Abstract
BACKGROUND:
Prevalence of and severity of lower urinary tract symptoms (LUTS) according to male sexual orientation have been scantly analysed. We aimed to assess the prevalence and severity of LUTS in a cohort of Caucasian-European men who have sex with men seeking medical help for uroandrologic reasons other than LUTS.
METHODS:
Data from 949 consecutive individuals in an outpatient setting were analysed. Severity of LUTS was measured with the International Prostate Symptom Score (IPSS). Men with storage symptoms scored 1–3 and ⩾4 (of 15), and voiding symptoms scored 1–4 and ⩾5 (of 20) were considered as having mild and moderate-to-severe symptoms, respectively. For individual symptoms, patients with scores ⩾1 were deemed symptomatic (according to Apostolidis et al.15). Descriptive statistics and logistic regression models tested the association between LUTS and sexual orientation.
RESULTS:
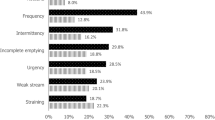
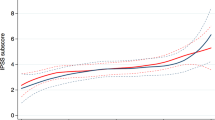
Complete data were available for 213 (22.4%) men who have sex with men (MSM) and 736 (77.6%) heterosexuals (mean age (s.d.): 41.0 (12.2) vs 39.9 (12.1) years). Compared with heterosexuals, MSM reported higher rates of total IPSS scores suggestive of moderate (21.6% vs 20%) and severe LUTS (3.8% vs 2.4%) (P=0.004). Similarly, MSM showed higher rates of mild (48.8% vs 45.2%) and moderate-to-severe (39.4% vs 30.4%) storage symptoms (all P<0.001), and of mild (45.1% vs 34.8%) and moderate-to-severe (20.2% vs 19.2%) voiding symptoms (all P<0.01). MSM status was an independent predictor of mild voiding symptoms (odds ratio (OR): 1.40; P=0.004), moderate-to-severe storage symptoms (OR: 1.40; P=0.04) and severe total IPSS (OR: 1.49; P=0.03), after adjusting for other variables.
CONCLUSIONS:
These findings suggest a higher prevalence and severity of LUTS in MSM compared with heterosexual men seeking medical help for uroandrologic reasons other than LUTS.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Black D, Gates G, Sanders S, Taylor R . Demographics of the gay and lesbian population in the United States: evidence from available systematic data sources. Demography 2000; 37: 139–154.
Siegel K, Schrimshaw EW, Lekas HM, Parsons JT . Sexual behaviors of non-gay identified nondisclosing men who have sex with men and women. Arch Sex Behav 2008; 37: 720–735.
Conron KJ, Mimiaga MJ, Landers SJ . A population-based study of sexual orientation identity and gender differences in adult health. Am J Public Health 2010; 100: 1953–1960.
Metcalfe R, Laird G, Nandwani R . Don't ask, sometimes tell. A survey of men who have sex with men sexual orientation disclosure in general practice. Int J STD AIDS 2014 (e-pub ahead of print).
de Vries HJ . Sexually transmitted infections in men who have sex with men. Clin Dermatol 2014; 32: 181–188.
van Rijn VM, Mooij SH, Mollers M, Snijders PJ, Speksnijder AD, King AJ et al. Anal, penile, and oral high-risk HPV infections and HPV seropositivity in HIV-positive and HIV-negative men who have sex with men. PLoS One 2014; 9: e92208.
Cooper F, Barber T . 'Gay bowel syndrome': relic or real (and returning) phenomenon? Curr Opin Infect Dis 2014; 27: 84–89.
Mao L, Templeton DJ, Crawford J, Imrie J, Prestage JP, Grulich AE et al. Does circumcision make a difference to the sexual experience of gay men? Findings from the Health in Men (HIM) cohort. J Sex Med 2008; 5: 2557–2561.
Bancroft J, Carnes L, Janssen E, Goodrich D, Long JS . Erectile and ejaculatory problems in gay and heterosexual men. Arch Sex Behav 2005; 34: 285–297.
Jern P, Santtila P, Johansson A, Alanko K, Salo B, Sandnabba NK . Is there an association between same-sex sexual experience and ejaculatory dysfunction? J Sex Marital Ther 2010; 36: 303–312.
Hirshfield S, Chiasson MA, Wagmiller RL Jr, Remien RH, Humberstone M, Scheinmann R et al. Sexual dysfunction in an Internet sample of U.S. men who have sex with men. J Sex Med 2010; 7: 3104–3114.
Shindel AW, Vittinghoff E, Breyer BN . Erectile dysfunction and premature ejaculation in men who have sex with men. J Sex Med 2012; 9: 576–584.
Oelke M, Bachmann A, Descazeaud A, Emberton M, Gravas S, Michel MC et al. EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol 2013; 64: 118–140.
Nørby B, Nordling J, Mortensen S . Lower urinary tract symptoms in the Danish population: a population-based study of symptom prevalence, health-care seeking behavior and prevalence of treatment in elderly males and females. Eur Urol 2005; 47: 817–823.
Apostolidis A, Kirana PS, Chiu G, Link C, Tsiouprou M, Hatzichristou D . Gender and age differences in the perception of bother and health care seeking for lower urinary tract symptoms: results from the hospitalised and outpatients' profile and expectations study. Eur Urol 2009; 56: 937–947.
Agarwal A, Eryuzlu LN, Cartwright R, Thorlund K, Tammella TM, Guyatt GH et al. What is the most bothersome lower urinary tract symptom? Individual- and population-level perspectives for both men and women. Eur Urol 2014; 65: 1211–1217.
Breyer BN, Vittinghoff E, Van Den Eeden SK, Erickson BA, Shindel AW . Effect of sexually transmitted infections, lifetime sexual partner count, and recreational drug use on lower urinary tract symptoms in men who have sex with men. Urology 2012; 79: 188–193.
Charlson ME, Pompei P, Ales KL, MacKenzie CR . A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40: 373–383.
National Institutes of Health, National Heart, Lung, and Blood Institute. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—The Evidence Report. Obes Res 1998; 6: 51–210S.
Sutcliffe S, Rohrmann S, Giovannucci E, Nelson KE, De Marzo AM, Isaacs WB et al. Viral infections and lower urinary tract symptoms in the third national health and nutrition examination survey. J Urol 2007; 178: 2181–2185.
St Sauver JL, Jacobson DJ, McGree ME, Girman CJ, Lieber MM, Jacobsen SJ . Longitudinal association between prostatitis and development of benign prostatic hyperplasia. Urology 2008; 71: 475–479.
Signorello LB, Tzonou A, Lagiou P, Samoli E, Zavitsanos X, Trichopoulos D . The epidemiology of benign prostatic hyperplasia: a study in Greece. BJU Int 1999; 84: 286–291.
St Sauver JL, Sarma AV, Jacobson DJ, McGree ME, Lieber MM, Girman CJ et al. Associations between C-reactive protein and benign prostatic hyperplasia/lower urinary tract symptom outcomes in a population-based cohort. Am J Epidemiol 2009; 169: 1281–1290.
Sutcliffe S, Giovannucci E, De Marzo AM, Willett WC, Platz EA . Sexually transmitted infections, prostatitis, ejaculation frequency, and the odds of lower urinary tract symptoms. Am J Epidemiol 2005; 162: 898–906.
Gandaglia G, Briganti A, Gontero P, Mondaini N, Novara G, Salonia A et al. The role of chronic prostatic inflammation in the pathogenesis and progression of benign prostatic hyperplasia (BPH). BJU Int 2013; 112: 432–441.
Mills TC, Paul J, Stall R, Pollack L, Canchola J, Chang YJ et al. Distress and depression in men who have sex with men: The Urban Men’s Health Study. Am J Psychiatry 2004; 161: 278–285.
Skeldon SC, Goldenberg SL . Urological complications of illicit drug use. Nat Rev Urol 2014; 11: 169–177.
Forster JA, Harrison SC . Ketamine uropathy: rising to the challenges of a new condition. BJU Int 2012; 109: 1277–1278.
Blank TO . The challenge of prostate cancer: half a man or a man and a half? Generations 2008; 32: 68–72.
Wassersug RJ, Lyons A, Duncan D, Dowsett GW, Pitts M . Diagnostic and outcome differences between heterosexual and non heterosexual men treated for prostate cancer. Urology 2013; 82: 565–571.
Hart TL, Coon DW, Kowalkowski MA, Zhang K, Hersom JI, Golz HH et al. Changes in sexual roles and quality of life for gay men after prostate cancer: challenges for sexual health providers. J Sex Med 2014; 11: 2308–2317.
Cinar A, Hall SA, Link CL, Kaplan SA, Kopp ZS, Roehrborn CG et al. Cluster analysis and lower urinary tract symptoms in men: findings from the Boston Area Community Health Survey. BJU Int 2008; 101: 1247–1256.
Acknowledgements
We thank Dana Kuefner, PhD, for reviewing the language in this manuscript. This study was approved by the Ethical committee of San Raffaele Hospital and all participants provided their informed consent before participation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Boeri, L., Capogrosso, P., Ventimiglia, E. et al. Lower urinary tract symptoms among Caucasian-European men who have sex with men: findings from a real-life survey. Prostate Cancer Prostatic Dis 18, 376–381 (2015). https://doi.org/10.1038/pcan.2015.41
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2015.41
This article is cited by
-
Understanding Prostate Cancer in Gay, Bisexual, and Other Men Who Have Sex with Men and Transgender Women: A Review of the Literature
Current Sexual Health Reports (2019)