Abstract
Background:
Whole-gland extirpation or irradiation is considered the gold standard for curative oncological treatment for localized prostate cancer, but is often associated with sexual and urinary impairment that adversely affects quality of life. This has led to increased interest in developing therapies with effective cancer control but less morbidity. We aimed to provide details of physician consensus on patient selection for prostate focal therapy (FT) in the era of contemporary prostate cancer management.
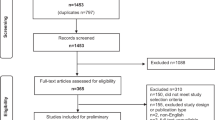
Methods:
We undertook a four-stage Delphi consensus project among a panel of 47 international experts in prostate FT. Data on three main domains (role of biopsy/imaging, disease and patient factors) were collected in three iterative rounds of online questionnaires and feedback. Consensus was defined as agreement in ⩾80% of physicians. Finally, an in-person meeting was attended by a core group of 16 experts to review the data and formulate the consensus statement.
Results:
Consensus was obtained in 16 of 18 subdomains. Multiparametric magnetic resonance imaging (mpMRI) is a standard imaging tool for patient selection for FT. In the presence of an mpMRI-suspicious lesion, histological confirmation is necessary prior to FT. In addition, systematic biopsy remains necessary to assess mpMRI-negative areas. However, adequate criteria for systematic biopsy remains indeterminate. FT can be recommended in D’Amico low-/intermediate-risk cancer including Gleason 4+3. Gleason 3+4 cancer, where localized, discrete and of favorable size represents the ideal case for FT. Tumor foci <1.5 ml on mpMRI or <20% of the prostate are suitable for FT, or up to 3 ml or 25% if localized to one hemi-gland. Gleason 3+3 at one core 1mm is acceptable in the untreated area. Preservation of sexual function is an important goal, but lack of erectile function should not exclude a patient from FT.
Conclusions:
This consensus provides a contemporary insight into expert opinion of patient selection for FT of clinically localized prostate cancer.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Thompson I, Thrasher JB, Aus G, Burnett AL, Canby-Hagino ED, Cookson MS et al. Guideline for the management of clinically localized prostate cancer: 2007 update. J Urol 2007; 177: 2106–2131.
Heidenreich A, Bellmunt J, Bolla M, Joniau S, Mason M, Matveev V et al. EAU guidelines on prostate cancer. Part 1: screening, diagnosis, and treatment of clinically localised disease. Eur Urol 2011; 59: 61–71.
Resnick MJ, Koyama T, Fan KH, Albertsen PC, Goodman M, Hamilton AS et al. Long-term functional outcomes after treatment for localized prostate cancer. N Engl J Med 2013; 368: 436–445.
Albertsen PC, Hanley JA, Fine J . 20-year outcomes following conservative management of clinically localized prostate cancer. JAMA 2005; 293: 2095–2101.
Johansson JE, Andren O, Andersson SO, Dickman PW, Holmberg L, Magnuson A et al. Natural history of early, localized prostate cancer. JAMA 2004; 291: 2713–2719.
Tosoian JJ, Mamawala M, Epstein JI, Landis P, Wolf S, Trock BJ et al. Intermediate and longer-term outcomes from a prospective active-surveillance program for favorable-risk prostate cancer. J Clin Oncol 2015; 33: 3379–3385.
Klotz L, Vesprini D, Sethukavalan P, Jethava V, Zhang L, Jain S et al. Long-term follow-up of a large active surveillance cohort of patients with prostate cancer. J Clin Oncol 2015; 33: 272–277.
Yamamoto T, Musunuru B, Vesprini D, Zhang L, Ghanem G, Loblaw A et al. Metastatic prostate cancer in men initially treated with active surveillance. J Urol 2016; 195: 1409–1414.
Klotz L . Active surveillance: patient selection. Curr Opin Urol 2013; 23: 239–244.
Onik G, Barzell W . Transperineal 3D mapping biopsy of the prostate: an essential tool in selecting patients for focal prostate cancer therapy. Urol Oncol 2008; 26: 506–510.
Tsivian M, Abern MR, Qi P, Polascik TJ . Short-term functional outcomes and complications associated with transperineal template prostate mapping biopsy. Urology 2013; 82: 166–170.
Arumainayagam N, Ahmed HU, Moore CM, Freeman A, Allen C, Sohaib SA et al. Multiparametric MR imaging for detection of clinically significant prostate cancer: a validation cohort study with transperineal template prostate mapping as the reference standard. Radiology 2013; 268: 761–769.
Rosenkrantz AB, Mendrinos S, Babb JS, Taneja SS . Prostate cancer foci detected on multiparametric magnetic resonance imaging are histologically distinct from those not detected. J Urol 2012; 187: 2032–2038.
Siddiqui MM, Rais-Bahrami S, Turkbey B, George AK, Rothwax J, Shakir N et al. Comparison of MR/ultrasound fusion-guided biopsy with ultrasound-guided biopsy for the diagnosis of prostate cancer. JAMA 2015; 313: 390–397.
Gupta RT, Brown AF, Silverman RK, Tay KJ, Madden JF, George DJ et al. Can radiologic staging with multiparametric MRI enhance the accuracy of the partin tables in predicting organ-confined prostate cancer? AJR Am J Roentgenol 2016; 207: 87–95.
Klotz L, Polascik TJ . Low-risk and very-low-risk prostate cancer: is there a role for focal therapy in the era of active surveillance? Yes, the two approaches complement each other. Oncology (Williston Park) 2014; 28: 950–c3.
Valerio M, Ahmed HU, Emberton M, Lawrentschuk N, Lazzeri M, Montironi R et al. The role of focal therapy in the management of localised prostate cancer: a systematic review. Eur Urol 2014; 66: 732–751.
Tsivian M, Kimura M, Sun L, Mouraviev V, Mayes JM, Polascik TJ . Predicting unilateral prostate cancer on routine diagnostic biopsy: sextant vs extended. BJU Int 2010; 105: 1089–1092.
Linstone HA, Turoff M The Delphi Method: Techniques and Applications. Addison-Wesley Educational Publishers (December 1975): Reading, Mass, 2002..
Kayat Bittencourt L, Litjens G, Hulsbergen-van de Kaa CA, Turkbey B, Gasparetto EL, Barentsz JO . Prostate Cancer: the European Society of Urogenital Radiology Prostate Imaging Reporting and Data System Criteria for Predicting Extraprostatic Extension by Using 3-T Multiparametric MR Imaging. Radiology 2015; 276: 479–489.
de la Rosette J, Ahmed H, Barentsz J, Johansen TB, Brausi M, Emberton M et al. Focal therapy in prostate cancer-report from a consensus panel. J Endourol 2010; 24: 775–780.
Ahmed HU, Akin O, Coleman JA, Crane S, Emberton M, Goldenberg L et al. Transatlantic Consensus Group on active surveillance and focal therapy for prostate cancer. BJU Int 2012; 109: 1636–1647.
Donaldson IA, Alonzi R, Barratt D, Barret E, Berge V, Bott S et al. Focal therapy: patients, interventions, and outcomes—a report from a consensus meeting. Eur Urol 2015; 67: 771–777.
Fu Q, Moul JW, Banez LL, Sun L, Mouraviev V, Xie D et al. Preoperative predictors of pathologic stage T2a in low-risk prostate cancer: implications for focal therapy. Urol Int 2012; 89: 296–300.
Gallina A, Maccagnano C, Suardi N, Capitanio U, Abdollah F, Raber M et al. Unilateral positive biopsies in low risk prostate cancer patients diagnosed with extended transrectal ultrasound-guided biopsy schemes do not predict unilateral prostate cancer at radical prostatectomy. BJU Int 2012; 110 (2 Pt 2): E64–E68.
Fumado L, Cecchini L, Juanpere N, Ubre A, Lorente JA, Alcaraz A et al. Prostate biopsy is an unreliable tool to select patients eligible for focal therapy. Urol Int 2015; 95: 197–202.
Matsuoka Y, Numao N, Saito K, Tanaka H, Kumagai J, Yoshida S et al. Candidate selection for quadrant-based focal ablation through a combination of diffusion-weighted magnetic resonance imaging and prostate biopsy. BJU Int 2016; 117: 94–101.
Tran M, Thompson J, Bohm M, Pulbrook M, Moses D, Shnier R et al. Combination of multiparametric MRI and transperineal template-guided mapping biopsy of the prostate to identify candidates for hemi-ablative focal therapy. BJU Int 2016; 117: 48–54.
Donaldson IA, Alonzi R, Barratt D, Barret E, Berge V, Bott S et al. Focal therapy: patients, interventions, and outcomes-a report from a consensus meeting. Eur Urol 2015; 67: 717–777.
Postema AW, De Reijke TM, Ukimura O, Van den Bos W, Azzouzi AR, Barret E et al. Standardization of definitions in focal therapy of prostate cancer: report from a Delphi consensus project. World J Urol 2016; 34: 1373–1382.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Tay, K., Scheltema, M., Ahmed, H. et al. Patient selection for prostate focal therapy in the era of active surveillance: an International Delphi Consensus Project. Prostate Cancer Prostatic Dis 20, 294–299 (2017). https://doi.org/10.1038/pcan.2017.8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2017.8
This article is cited by
-
Treatment of localized prostate cancer in elderly patients: the role of partial cryoablation
International Urology and Nephrology (2023)
-
Single-center, prospective phase 2 trial of high-intensity focused ultrasound (HIFU) in patients with unilateral localized prostate cancer: good functional results but oncologically not as safe as expected
World Journal of Urology (2023)
-
Reducing the number of systematic biopsy cores in the era of MRI targeted biopsy—implications on clinically-significant prostate cancer detection and relevance to focal therapy planning
Prostate Cancer and Prostatic Diseases (2022)
-
Value of magnetic resonance imaging/ultrasound fusion prostate biopsy to select patients for focal therapy
World Journal of Urology (2022)
-
Focal therapy for prostate cancer—ready to be a standard of care?
Prostate Cancer and Prostatic Diseases (2021)