Abstract
Background:
The Affordable Care Act (ACA) aims to expand health insurance coverage to over 30 million previously uninsured Americans. To help evaluate the potential impact of the ACA on prostate cancer care, we examined the associations between insurance coverage and prostate cancer outcomes among men <65 years old who are not yet eligible for Medicare.
Methods:
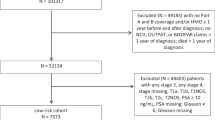
The Surveillance, Epidemiology and End Results Program was used to identify 85 203 men aged <65 years diagnosed with prostate cancer from 2007 to 2010. Multivariable logistic regression modeled the association between insurance status and stage at presentation. Among men with high-risk disease, the associations between insurance status and receipt of definitive therapy, prostate cancer-specific mortality (PCSM) and all-cause mortality were determined using multivariable logistic, Fine and Gray competing-risks and Cox regression models, respectively.
Results:
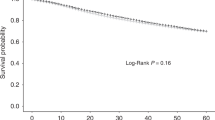
Uninsured patients were more likely to be non-white and come from regions of rural residence, lower median household income and lower education level (P<0.001 for all cases). Insured men were less likely to present with metastatic disease (adjusted odds ratio (AOR) 0.23; 95% confidence interval (CI) 0.20–0.27; P<0.001). Among men with high-risk disease, insured men were more likely to receive definitive treatment (AOR 2.29; 95% CI 1.81–2.89; P<0.001), and had decreased PCSM (adjusted hazard ratio 0.56; 95% CI 0.31–0.98; P=0.04) and all-cause mortality (adjusted hazard ratio 0.60; 0.39–0.91; P=0.01).
Conclusions:
Insured men with prostate cancer are less likely to present with metastatic disease, more likely to be treated if they develop high-risk disease and are more likely to survive their cancer, suggesting that expanding health coverage under the ACA may significantly improve outcomes for men with prostate cancer who are not yet eligible for Medicare.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
United States Census Bureau. Census 2000 Gateway. [online database] Available at http://www.census.gov/main/www/cen2000html. Accessed 27 December 2013.
Patient Protection and Affordable Care Act. Pub. L. No. 111-148, 114 Stat. 119 (210).
Sommers BD, Bindman AB . New physicians, the Affordable Care Act, and the changing practice of medicine. JAMA 2012; 307: 1697–1698.
Ferris LW, Farber M, Guidi TU, Laffey WJ . Impact of health care reform on the cancer patient: a view from cancer executives. Cancer J 2010; 16: 600–605.
Keegan KA, Penson DF . The Patient Protection and Affordable Care Act: the impact on urologic cancer care. Urol Oncol 2013; 31: 980–984.
Albright HW, Moreno M, Feeley TW, Walter R, Samuels M, Pereira A et al. The implications of the 2010 Patient Protection and Affordable Care Act and the Health Care and Education Reconciliation Act on cancer care delivery. Cancer 2011; 117: 1564–1574.
Siegel R, Ma J, Zou Z, Jemal A . Cancer statistics, 2014. CA Cancer J Clin 2014; 64: 9–29.
SEER Cancer Statistics Review, 1975-2010 National Cancer Institute: Bethesda, MDhttp://seer.cancer.gov/csr/1975_2010/based on November 2012 SEER data submission, posted to the SEER website 2013.
Surveillance, Epidemiology, and End Results (SEER) Program. Research Data (1973-2010), National Cancer Institute, DCCPS, Surveillance Research Program, Surveillance Systems Branch, based on November 2012 SEER data submission, posted to the SEER website 2013. www.seer.cancer.gov.
NCCN Clinical Practice Guidelines in Oncology. Prostate Cancer 2014. Available at http://www.nccn.org. Accessed 30 December 2013.
United States Department of Agriculture Rural-Urban Continuum Codes. [online database] Available at http://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx. Accessed 27 December 2013.
Boorjian SA, Karnes RJ, Rangel LJ, Bergstralh EJ, Blute ML . Mayo Clinic validation of the D'amico risk group classification for predicting survival following radical prostatectomy. J Urol 2008; 179: 1354–1360.
Cox DR . Regression models and life-tables. J R Stat Soc B 1972; 34: 187–220.
Fine J, Gray R . A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 1999; 94: 496–509.
Shen JJ, Washington EL . Disparities in outcomes among patients with stroke associated with insurance status. Stroke 2007; 38: 1010–1016.
Glueckert LN, Redden D, Thompson MA, Haque A, Gray SH, Locke J et al. What liver transplant outcomes can be expected in the uninsured who become insured via the Affordable Care Act? Am J Transplant 2013; 13: 1533–1540.
Hasan O, Orav EJ, Hicks LS . Insurance status and hospital care for myocardial infarction, stroke, and pneumonia. J Hosp Med 2010; 5: 452–459.
Shi L, Lebrun LA, Zhu J, Tsai J . Cancer screening among racial/ethnic and insurance groups in the United States: a comparison of disparities in 2000 and 2008. J Health Care Poor Underserved 2011; 22: 945–961.
Ayanian JZ, Kohler BA, Abe T, Epstein AM . The relation between health insurance coverage and clinical outcomes among women with breast cancer. N Engl J Med 1993; 329: 326–331.
Trinh QD, Schmitges J, Sun M, Sammon J, Shariat SF, Zorn K et al. Morbidity and mortality of radical prostatectomy differs by insurance status. Cancer 2012; 118: 1803–1810.
Kelz RR, Gimotty PA, Polsky D, Norman S, Fraker D, DeMichele A . Morbidity and mortality of colorectal carcinoma surgery differs by insurance status. Cancer 2004; 101: 2187–2194.
Brookfield KF, Cheung MC, Lucci J, Fleming LE, Koniaris LG . Disparities in survival among women with invasive cervical cancer: a problem of access to care. Cancer 2009; 115: 166–178.
Dasenbrock HH, Wolinsky JP, Sciubba DM, Witham TF, Gokaslan ZL, Bydon A . The impact of insurance status on outcomes after surgery for spinal metastases. Cancer 2012; 118: 4833–4841.
Fedewa SA, Etzioni R, Flanders WD, Jemal A, Ward EM . Association of insurance and race/ethnicity with disease severity among men diagnosed with prostate cancer, National Cancer Database 2004-2006. Cancer Epidemiol Biomarkers Prev 2010; 19: 2437–2444.
Sadetsky N, Lubeck DP, Pasta DJ, Latini DM, DuChane J, Carroll PR . Insurance and quality of life in men with prostate cancer: data from the Cancer of the Prostate Strategic Urological Research Endeavor. BJU Int 2008; 101: 691–697.
Gallina A, Karakiewicz P, Chunk FK, Briganti A, Graefen M, Montorsi F et al. Health-insurance status is a determinant of the stage at presentation and of cancer control in European men treated with radical prostatectomy for clinically localized prostate cancer. BJU Int 2007; 99: 1404–1408.
Penson DF, Stoddard ML, Pasta DJ, Lubeck DP, Flanders SC, Litwin MS . The association between socioeconomic status, health insurance coverage, and quality of life in men with prostate cancer. J Clin Epidemiol 2001; 54: 350–358.
Roetzheim RG, Pal N, Tennant C, Voti L, Ayanian JZ, Schwabe A et al. Effects of health insurance and race on early detection of cancer. J Natl Cancer Inst 1999; 91: 1409–1415.
Niu X, Roche LM, Pawlish KS, Henry KA . Cancer survival disparities by health insurance status. Cancer Med 2013; 2: 403–411.
Cooperberg MR, Lubeck DP, Meng MV, Mehta SS, Carroll PR . The changing face of low-risk prostate cancer: trends in clinical presentation and primary management. J Clin Oncol 2004; 22: 2141–2149.
Miller DC, Litwin MS, Bergman J, Stepanian S, Connor SE, Kwan L et al. Prostate cancer severity among low income, uninsured men. J Urol 2009; 181: 579–583.
Brown ER, Davidson PL, Yu H, Wyn R, Andersen RM, Becerra L et al. Effects of community factors on access to ambulatory care for lower-income adults in large urban communities. Inquiry 2004; 41: 39–56.
Stein JA, Andersen RM, Gelberg L . The Behavioral Model for Vulnerable Populations: application to medical care use and outcomes for homeless people. Health Serv Res 2000; 34: 1273–1302.
Miller DC, Gelberg L, Kwan L, Stepanian S, Fink A, Andersen RM et al. Racial disparities in access to care for men in a public assistance program for men in a public assistance program for prostate cancer. J Community Health 2008; 33: 318–335.
Andersen RM, Yu H, Wyn R, Davidson PL, Brown ER, Teleki S . Access to medical care for low-income persons: how do communities make a difference? Med Care Res Rev 2002; 59: 384–411.
Underwood W, De Monner S, Ubel P, Fagerlin A, Sanda MG, Wei JT . Racial/ethnic disparities in the treatment of localized/regional prostate cancer. J Urol 2004; 171: 1504–1507.
Presley CJ, Raldow AC, Cramer LD, Soulos PR, Long JB, Yu JB et al. A new approach to understanding racial disparities in prostate cancer treatment. J Geriatr Oncol 2013; 4: 1–8.
Hamilton AS, Fleming ST, Wang D, Goodman M, Wu XC, Owen JB et al. Clinical and demographic factors associated with receipt of non guideline-concordant initial therapy for nonmetastatic prostate cancer. Am J Clin Oncol 2014; e-pub ahead of print (Accessed 1 February 2014).
Stokes WA, Hendrix LH, Royce TJ, Allen IM, Godley PA, Wang AZ et al. Racial differences in time from prostate cancer diagnosis to treatment initiation: a population-based study. Cancer 2013; 119: 2486–2493.
Tewari AK, Gold HT, Demers RY, Johnson CC, Yadav R, Wagner EH et al. Effect of socioeconomic factors on long-term mortality in men with clinically localized prostate cancer. Urology 2009; 73: 624–630.
Mahal BA, Ziehr DR, Aizer AA, Hyatt AS, Sammon JD, Schmid M et al. The influence of insurance status on racial disparities in the treatment of African-American men with high-risk prostate cancer. Urol Oncol 2014; e-pub ahead of print (Accessed 1 May 2014).
Steelfisher GK, Blendon RJ, Sussman T, Connolly JM, Benson JM, Herrmann MJ . Physicians’ views of the Massachusetts Health Care Reform Law—a poll. N Engl J Med 2009; 361: e39.
Staiger DO, Auerbach DI, Buerhaus PI . Health care reform and the health care workforce—the Massachusetts experience. N Engl J Med 2011; 365: e24.
Wilensky GR . The shortfalls of ‘Obamacare’. N Engl J Med 2012; 367: 1479–1481.
Moyer VA . Screening for prostate cancer: U.S. Preventative Services Task Force recommendation statement. Ann Intern Med 2012; 157: 120–134.
Acknowledgements
This work is supported by David and Cynthia Chapin, the Prostate Cancer Foundation, Fitz’s Cancer Warriors, Hugh Simons in honor of Frank and Anne Simons and a grant from an anonymous family foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Paul L Nguyen consulted for Ferring and Medivation, and Quoc-Dien Trinh gave a paid lecture for Intuitive Surgical. The other authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Mahal, B., Aizer, A., Ziehr, D. et al. The association between insurance status and prostate cancer outcomes: implications for the Affordable Care Act. Prostate Cancer Prostatic Dis 17, 273–279 (2014). https://doi.org/10.1038/pcan.2014.23
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2014.23
This article is cited by
-
A qualitative study of barriers and facilitators for health behavior change in low-income men with prostate cancer
Supportive Care in Cancer (2024)
-
Price transparency of prostate cancer care in the United States: An analysis of pricing and disclosure following the centers for medicare and medicaid mandate
Prostate Cancer and Prostatic Diseases (2023)
-
Five-year survival of patients with late-stage prostate cancer: comparison of the Military Health System and the U.S. general population
British Journal of Cancer (2023)
-
Patient-reported outcomes before treatment for localized prostate cancer: are there differences among countries? Data from the True North Global Registry
BMC Urology (2023)
-
Prostate Cancer Screening and Young Black Men: Can Early Communication Avoid Later Health Disparities?
Journal of Cancer Education (2022)