Abstract
Background:
Limited information is known about the clinical significance of cancers diagnosed upon repeat biopsy for the indication of atypical small acinar proliferation (ASAP). With increasing concern regarding overdiagnosis and overtreatment of prostate cancer, and the reported rise in infectious complications related to prostate biopsy, we examined the outcomes of patients rebiopsied for a diagnosis of ASAP.
Methods:
Clinical, pathologic and outcomes data of patients diagnosed with ASAP on prostate biopsy at our institutions between 2000 and 2010 were abstracted through chart review. Statistical analyses included Fisher’s exact and the two-sample Wilcoxon rank sum tests. Logistic regression evaluated risk factors for the probability of cancer following a diagnosis of ASAP.
Results:
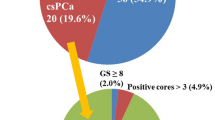
A total of 349 patients met the inclusion criteria with median follow-up of 4.4 years. Median age was 65.3 years with a median PSA of 5.3 ng ml–1. Of men diagnosed with ASAP, 250/349 (71.6%) had a repeat biopsy within 1 year with 94/246 (38.2%) demonstrating prostate cancer; only 26/245 (10.6%) had ⩾Gleason 7 disease. Of men diagnosed with ASAP, 284/349 (81.4%) underwent biopsy at some time during follow-up. Prostate cancer was diagnosed in 132/279 (47.3%) of these men, 48/278 (17.3%) with ⩾Gleason 7 disease. Multivariate analyses suggested that older age, no previous biopsy and PSA density were predictive of cancer on repeat biopsy within 1 year from ASAP. Univariate analysis revealed PSA density was associated with the presence of ⩾Gleason 7 disease at 1 year and any time after a diagnosis of ASAP.
Conclusions:
The overall rate of intermediate- and high-grade prostate cancer found on repeat biopsy for ASAP is low. Further investigation into ways to further risk stratify these men may be warranted. However, until such tests become available, repeat biopsy of men diagnosed with ASAP remains prudent.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Siegel R, Naishadham D, Jemal A . Cancer statistics. 2013 CA Cancer J Clin 2013; 63: 11–30.
Andriole GL, Grubb RL III, Buys SS, Chia D, Church TR, Fouad MN et al. Mortality results from a randomized prostate-cancer screening trial. N Engl J Med 2009; 360: 1310–1319.
Schroder FH, Hugosson J, Roobol MJ, Tammela TLJ, Ciatto S, Nelen V et al. Screening and prostate-cancer mortality in a randomized european study. N Engl J Med 2009; 360: 1320–1328.
Mosharafa AA, Torky MH, El Said WM, Meshref A . Rising incidence of acute prostatitis following prostate biopsy: fluoroquinolone resistance and exposure is a significant risk factor. Urology 2011; 78: 511–514.
Zaytoun OM, Vargo EH, Rajan R, Berglund R, Gordon S, Jones JS . Emergence of fluoroquinolone-resistant Escherichia coli as cause of postprostate biopsy infection: implications for prophylaxis and treatment. Urology 2011; 77: 1035–1041.
Iczkowski KA, Bassler TJ, Schwob VS, Bassler IC, Kunnel BS, Orozco RE et al. Diagnosis of “suspicious for malignancy” in prostate biopsies: predictive value for cancer. Urology 1998; 51: 749–757; discussion 57–58.
Ouyang RC, Kenwright DN, Nacey JN, Delahunt B . The presence of atypical small acinar proliferation in prostate needle biopsy is predictive of carcinoma on subsequent biopsy. BJU Int 2001; 87: 70–74.
Epstein JI, Herawi M . Prostate needle biopsies containing prostatic intraepithelial neoplasia or atypical foci suspicious for carcinoma: implications for patient care. J Urol 2006; 175: 820–834.
Moyer VA . Force USPST. Screening for prostate cancer: U.S. preventive services task force recommendation statement. Ann Intern Med 2012; 157: 120–134.
Carter HB, Albertsen PC, Barry MJ, Etzioni R, Freedland SJ, Greene KL et al. Early detection of prostate cancer: AUA guideline. J Urol 2013; 190: 419–426.
Ehdaie B, Vertosick E, Spaliviero M, Giallo-Uvino A, Taur Y, O'Sullivan M et al. The impact of repeat biopsies on infectious complications in men with prostate cancer on active surveillance. J Urol 2014; 191: 660–664.
Hoedemaeker RF, Kranse R, Rietbergen JB, Kruger AE, Schroder FH, van der Kwast TH . Evaluation of prostate needle biopsies in a population-based screening study: the impact of borderline lesions. Cancer 1999; 85: 145–152.
Chan TY, Epstein JI . Follow-up of atypical prostate needle biopsies suspicious for cancer. Urology 1999; 53: 351–355.
Chen YB, Pierorazio PM, Epstein JI . Initial atypical diagnosis with carcinoma on subsequent prostate needle biopsy: findings at radical prostatectomy. J Urol 2010; 184: 1953–1957.
Pinto PA, Chung PH, Rastinehad AR, Baccala AA Jr ., Kruecker J, Benjamin CJ et al. Magnetic resonance imaging/ultrasound fusion guided prostate biopsy improves cancer detection following transrectal ultrasound biopsy and correlates with multiparametric magnetic resonance imaging. J Urol 2011; 186: 1281–1285.
Vourganti S, Rastinehad A, Yerram NK, Nix J, Volkin D, Hoang A et al. Multiparametric magnetic resonance imaging and ultrasound fusion biopsy detect prostate cancer in patients with prior negative transrectal ultrasound biopsies. J Urol 2012; 188: 2152–2157.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Warlick, C., Feia, K., Tomasini, J. et al. Rate of Gleason 7 or higher prostate cancer on repeat biopsy after a diagnosis of atypical small acinar proliferation. Prostate Cancer Prostatic Dis 18, 255–259 (2015). https://doi.org/10.1038/pcan.2015.14
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2015.14
This article is cited by
-
Clinical strategy of repeat biopsy in patients with atypical small acinar proliferation (ASAP)
Scientific Reports (2021)
-
Managing high-grade prostatic intraepithelial neoplasia (HGPIN) and atypical glands on prostate biopsy
Nature Reviews Urology (2018)
-
Atypical small acinar proliferation at index prostate biopsy: rethinking the re-biopsy paradigm
International Urology and Nephrology (2018)
-
Incidence, grade and distribution of prostate cancer following transperineal template-guided mapping biopsy in patients with atypical small acinar proliferation
World Journal of Urology (2017)
-
Atypical small acinar proliferation (ASAP): Is a repeat biopsy necessary ASAP? A multi-institutional review
Prostate Cancer and Prostatic Diseases (2016)