Abstract
We aimed to evaluate the efficacy and safety of combination treatment using anticholinergics with α-blocker for initial treatment of both overactive bladder (OAB) and other lower urinary tract symptoms (LUTS), secondary to BPH. A 12-week, randomized, double-blind, placebo-controlled trial was conducted at four urology clinics in Korea, involving men, aged 50 years or older, with LUTS related to BPH and OAB. A total of 176 patients were randomly assigned to receive doxazosin (4 mg) plus placebo or doxazosin (4 mg) plus tolterodine SR (4 mg), once a day for 12 weeks. Changes from baseline in total International Prostate Symptom Score (IPSS), bladder diary variables, patient perception of bladder condition (PPBC), uroflowmetry, postvoid residual volume and IPSS subscores (voiding and storage) were analyzed. Of the 176 enrolled patients, 91 had doxazosin gastrointestinal therapeutic system (GITS) and placebo, and 85 had combined medication with doxazosin GITS and tolterodine SR. Compared with the doxazosin plus placebo group, the doxazosin plus tolterodine group showed significant reductions in IPSS storage subscore and improvement in the quality of life item, urgency episodes, as well as in micturition frequency at weeks 4 and 12. However, it failed to improve PPBC at week 4 as well as at week 12. Earlier intervention with anticholinergics plus α-blocker was tolerated well, including the questions about urinary retention (n=1) and dry mouth (n=2). Initial combination treatment of anticholinergics plus α-blocker showed positive results for men with LUTS related to BPH and OAB symptoms and did not increase the risk of urinary retention.
Similar content being viewed by others
Introduction
BPH and associated lower urinary tract symptoms (LUTS) are progressive diseases that significantly affect the daily lives of sufferers.1, 2 Overactive bladder (OAB) is a serious health problem because of its high prevalence and the burdens associated with it.
The treatment of LUTS in men is complicated by the fact that storage and voiding symptoms frequently coexist.3 It is unclear whether storage symptoms may develop secondarily to benign prostatic obstruction (BPO) in men.4 However, storage symptoms often occur independently of BPO and persist in many men, despite pharmacological or surgical treatment.5 Therefore, therapies that target the prostate often fail to alleviate OAB and may not be the most appropriate therapy for men with storage LUTS.3 If OAB can be detected early, then combination therapy can be instituted and more men can show clinical improvement sooner, with no additional adverse events.
We aimed to evaluate the efficacy and safety of combination treatment using anticholinergics plus α-blocker in initial treatment of both OAB and BPH. We hypothesized that patients, with LUTS related to BPH and OAB, who were given an initial combination treatment of anticholinergics plus α-blocker would experience greater treatment benefits, without risk of acute urinary retention (AUR) or voiding difficulty, than would men who received a placebo plus doxazosin gastrointestinal therapeutic system (GITS).
Materials and methods
Study design
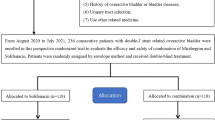
This was a 12-week, randomized, double-blind, placebo-controlled study conducted in four urology centers in Korea. Before initiating this study, we obtained approval from the institutional review board and from the ethics committee of each hospital. The symptoms of BPH were observed via maximal urinary flow rate (Qmax) assessed by uroflowmetry, postvoid residual volume (PVR) assessed by ultrasound and International Prostate Symptom Score (IPSS). Prostate volume was assessed by transrectal ultrasound of the prostate and PSA was also performed. We also evaluated the initial 3-day bladder diary of all enrolled patients, using a 5-point urgency rating scale6 and the patients perception of bladder condition (PPBC).7 After the initial evaluation, patients were randomly assigned to receive doxazosin GITS plus placebo or doxazosin GITS plus tolterodine SR (4 mg), once a day for 12 weeks. Patients were instructed to take the medication once daily at bedtime for 12 weeks. At the second (4 weeks after medication) and third visits (12 weeks after medication), all patients completed the IPSS, PPBC, 3-day bladder diary, Qmax and PVR.
Patients
A total of 176 patients with LUTS related to BPH and OAB were enrolled in this study. Eligible patients were men with LUTS who had been initially diagnosed with BPH. Inclusion criteria were: male, age 50 years or older, total IPSS of ⩾14 (voiding subscore ⩾8 and storage subscore ⩾6), IPSS quality of life (QOL) score of ⩾3, micturition frequency (⩾8 micturitions per 24 h); and urgency (⩾1 micturitions with urgency rating 3 per 24 h); prostate volume of ⩾20 cc by transrectal ultrasound of the prostate. Inclusion criteria also required the Qmax ⩽15 ml s−1 and a voided volume of at least 125 ml. We did not perform an urodynamic study. Patients were excluded if they had neurogenic bladder dysfunction, confirmed prostate cancer, acute or chronic urinary retention status, acute or chronic prostatitis within the previous 3 months, PSA levels of over 10 ng ml−1, a history of recurrent urinary tract infection or bladder stones, previous medication history for BPH and previous surgical intervention related to BPO.
Outcomes
The primary objective was to evaluate the efficacy of initial combination treatment of anticholinergics and α-blocker over 12-week period in Korean patients with LUTS related to BPH and OAB. Primary outcome was the 12-week changes in IPSS storage subscores. Secondary outcomes were the 12-week changes in the QOL scores, IPSS total scores, urinary frequency urgency in voiding diary and the incidence of AUR. We also evaluated the changes of Qmax and PVR at baseline and at weeks 4 and 12.
Statistical analysis
The intent to treat and safety populations included all randomized patients who took one or more doses of the study drug. The sample size calculations were based on an analysis of whether the effects of tolterodine and placebo were equivalent.8 The number of patients needed to detect equivalence with 90% power was 145. The randomization scheme was prepared by the study biostatistician, applying a blocked randomization to minimize systematic error and potential investigator bias. Treatment allocations were balanced across the two treatment groups and blinded to patients, site investigators and all study personal directly involved in conduct of this study.
All data were indicated as mean±s.e.m., and we analyzed the data using SPSS (version 12.0, Chicago, IL, USA). The changes from baseline in total IPSS scores, IPSS subscore (voiding and storage symptoms), QOL scores, Qmax, PVR, PPBC and urgency, frequency episodes in voiding diary were analyzed using a paired Student’s t-test. An independent t-test was used to compare data between the placebo and combination groups. A χ2-test was used to determine the statistical significance of differences in adverse events between two groups. Missing data for total IPSS, IPSS subscore, PPBC and QOL item scores were handled using the last observation carried forward technique. Diary values were averaged for all available diary days, but completion of two or more days of a three-diary period was required for the data to be included in the analysis. If fewer than 2 days of the diary period were completed, postbaseline data were imputed using the last observation carried forward.
Results
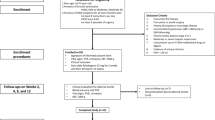
Patient disposition is shown in Figure 1, and baseline clinical characteristics are summarized in Table 1. Of the 176 men enrolled, 91 patients had doxazosin GITS and placebo, and 85 patients had combined medication with doxazosin GITS and tolterodine SR. Overall, 49 patients were lost to follow-up and dropped out, and the remaining 127 were followed up for 12 weeks (63 in the doxazosin plus placebo group versus 64 in the doxazosin plus tolterodine group). There were no significant differences in the baseline characteristics between the two groups (Table 1).
Patients reporting symptom improvement after medication at weeks 4 and 12 are shown in Table 2. The mean change in total IPSS from baseline to weeks 4 and 12 was −7.1 and −6.4 points for the doxazosin plus placebo group and −5.5 and −6.3 points for the doxazosin plus tolterodine group, respectively. The mean change in IPSS storage subscore from baseline to weeks 4 and 12 was −1.7 and −1.8 for the placebo group and −3.1 and −3.2 for the doxazosin plus tolterodine group, respectively, (Table 2). The mean change in IPSS QOL score from baseline to weeks 4 and 12 was −0.6 and −0.6 for the doxazosin plus placebo group and −1.0 and −1.3 for the doxazosin plus tolterodine group, respectively, (Table 2). In both groups, total IPSS, QOL, IPSS storage subscores were significantly improved at weeks 4 and 12 of follow-up. Compared with the placebo group, patients receiving anticholinergics plus α-blocker showed significant reductions in IPSS storage subscore at weeks 4 (P=0.024) and 12 (P=0.006) (Figure 2). IPSS QOL score in the doxazosin plus tolterodine group showed significant reductions at week 12 compared with the doxazosin plus placebo group (P=0.018). Urgency episodes in the voiding diary as well as micturition frequency were significantly improved in patients receiving tolterodine plus doxazosin at weeks 4 and 12 (Figure 2). However, the treatment failed to improve PPBC in weeks 4 and 12 in both groups.
Mean changes in IPSS total, voiding, storage and QOL scores from baseline to week 12. *P<0.05 changes from baseline to week 4 by paired t-test. †P<0.05 changes from baseline to week 12 by paired t-test. GITS, gastrointestinal therapeutic system; IPSS, International Prostate Symptom Score; QOL, quality of living.
Qmax was significantly improved in both group at weeks 4 and 12, even though there was no significant difference between the two groups (from 10.8 ml s−1 baseline to 13.9 ml s−1 at week 4 and 15.3 ml s−1 at week 12 in the doxazosin plus placebo group and from 11.1 ml s−1 at baseline to 13.9 ml s−1 at week 4 and 14.2 ml s−1 at week 12 in the doxazosin plus tolterodine group). PVR was significantly increased at week 12 in the doxazosin plus tolterodine group (from 33 cc at baseline to 36 cc at week 12) compared with the placebo group (from 34 cc at baseline to 24 cc at week 12).
There was no significant difference between the two treatment groups in the overall incidence of adverse effects (P=0.667). Earlier intervention with tolterodine plus doxazosin was tolerated well, including AUR (n=1) and dry mouth (n=2). A patient having placebo demonstrated dry mouth.
Discussion
In our study, we included male patients with both voiding and storage symptoms. Understandably, the most frequently observed LUTS in real clinical circumstances are both voiding and storage symptoms. The incidence of OAB associated with BPO is 40–75%, and because the symptoms of the two are similar and often overlap, it can be difficult to separate them diagnostically.9, 10 Both may result from pathophysiological mechanisms, such as benign prostatic enlargement, BPO, detrusor overactivity or from a combination of prostate and bladder dysfunctions.11 It is debatable whether a distinction between male LUTS and OAB is clinically relevant and whether or not it influences treatment decisions. However, most previous clinical studies focused on either of the two symptoms.12, 13, 14, 15 These studies provided limited information on the associated LUTS secondary to BPH in patients with storage symptoms. Another TIMES study16 included the more severe OAB (more than three micturitions with urgency per 24 h) than that of the International Continence Society terminology17 or other clinical studies;14, 18, 19 however, the clinically significant bladder outlet obstruction was excluded. Our study is important in that we included male patients with not only storage (storage subscore ⩾6) but also voiding (voiding sub-score ⩾8) symptoms.
Most urologists appear to give more weight, in elderly men, to voiding symptoms than to storage symptoms, and they are more concerned with the initial treatment with anticholinergics for males with storage symptoms.20, 21 The 2010 Guidelines from the European Association of Urologists suggested that combination treatment should cautiously be prescribed in men who are suspicious of having BPO. In a clinical practice setting, many physicians are still reluctant to prescribe anticholinergics because of the concern of AUR, especially in men with voiding symptoms. However, prescribing anticholinergics to men with LUTS or even voiding symptoms was not shown to elevate the risk of AUR in previous studies, which is consistent with our results.22, 23, 24 Our results will help encourage urologists to treat, initially, patients with concomitant voiding and storage symptoms with combined α-blocker and anticholinergic agent without fear of AUR.
We observed that initial combination treatment of anticholinergics was safe and more effective in men with concomitant voiding and storage symptoms than α-blocker monotherapy. Lee et al.25 observed that not only total IPSS but also patient satisfaction was better in the group with combination treatment rather than α-blocker monotherapy. However, the subtle divergence in the results of the Lee et al.25 study from those of the current trial is likely due, at least in part, to differences in study design. Both groups received active treatment (propiverine hydrochloride plus doxazosin GITS or doxazosin GITS only), and there was no placebo-controlled group.
We evaluated treatment efficacy of voiding symptoms via patient-reported outcomes (e.g., IPSS, bladder diary and PPBC). Several questionnaires such as the IPSS, PPBC, bladder diary, OAB-q, urgency perception scale, perception of treatment benefit, visual analog scale and ICIQ-male lower urinary track symptoms are available for the assessment of voiding symptoms. PPBC questionnaire is a single-item global questionnaire and is practical because of their brevity, ease of use and interpretation. Even though multi-item questionnaires such as OAB-q, KHQ, ICIQ-male lower urinary track symptoms provide a rich source of information on numerous domains of the patient’s life, such questionnaires may be difficult to score and interpret quickly, particularly in a clinical setting. In one of these, the validated PPBC, the subjects indicated which one of six statements best described the extent of their bladder-related problems on a six-point scale ranging from 1 (my bladder condition does not cause me any problems at all) to 6 (my bladder condition causes me many severe problems).7, 26 However, PPBC did not show improvement during follow-up in our study in each groups, even though both the aniticholinergic and placebo groups showed improvement of total IPSS, QOL score and IPSS storage subscore and anticholinergic group showed improvement of urgency and micturition frequency in voiding diary. Matza et al.26 reported that the PPBC should not be expected to be as reliable as multi-item scales, and recommended that it be used as a global index to complement other instruments in evaluations of treatment effectiveness. Similarly, our results suggest that PPBC is not a good tool for the evaluation of patients with LUTS related to BPH and OAB. The bladder diary is often used to qualify patients with OAB for enrollment in studies of anticholinergics. In a study analyzing the validity of a voiding diary, specifically designed to assess the OAB, the measure of urgency episodes had equal or higher interclass correlation coefficients than those for urinary frequency and incontinence episodes.27 However, patients may be unwilling to fill up the bladder diary, considering it as a nuisance. Considering the burden of keeping a bladder diary, IPSS categorized by voiding and storage subscore might be used as an efficient tool for diagnosis and treatment follow-up in men with LUTS related to BPH and OAB.
This prospective randomized study evaluated men with both voiding and storage symptoms that had not been treated previously. It is, therefore, reflective of clinical practice, as men are usually treated empirically without invasive evaluation (e.g., urodynamic study). Nevertheless, this trial should be interpreted within the context of its limitations. First, given the short duration of this trial, an investigation on tolterodine ER plus doxazosin GITS therapy for a longer period would be required. Second, the study lacked a true non-treatment group; both treatment groups received active treatment (doxazosin GITS plus tolterodine ER or doxazosin GITS plus placebo). Third, the use of a bladder diary, which is not typically used in BPH studies, may have led to behavioral modification because of increased awareness of symptoms in both treatment groups. This may have diluted the difference between the treatment groups.28 Furthermore, we did not perform statistical testing to evaluate the correlation between IPSS storage subscore and bladder diary or PPBC. This might weaken our support for IPSS in the diagnosis of patients with LUTS related to BPH and OAB. Finally, BPO or detrusor overactivity was not confirmed by objective parameters, such as urodynamic study or PSA. We only regarded the voiding and storage symptoms as the patient’s subjective symptoms scores. This selection bias might result in the low risk of BPH progression or of BPO. Finally, patient-reported outcomes (e.g., bladder diary and PPBC) provide insights into behavioral modifications that may improve symptoms by enhancing patients’ awareness of their bladder habits. Men are routinely not required to complete bladder diaries in BPH trials; therefore, the patients enrolled in our study were susceptible to the training effect of the bladder diary.
Conclusions
Initial combination treatment of anticholinergics plus α-blocker provided benefits for patients with LUTS related to BPH and OAB symptoms, and did not increase the risk of voiding difficulty and AUR. Considering the burden of keeping a bladder diary and the limitations of PPBC as an efficacy parameter, IPSS categorized by voiding and storage subscore might be used as an efficient tool for the diagnosis and treatment follow-up for patients with LUTS related to BPH and OAB.
References
Emberton M, Fitzpatrick JM, Garcia-Losa M, Qizilbash N, Djavan B . Progression of benign prostatic hyperplasia: systematic review of the placebo arms of clinical trials. BJU Int 2008; 102: 981–986.
Jacobsen SJ, Girman CJ, Lieber MM . Natural history of benign prostatic hyperplasia. Urology 2001; 58: 5–16; discussion 16.
Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol 2006; 50: 1306–1314 discussion 1314-5.
Chapple CR, Roehrborn CG . A shifted paradigm for the further understanding, evaluation, and treatment of lower urinary tract symptoms in men: focus on the bladder. Eur Urol 2006; 49: 651–658.
de Nunzio C, Franco G, Rocchegiani A, Iori F, Leonardo C, Laurenti C . The evolution of detrusor overactivity after watchful waiting, medical therapy and surgery in patients with bladder outlet obstruction. J Urol 2003; 169: 535–539.
Coyne KS, Matza L, Thompson C, Kopp Z, Jumadilova Z, Brubaker L . From an OAB patient perspective: health-related quality of life improves when frequency and urgency improve. In: 35th Annual Meeting of the International Continence Society; August 28–September 2 2005; Montreal, Quebec.
Coyne KS, Matza LS, Kopp Z, Abrams P . The validation of the patient perception of bladder condition (PPBC): a single-item global measure for patients with overactive bladder. Eur Urol 2006; 49: 1079–1086.
Takei M, Homma Y . Long-term safety, toloerability and efficacy of extended-release tolterodine in the treatment of overactive bladder in Japanease patients. Int J Urol 2005; 12: 456–464.
Blaivas JG, Marks BK, Weiss JP, Panagopoulos G, Somaroo C . Differential diagnosis of overactive bladder in men. J Urol 2009; 182: 2814–2817.
Ameda K, Sullivan MP, Bae RJ, Yalla SV . Urodynamic characterization of nonobstructive voiding dysfunction in symptomatic elderly men. J Urol 1999; 162: 142–146.
Barry MJ, Cockett AT, Holtgrewe HL, McConnell JD, Sihelnik SA, Winfield HN . Relationship of symptoms of prostatism to commonly used physiological and anatomical measures of the severity of benign prostatic hyperplasia. J Urol 1993; 150: 351–358.
Hofner K, Burkart M, Jacob G, Jonas U . Symptomatic and quality of life response to tolterodine in subgroups of men with overactive bladder symptoms and presumed non-obstructive benign prostatic hyperplasia. World J Urol 2010; 28: 353–357.
Diokno A, Sand P, Labasky R, Sieber P, Antoci J, Leach G et al. Long-term safety of extended-release oxybutynin chloride in a community-dwelling population of participants with overactive bladder: a one-year study. Int Urol Nephrol 2002; 34: 43–49.
Haab F, Cardozo L, Chapple C, Ridder AM . Long-term open-label solifenacin treatment associated with persistence with therapy in patients with overactive bladder syndrome. Eur Urol 2005; 47: 376–384.
Haab F, Corcos J, Siami P, Glavind K, Dwyer P, Steel M et al. Long-term treatment with darifenacin for overactive bladder: results of a 2-year, open-label extension study. BJU Int 2006; 98: 1025–1032.
Kaplan SA, Roehrborn CG, Rovner ES, Carlsson M, Bavendam T, Guan Z . Tolterodine and tamsulosin for treatment of men with lower urinary tract symptoms and overactive bladder: a randomized controlled trial. JAMA 2006; 296: 2319–2328.
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn 2002; 21: 167–178.
Yokoyama T, Uematsu K, Watanabe T, Sasaki K, Kumon H, Nagai A . Naftopidil and propiverine hydrochloride for treatment of male lower urinary tract symptoms suggestive of benign prostatic hyperplasia and concomitant overactive bladder: a prospective randomized controlled study. Scand J Urol Nephrol 2009; 43: 307–314.
Stewart WF, Van Rooyen JB, Cundiff GW, Abrams P, Herzog AR, Corey R et al. Prevalence and burden of overactive bladder in the United States. World J Urol 2003; 20: 327–336.
Yamaguchi O, Aikawa K, Shishido K, Nomiya M . Place of overactive bladder in male lower urinary tract symptoms. World J Urol 2009; 27: 723–728.
Lee SH, Kim JC, Lee KS, Lee JG, Park CH, Hong SJ et al. The urologist's view of male overactive bladder: discrepancy between reality and belief in practical setting. Yonsei Med J 2010; 51: 432–437.
Abrams P, Kaplan S, De Koning Gans HJ, Millard R . Safety and tolerability of tolterodine for the treatment of overactive bladder in men with bladder outlet obstruction. J Urol 2006; 175: 999–1004; discussion 1004.
Kaplan SA, Walmsley K, Te AE . Tolterodine extended release attenuates lower urinary tract symptoms in men with benign prostatic hyperplasia. J Urol 2005; 174: 2273–2275; discussion 2275–2276.
Lee JY, Kim HW, Lee SJ, Koh JS, Suh HJ, Chancellor MB . Comparison of doxazosin with or without tolterodine in men with symptomatic bladder outlet obstruction and an overactive bladder. BJU Int 2004; 94: 817–820.
Lee KS, Choo MS, Kim DY, Kim JC, Kim HJ, Min KS et al. Combination treatment with propiverine hydrochloride plus doxazosin controlled release gastrointestinal therapeutic system formulation for overactive bladder and coexisting benign prostatic obstruction: a prospective, randomized, controlled multicenter study. J Urol 2005; 174: 1334–1338.
Matza LS, Thompson CL, Krasnow J, Brewster-Jordan J, Zyczynski T, Coyne KS . Test-retest reliability of four questionnaires for patients with overactive bladder: the overactive bladder questionnaire (OAB-q), patient perception of bladder condition (PPBC), urgency questionnaire (UQ), and the primary OAB symptom questionnaire (POSQ). Neurourol Urodyn 2005; 24: 215–225.
Brown JS, McNaughton KS, Wyman JF, Burgio KL, Harkaway R, Bergner D et al. Measurement characteristics of a voiding diary for use by men and women with overactive bladder. Urology 2003; 61: 802–809.
Burgio KL, Locher JL, Goode PS, Hardin JM, McDowell BJ, Dombrowski M et al. Behavioral vs drug treatment for urge urinary incontinence in older women: a randomized controlled trial. JAMA 1998; 280: 1995–2000.
Acknowledgements
This study was supported by grants and drugs from Pfizer.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Lee, S., Chung, B., Kim, S. et al. Initial combined treatment with anticholinergics and α-blockers for men with lower urinary tract symptoms related to BPH and overactive bladder: a prospective, randomized, multi-center, double-blind, placebo-controlled study. Prostate Cancer Prostatic Dis 14, 320–325 (2011). https://doi.org/10.1038/pcan.2011.22
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2011.22
Keywords
This article is cited by
-
Treatment of Concomitant OAB and BPH
Current Urology Reports (2017)
-
Promising Molecular Targets and Biomarkers for Male BPH and LUTS
Current Urology Reports (2013)
-
Current Understanding of the Interplay between Oab & Bph
Current Bladder Dysfunction Reports (2013)
-
Contemporary Combination Therapy in the Treatment of LUTS/BPH
Current Bladder Dysfunction Reports (2013)
-
Overactive Bladder in Elderly Men: Epidemiology, Evaluation, Clinical Effects, and Management
Current Urology Reports (2013)