Abstract
Background:
Epidemiological data indicate that lower urinary tract symptoms (LUTS)/BPH can be associated with metabolic syndrome (MetS). Chronic inflammation has been proposed as a candidate mechanism at the crossroad between these two clinical entities.
Aim of study is to examine the correlation among pre-operatory LUTS/BPH severity, MetS features and inflammatory infiltrates in prostatectomy specimens.
Methods:
A total of 271 consecutive men treated with simple prostatectomy were retrospectively selected for this study in two tertiary referral centers for LUTS/BPH. Prostate diameters and volume were measured by transrectal ultrasound, LUTS scored by International Prostate Symptom Score (IPSS) and obstruction by uroflowmetry. The International Diabetes Federation and American Heart Association and the National Heart, Lung and Blood Institute was used to define MetS. The inflammatory infiltrate was investigated combining anatomic location, grade and extent of flogosis into the overall inflammatory score (IS); the glandular disruption (GD) was used as a further marker.
Results:
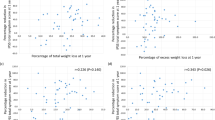
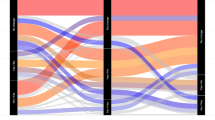
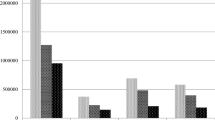
Eighty-six (31.7%) men were affected by MetS. Prostatic volume and anterior-posterior (AP) diameter were positively associated to the number of MetS components. Among MetS determinants, only dyslipidaemia (increased serum triglycerides and reduced serum high-density lipoprotein) was associated with an increased risk of having a prostatic volume >60 cm3 (hazard ratio (HR)=3.268, P<0.001). A significant positive correlation between the presence of MetS and the IS was observed. MetS patients presented lower uroflowmetric parameters as compared with those without MetS (Maximum flow rate (Qmax): 8.6 vs 10.1, P=0.008 and average flow rate (Qave): 4.6 vs 5.3, P=0.033, respectively), and higher obstructive urinary symptoms score (P=0.064). A positive correlation among both IS–GD and IPSS Score was also observed (adjusted r=0.172, P=0.008 and adjusted r=0.128, P=0.050).
Conclusions:
MetS is associated with prostate volume, prostatic AP diameter and intraprostatic IS. The significantly positive association between MetS and prostatic AP diameter could support the observation that MetS patients presented lower uroflowmetric parameters. In conclusion, MetS can be regarded as a new determinant of prostate inflammation and BPH progression.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Gacci M, Eardley I, Giuliano F, Hatzichristou D, Kaplan SA, Maggi M et al. Critical analysis of the relationship between sexual dysfunctions and lower urinary tract symptoms due to benign prostatic hyperplasia. Eur Urol 2011; 60: 809–825.
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U et al. Standardisation sub-committee of the International Continence Society. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology 2003; 61: 37–49.
Samdeep M, Kevin T . McVary Lower urinary tract symptoms, obesity and the metabolic syndrome. Curr Opin Urol 2010; 20: 7–12.
Roherborn CG . Pathology of benign prostatic hyperplasia. Int J Impot Res 2008; 20 (Suppl 3): S11–S18.
Hammarsten J, Högstedt B, Holthuis N, Mellström D . Components of the metabolic syndrome-risk factors for the development of benign prostatic hyperplasia. Prostate Cancer Prostatic Dis 1998; 1: 157–162.
Hammarsten J, Högstedt B . Calculated fast-growing benign prostatic hyperplasia—a risk factor for developing clinical prostate cancer. Scand J Urol Nephrol 2002; 36: 330–338.
Nandeesha H, Koner BC, Dorairajan LN, Sen SK . Hyperinsulinemia and dyslipidaemia in non-diabetic benign prostatic hyperplasia. Clin Chim Acta 2006; 370: 89–93.
Dahle SE, Chokkalingam AP, Gao YT, Deng J, Stanczyk FZ, Hsing AW . Body size and serum levels of insulin and leptin in relation to the risk of benign prostatic hyperplasia. J Urol 2002; 168: 599–604.
Ozden C, Ozdal OL, Urgancioglu G, Koyuncu H, Gokkaya S, Memis A . The correlation between metabolic syndrome and prostatic growth in patients with benign prostatic hyperplasia. Eur Urol 2007; 51: 199–203.
De Nunzio C, Aronson W, Freedland SJ, Giovannucci E, Parsons JK . The correlation between metabolic syndrome and prostatic diseases. Eur Urol 2012; 61: 560–570.
De Nunzio C, Kramer G, Marberger M, Montironi R, Nelson W, Schröder F et al. The controversial relationship between benign prostatic hyperplasia and prostate cancer: the role of inflammation. Eur Urol 2011; 60: 106–117.
Gacci M, Bartoletti R, Figlioli S, Sarti E, Eisner B, Boddi V et al. Urinary symptoms, quality of life and sexual function in patients with benign prostatic hypertrophy before and after prostatectomy: a prospective study. BJU Int 2003; 91: 196–200.
Tubaro A, Carter S, Hind A, Vicentini C, Miano L . A prospective study of the safety and efficacy of suprapubic transvesical prostatectomy in patients with benign prostatic hyperplasia. J Urol 2001; 166: 172–176.
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA et alInternational Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; International Association for the Study of Obesity. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009; 120: 1640–1645.
Corona G, Mannucci E, Petrone L, Schulman C, Balercia G, Fisher AD et al. A comparison of NCEP-ATPIII and IDF metabolic syndrome definitions with relation to metabolic syndrome-associated sexual dysfunction. J Sex Med 2007; 4: 789–796.
Curtis Nickel J . Inflammation and benign prostatic hyperplasia. Urol Clin North Am 2008; 35: 109–115.
Smith AD, Badlani G, Preminger GM, Kavoussi LR . Smith’s Textbook of Endourology 3rd edn 2011.
Aarnink RG, de la Rosette JJ, Huynen AL, Giesen RJ, Debruyne FM, Wijkstra H . Standardized assessmet to enhance the diagnostic value of prostate volume; part i: morphometry in patients with lower urinary tract symptoms. Prostate 29: 317–326 1996.
Boyle P, Gould AL, Roehrborn CG . Prostate volume predicts outcome of treatment of benign prostatic hyperplasia with finasteride: meta-analysis of randomized clinical trials. Urology 1996; 48: 398–405.
Rove KO, Sullivan KF, Crawford ED . High-intensity focused ultrasound: ready for primetime. Urol Clin North Am 2010; 37: 27–35.
Hammarsten J, Hogstedt B . Hyperinsulinemia as a risk factor for developing benign prostatic hyperplasia. Eur Urol 2001; 39: 151–158.
Parsons JK, Carter HB, Partin AW, Windham BG, Metter EJ, Ferrucci L et al. Metabolic factors associated with benign prostatic hyperplasia. J Clin Endocrinol Metab 2006; 91: 2562–2568.
Lee RK, Chung D, Chughtai B, Te AE, Kaplan SA . Central obesity as measured by waist circumference is predictive of severity of lower urinary tract symptoms. BJU Int 2012; 110: 540–545.
Fibbi B, Penna G, Morelli A, Adorini L, Maggi M . Chronic inflammation in the pathogenesis of benign prostatic hyperplasia. Int J Androl 2010; 33: 475–488.
Schauer IG, Rowley DR . The functional role of reactive stroma in benign prostatic hyperplasia. Differentiation 2011; 82: 200–210.
Nickel JC, Roehrborn CG, O'Leary MP, Bostwick DG, Somerville MC, Rittmaster RS . The relationship between prostate inflammation and lower urinary tract symptoms: examination of baseline data from the REDUCE trial. Eur Urol 2008; 54: 1379–1384.
Roehrborn CG . Benign prostatic hyperplasia: an overview. Rev Urol 2005; 7 (Suppl 9): S3–S14.
Vignozzi L, Morelli A, Sarchielli E, Comeglio P, Filippi S, Cellai I et al. Testosterone protects from metabolic syndrome-associated prostate inflammation: an experimental study in rabbit. J Endocrinol 2012; 212: 71–84.
Morelli A, Comeglio P, Filippi S, Sarchielli E, Cellai I, Vignozzi L et al. Testosterone and farnesoid X receptor agonist INT-747 counteract high fat diet-induced bladder alterations in a rabbit model of metabolic syndrome. J Steroid Biochem Mol Biol 2012; 132: 80–92.
Filippi S, Vignozzi L, Morelli A, Chavalmane AK, Sarchielli E, Fibbi B et al. Testosterone partially ameliorates metabolic profile and erectile responsiveness to PDE5 inhibitors in an animal model of male metabolic syndrome. J Sex Med 2009; 6: 3274–3288.
Vignozzi L, Morelli A, Filippi S, Comeglio P, Chavalmane AK, Marchetta M et al. Farnesoid X receptor activation improves erectile function in animal models of metabolic syndrome and diabetes. J Sex Med 2011; 8: 57–77.
McVary KT, Roehrborn CG, Avins AL, Barry MJ, Bruskewitz RC, Donnell RF et al. Update on AUA guideline on the management of benign prostatic hyperplasia. J Urol 2011; 185: 1793–1803.
Crawford ED, Wilsson SS, Roehroborn CG . MTOPS study group, Baseline factors as predictors of clinical progression of benign prostatic hyperplasia in men treated with placebo. J Urol 2006; 175: 1422–1426.
Yang XJ, Lecksell K, Short K, Gottesman J, Peterson L, Bannow J et al. Does long-term finasteride therapy affect the histologic features of benign prostatic tissue and prostate cancer on needle biopsy? PLESS Study Group. Proscar Long-Term Efficacy and Safety Study. Urology 1999; 53: 696–700.
Nickel JC, Downey J, Pontari MA, Shoskes DA, Zeitlin SI . A randomized placebo-controlled multicentre study to evaluate the safety and efficacy of finasteride for male chronic pelvic pain syndrome (category IIIA chronic nonbacterial prostatitis). BJU Int 2004; 93: 991–995.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Gacci, M., Vignozzi, L., Sebastianelli, A. et al. Metabolic syndrome and lower urinary tract symptoms: the role of inflammation. Prostate Cancer Prostatic Dis 16, 101–106 (2013). https://doi.org/10.1038/pcan.2012.44
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2012.44
Keywords
This article is cited by
-
Correlation between metabolic syndrome and periurethral prostatic fibrosis: results of a prospective study
BMC Urology (2024)
-
Sleep-related disorders and lower urinary tract symptoms in middle-aged and elderly males: a cross-sectional study based on NHANES 2005–2008
Sleep and Breathing (2024)
-
Simvastatin inhibits prostatic hyperplasia in rats with metabolic syndrome
International Urology and Nephrology (2022)
-
The association of pathogenic factors of metabolic syndrome on serum prostate-specific antigen levels: a pilot study
BMC Urology (2019)
-
Prostatic inflammation: a potential treatment target for male LUTS due to benign prostatic obstruction
Prostate Cancer and Prostatic Diseases (2018)