Abstract
Background:
To assess the added value of biopsy factors, like maximum cancer length in a core (MCL), cumulative cancer length (CCL), cumulative length of positive cores (CLPC), percentage of cancer involvement in positive cores (CIPC) and the Prostate Cancer Research International: Active Surveillance (PRIAS) criteria in patients who underwent radical prostatectomy (RP) but eligible for active surveillance (AS).
Methods:
From January 2002 to December 2007, 750 consecutive subjects underwent RP. We identified 147 (19.07%) patients who were eligible for AS based on PRIAS criteria: clinical stage T1c or T2, PSA level of⩽10 ng ml−1, Gleason score ⩽6, PSA-D of <0.2 ng ml−2 and one or two positive biopsy cores. We calculated the diagnostic accuracy of biopsy factors in determining pathological confirmed unfavorable disease. Decision curve analysis (DCA) were performed.
Results:
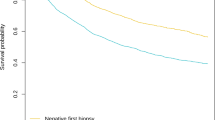
Of all subjects, 95 patients (66.43%) had favorable whereas 48 had (33.57%) unfavorable disease. On multivariate analyses, the inclusion of MCL, CCL, CLPC and CIPC significantly increased the accuracy of the base multivariate model in predicting unfavorable disease. The gain in predictive accuracy for MCL in a core, CCL, CLPC and CIPC ranged from 13 to 27%. The DCA shows that adding MCL, CCL, CLPC and CIPC resulted in a greater net benefit when the probability of ranges between 15 and 50%. The models can be applied at the cost of missing not more than 16.83% of unfavorable disease.
Conclusions:
Our findings suggested that the addition of these biopsy factors to PRIAS criteria has the potential to significantly increase the ability to detect unfavorable disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Schroder FH, Hugosson J, Roobol MJ, Tammela TL, Ciatto S, Nelen V et al. Prostate-cancer mortality at 11 years of follow-up. N Engl J Med 2012; 366: 981–990.
Hugosson J, Carlsson S, Aus G, Bergdahl S, Khatami A, Lodding P et al. Mortality results from the Goteborg randomised population-based prostate-cancer screening trial. Lancet Oncol 2010; 11: 725–732.
Wong LM, Ferrara S, Alibhai SM, Evans A, Van der Kwast T, Trottier G et al. Diagnostic prostate biopsy performed in a non-academic center increases the risk of re-classification at confirmatory biopsy for men considering active surveillance for prostate cancer. Prostate Cancer Prostatic Dis 2015; 18: 69–74.
Wong LM, Neal DE, Finelli A, Davis S, Bonner C, Kapoor J et al. Evaluation of models predicting insignificant prostate cancer to select men for active surveillance of prostate cancer. Prostate Cancer Prostatic Dis 2015; (e-pub ahead of print).
Gorin MA, Eldefrawy A, Ekwenna O, Soloway MS . Active surveillance for low-risk prostate cancer: knowledge, acceptance and practice among urologists. Prostate Cancer Prostatic Dis 2012; 15: 177–181.
Tseng KS, Landis P, Epstein JI, Trock BJ, Carter HB . Risk stratification of men choosing surveillance for low risk prostate cancer. J Urol 2010; 183: 1779–1785.
Louie-Johnsun M, Neill M, Treurnicht K, Jarmulowicz M, Eden C . Final outcomes of patients with low-risk prostate cancer suitable for active surveillance but treated surgically. BJU Int 2009; 104: 1501–1504.
Mufarrij P, Sankin A, Godoy G, Lepor H . Pathologic outcomes of candidates for active surveillance undergoing radical prostatectomy. Urology 2010; 76: 689–692.
Iremashvili V, Pelaez L, Manoharan M, Jorda M, Rosenberg DL, Soloway MS . Pathologic prostate cancer characteristics in patients eligible for active surveillance: a head-to-head comparison of contemporary protocols. Eur Urol 2012; 62: 462–468.
Russo GI, Cimino S, Castelli T, Favilla V, Urzi D, Veroux M et al. Percentage of cancer involvement in positive cores can predict unfavorable disease in men with low-risk prostate cancer but eligible for the prostate cancer international: active surveillance criteria. Urol Oncol 2014; 32: 291–296.
Vickers AJ, Elkin EB . Decision curve analysis: a novel method for evaluating prediction models. Med Decis Making 2006; 26: 565–574.
El Hajj A, Ploussard G, de la Taille A, Allory Y, Vordos D, Hoznek A et al. Analysis of outcomes after radical prostatectomy in patients eligible for active surveillance (PRIAS). BJU Int 2013; 111: 53–59.
Bul M, Zhu X, Valdagni R, Pickles T, Kakehi Y, Rannikko A et al. Active surveillance for low-risk prostate cancer worldwide: the PRIAS study. Eur Urol 2013; 63: 597–603.
Cantiello F, Russo GI, Ferro M, Cicione A, Cimino S, Favilla V et al. Prognostic accuracy of prostate health index and urinary prostate cancer antigen 3 in predicting pathologic features after radical prostatectomy. Urol Oncol 2015; 33: 163.e15–23.
Boccon-Gibod L, van der Kwast TH, Montironi R, Bono A . Handling and pathology reporting of prostate biopsies. Eur Urol 2004; 46: 177–181.
Obek C, Doganca T, Erdal S, Erdogan S, Durak H . Core length in prostate biopsy: size matters. J Urol 2012; 187: 2051–2055.
Loeb S, Bruinsma SM, Nicholson J, Briganti A, Pickles T, Kakehi Y et al. Active surveillance for prostate cancer: a systematic review of clinicopathologic variables and biomarkers for risk stratification. Eur Urol 2014; pii S0302-2838(14)01018-5.
Moore CM, Robertson NL, Arsanious N, Middleton T, Villers A, Klotz L et al. Image-guided prostate biopsy using magnetic resonance imaging-derived targets: a systematic review. Eur Urol 2013; 63: 125–140.
Pinto F, Totaro A, Calarco A, Sacco E, Volpe A, Racioppi M et al. Imaging in prostate cancer diagnosis: present role and future perspectives. Urol Int 2011; 86: 373–382.
Robertson NL, Hu Y, Ahmed HU, Freeman A, Barratt D, Emberton M . Prostate cancer risk inflation as a consequence of image-targeted biopsy of the prostate: a computer simulation study. Eur Urol 2014; 65: 628–634.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Prostate Cancer and Prostatic Diseases website
Supplementary information
Rights and permissions
About this article
Cite this article
Russo, G., Castelli, T., Favilla, V. et al. Performance of biopsy factors in predicting unfavorable disease in patients eligible for active surveillance according to the PRIAS criteria. Prostate Cancer Prostatic Dis 18, 338–342 (2015). https://doi.org/10.1038/pcan.2015.26
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2015.26