG. For example, an inhibition of NO synthase prevented the hypertension-induced increase in both cGMP and PG (Table 3). Furthermore, the sodium nitroprusside-induced vasodilation was significantly attenuated after an inhibition of PG synthesis by indomethacin (Fig. 3). On the other hand, because cyclooxygenase activity is O2-dependent, a decrease in PG levels after NO synthase inhibitors could have been indirectly caused by the decrease in tissue oxygen delivery induced by these drugs; this is, however, unlikely because PG concentrations at basal OPP were not altered by L-NAME and L-NMMA.
The present study does not identify the relative contribution of NO and PG in the control of autoregulation of RBF and ChBF. It may appear that PG exert a more significant role in this physiologic process, because inhibition of cyclooxygenase enhances autoregulation in the newborn(3, 4, 23) in a manner comparable to that caused by the blockers of NO synthesis (Figs. 1 and2). However, an important role for NO cannot be excluded especially because the vasodilatory effects of PGE2 and PGD2 are in part produced by NO(35, 36). It is very likely that both NO and PG contribute together as well as independently in setting the narrow range of autoregulation of RBF and ChBF of the newborn.
In summary, this study reveals a role for NO in the autoregulation of RBF and ChBF. When OPP is acutely increased NO and PG are released; by possibly interacting with dilator PG NO contributes to the narrow or absent range of autoregulation of RBF and ChBF in the newborn. The reduced upper limit of RBF autoregulation and an absence of ChBF autoregulation in the newborn(3, 4) suggest a decreased vasoconstriction (or excess vasodilation)(3, 4). Both NO as well as PGE2 and PGI2 indeed cause more vasodilation in ocular tissues of newborns than in those of adults(19, 34); consequently, an inhibition of their synthesis can establish effective autoregulation of RBF and ChBF in the newborn (Figs. 1 and2)(3, 4). However, an effective autoregulation of blood flow during increased perfusion pressure must require an active vasoconstriction and not simply an elimination of vasodilation(37). Thus, it is apparent from the data of the present and other(3, 4) studies that in the newborn, NO and PG prevent or mask the vasoconstriction essential for maintaining blood flow constant during increases in perfusion pressure(38).
Abbreviations
- NO:
-
nitric oxide
- RBF:
-
retinal blood flow
- ChBF:
-
choroidal blood flow
- cGMP:
-
guanosine 3′,5′-cyclic monophosphate
- PG:
-
prostaglandin
- L-NAME:
-
NG-nitro-L-arginine methyl ester
- L-NMMA:
-
NG-monomethyl-L-arginine
- ChVR:
-
choroidal vascular resistance
- OPP:
-
ocular perfusion pressure
- BP:
-
blood pressure
- IOP:
-
intraocular pressure
References
Alm A, Bill A 1972 The oxygen supply to the retina. II. Effects of high intraocular pressure and of increased arterial carbon dioxide tension on uveal and retinal blood flow in cats. Acta Physiol Scand 84: 306–319.
Kiel JW, Shepherd AP 1992 Autoregulation of choroidal blood flow in the rabbit. Invest Ophthalmol Vis Sci 33: 2399–2410.
Chemtob S, Beharry K, Rex J, Chatterjee T, Varma DR, Aranda JV 1991 Ibuprofen enhances retinal and choroidal blood flow autoregulation in newborn piglets. Invest Ophthalmol Vis Sci 32: 1799–1807.
Hardy P, Abran D, Li D-Y, Fernandez H, Varma DR, Chemtob S 1994 Free radicals in retinal and choroidal blood flow autoregulation in the piglet: interaction with prostaglandins. Invest Ophthalmol Vis Sci 35: 580–591.
Flynn JT, Bancalari E, Snyder ES 1992 A cohort study of transcutaneous oxygen tension and the incidence and severity of retinopathy of prematurity. N Engl J Med 326: 1050–1054.
Vargas HM, Ignarro LJ, Chaudhuri G 1990 Physiological release of nitric oxide is dependent on the level of vascular tone. Eur J Pharmacol 190: 393–397.
Ueeda M, Silvia SK, Olsson RA 1992 Nitric oxide modulates coronary autoregulation in the guinea pig. Circ Res 70: 1296–1303.
Salvemini D, Misko TP, Masferrer JL, Seibert K, Currie MG, Needleman P 1993 Nitric oxide activates cyclooxygenase enzyme. Proc Natl Acad Sci USA 90: 7240–7244.
Korbut R, Ocetkiewicz A, Gryglewski RJ 1993 Nitric oxide complements prostacyclin in the regulation of endothelial thromboresistance under flow conditions. Method Find Exp Clin Pharmacol 15: 179–181.
Abran D, Varma DR, Chemtob S 1995 Increased thromboxane-mediated contractions of retinal vessels of newborn pigs to peroxides. Am J Physiol 268:H628–H632.
Wolin MS, Messina EJ, Kaley G 1989 Involvement of prostaglandins in arteriolar vasodilation to peroxides. Adv Prostaglandin Thromboxane Leukot Res 19: 281–284.
Gruetter CA, Gruetter DY, Lyon JE, Kadowitz PJ, Ignarro LJ 1981 Relationship between cyclic guanosine 3′:5′-monophosphate formation and relaxation of coronary arterial smooth muscle by glyceryl trinitrate, nitroprusside, nitrite and nitric oxide: effects of methylene blue and methemoglobin. J Pharmacol Exp Ther 219: 181–186.
Waldman SA, Murad F 1988 Biochemical mechanisms underlying vascular smooth muscle relaxation: the guanylate cyclase-cyclic GMP system. J Cardiovasc Pharmacol 12:S115–S118.
Chemtob S, Beharry K, Rex J, Varma DR, Aranda JV 1990 Changes in cerebrovascular prostaglandins and thromboxane as a function of systemic blood pressure: cerebral blood flow autoregulation of newborn piglets. Circ Res 67: 674–682.
Aaslid R, Lindegaard KF, Sorteberg W, Nornes H 1989 Cerebral autoregulation dynamics in humans. Stroke 20: 45–52.
Buxton ILO, Cheek DJ, Eckman D, Westfall DP, Sanders KM, Keef KD 1993 NG-Nitro-l-arginine methyl ester and other alkyl esters of arginine are muscarinic receptor antagonists. Circ Res 72: 387–395.
Bradford MM 1976 A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein dye binding. Anal Biochem 72: 248–254.
Varma DR, Chemtob S 1993 Endothelium- and β-2 adrenoceptor-independent relaxation of rat aorta by tyramine and certain other phenylethylamines. J Pharmacol Exp Ther 265: 1096–1104.
Abran D, Varma DR, Li D-Y, Chemtob S 1994 Reduced responses of the newborn pig retinal vessels to prostaglandins but not to thromboxane. Can J Physiol Pharmacol 72: 168–173.
Baumbach GL, Heistad DD 1985 Regional, segmental and temporal heterogeneity of cerebral vascular autoregulation. Ann Biomed Eng 13: 303–310.
Yamashita Y, Goddard-Finegold J, Contant CF, Martin CG, Michael LH 1993 Phenobarbital and cerebral blood flow during hypotension in newborn pigs. Pediatr Res 33: 598–602.
Sokal RR, Rohlf Fj 1981 Correlation and multiple and curvilinear regression. In: Sokal RR, Rohlf FJ (eds) Biometry. WH Freeman, New York, pp 561–690.
Chemtob S, Beharry K, Rex J, Varma DR, Aranda JV 1990 Prostanoids determine the range of cerebral blood flow autoregulation of newborn piglets. Stroke 21: 774–784.
Wang Q, Paulson OB, Lassen NA 1992 Is autoregulation of cerebral blood flow in rats influenced by nitro-L-arginine, a blocker of the synthesis of nitric oxide?. Acta Physiol Scand 145: 297–298.
Buchanan JE, Phillis JW 1993 The role of nitric oxide in the regulation of cerebral blood flow. Brain Res 610: 248–255.
Deussen A, Sonntag M, Vogel R 1993 L-Arginine-derived nitric oxide: a major determinant of uveal blood flow. Exp Eye Res 57: 129–134.
Iadecola C, Pelligrino DA, Moskowitz MA, Lassen NA 1994 Nitric oxide synthase inhibition and cerebrovascular regulation. J Cerebr Blood Flow Metab 14: 175–192.
Raij L 1993 Nitric oxide and the kidney. Circulation 87:V26–V29.
Parent R, Al-Obaidi M, Lavallee M 1993 Nitric oxide formation contributes to β-adrenergic dilation of resistance coronary vessels in conscious dogs. Circ Res 73: 241–251.
Vanhoutte PM, Miller VM 1985 Heterogeneity of endothelium-dependent responses in mammalian blood vessels. J Cardiovasc Pharmacol 7:S12–S23.
Keith RA, Burkman AM, Sokoloski TD, Fertel RH 1982 Vascular tolerance to nitroglycerin and cyclic GMP generation in rat aortic smooth muscle. J Pharmacol Exp Ther 221: 525–531.
Ignarro LJ, Gold ME, Buga GM, Byrns RE, Wood KS, Chaudhuri G, Frank G 1989 Basic polyamino acids rich in arginine, lysine, or ornithine cause both enhancement of and refractoriness to formation of endothelium-derived nitric oxide in pulmonary artery and vein. Circ Res 64: 315–329.
Abran D, Varma DR, Chemtob S 1995 The retinal vasomotor effects of nitric oxide are greater in the newborn than in the adult pig and are mediated in part by PGI2. Pediatr Res 37: 73A( abstr)
Abran D, Varma DR, Chemtob S 1995 The retinal vasomotor effects of nitric oxide are greater in the newborn than in the adult pig and are mediated in part by PGI2. Pediatr Res 37: 73A
Warren JB, Loi RK, Wilson AJ 1994 PGD2 is an intermediate in agonist-stimulated nitric oxide release in rabbit skin microcirculation. Am J Physiol 266:H1846–H1853.
Koller A, Sun D, Messina EJ, Kaley G 1993 L-arginine analogues blunt prostaglandin-related dilation of arterioles. Am J Physiol 264:H1194–H1199.
Guyton AC 1991 Overview of the circulation, and physics of pressure, flow, and resistance: hemodynamics. In: Guyton AC (eds) Texbook of Medical Physiology. WB Saunders, Philadelphia, 150–158.
Griffith TM, Edwards DH 1990 Myogenic autoregulation of flow may be inversely related to endothelium derived relaxing factor activity. Am J Physiol 258:H1171–H1180.
Acknowledgements
The authors thank Hensy Fernandez for her technical assistance and also F. Menard Inc. (Ange-Gardien, Quebec) for their generous supply of newborn pigs.
Author information
Authors and Affiliations
Additional information
Supported by grants from the Medical Research Council of Canada, the American Heart Association, the Heart and Stroke Foundation of Quebec, the United Cerebral Palsy Foundation, the Hospital for Sick Children's Foundation, and the March of Dimes Birth Defects Foundation. P.H. is a recipient of a Fellowship from the Heart and Stroke Foundation of Canada.
Rights and permissions
About this article
Cite this article
Hardy, P., Nuyt, A., Abran, D. et al. Nitric Oxide in Retinal and Choroidal Blood Flow Autoregulation in Newborn Pigs: Interactions with Prostaglandins. Pediatr Res 39, 487–493 (1996). https://doi.org/10.1203/00006450-199603000-00017
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199603000-00017
This article is cited by
-
Choroidal measurements in decision making for retinopathy of prematurity: a decision tree analysis
International Journal of Retina and Vitreous (2024)
-
Retinopathy of prematurity: inflammation, choroidal degeneration, and novel promising therapeutic strategies
Journal of Neuroinflammation (2017)
-
Effect of oral niacin on central retinal vein occlusion
Graefe's Archive for Clinical and Experimental Ophthalmology (2017)
-
Untersuchung der Aderhautdicke bei aggressiver posteriorer Retinopathia praematurorum, Threshold Disease und Frühgeborenenretinopathie ohne Laserphotokoagulation
Der Ophthalmologe (2016)