Abstract
To examine the effect of timely zoledronic acid (ZA) treatment on clinical outcomes and health care utilization in patients with bone-metastatic prostate cancer. Patients with prostate cancer and bone metastasis were identified in a Veterans Affairs database (01/2002–09/2009). Eligible patients had no documented skeletal-related events (SREs) before the index date (that is, the first bone metastasis diagnosis date). Patients who received early ZA treatment, defined as having a ZA infusion after the index date and before any recorded SREs, were matched 1:1 on propensity score to patients not treated with bisphosphonates (BPs). Risks of SREs, hospitalization and death during the 6-month post-index period were compared between matched cohorts using Kaplan–Meier analyses. Baseline characteristics were well balanced between the matched cohorts (n=73 per group). 6-month SRE-free survival and hospitalization-free survival were higher in patients receiving timely ZA than patients without BP treatment (91.7 versus 71.5%, P<0.01; 80.5 versus 66.3%, P=0.05, respectively). 6-month mortality risk was significantly lower in patients treated with ZA versus those without BP treatment (4.3 versus 13.8%, P=0.04). Timely ZA intervention in bone-metastatic prostate cancer patients was associated with significant reductions in 6-month risks of SREs, hospitalization and mortality, as compared with no BP treatment.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Klein EA, Thompson IM . Update on chemoprevention of prostate cancer. Curr Opin Urol 2004; 14: 143–149.
Coleman RE . Skeletal complications of malignancy. Cancer 1997; 80 (8 Suppl): 1588–1594.
Michaud LB . Managing cancer treatment-induced bone loss and osteoporosis in patients with breast or prostate cancer. Am J Health Syst Pharm 2010; 67 (7 Suppl 3): S20–S30.
Vessella RL, Corey E . Targeting factors involved in bone remodeling as treatment strategies in prostate cancer bone metastasis. Clin Cancer Res 2006; 12 (20 Suppl): S6285–S6290.
Yigitbasi O, Ozturk U, Goktug HN, Gucuk A, Bakirtas H . Prognostic factors in metastatic prostate cancer. Urol Oncol 2009; doi:10.1016/j.urolonc.2009.03.013.
DePuy V, Anstrom KJ, Castel LD, Schulman KA, Weinfurt KP, Saad F . Effects of skeletal morbidities on longitudinal patient-reported outcomes and survival in patients with metastatic prostate cancer. Support Care Cancer 2007; 15: 869–876.
Coleman RE . Metastatic bone disease: clinical features, pathophysiology and treatment strategies. Cancer Treat Rev 2001; 27: 165–176.
Polascik TJ . Bisphosphonates in oncology: evidence for the prevention of skeletal events in patients with bone metastases. Drug Des Devel Ther 2009; 3: 27–40.
Berenson JR, Rajdev L, Broder M . Managing bone complications of solid tumors. Cancer Biol Ther 2006; 5: 1086–1089.
Mohler J, Bahnson RR, Boston B, Busby JE, D'Amico A, Eastham JA et al. NCCN clinical practice guidelines in oncology: prostate cancer. J Natl Compr Canc Netw 2010; 8: 162–200.
Berruti A, Dogliotti L, Bitossi R, Fasolis G, Gorzegno G, Bellina M et al. Incidence of skeletal complications in patients with bone metastatic prostate cancer and hormone refractory disease: predictive role of bone resorption and formation markers evaluated at baseline. J Urol 2000; 164: 1248–1253.
Veri A, D'Andrea MR, Bonginelli P, Gasparini G . Clinical usefulness of bisphosphonates in oncology: treatment of bone metastases, antitumoral activity and effect on bone resorption markers. Int J Biol Markers 2007; 22: 24–33.
Small EJ, Smith MR, Seaman JJ, Petrone S, Kowalski MO . Combined analysis of two multicenter, randomized, placebo-controlled studies of pamidronate disodium for the palliation of bone pain in men with metastatic prostate cancer. J Clin Oncol 2003; 21: 4277–4284.
Dhillon S, Lyseng-Williamson KA . Zoledronic acid: a review of its use in the management of bone metastases of malignancy. Drugs 2008; 68: 507–534.
Corey E, Brown LG, Quinn JE, Poot M, Roudier MP, Higano CS et al. Zoledronic acid exhibits inhibitory effects on osteoblastic and osteolytic metastases of prostate cancer. [Erratum appears in Clin Cancer Res 2003 Apr; 9: 1574-5]. Clin Cancer Res 2003; 9: 295–306.
Saad F, Gleason DM, Murray R, Tchekmedyian S, Venner P, Lacombe L et al. A randomized, placebo-controlled trial of zoledronic acid in patients with hormone-refractory metastatic prostate carcinoma. J Natl Cancer Inst 2002; 94: 1458–1468.
Saad F, Gleason DM, Murray R, Tchekmedyian S, Venner P, Lacombe L et al. Long-term efficacy of zoledronic acid for the prevention of skeletal complications in patients with metastatic hormone-refractory prostate cancer. J Natl Cancer Inst 2004; 96: 879–882.
Weinfurt KP, Anstrom KJ, Castel LD, Schulman KA, Saad F . Effect of zoledronic acid on pain associated with bone metastasis in patients with prostate cancer. Ann Oncol 2006; 17: 986–989.
Gnant M, Mlineritsch B, Schippinger W, Luschin-Ebengreuth G, Postlberger S, Menzel C et al. Endocrine therapy plus zoledronic acid in premenopausal breast cancer. [Erratum appears in N Engl J Med 2009 May 28; 360: 2379]. N Engl J Med 2009; 360: 679–691.
Rosen LS, Gordon D, Tchekmedyian NS, Yanagihara R, Hirsh V, Krzakowski M et al. Long-term efficacy and safety of zoledronic acid in the treatment of skeletal metastases in patients with nonsmall cell lung carcinoma and other solid tumors: a randomized, Phase III, double-blind, placebo-controlled trial. Cancer 2004; 100: 2613–2621.
Matczak E, Hirsh V, Lipton A, Cook RJ, Langer C, Hei YJ et al. Effects of zoledronic acid on survival in patients with lung cancer and high baseline N-telopeptide (NTX) levels: stratified by baseline bone alkaline phosphatase (BALP). J Clin Oncol (Meeting Abstracts) 2006; 24 (Suppl): 7228.
Morgan G, Davies F, Gregory W, Bell SE, Szubert A, Navarro N et al. Evaluating the effects of zoledronic acid (ZOL) on overall survival (OS) in patients (Pts) with multiple myeloma (MM): results of the Medical Research Council (MRC) Myeloma IX study. J Clin Oncol (Post-Meeting Edition) 2010; 28 (15 Suppl): 8021.
Krupski TL, Foley KA, Baser O, Long S, Macarios D, Litwin MS . Health care cost associated with prostate cancer, androgen deprivation therapy and bone complications. J Urol 2007; 178 (4 Part 1): 1423–1428.
Winter MC, Holen I, Coleman RE . Exploring the anti-tumour activity of bisphosphonates in early breast cancer. Cancer Treat Rev 2008; 34: 453–475.
Santini D, Vincenzi B, Dicuonzo G, Avvisati G, Massacesi C, Battistoni F et al. Zoledronic acid induces significant and long-lasting modifications of circulating angiogenic factors in cancer patients. Clin Cancer Res 2003; 9: 2893–2897.
Vincenzi B, Santini D, Dicuonzo G, Battistoni F, Gavasci M, La Cesa A et al. Zoledronic acid-related angiogenesis modifications and survival in advanced breast cancer patients. J Interferon Cytokine Res 2005; 25: 144–151.
Acknowledgements
The funding for this study was provided by Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA. We wish to thank the Veterans Integrated Service Networks (VISN) 16 data warehouse for the de-identified data set. The contents of this manuscript do not represent the views of the Department of Veterans Affairs or the United States Government. The authors thank Arielle Bensimon for editing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
NV Velde, L Shi, and J Liu are affiliated with Tulane University and Southeast Louisiana Veterans Health Care System and do not have financial interest associated with this publication. Similarly, EQ Wu, M Lu, AP Yu, H Sharma and CPS Fan are employees of Analysis Group, Inc. and do not have financial interest associated with this publication. A Guo is an employee of Novartis Pharmaceuticals and may hold stocks of the company.
Rights and permissions
About this article
Cite this article
Velde, N., Wu, E., Guo, A. et al. The benefits of timely intervention with zoledronic acid in patients with metastatic prostate cancer to bones: a retrospective study of the US Veterans Affairs population. Prostate Cancer Prostatic Dis 14, 79–84 (2011). https://doi.org/10.1038/pcan.2010.49
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2010.49
Keywords
This article is cited by
-
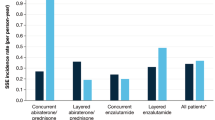
Measurement of skeletal related events in SEER-Medicare: a comparison of claims-based methods
BMC Medical Research Methodology (2015)
-
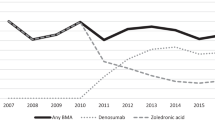
Use of intravenous bisphosphonates in patients with breast, lung, or prostate cancer and metastases to bone: a 15-year study in two large US health systems
Supportive Care in Cancer (2014)
-
Possible anti-tumor activity of initial treatment with zoledronic acid with hormonal therapy for bone-metastatic prostate cancer in multicenter clinical trial
International Journal of Clinical Oncology (2013)
-
Die ossäre Metastasierung des Prostatakarzinoms
Der Urologe (2012)